INTRODUCTION
Mortality information is useful for measuring the impact of health interventions.1 The World Health Organization (WHO) has established a set of guidelines and rules for the coding and selection of the underlying cause of death, aimed at medical certification; however, there are concerns about the reliability of this coding.2)-(5 Inter-coder agreement is higher in countries where specific coder engagement and retention policies have been implemented, reaching nearly 80%.2),(6 Similarly, automated coding software achieves comparable performance.
Incorrect use of coding and definition of the underlying cause of death affects data quality and its comparability between countries. There is software for automating these notifications, which is increasingly being adopted by countries,7)-(10 indicating a trend in the use of artificial intelligence in this process.11 In Latin America, there are experiences of implementing such software, from Mexico to Brazil, Chile, Colombia and Peru.12
Specifically, in Peru, in 2017, the Sistema Informático Nacional de Defunciones (SINADEF) was implemented, enabling death certificates to be performed via electronic forms in real time, improving the quality and timeliness of notifications.13),(14 The Peruvian Ministry of Health (MINSA) also decided to adopt the Iris software, developed by an international consortium led by the German Institute of Medical Information and Documentation, which uses an algorithm based on the rules of the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10), in order to automate the coding and selection of the underlying cause of death.15
The objective of this research note was to describe software performance in the automatic selection of the underlying cause of death in Peru between 2016 and 2019.
METHODS
Study design
This was a descriptive study on software performance in the automatic selection of the underlying cause of death in Peru, between 2016 and 2019. This performance was defined as the software’s ability to obtain the underlying cause of death
Setting
By 2016, all deaths were documented on paper-based death certificates, transcribed into a desktop software called Vital Events and submitted to MINSA as files. In 2017, the Web-based SINADEF was implemented. This system allows death certificates to be registered in two ways: either directly typed online by physicians; or transcribed from paper-based formats. In 2018, the Iris software was adopted, and since 2016, mortality databases have been processed using this application to determine the underlying causes of death. The Iris dictionary was adapted with 12,246 medical terms in natural language, using the causes of death directly filled in by doctors as a reference.
Participants
This study included deaths that occurred in Peru between 2016 and 2019.16 Undeclared deaths and those that were not available at the time of data processing using the software were excluded.
Variables
The variables investigated were as follows: processed death certificate (with underlying cause of death; without underlying cause of death); recorded medical terms (with ICD-10 code; without ICD-10 code); type of error on the death certificate rejected by the software (syntax; code; system); type of death certificate (paper-based format; online); and year of death (2016 to 2019).
Data sources and measurement
The data source was comprised of death certificate databases covering the period from 2016 to 2019, provided by the MINSA in spreadsheet format. The data were processed using Iris on the following dates: 2016 mortality database on 06/01/2018; 2017 database on 04/26/2019; 2018 database on 6/20/2020; and 2019 database on 6/22/2021.
Bias control
Mortality database records underwent quality control to remove any potential duplicate records or modify records with inconsistent data.
Statistical methods
The variables obtained after processing using Iris were presented in simple frequency distribution tables. The trend analysis was performed using the chi-square test for trend. The Iris performance index (number of death certificates with underlying cause of death divided by the total number of death certificates) and the Iris performance index in ICD-10 coding (number of medical terms with ICD-10 codes divided by the total number of medical terms) were considered dependent variables; and the independent variable was the year of death. Pearson’s correlation coefficient and the coefficient of determination (R2) were used to analyze the linear correlation between the type of death certificate and Iris performance. The significance level used was 5%. Microsoft Excel® 2016 software was used for the analyses.
Ethical aspects
The study was based on the analysis of variables included in the mortality databases of the MINSA, also available on the National Open Data Platform https://www.datosabiertos.gob.pe/, which do not contain information that would allow the identification of deceased individuals.
RESULTS
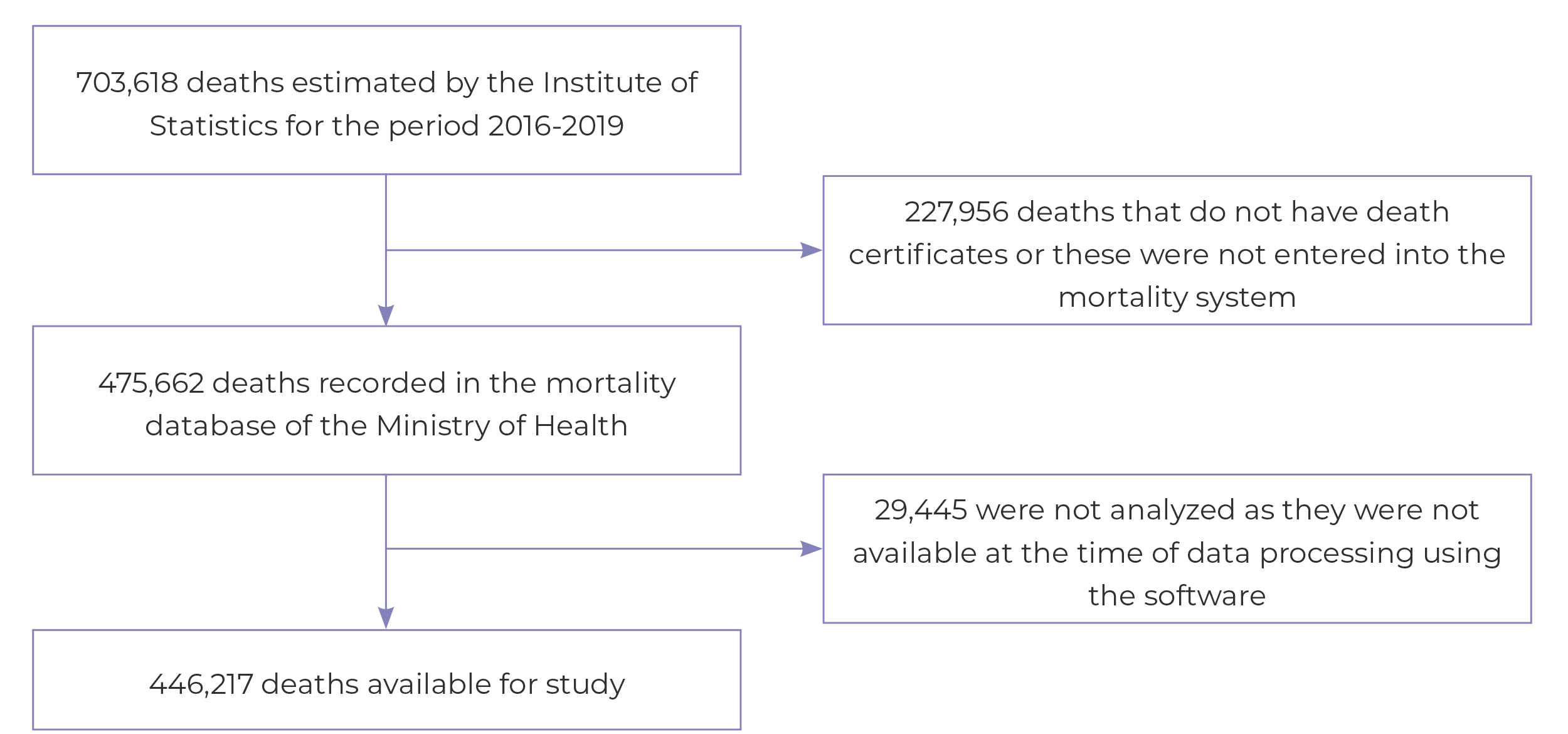
Between 2016 and 2019, a total of 446,217 deaths of residents in all regions of Peru, recorded in the MINSA mortality database, were analyzed. This amount corresponded to 67% of the estimated deaths for the study period. Deaths that were not registered on the mortality system at the time of processing were excluded (Figure 1).
It could be seen a progressive increase in the software performance index, with the percentage of processed death certificates ranging from 69.6% in 2016 to 78.8% in 2019 (p-value < 0.001) (Table 1).
Table 1 Software performance in the selection of the underlying cause of death and death certificate processing (n = 446,217), Peru, 2016-2019
| Software performance | 2016 | 2017 | 2018 | 2019 | p-valuea | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Processed death certificates | < 0.001 | ||||||||
| With underlying cause of death | 67,697 | 69.6 | 86,848 | 71.8 | 79,979 | 74.8 | 95,405 | 78.8 | |
| Without underlying cause of death | 29,542 | 30.4 | 34,174 | 28.2 | 26,926 | 25.2 | 24,653 | 21.2 | |
| Total | 97,241 | 100.0 | 121,024 | 100.0 | 106,905 | 100.0 | 121,047 | 100.0 | |
| Processed medical terms | < 0.001 | ||||||||
| With ICD-10 codes | 222,446 | 87.2 | 321,904 | 89.8 | 299,988 | 91.1 | 346,635 | 92.7 | |
| Without ICD-10 codes | 32,641 | 12.8 | 36,623 | 10.2 | 29,401 | 8.9 | 27,297 | 7.3 | |
| Total | 255,087 | 100.0 | 358,527 | 100.0 | 329,389 | 100.0 | 373,932 | 100.0 | |
| Death certificates rejected by type of error | < 0.001 | ||||||||
| Syntax error | - | - | 744 | 2.3 | 545 | 2.1 | 582 | 2.4 | |
| Code error | 26,819 | 90.8 | 30,337 | 94.0 | 24,616 | 94.9 | 23,130 | 93.8 | |
| System error | 2,725 | 9.2 | 1,185 | 3.7 | 790 | 3.0 | 941 | 3.8 | |
| Total | 29,544 | 100.0 | 32,266 | 100.0 | 25,951 | 100.0 | 24,653 | 100.0 | |
| Type of death certificate | < 0.001 | ||||||||
| Paper-based format | 96,605 | 100.0 | 85,986 | 71.0 | 32,227 | 30.1 | 25,397 | 21.0 | |
| Online | 636 | 0.0 | 35,038 | 29.0 | 74,678 | 69.9 | 95,650 | 79.0 | |
| Total | 97,241 | 100.0 | 121,024 | 100.0 | 106,905 | 100.0 | 121,047 | 100.0 | |
a) Chi-square test for trend.
There was also an increasing trend in the software performance index in ICD-10 coding, with a progressive increase in the proportion of this performance: from 87.2% in 2016 to 92.7% in 2019 (p-value < 0.001). However, the highest proportion of errors in the records that the software failed to process were coding errors (Table 1).
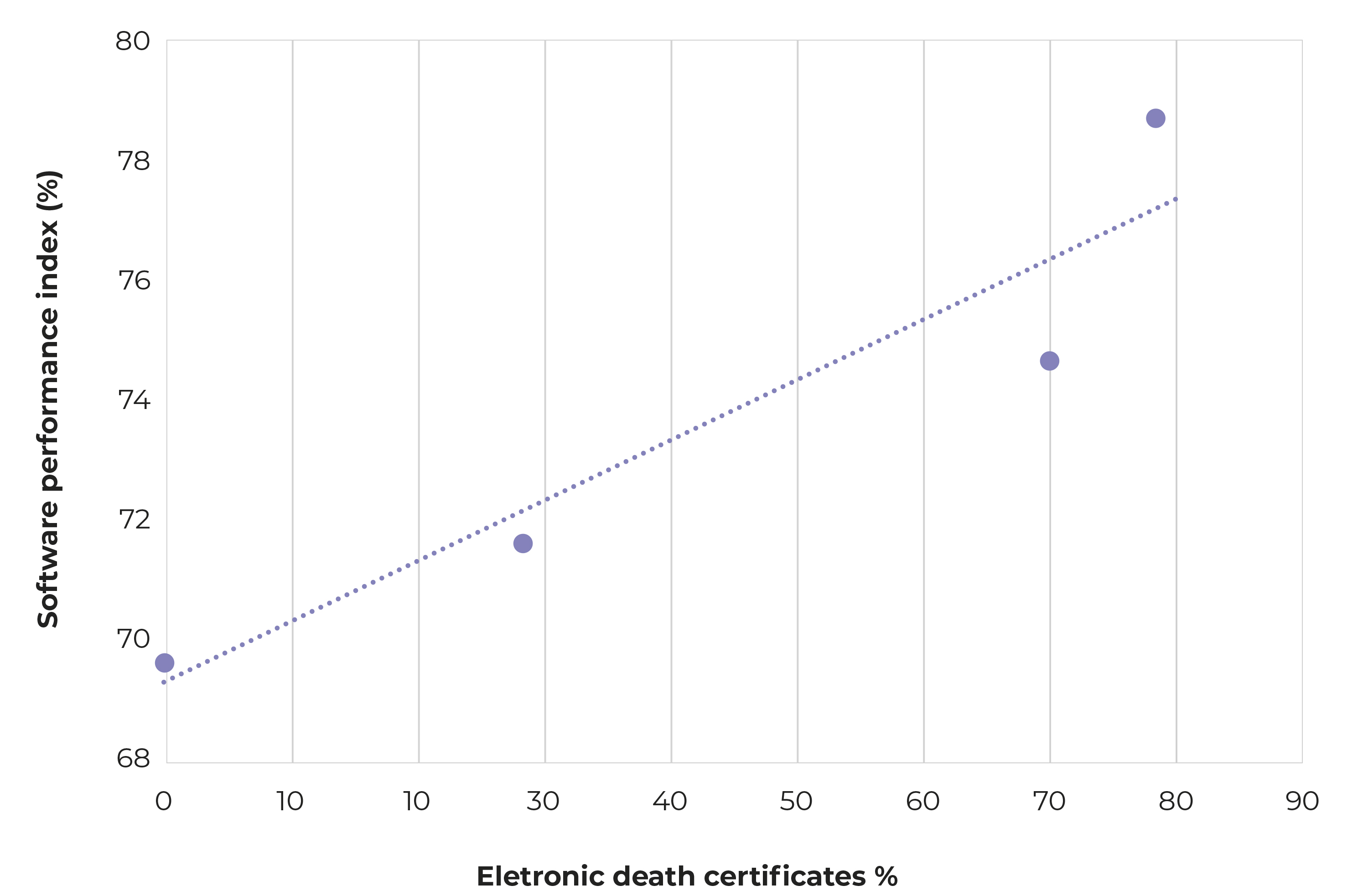
It could be seen a direct linear correlation between the proportion of death certificates directly filled out by physicians on SINADEF and the Iris performance: Pearson’s correlation coefficient = 0.95; R2 = 0.89 (Figure 2).
DISCUSSION
During the study period, the software performance increased due to the progress in its ability to code the terms used by physicians for reporting causes of death with ICD-10. There was a correlation between the proportion of declarations directly filled out by the physicians and the software performance. The implementation of SINADEF played an important role in this process, enabling the development of a dictionary adapted to the Peruvian context and contributing to an increasing number of medical terms each year. Studies have shown improvements achieved after training physicians in filling out death certificates, and in the quality of the data they record,17),(18 in addition to the possibility of improving the software performance.
One limitation of this study lies in the lack of an analysis of the agreement between the software and the application of rules by experienced coders. In Peru, this type of analysis is difficult because, before the implementation of SINADEF, most death certificates were coded by employees without formal training in ICD-10. A second limitation is related to the fact that, in this study, the Iris performance was not analyzed by sociodemographic variables or disease group.
The highest performance of the software was around 80%. A study conducted in São Paulo, in 2010, with a sample of 666 deaths aimed at testing the software Portuguese dictionary, found a performance of 95%.19 In the Netherlands, during a study on the implementation of an automated coding system with data from 134,262 deaths that occurred in 2009, there was an increase in performance from 17% in the first batch to 69% in the last batch, after a series of improvements in the dictionary.20 In Spain, a study to assess the impact of automating cause of death records on mortality in the autonomous community (geopolitical macro-region) of Navarra, based on 5,060 deaths that occurred in 2014, identified a performance of 90%.21 When evaluating the use of Iris in a small sample of deaths in Burkina Faso, a performance of 90% was found.10
In this study, automatic coding of medical terms for causes of death was 93%, while in Italy, in 2016, this proportion was 78%.22
Most of the errors that led the software to reject a death certificate occurred during coding: typos, spelling errors, or errors with unusual characters.19 However, the software also faces challenges in accurately coding external causes of death, because forensic medical examiner use a wide range of causes of death, which affects the efficiency of the dictionary.20
There is a global movement towards automated selection of the underlying cause of death. Nearly all countries in the European Union use Iris. In Latin America, the software is being implemented in several countries. In Brazil, it has been integrated into a mobile application for doctors, aiming to improve the completion of the Death Certificate (DC).23),(24
It can be concluded that there is a trend of improvement in the performance of the software for selecting the underlying cause of death in Peru. This improvement seems to be associated with the implementation of the SINADEF and the optimization of the dictionary of medical terms. Further studies on Iris are needed to assess the impact of the software on mortality statistics. Taking into consideration that its implementation in the region will enhance data comparability, it is necessary to study the agreement between the medical terms of the dictionaries used in South American countries.











 texto en
texto en