Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.27 no.2 Brasília jun. 2018 Epub 11-Jun-2018
http://dx.doi.org/10.5123/s1679-49742018000200012
ORIGINAL ARTICLE
Dengue incidence and associated costs in the periods before (2000-2008) and after (2009-2013) the construction of the hydroelectric power plants in Rondônia, Brazil*
1Universidade Federal de São Paulo, Instituto de Ciências Ambientais, Químicas e Farmacêuticas, Laboratório de Economia, Saúde e Poluição Ambiental, São Paulo, SP, Brasil
Objective:
to describe the incidence of dengue cases and associated costs in the period before and after the construction of the Jirau and Santo Antônio hydroelectric power plants (HPP), in Rondônia State, Brazil.
Methods:
economic evaluation study, based on data from the Notifiable Diseases Information System (SINAN) and the National Hospital Information System (SIH/SUS); dengue direct costs were calculated and segmented regression analysis was carried out.
Results:
dengue incidence mean was higher in the period after HPP construction (880.29/100,000 inhabitants) than before them (356.34/100,000 inhabitants) (p≤0.05); direct costs were estimated at US$3.47 million in the pre-construction period and US$7.1 million in the post-construction period.
Conclusion:
there was an increase in the incidence and direct costs of dengue after HPP construction; the environmental licensing process should include more detailed health impact assessments.
Keywords: Hydroelectric Power Plants; Dengue; Costs and Cost Analysis; Health Impact Assessment; Health Management
Introduction
In Brazil, the expansion of the electricity sector has provided many situations of direct or latent conflicts, in several communities, mainly in the Amazon Region. These conflicts are often related to the consequences of the construction of hydroelectric plants and high voltage transmission lines.1
Among the main effects resulting from this expansion of the electricity sector, we can highlight (i) disordered population growth, (ii) reduction in the availability of hunting and fishing, (iii) reduction of arable lands, (iv) reallocation of communities to other regions, often accompanied by changes in their lifestyles, (v) flooding of large territories, (vi) invasion of indigenous lands1 and (vii) proliferation of vector mosquitoes, which may lead to increased incidence of malaria, dengue, yellow fever, leishmaniasis and other infectious diseases.2
Notwithstanding the benefits that acceleration of growth can bring, it is essential to assess and monitor socio-environmental conditions in order to favor the evaluation and management of the environmental and health impacts resulting from these processes.3
According to Brazilian legislation, any enterprise considered to be potential polluters must apply for Environmental Licensing for its location, installation and operation from the competent agency (federal, state or municipal).4 The environmental licensing process includes the preparation of an environmental impact study and its respective environmental impact report (EIS-EIR). Although the institutionalization and compulsory requirement of EIS-EIR has been a milestone in the evolution of Brazilian environmentalism, there is still a need to include comprehensive assessments of health effects as part of the environmental licensing process.5
In high-income countries, methodologies such as Health Impact Assessment (HIA), which can be conducted independently from or integrated with EIS, are adopted. When negative effects on human health are identified prior to project implementation, these impacts can be mitigated as much as possible and more efficiently.6 In Brazil, with the exception of malaria, which has rules for analysis within environmental licensing,7 no specific legislation or guidelines have been articulated for other health problems, e.g. for evaluation of dengue, yellow fever, Zika and leishmaniasis.
The literature on the costs of dengue in Brazil is recent and limited, often leading to conflicting results due to the differences in the cost of hospitalization and outpatient care among the public and private sectors.8-11 In a systematic review, Constenla et al.12 concluded that the costs of dengue are substantial, with hospital care and productivity losses being the largest contributors to these costs.
In the state of Rondônia, there was a significant increase in the incidence of dengue in the period from 1999 to 2010.9 This growth may be related to the construction of hydroelectric plants and high voltage transmission lines. However, the costs of the disease were not studied considering the periods before and after this construction took place.
The objective of the present study was to describe the incidence of dengue and associated costs before (2000 to 2008) and after (2009 to 2013) the construction of Jirau and Santo Antônio hydroelectric power plants (HPP) in Rondônia, Brazil.
Methods
This is an economic evaluation study. The cost considered in this study was based on the direct cost of dengue, taking into account the number of cases reported and hospital admissions recorded.
The state of Rondônia, located in the Northern region of Brazil, has a territorial extension of 237,765,293km² and 52 municipalities. The capital of the state and its most populous municipality is Porto Velho, with 428,527 inhabitants (data from the 2010 demographic census).13 There are two HPPs built along the Madeira River. Their construction began between the end of 2008 and the beginning of 2009, and although they have been generating energy since 2012, they are still not fully completed. Jirau HPP, 120km away from the center of Porto Velho, received its Installation License in August 2008 and building work began in September 2008, while the Santo Antônio HPP is 10km from the center of Porto Velho and obtained its Installation License in June 2009 (Figure 1). The expected flooded area at Jirau HPP is 258km², whilst at Santo Antônio HPP it is 271km².

Source: Google Earth Pro®.
Figure 1 - Map of Rondônia region, highlighting the municipality of Porto Velho, Madeira river and the Jirau and Santo Antônio hydroelectric power plants
The incidence and number of hospitalizations owing to dengue were obtained from the Notifiable Diseases Information System(SINAN) and the National Hospital Information System (SIH/SUS).
In order to calculate the dengue incidence rate from 2000 to 2013, the totals of dengue cases reported on SINAN14 (ICD-10, A90) were used as numerators; the denominators (population sizes in each year) were obtained from the website of the Brazilian Institute of Geography and Statistics (IBGE). The dengue incidence rate was estimated per 100,000 inhabitants.
Segmented Regression was used to compare the periods before (period 1: 2000 to 2008) and after (period 2: 2009 to 2013) the construction of the two hydroelectric plants, as a pre-test and post-test comparison strategy, for time data. What makes this type of analysis different from other pre- and post-test measures are the conditions under which it is performed: a cut-off score between the groups analyzed, based on a specific condition. This statistical model uses as a control individuals in the pre-intervention period, dispensing the use of randomized control groups for comparison and evaluation of the efficacy of a program or treatment.15,16
The construction of the Santo Antônio HPP began at the end of 2008 and the Jirau HPP at the beginning of 2009. The segmentation of the time series between the years 2008 and 2009 was considered. Thus, what was denominated as period 1, pre-start of works (2000 to 2008), and period 2, post-start of works (2009 to 2013).
Equation 1: Segmented Regression equation This regression model is derived from Equation 1, adapted from Wagner et al.16
Where:
Yt = result of intervention over time
T = time since the beginning of the observation period
D = a dummy variable for the pre- or post-test intervention - uses zero for pre-intervention and 1 for post-intervention
P = time since intervention - uses zero for the period prior to intervention
bo = value at time zero
b2 = change in level immediately after intervention
b3 = change in slope from pre- to post-intervention period
Several methods have been used to assess health costs associated with environmental impacts. In the present study, the gross costing method was used, which identifies the cost items at high level of aggregation, encompassing some of the most relevant cost components for the service analyzed.17 The dengue cost approach considered direct costs of the disease for the health system, applying the average number of outpatient medical visits (Equation 3) to the number of cases; the mean cost of hospitalization in Brazilian National Health System (SUS) services in Rondônia was applied to cases that evolved to hospitalization (Equation 2).
Equation 2: total cost of hospitalization owing to dengue
Where:
Ctid = total cost of hospitalization owing to dengue
vi = mean value of a daily hospitalization
di = average number of days of hospitalization
ni = number of hospitalizations owing to dengue
In this case study, the mean cost of hospitalization owing to dengue was BRL285.57 and average inpatient stay was three days (SIH/SUS data), amounts shown for Rondônia in 2016. The conversion of these values from Reais into US Dollars was performed on February 3rd 2017 (US$ 1.00 = R$ 3.1235)
In this case study, the mean cost of hospitalization owing to dengue was BRL285.57 and average inpatient stay was three days (SIH/SUS data), amounts shown for Rondônia in 2016. The conversion of these values from Reais into US Dollars was performed on February 3rd 2017 (US$ 1.00 = R$ 3.1235) (Central Bank), resulting in an average cost of US$274.28 for three-day hospitalizations. As the costs of outpatient services are unavailable on SIH/SUS, the amount of direct costs as obtained by a study by Martelli et al.11 were assumed. All reported cases had at least one outpatient medical visit (Equation 3) (Central Bank), resulting in an average cost of US$274.28 for three-day hospitalizations. As the costs of outpatient services are unavailable on SIH/SUS, the amount of direct costs as obtained by a study by Martelli et al.11 were assumed. All reported cases had at least one outpatient medical visit (Equation 3).
Equation 3: total direct cost of outpatient medical care for dengue
Where:
Ctad = total cost of outpatient medical care for dengue
nd = number of dengue cases
va = mean value of the direct costs of outpatient medical care
Thus, the direct cost for dengue care provided by the public sector to the Northern region of the country was considered based on the unit amount of US$38.00,11 including medical visits, medications and examinations.11
Finally, the total costs of health system expenditure owing to dengue were calculated as the sum of hospitalization costs and outpatient costs, as expressed in Equation 4:
Equation 4: total direct cost of health due to dengue
Where:
Ctid = total cost of hospitalization for dengue
Ctad = total cost of outpatient medical care for dengue
The SPSS Statistics® version 21 was used for the analyses, and the significance level was set at p≤0.05.
The research project was approved by the Research Ethics Committee of the Federal University of São Paulo (UNIFESP) - Process No. 250.107 - on April 19th, 2013.
Results
The results of the segmented regression analysis showed that between period 1 (2000 to 2008) and period 2 (2009 to 2013) there was a significant difference in the incidence rate of dengue (p <0.001), observed by the rupture in the graph between the years of 2008 and 2009 (Figure 2). In addition, there was a significant change in incidence rate curvature (β = -0.439; p <0.001), as can be seen in Figure 2.
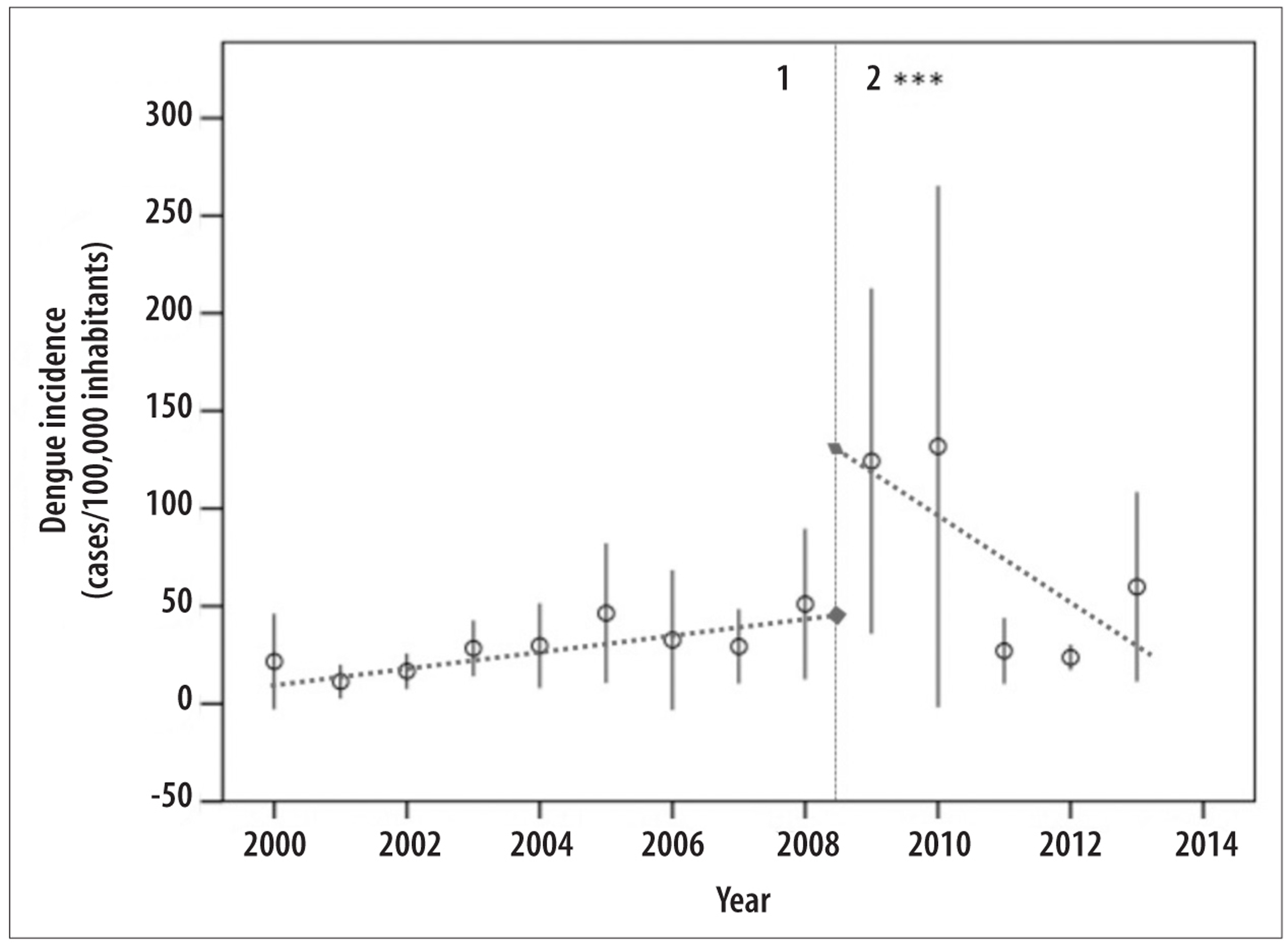
***p<0.001 for parameters: rupture in the trend line and slope differences between the 1st and 2nd periods.
Figure 2 - Annual average rate of dengue incidence, with 95% confidence intervals (95%CI) and segmented regression analysis comparing the 2000-2008 and 2009-2013 periods, in Rondônia
In Table 1, it can be verified that the average annual number of dengue cases for period 1 (period before the beginning of construction works) was 5,470 cases (average incidence rate of 356 cases/100 thousand inhabitants), representing more than US$386,000 annually, and a total of some $3.47 million in the period. From 2009 to 2013, the annual average number of cases increased to 14,708 (average incidence rate of 880 cases/100 thousand inhabitants), resulting in average annual expenses of approximately US$1.4 million, and a total of US$7.1 million in five years (Table 1). The average amount of direct costs, per reported dengue case, was approximately US$86.10.
Table 1 - Dengue incidence rate, number of notified cases, hospitalizations, and direct costs, Rondônia, 2000-2013
| Year | Incidence rate (per 100 thousand inhab.) | Number of notified cases | Number of dengue hospitalizations | Total cost of hospitalizations (US$) | Total outpatient costs (US$) | Total costs (US$) |
|---|---|---|---|---|---|---|
| 2000 | 260.07 | 3,645 | 18 | 4,937.04 | 138,510.00 | 143,447.04 |
| 2001 | 136.26 | 1,950 | 208 | 57,050.24 | 74,100.00 | 131,150.24 |
| 2002 | 200.57 | 2,928 | 716 | 196,384.48 | 111,264.00 | 307,648.48 |
| 2003 | 340.69 | 5,069 | 602 | 165,116.56 | 192,622.00 | 357,738.56 |
| 2004 | 356.86 | 5,407 | 440 | 120,683.20 | 205,466.00 | 326,149.20 |
| 2005 | 556.52 | 8,580 | 1,376 | 377,409.28 | 326,040.00 | 703,449.28 |
| 2006 | 391.44 | 6,136 | 722 | 198,030.16 | 233,168.00 | 431,198.16 |
| 2007 | 351.93 | 5,605 | 622 | 170,602.16 | 212,990.00 | 383,592.16 |
| 2008 | 612.74 | 9,908 | 1,146 | 314,324.88 | 376,504.00 | 690,828.88 |
| Annual average (2000-2008) | 356.34 | 5,470 | 650 | 178,282.00 | 207,860.00 | 386,133.56 |
| Subtotal | - | 49,228 | 5,850 | 1,604,538.00 | 1,870,664.00 | 3,475,202.00 |
| 2009 | 1,491.28 | 24,466 | 4,281 | 1,174,192.68 | 929,708.00 | 2,103,900.68 |
| 2010 | 1,581.37 | 26,306 | 4,679 | 1,283,356.12 | 999,628.00 | 2,282,984.12 |
| 2011 | 325.27 | 5,483 | 2,139 | 586,684.92 | 208,354.00 | 795,038.92 |
| 2012 | 284.96 | 4,865 | 1,559 | 427,602.52 | 184,870.00 | 612,472.52 |
| 2013 | 718.60 | 12,419 | 3,020 | 828,325.60 | 471,922.00 | 1,300,247.60 |
| Annual average (2009-2013) | 880.29 | 14,708 | 3,135,6 | 860,032.37 | 558,904.00 | 1,418,928.77 |
| Subtotal | - | 73,539 | 15,678 | 4,300,161.84 | 2,794,482.00 | 7,094,643.84 |
| Total | - | 122,767 | 21,528 | 5,904,699.84 | 4,665,146.00 | 10,569,845.84 |
The mean number of hospitalizations also showed differences between the two periods: in period 1, this average represented about 650 hospitalizations, while in period 2, it increased to more than 3,100 cases (Table 1).
Discussion
The present study presents the direct costs of dengue for the health system during 14 years in the state of Rondônia. It innovates by discussing costs and a possible association between dengue cases and population growth as a result of major infrastructure works, such as HPP construction on the Madeira River within the city limits of the state capital, Porto Velho.
The results indicated that, from 2000 to 2013, more than 122 thousand dengue cases were reported in Rondônia, with more than 21,000 hospitalizations, resulting in an estimated cost of US$10,569,845.84. This amount corresponds only to the direct costs subsidized by SUS and are considerably underestimated since they do not consider salary losses, absenteeism, reduction in the quality of life, incapacities, besides not including underreported cases. In Brazil, under-reported cases of dengue are estimated to range from 16.9 to 26.7 times the number of reported cases.18
The main limitation of this study is related to the method used, depending on the number of dengue cases recorded in a passive surveillance system (SINAN). In addition, the macro-accounting method is less sensitive than micro-accounting, because it does not use primary data to verify the cost of dengue. Also, it was not the purpose of this study to assess the indirect costs of the disease. In this way, the total costs for individuals were disregarded.
Direct costs in health services - as well as indirect costos - owing to dengue are not easily obtained and can vary significantly between studies. According to Vieira Machado et al.,10 the direct costs of hospitalizations owing to dengue in the private sector in 2010 were 280% higher than in public services. As a result, their average cost of hospitalization was US$740.10, with an average change in direct expenses ranging from US$ 428.70 in the public sector to US$1,003.50 in the private sector. In our study, the average cost considered per hospitalization was US$273.88, based on the amounts provided for the state of Rondônia. This average is lower than that reported in other studies, since the present study did not consider the values of hospital admissions at private hospitals, nor the indirect costs.10,19 In addition, the financial amounts transferred to public hospitals are often insufficient to meet to the real cost of an individual with dengue, especially in the most severe cases.10,11
In a study conducted in the municipality of Goiânia, capital of the state of Goiás,19 the authors considered the direct and indirect costs of dengue cases, reaching an average of US$291 for outpatient cases and US$676 for hospitalizations. The same study found an average cost for each reported case of dengue of approximately US$351 in 2005.19 However, the public and the private sectors usually present quite different costs for outpatient cases and hospitalizations. According to a micro-cost analysis performed in a Brazilian multicenter cohort study, the authors showed that outpatient direct costs ranged from $31 to $89 for the public sector and from $91 to $168 for the private sector. The direct cost of hospitalizations varied between US$198 and US$376 for the public sector and between US$318 and US$906 for the private sector among the regions studied (2013 data).11
We can notice a difference in costs between the public and private sectors. This can lead to health institutions facing underpayments and losses, and can even compromise SUS sustainability. The annual national economic impact was US$164 million, from the public paymaster’s perspective, but it could be as much as $447.00 million (adjusting for underreporting).11
In this study, we also analyzed the differences between two periods, 2000-2008 and 2009-2013, whereby there was a large increase in the incidence of dengue cases in the state of Rondônia, especially in 2009 and 2010. The average costs of hospitalization and outpatient care increased 3.7-fold, from US$386,000 annually in the 1st period to more than US$1.4 million annually in the 2nd period.
The 2nd period began with a high number of dengue cases, and a subsequent decrease over time. There was a large outbreak of dengue in Rondônia between 2009 and 2010.
Some factors may be related to the large increase in dengue cases in 2009 and 2010, such as temperature rise, lack of infrastructure, population density growth, disorderly planning and accelerated urbanization.20 According to the study by Struchiner et al.,21 population growth seems to play a more important role than temperature increase, considering the development of Aedes mosquitoes. Urbanization substantially increases density, larval development rate, and survival time of the adult mosquito.22 This points to the negative impacts of urbanization and population growth in municipalities with little infrastructure. With the advent of the Growth Acceleration Program (PAC) in Rondônia, centered in Porto Velho in 2008 and 2009, the municipality and its surrounding areas suffered disorderly growth, overburdened health services and high population growth, suggesting that this factor may be associated with an increase in the number of dengue cases.
The construction of the Jirau and Santo Antônio HPPs has affected a wide range of health determinants. Analyzing the effects of population growth more deeply could lead to a more transparent economic assessment of the process. For example, the number of jobs that HPP construction has brought to the region is emphasized; however, the effects of the disorderly growth of the population in regions that lack infrastructure can result in serious health outcomes.1
The increase in reported and confirmed dengue cases in Rondônia, from 2008 to 2010, was also found in a study by Lucena et al.8 These authors confirm that reported dengue cases in 2008 were about 185.6% higher than in 2007. The predominant serotype was DENV-3, which was common in the region at that time.8 This leads to a hypothesis: the disorderly growth of cities owing both to urbanization and to the jobs generated by the HPP construction works, may have attracted people who did not belong to that region and who were therefore not immune to the local circulating dengue serotypes.8 This influx of people, not immune to this serotype, may have caused the high number of notifications in the years that followed, with a subsequent fall in the number of cases as the population acquired antibodies to that serotype. In addition, it is possible that the reintroduction of DENV-1 and DENV-2 serotypes occurred in Rondônia due to the large increase in dengue cases in ten municipalities in the state, which could also have affected dengue control in 2008.23
The possible association of increased dengue incidence with the onset of the infrastructure projects referred to in this research is particularly important since SUS is burdened with the majority of health losses. The indication that the HPP entrepreneurs should be held accountable for having contributed significantly to the increase in dengue cases, due to disordered population growth, would facilitate the creation of effective ways of mitigating its effects on health, providing better living conditions for the population, as well as partial unburdening of the State and of health facilities in the region. Furthermore, given the fact that the dengue vector can also transmit Zika and chikungunya,24 comprehensive analysis of health impacts like these using appropriate measures is of the utmost importance, , such as health impact assessment (HIA) as part of the environmental licensing process.
The HPP reservoirs themselves cause many environmental impacts: they eliminate natural ecosystems, but also block the migration of fish, affecting biodiversity and commercial production. In addition, they cause changes in flood patterns and may affect floodplain lakes and downstream fishing.25 The construction of these power plants is believed to have brought thousands of jobs to the region, leading to intense population migration and increased income in the region. However, during the construction phase of a hydroelectric plant, while many workers are employed in the initial phases, during the operational phases of an HPP, the number of workers required decreases drastically, reaching less than 10% of the workforce initially contracted, which can have overwhelming effects in the region if measures are not taken to reallocate workers.26
In Brazil, the only normative health analysis that must be considered in EIS-EIR for projects in the Amazon Region is their malarigenous potential.7 Although it is a relevant factor, this analysis is extremely insufficient for obtaining a process HIA and it is likely that this negligence overloads the health system, thus implying a greater burden on the population and the government. It is known that HPP can increase mosquito proliferation, which is why several vectors must be considered in order to carry out mitigation measures, and not just the malarigenous potential of projects.
When issuing environmental licenses in Brazil, it is common practice to analyze health impacts superficially,27 and there is a need to include more detailed forms of analysis, as proposed by several researchers.5,6,28 Since there is no mandatory standard for the evaluation of health impacts, whether in national policies, projects or programs, the HIA methodology, applied in developed countries and which is even the subject of a national implementation guide published by the Brazilian Ministry of Health,27 arises as a possible structured way of bringing together analysis, work in partnership, public consultation and the evidence available for better decision-making.27,29
Encouraging dialogue among the various stakeholders, the population and entrepreneurs and investors of the different economic sectors of the country or region, can result in joining efforts for the implementation of efficient mitigation policies. In this scenario, associating economic costs with health outcomes, such as an estimate of the total cost of the disease or the willingness to pay for a reduction of these effects, could represent a strategy for discussing and encouraging the inclusion of health in discussions and decision-making about this type of enterprise.30 Because this is a complex problem to solve, we recommend work in partnership, between entrepreneurs and the federal government, taking into account appropriate HIA tools, in order to intensify actions to prevent the population from being infected with diseases such as dengue.
Acknowledgments
To Gianni Mara Silva dos Santos, of the Federal University of São Paulo (UNIFESP), for her contribution with the statistical analyses. To the Health Ministry’s Health Surveillance Secretariat (SVS/MS), for the funding provided.
REFERENCES
1. Koifman S. Geração e transmissão da energia elétrica: impacto sobre os povos indígenas no Brasil. Cad Saúde Pública. 2001 mar-abr;17(2):413-23. [ Links ]
2. Guerra SMG, Carvalho AV. Um paralelo entre os impactos das usinas hidrelétricas e termoelétricas. Rev Adm Empres. 1995 jul-ago;35(4): 83-90. [ Links ]
3. Pereira CAR, Winkler MS, Souza SH. Análise de condições ambientais em comunidades ribeirinhas de Porto Velho, Rondônia, Brasil. Rev Bras Geogr Fís. 2016;9(2): 440-55. [ Links ]
4. Brasil. Ministério do Meio Ambiente. Conselho Nacional do Meio Ambiente. Resolução CONAMA nº 001, de 23 de janeiro de 1986. Dispõe sobre critérios básicos e diretrizes gerais para a avaliação de impacto ambiental. Diário Oficial da República Federativa do Brasil, Brasília (DF), 1986 fev 17; Seção 1:2548-9. [ Links ]
5. Silveira M, Araújo Neto MD. Environmental licensing of major undertakings: possible connection between health and environment. Ciênc Saúde Coletiva. 2014 Sep;19(9):3829-38. [ Links ]
6. Abe KC, Miraglia SGEK. Avaliação de Impacto à Saúde (AIS) no Brasil e América Latina: uma ferramenta essencial a projetos, planos e políticas. Interface (Botucatu). No prelo 2017. [ Links ]
7. Brasil. Ministério do Meio Ambiente. Conselho Nacional do Meio Ambiente. Resolução CONAMA nº 286, de 30 de agosto de 2001. Dispõe sobre o licenciamento ambiental de empreendimentos nas regiões endêmicas de malária. Diário Oficial da República Federativa do Brasil, Brasília (DF), 2001 dez 17; Seção 1:223. [ Links ]
8. Lucena LT, Aguiar LO, Bogoevich ACA, Azevedo FS, Santos ACP, Vale DBAP, et al. Dengue na Amazônia: aspectos epidemiológicos no Estado de Rondônia, Brasil, de 1999 a 2010. Rev Pan-Amaz Saúde. 2011 set;2(3):19-25. [ Links ]
9. Parente MPPD. Impacto econômico do episódio da dengue na cidade de Teresina, Piauí, Brasil [tese]. Goiânia: Universidade Federal de Goiás; 2014. [ Links ]
10. Vieira Machado AA, Estevan AO, Sales A, Brabes KC, Croda J, Negrão FJ. Direct costs of dengue hospitalization in Brazil: public and private health care systems and use of WHO guidelines. PLoS Negl Trop Dis. 2014 Sep;8(9): e3104. [ Links ]
11. Martelli CMT, Siqueira Júnior JB, Parente MP, Zara AL, Oliveira CS, Braga C, et al. Economic impact of dengue: multicenter study across four Brazilian regions. PLoS Negl Trop Dis. 2015 Sep;9(9):e0004042. [ Links ]
12. Constenla D, Garcia C, Lefcourt N. Assessing the economics of dengue: results from a systematic review of the literature and expert survey. Pharmacoeconomics. 2015 Nov;22(11): 1107-35. [ Links ]
13. Ministério das Cidades (BR). Instituto Brasileiro de Geografia e Estatística. Cidades - Rondônia e Porto Velho [Internet]. 2017 [citado 2017 set 30]. Disponível em: Disponível em: https://cidades.ibge.gov.br/brasil/ro/porto-velho/panorama . [ Links ]
14. Ministério da Saúde (BR). Sistema de Informação de Agravos de Notificação (SINAN) [Internet]. 2016 [citado 2016 out 17]. Disponível em: http://portalsinan.saude.gov.br/. [ Links ]
15. Bando DH, Kawano MK, Kumagai LT, Gouveia JLV, Reis TM, Bernardo ES, et al. Tendência das taxas de mortalidade infantil e de seus componentes em Guarulhos-SP, no período de 1996 a 2011. Epidemiol Serv Saúde. 2014 out-dez;23(4):767-72. [ Links ]
16. Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002 Aug;27(4): 299-309. [ Links ]
17. Tan SS, Rutten FF, Van Ineveld BM, Redekop WK, Hakkaart-van Roijen L. Comparing methodologies for the cost estimation of hospital services. Eur J Health Econ. 2009 Feb;10(1):39-45. [ Links ]
18. Sarti E, L’Azou M, Mercado M, Kuri P, Siqueira Júnior JB, Solis E, et al. A comparative study on active and passive epidemiological surveillance for dengue in five countries of Latin America. Int J Infect Dis. 2016 Mar;44: 44-9. [ Links ]
19. Suaya JA, Shepard DS, Siqueira Júnior JB, Martelli CT, Lum LC, Tan LH, et al. Cost of dengue cases in eight countries in the Americas and Asia: a prospective study. Am J Trop Med Hyg. 2009 May;80(5):846-55. [ Links ]
20. Böhm AW, Costa CD, Neves RG, Flores TR, Nunes BP. Dengue incidence trend in Brazil, 2002-2012. Epidemiol Serv Saúde. 2016 Oct-Dec;25(4):725-33. [ Links ]
21. Struchiner CJ, Rocklov J, Wilder-Smith A, Massad E. Increasing dengue incidence in singapore over the past 40 years: population growth, climate and mobility. PLoS One. 2015 Aug;10(8):e0136286. [ Links ]
22. Li Y, Kamara F, Zhou G, Puthiyakunnon S, Li C, Liu Y, et al. Urbanization increases Aedes albopictus larval habitats and accelerates mosquito development and survivorship. PLoS Negl Trop Dis. 2014 Nov;8(11):e3301. [ Links ]
23. Ministério da Saúde (BR). Fundação Nacional de Saúde. Programa nacional de controle da dengue (PNCD): instituído em 24 de julho de 2002 [Internet]. Brasília: Fundação Nacional de Saúde (FUNASA); 2002 [citado 2017 dez 9]. 32 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/pncd_2002.pdf . [ Links ]
24. Vasconcelos PFC. Doença pelo vírus Zika: um novo problema emergente nas Américas? Rev Pan-Amaz Saúde. 2015 jun;6(2): 9-10. [ Links ]
25. Fearnside MP. Hidrelétricas na Amazônia: impactos ambientais e sociais na tomada de decições sobre grandes obras [Internet]. Manaus: Ed. do INPA, 2015 [citado 2017 dez 9]. 296 p. Disponível em: Disponível em: http://philip.inpa.gov.br/publ_livres/2015/Livro-Hidro-V1/Livro%20Hidrel%C3%A9tricas%20V.1.pdf . [ Links ]
26. Alves J, Thomaz Junior A. A migração do trabalho para o complexo hidrelétrico madeira. In: Anais da XIII Jornada do trabalho: a irreformabilidade do capital e os conflitos territoriais no limiar do século XXI. Os novos desafios da geografia do trabalho; 2012 9 out - 12 out; Presidente Prudente (SP). Presidente Prudente (SP): Universidade Estadual Paulista; 2012. p. 1-17. [ Links ]
27. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigiância em Saúde Ambiental e Saúde do Trabalhador. Avaliação de impacto à saúde - AIS: metodologia adaptada para aplicação no Brasil [Internet]. Brasília: Ministério da Saúde; 2014 [citado 2017 dez 9]. 68 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/avaliacao_impacto_saude_ais_metodologia.pdf . [ Links ]
28. Barbosa EM, Barata MML, Hacon SS. A saúde no licenciamento ambiental: uma proposta metodológica para a avaliação dos impactos da indústria de petróleo e gás. Ciênc Saúde Coletiva. 2012 fev;17(2):299-310. [ Links ]
29. Lock K. Health impact assessment. BMJ. 2000 May;320(7246):1395-8. [ Links ]
30. Abe KC, Miraglia SG. Health impact assessment of air pollution in São Paulo, Brazil. Int J Environ Res Public Health. 2016 Jul;13(7):E694. [ Links ]
Article based on a research Project of the Laboratory of Economics, Health and Environmental Pollution of the Federal University of São Paulo (UNIFESP), entitled ‘Health Impact Assessment of the implementation of major enterprises’, by Simone G. E. K. Miraglia and on the PhD thesis by Karina Camasmie Abe, entitled ‘Analysis of the Health Impact Assessment methodology in Brazil with a focus on large enterprises and public policies’, defended at the UNIFESP Post-graduation Program in Health Management and Informatics, in 2017. The study was funded by the Health Ministry’s Health Surveillance Secretariat (SVS/MS) - Cooperation Term No. 201/2012 - and by the Education Ministry’s Coordination for the Improvement of Higher Education Personnel (Social Demand Program/CAPES/MEC).
Received: June 12, 2017; Accepted: November 22, 2017










 texto en
texto en 


