Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.27 no.2 Brasília jun. 2018 Epub 17-Abr-2018
http://dx.doi.org/10.5123/s1679-49742018000200003
ORIGINAL ARTICLE
Temporal trend and associated factors to advanced stage at diagnosis of cervical cancer: analysis of data from hospital based cancer registries in Brazil, 2000-2012*
1Universidade do Estado do Rio de Janeiro, Instituto de Medicina Social, Rio de Janeiro, RJ, Brasil
Objective:
To analyze the time trend and analyze the determinants of stage at diagnosis of cervical cancer in Brazil.
Methods:
Time trend analysis and cross-sectional study using data from hospital-based cancer registries (2000-2012); multinomial and joinpoint regression statistical models were used.
Results:
65.843 cases were analyzed; the median interval between diagnosis and treatment was 59 days; the percentage of advanced staging increased, annual percent change 1.10% (95%CI 0.80;1.50); women with higher education (compared to unlettered) had less odds of late stage diagnosis (OR=0.38; 95%CI 0.31;0.47); among indigenous (OR=2.38; 95%CI 1.06;5.33) and black women (OR=1.16; 95%CI 1.02;1.31), compared to white, and in the North region (OR=2.55; 95%CI 2.26;2.89), compared to the Southeast, the odds was higher; other factors positively related to advanced stage were 'age', 'histology', and marital status'.
Keywords: Uterine Cervical Neoplasms; Women's Health; Hospital Records; Health Services Accessibility; Medical Oncology
Introduction
The cancer of the uterine cervix occupies a prominent place among the tumors that affect women around the world, with frequent occurrence, especially in less developed regions.1 In 2012, the mortality rate for this type of cancer came to be 18 times higher in areas with fewer resources, such as the Central Africa, when compared to high-income countries, such as in Western Europe. In the same year, it was the fourth type of cancer more common in women in the world, with 85% of the cases in middle and low income countries.1
In Brazil, there were an estimated 16,340 new cases in 2016, with an incidence of 15.85 cases per 100 thousand women.2 It was the most common cancer among women in the Northern region of the country and the second in incidence in the Midwest and Northeast regions.2 The national mortality rate, standardized by age, estimated for 2012, was 7.3 per 100 thousand women.1
The implementation of organized screening can lead to a reduction of approximately 80% in mortality from the disease, as observed in high-income countries since the beginning of the 20th century.3 In middle and low income countries, the results are less expressive due to limitations of access to health services, low coverage of screening programs and delays in the implementation of diagnostic and therapeutic procedures.4,5
With the objective of guaranteeing comprehensive care to individuals with a diagnosis of cancer, the Ministry of Health of Brazil, by means of decree GM/MS No. 2,439, of 8 December 2005, established the National Policy of Oncology Care, emphasizing the importance of prevention, early diagnosis and timely treatment as measures to reduce the incidence and mortality from the disease.6
Recent studies addressed the risk of diagnosis in advanced stage and the time for initiation of treatment in Brazil,7,8 turning up the debate about a trend of increasing percentage of diagnosis in advanced stage even in a context of increasing availability of screening in the country, especially since the decade of 1990.5
The objectives of the present study were to analyze the temporal trends and factors associated with the diagnosis in advanced stages of cervical cancer in Brazil.
Methods
The proportion of patients diagnosed with cancer of the uterine cervix in stages III and IV since 2000 to 2014 was calculated and selected epidemiological and clinical characteristics associated with being diagnosed in late stages were analyzed in this study.
The dataset relating to health units (clinics and hospitals that perform oncologic care) from all over the country, except for those located in the state of São Paulo, was obtained through the Hospital Cancer Registry (HCR) application, available on the website of the National Cancer Institute José Alencar Gomes da Silva (INCA) on the internet (https://irhc.inca.gov.br/RHCNet). The data from São Paulo units were obtained through the Fundação Oncocentro de São Paulo (FOSP) website (http://www.fosp.saude.sp.gov.br/publicacoes/acessobancodados). Access to electronic sites to obtain the data was performed on 21 January 2016.
The study population comprised cases of cervical cancer (code C53 of the 10th Revision the International Statistical Classification of Diseases and Related Health Problems [ICD-10]) registered by the HCR, with diagnosis between the years of 2000 and 2012, with histopathological confirmation, 18 years of age or older at the time of diagnosis, and with information about staging available.
Cases of invasive tumors with histopathological confirmation were considered eligible. All cases of in situ or intraepithelial neoplasms, as well as benign and non-invasive tumors, were excluded. Sarcomas, lymphomas and neuroendocrine tumors, were also excluded due to distinct occurrence, diagnosis, risk factors and treatment in comparison with the pathology object of this study.
Only cases classified by the RHC as analytical (i.e., cases for which the main treatment was performed in the institution responsible for the record) were included in the study. That selection was necessary because some cases might have been recorded by different institutions (once as analytical and again as non-analytical), and would thus be counted more than once.
Central tendency and spread measures for the interval in days between the date of diagnosis (date of the histopathological report) and the date of the beginning of the first specific treatment for the disease, were calculated, as well as for the interval between the date of the first consultation within the institution and the initiation of treatment. The percentage of cases for which the time from diagnosis to the start of the specific treatment exceeded 60 days was calculated.
Cases in which the patient’s place of birth differed from the state where the hospital care facility was located were also recorded. That procedure was designed to achieve an approximation to the hypothetical barrier-to access situation, in which patients have to travel to a location different from their place of residence to seek care.
The study variables included:
- Schooling (none; incomplete primary education; complete primary education; secondary education; college education);
- Region of health unit (Country macroregion in which the health institution that held the record is located);
- Region of birth (Country macroregion of birth of the person);
- Ethnicity/skin color (asian; white; indigenous; brown; black);
- Marital status (single; married; civil union; divorced; widow);
- Age (age ranges, the first being comprised of women aged less than 30 years old; the other categories were defined by ranges from 5 to 5 years until 70 years or more);
- Diagnosis and previous treatment (with diagnosis and treatment; with diagnosis, without treatment; without diagnosis, without treatment);
- Histological type (squamous tumours; adenocarcinomas; others, including tumors that do not fit none of the above categories);
- Treatment accomplishment (yes; no);
- Family history of cancer (presence; absence);
- Smoking (never smoker; former smoker; current smoker);
- Alcoholism (never user; former user; current user).9
According to the classification of the International Federation of Gynecology and Obstetrics (FIGO) for staging,10 cervical cancer stage I is restricted to the uterus. The tumors in stage II are those that spread beyond the cervix without, however, reaching the pelvic wall or the lower third of the vagina. Stage III tumors are those that affect the pelvic wall, the lower third of the vagina, or that cause ureteral obstruction. Stage IV tumors invade the mucosa of the rectum or bladder or extend beyond the true pelvis. The cases were classified according to the stage at the time of diagnosis. In group 1 (initial disease), were included those at stage I; in group 2 (localized disease), those at stage II; and in group 3 (advanced disease), those at stages III and IV.
Time trends for cervical cancer stage over the observation period were studied using a joinpoint regression model, with stage as the outcome (expressed as a percentage of cases at stages III and IV) and year of diagnosis as the independent variable. In order to fit the model, joinpoints (tendencies indicated by straight line segments) from 0-3 were admitted, and annual percentage changes (APCs) were estimated, with 95% confidence intervals (95%CIs).11 The Joinpoint application version 4.2.02 (2015) was used in the analysis of temporal trend.
The factors associated with cervical cancer stage at diagnosis were examined using a multinomial logistic regression model for stage, which was divided into three categories: the cases classified as localized disease and advanced disease were compared with those classified as initial disease (reference). Initially, univariate analysis was conducted by means of multinomial logistic regression model and the Wald test. All variables with less than 35% of records with missing information and which in this first analyses showed a p value equal or smaller than 0.2012 were included in the multivariate model.
In order tho analyze the influence of smoking, alcohol use, marital status, ethnicity/skin color and family history of cancer in the stage at diagnosis, we performed a second analysis using the same methodology, but excluding the cases from the units located in São Paulo state, once the information related to these variables were not available in the dataset obtained from FOSP.
The analyzes were performed using the application R version 3.0.3 of 2014; the coefficients of the regression models were extracted using the package Texreg.13 All Spreadsheets were edited using the Apache OpenOffice 4.1.1 application of 2014.
The study was approved by the Committee for Ethics in Research (CEP) of the Institute of Social Medicine of the State University of Rio de Janeiro - UERJ, according to resolution of the National Health Council (CNS) No. 196, October 10, 1996, upon presentation certificate for consideration Ethics (CAAE) No. 50685115.9.0000.5260, October 28, 2015.
Results
In total, 65,843 women met the criteria for inclusion in the study. The median age at diagnosis was 52 years (18 to 111 years), 17% were illiterate and 36% had incomplete primary education. There was no information about schooling for 26% of the cases (Table 1).
Table 1 - Sociodemographic characteristics of the studied patients diagnosed with cervical cancer according to the Hospital Cancer Registries, Brazil, 2000-2012
| Sociodemographic characteristics | N | % |
|---|---|---|
| Education level | ||
| None | 11,156 | 16.94 |
| Incomplete primary education school | 23,728 | 36.04 |
| Complete primary education school | 8,075 | 12.26 |
| Secondary education | 4,706 | 7.15 |
| College education | 1,053 | 1.60 |
| No information | 17,125 | 26.01 |
| Region of hospital unit | ||
| Midwest | 1,243 | 1.89 |
| Northeast | 20,547 | 31.21 |
| North | 6,371 | 9.68 |
| Southeast | 30,215 | 45.89 |
| South | 7,467 | 11.34 |
| Region of birth | ||
| Midwest | 1,265 | 2.01 |
| Northeast | 26,335 | 41.86 |
| North | 5,617 | 8.93 |
| Southeast | 22,579 | 35.89 |
| South | 6,952 | 11.05 |
| Foreign | 160 | 0.25 |
| Region of birth differs from the federation unit of the hospital unit | ||
| No | 46,058 | 69.95 |
| Yes | 16,690 | 25.35 |
| No information | 3,095 | 4.70 |
| Smoking | ||
| Former smoker | 1,401 | 2.86 |
| Never | 18,815 | 38.35 |
| Yes | 11,261 | 22.95 |
| No information | 17,583 | 35.84 |
| Alcoholism | ||
| Former user | 537 | 1.09 |
| Never | 23,256 | 47.40 |
| Yes | 3,792 | 7.73 |
| No information | 21,475 | 43.77 |
| Marital status | ||
| Single | 12,875 | 26.24 |
| Married | 22,155 | 45.16 |
| Civil union | 359 | 0.73 |
| Divorced | 2,762 | 6.04 |
| Widow | 2,762 | 5.63 |
| No information | 3,357 | 6.84 |
| Ethnicity/skin color | ||
| Asian | 460 | 0.94 |
| White | 15,972 | 32.56 |
| Indigenous | 143 | 0.29 |
| Brown | 24,947 | 50.85 |
| Black | 2,947 | 6.01 |
| No information | 4,591 | 9.36 |
The time between the date of diagnosis and the begining of treatment ranged from 0 to 180 days (median of 59 days). The interval between the first consultation and the initiation of treatment ranged from 0 to 182 days (median of 36 days). In 49.20% of cases, the time between diagnosis and initiation of treatment exceeded 60 days (Table 2).
Table 2 - Clinical features and characteristics related to the diagnosis and treatment of women diagnosed with cervical cancer who fulfilled the criteria for inclusion in the study, according to Hospital Cancer Registries, Brazil, 2000-2012
| Clinical characteristics and related to diagnosis and treatment | N | % |
|---|---|---|
| Treatment in the institution | ||
| Completed treatment | 55,155 | 83.77 |
| Not completed treatment | 3,800 | 5.77 |
| No information | 6,888 | 10.46 |
| Status of the disease at the end of the treatment | ||
| Without evidence of the disease | 11,390 | 30.0 |
| Partial Remission | 1,673 | 2.54 |
| Stable Disease | 12,156 | 18.46 |
| Disease progression | 3,193 | 4.85 |
| Outside therapeutic possibilities | 618 | 0.94 |
| Death | 6,183 | 9.39 |
| Not applicable | 2,778 | 4.22 |
| No information | 27,852 | 30.0 |
| Family history of cancer | ||
| No | 17,497 | 35.66 |
| Yes | 9,846 | 20.07 |
| No information | 21,717 | 44.27 |
| Prior diagnosis and treatment | ||
| With diagnosis and treatment | 6,492 | 9.86 |
| With diagnosis, without treatment | 39,064 | 59.33 |
| Without diagnosis | 18,939 | 28.76 |
| Without treatment | 25,431 | 38.62 |
| Histological type | ||
| Adenocarcinoma | 7,651 | 11.62 |
| Squamous | 54,351 | 82.55 |
| Adenosquamous | 803 | 1.22 |
| Invasive cancer, without specification | 3,038 | 4.61 |
| Stage at diagnosis | ||
| I | 14,024 | 30.0 |
| II | 21,293 | 32.34 |
| III | 25,782 | 39.16 |
| IV | 4,744 | 7.21 |
Women from 45 to 49 years accounted for 13.05% of the cases. The Southeast region originated 45.90% of the cases included followed by the Northeast (31.20%), South (11.34%), North (9.70%) and Midwest regions (1.89%). For 25% of women, the treatment was performed in a state different from that of birth.
The percentage of women who completed specific treatment was 77%, of whom 30% were without evidence of the disease at the end of it. The variable 'condition of the disease at the end of the treatment' contained 30% of observations without information. The majority of women (9.19%) arrived at the institution of reference with stablished diagnosis and only 9.86% had already received some type of specific treatment. The characteristics of the women studied are shown in Tables 1 and 2.
The percentage of cases in stages III and IV increased significantly from 2000 (46.80%) to 2012 (53.53%): annual percentage variation of 1.10; 95%CI 0.80;1.50 (Figure 1).
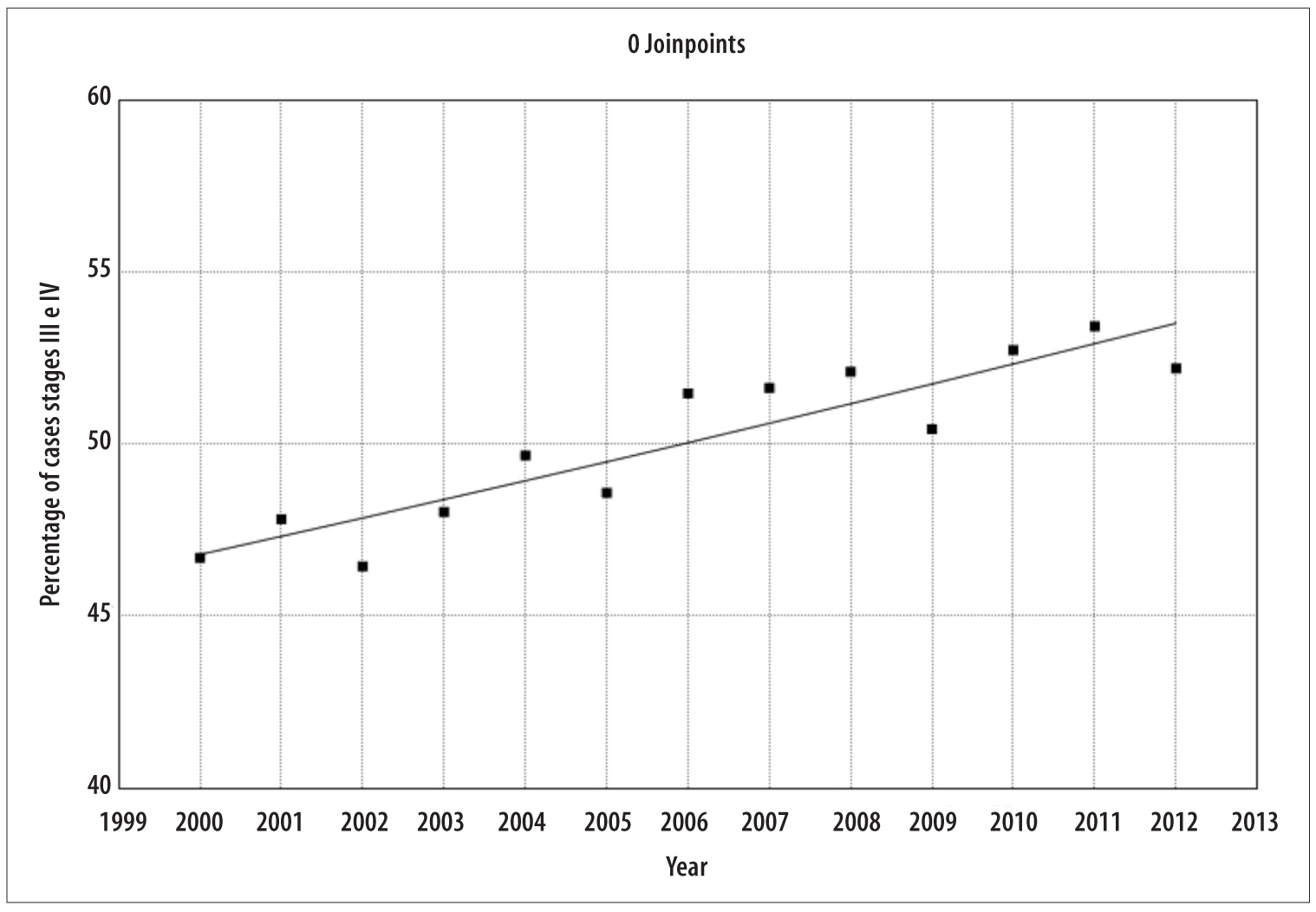
Figure 1 - Temporal trend of the percentage of cases of women diagnosed with cervical cancer in stages III and IV, in the studied population, according to the Hospital Cancer Registries, Brazil, 2000-2012
The multivariate logistic regression model was composed of all the variables included in the univariate analysis. The odds of having diagnosis of the disease in localized and advanced categories increased with age. This difference became statistically significant in the 40 to 44 years group, both for localized disease (OR=1.27 95%CI 1.09;1.47), as well as for advanced disease (OR=1.15 95%CI 1.00;1.32) (Table 3). When compared to women aged 30 years or younger, women from 65 to 69 years had higher odds of presenting localized (OR= 2.40; 95%CI 2.04;2.82) and advanced disease (OR=2.09 95%CI 1.79;2.44). Women with college education showed lower odds of developing localized disease (OR=0.65 95%CI 0.54; 0.77), as well as to develop advanced disease (OR= 0.45; 95%CI 0.39;0.53). Compared to women in the Southeastern region, women from other regions showed a greater chance of developing localized disease and advanced disease at diagnosis (Table 3).
Table 3 - Association between sociodemographic and clinical characteristics of the studied patients and the odds of being diagnosed with localized and advanced cervical cancer, Brazil, 2000-2012
| Demographic and clinical characteristics | Localized disease | Advanced disease | ||
|---|---|---|---|---|
| Crude analysis ORa (95%CIb) | Adjusted analysis ORa (95%CIb) | Crude analysis ORa (95%CIb) | Adjusted analysis ORa (95%CIb) | |
| Age (in years) | ||||
| <30 | 1.00 | 1.00 | 1.00 | 1.00 |
| 30-34 | 1.06 (0.93;1.22) | 1.01 (0.86;1.18) | 0.94 (0.83;1.06) | 0.90 (0.78;1.05) |
| 35-39 | 1.15 (1.01;1.31) | 1.11 (0.96;1.30) | 1.01 (0.89;1.13) | 0.98 (0.85;1.13) |
| 40-44 | 1.33 (1.18;1.51) | 1.27 (1.09;1.47) | 1.21 (1.08;1.36) | 1.15 (1.00;1.32) |
| 45-49 | 1.44 (1.27;1.63) | 1.46 (1.26;1.69) | 1.51 (1.35;2.70) | 1.51 (1.32;1.73) |
| 50-54 | 1.81 (1.59;2.05) | 1.80 (1.55;2.09) | 1.96 (1.74;2.20) | 1.84 (1.60;2.12) |
| 55-59 | 2.00 (1.76;2.27) | 1.94 (1.66;2.25) | 2.05 (1.83;2.31) | 1.89 (1.64;2.18) |
| 60-64 | 2.11 (1.85;2.40) | 1.96 (1.68;2.29) | 2.14 (1.89;2.41) | 1.86 (1.61;2.15) |
| 65-69 | 2.35 (2.05;2.69) | 2.40 (2.04;2.82) | 2.23 (1.57;2.53) | 2.09 (1.79;2.44) |
| ≥70 | 2.46 (2.17;2.79) | 2.38 (2.05;2.78) | 2.72 (2.42;3.06) | 2.35 (2.04;2.71) |
| Education level | ||||
| None | 1.00 | 1.00 | 1.00 | 1.00 |
| Incomplete primary education school | 0.66 (0.62;0.71) | 0.86 (0.80;0.93) | 0.60 (0.56;0.64) | 0.73 (0.68;0.78) |
| Complete primary education school | 0.60 (0.56;0.66) | 0.88 (0.80;0.96) | 0.53 (0.49;0.58) | 0.69 (0.63;0.75) |
| Secondary education | 0.46 (0.34;0.40) | 0.76 (0.69;0.84) | 0.37 (0.34;0.40) | 0.53 (0.48;0.59) |
| College education | 0.37 (0.31;0.43) | 0.65 (0.54;0.77) | 0.31 (0.26;0.36) | 0.45 (0.39;0.53) |
| Region of the hospital | ||||
| Southeast | 1.00 | 1.00 | 1.00 | 1.00 |
| Midwest | 1.51 (1.09;1.78) | 1.63 (1.32;2.00) | 1.48 (1.27;1.73) | 1.29 (1.06;1.58) |
| Northeast | 2.13 (2.03;2.24) | 1.88 (1.77;2.00) | 1.67 (1.59;1.75) | 1.32 (1.25;1.40) |
| North | 2.31 (2.13;2.49) | 2.48 (2.28;2.71) | 1.55 (1.44;1.62) | 1.63 (1.50;1.78) |
| South | 1.46 (1.35;1.57) | 1.49 (1.35;1.65) | 1.74 (1.62;1.86) | 1.71 (1.55;1.87) |
| Place of birth | ||||
| Same state of the treatment | 1.00 | 1.00 | 1.00 | 1.00 |
| Different state of the treatment | 0.89 (0.85;0.93) | 0.98 (0.92;1.03) | 0.86 (0.82;0.90) | 0.91 (0.86;0.96) |
| Histological type | ||||
| Squamous tumours | 1.00 | 1.00 | 1.00 | 1.00 |
| Adenocarcinomas | 0.58 (0.54;0.61) | 0.63 (0.59;0.68) | 0.45 (0.43;0.48) | 0.48 (0.44;0.51) |
| Others | 0.79 (0.72;0.87) | 0.83 (0.74;0.94) | 1.08 (0.99;1.18) | 1.15 (1.03;1.29) |
| Year of diagnosis | ||||
| 2000-2005 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2006-2012 | 0.97 (0.93;1.01) | 1.03 (0.98;1.09) | 1.15 (1.11;1.20) | 1.26 (1.20;1.33) |
a) OR: Odds ratio: calculated by taking the initial category 'disease' as a reference.
b) 95%CI: confidence interval.
Women who were born in a state different from that of the treatment healht unit presented lower odds of developing advanced disease (OR=0.91 95%CI 0.86;0.96), with no significant difference for localized disease. Women with adenocarcinomas had smaller odds of presenting localized (OR=0.63 95%CI 0.59;0.68) and advanced disease (OR=0.48 95%CI 0.44;0.51) when compared to women with squamous tumors (Table 3).
In the second analysis, excluding the 8,968 cases from the São Paulo state, were added only the variables 'ethnicity/skin color' and 'civil status' because they met the criteria established for inclusion in the multiple analysis. The variables 'smoking', 'alcoholism' and 'family history of cancer' were not included because they had more than 35% of missing data. Brown women had lower odds of presenting localized disease (OR=0.91 95%CI 0.84;0.98) when compared to white women. Indigenous women had higher odds of diagnosis in advanced category (OR=2.38; 95%CI 1.06;5.33), as well as black women (OR=1.16; 95%CI 1.02;1.31), compared to white women.
Widows had higher odds of presenting both localized disease (OR=1.11; 95%CI 1.01;1.23) and advanced disease (OR=1.34; 95%CI 1.22;1.48) when compared to married women. Divorced (OR=1.29; 95%CI 1.13;1.46) and single women (OR=1.46; 95%CI 1.36;1.57) showed higher odds of being diagnosed with advanced disease when compared to married women (Table 4).
Table 4 - Association between sociodemographic and clinical characteristics (including ethnicity/skin color and marital status) of the studied patients and the odds being diagnosed with localized and advanced stages, Brazil, 2000-2012
| Demographic and clinical characteristics | Localized disease | Advanced disease | ||
|---|---|---|---|---|
| Crude analysis ORa (95%CIb) | Adjusted analysis ORa (95%CIb) | Crude analysis ORa (95%CIb) | Adjusted analysis ORa (95%CIb) | |
| Age (in years) | ||||
| <30 | 1.00 | 1.00 | 1.00 | 1.00 |
| 30-34 | 1.03 (0.88;1.20) | 1.04 (0.86;1.26) | 0.91 (0.78;1.06) | 0.99 (0.82;1.19) |
| 35-39 | 1.04 (0.90;1.21) | 1.06 (0.89;1.27) | 0.95 (0.82;1.09) | 1.02 (0.86;1.21) |
| 40-44 | 1.17 (1.01;1.35) | 1.18 (0.99;1.41) | 1.09 (0.95;1.26) | 1.15 (0.97;1.36) |
| 45-49 | 1.35 (1.17;1.57) | 1.47 (1.24;1.76) | 1.46 (1.28;1.68) | 1.65 (1.39;1.95) |
| 50-54 | 1.66 (1.43;1.93) | 1.77 (1.48;2.12) | 1.86 (1.62;2.14) | 1.99 (1.68;2.37) |
| 55-59 | 1.75 (1.50;2.03) | 1.84 (1.53;2.21) | 1.88 (1.63;2.16) | 2.04 (1.71;2.43) |
| 60-64 | 1.91 (1.64;2.23) | 1.87 (1.55;2.26) | 1.96 (1.69;2.27) | 1.89 (1.57;2.26) |
| 65-69 | 2.19 (1.87;2.57) | 2.32 (1.90;2.83) | 2.10 (1.80;2.44) | 2.21 (1.83;2.69) |
| ≥70 | 2.19 (1.88;2.54) | 2.16 (1.78;2.60) | 2.43 (2.10;2.80) | 2.24 (1.87;2.69) |
| Education level | ||||
| None | 1.00 | 1.00 | 1.00 | 1.00 |
| Incomplete primary education school | 0.66 (0.63;0.73) | 0.68 (0.76;0.90) | 0.60 (0.33;0.40) | 0.61 (0.65;0.77) |
| Complete primary education school | 0.64 (0.59;0.71) | 0.88 (0.79;0.98) | 0.55 (0.50;0.60) | 0.69 (0.63;0.77) |
| Secondary education | 0.47 (0.42;0.52) | 0.67 (0.59;0.76) | 0.36 (0.34;0.40) | 0.47 (0.42;0.53) |
| College education | 0.39 (0.32;0.48) | 0.57 (0.46;0.70) | 0.30 (0.25;0.36) | 0.38 (0.31;0.47) |
| Region of the hospital | ||||
| Southeast | 1 | 1 | 1 | 1 |
| Midwest | 1.21 (1.02;1.43) | 1.37 (1.10;1.71) | 1.32 (1.13;1.55) | 1.15 (0.93;1.42) |
| Northeast | 1.70 (1.60;1.81) | 1.64 (1.52;1.77) | 1.49 (1.41;1.58) | 1.26 (1.17;1.35) |
| North | 1.84 (1.69;2.00) | 3.41 (3.01;3.86) | 1.38 (1.27;1.50) | 2.55 (2.26;2.89) |
| South | 1.26 (1.07;1.26) | 1.42 (1.25;1.60) | 1.55 (1.44;1.67) | 1.93 (1.72;2.16) |
| Place of birth | ||||
| Same state of the treatment | 1.00 | 1.00 | 1.00 | 1.00 |
| Different state of the treatment | 0.99 (0.93;1.05) | 0.93 (0.86;0.99) | 0.86 (0.85;0.95) | 0.90 (0.83;0.95) |
| Histological type | ||||
| Squamous tumours | 1.00 | 1.00 | 1.00 | 1.00 |
| Adenocarcinomas | 0.62 (0.57;0.67) | 0.67 (0.61;0.74) | 0.46 (0.43;0.50) | 0.48 (0.44;0.52) |
| Others | 0.72 (0.64;0.82) | 0.74 (0.63;0.86) | 0.96 (0.86;1.08) | 0.97 (0.84;1.13) |
| Year of diagnosis | ||||
| 2000-2005 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2006-2012 | 0.99 (0.94;1.04) | 0.99 (0.92;1.05) | 1.22 (1.17;1.29) | 1.23 (1.16;1.31) |
| Ethnicity/skin color | ||||
| White | 1.00 | 1.00 | 1.00 | 1.00 |
| Asian | 1.05 (0.81;1.37) | 0.77 (0.57;1.03) | 1.00 (0.78;1.28) | 0.94 (0.78;1.28) |
| Indigenous | 1.49 (0.85;2.62) | 1.66 (0.72;3.81) | 2.08 (1.24;3.52) | 2.38 (1.06;5.33) |
| Brown | 1.24 (1.17;1.31) | 0.91 (0.84;0.98) | 1.13 (1.07;1.19) | 0.99 (0.92;1.07) |
| Black | 1.00 (0.89;1.12) | 0.90 (0.79;1.03) | 1.19 (1.07;1.32) | 1.16 (1.02;1.31) |
| Marital status | ||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 |
| Divorced | 0.92 (0.82;1.03) | 1.05 (0.92;1.20) | 1.16 (1.04;1.29) | 1.29 (1.13;1.46) |
| Single | 0.98 (0.92;1.04) | 1.06 (0.99;1.14) | 1.28 (1.20;1.35) | 1.46 (1.36;1.57) |
| Widow | 1.36 (1.26;1.47) | 1.11 (1.01;1.23) | 1.66 (1.57;1.79) | 1.34 (1.22;1.48) |
a) OR: Odds ratio: calculated by taking the initial category 'disease' as a reference.
b) 95%CI: confidence interval.
Discussion
The diagnosis of cancer of the cervix in Brazil occurred late in over half of the cases and women with lower socioeconomic level presented higher odds of being diagnosed in advanced stages. Indigenous and black women showed significant association with advanced staging at diagnosis, in comparison with white women. Women treated in the Southeast region showed significantly lower odds of having late diagnosis, in comparison with the other macro-regions of the country. After the diagnosis, the time for initiation of treatment was greater than 60 days for almost half of women.
The present study has limitations to highlight. The data were obtained from secondary basis, thus restricting the analysis to information provided by the HCR. In consequence, important issues related to the natural history of the disease could not be analyzed in a direct manner. The low completeness found in some variables precluded their inclusion in the analysis. The HCR gathers information of cases treated in the great majority of health units in the country, being present in 91% of the units accredited by the Brazilian National Health System (SUS), with increasing coverage in recent years.9,14
Considering the fact that the information of the HCR is subject to constant updating and given the possibility of underreporting in health units located in regions with fewer resources, it is worth pointing out that part of the effect found in time trends may be due to incomplete registration by some of the health units. It is possible to argue, however, that the sub-registry mostly comes from less affluent regions and would affect mainly the most advanced cases. Hence, the increase in the percentage of diagnoses in stages III and IV could be even greater than that reported in the present study if, among the unregistered cases, the majority were composed of women diagnosed at an advanced stage.
The total number of registered cases was small when compared to the estimated annual incidence of the disease, even taking into account the increasing coverage in recent years. This suggests that the system passes through constant updating, with a progressive increase of its coverage. In addition, the HCR mainly covers users of SUS, leaving out almost all of the population covered by the supplementary system. This fact could be translated into a selection bias if the distribution of the outcome among users of supplementary system were substantially different from that observed in the sample studied.
In the year 2012, the Federal Law nº 12,73215 established as a maximum period for initiation of treatment of cancer the limit of 60 days after diagnosis. Although the sample of the present study has revealed the median time between diagnosis and initiation of treatment below the recommended time by law, in almost half of cases the limit was exceeded. This may explain, in conjunction with other factors such as barriers to access to treatment and biological characteristics of the disease, the high percentage of women with persistent disease at the end of treatment. There is clear need for the adoption of measures capable of reducing barriers and ensuring timely treatment of diagnosed cases, guaranteeing that the benefits related to screening programs are available to an increasing number of women.
We observed an increase in the percentage of diagnoses in stages III and IV during the period between the years 2000 and 2012. This finding is important since it suggests that the oncological care policies have not been able to provide early diagnosis, and, possibly, better prognosis as well as reduction in the incidence of the disease through treatment of pre-invasive lesions.16 Symptomatic women not covered by screening, possibly lose opportunities for diagnosis during ineffective visits to primary and secondary care units, resulting in the arrival to the oncologic care already in an advanced stage of the disease. It was not possible to identify change in the trend that could raise hypotheses about the effects of the Decree no. 2.439/2005) of the Brazilian Ministry of Health.
The odds of developing localized disease and advanced disease at diagnosis grew in parallel with age, with uniform trend between age groups. There is controversy in the literature regarding the effect of age on staging of cervical cancer. Evidence suggests that lower adherence to screening,17 differences in the natural history of the disease (as a shorter pre-invasive period, for instance) and changes due to the senescence of the immune system may be related to higher risk of diagnosis in advanced stage among the elderly population.18
The staging of cervical cancer in the population studied showed independent association with schooling, even after adjusting for other factors that could act as confounders. A retrospective cohort study conducted in China,18 including 68 women, proposed a model that incorporates socioeconomic factors, (including education), and genetic characteristics of (typing human leukocyte antigen) as risk factors for the development of cervical cancer. A cross-sectional study with data from Cancer Hospital registries in Brazil, covering the period from 2000 to 2009, analyzed 37,638 cases of cervical cancer and concluded that the diagnosis of cervical cancer in the country is done late in a significant proportion of women, in addition to reporting an association between low educational level and advanced staging.19
The relationship between low schooling and barriers to access to cervical cancer screening has already been pointed out previously. Cross-sectional survey, including 1,214 women in Belo Horizonte, MG,20 carried out in the year 2008, observed that low schooling, among other factors, has been associated with non-adherence to screening. Pointing out that, women with lower educational level would be exposed to higher risk of late diagnosis, in line with the results found.
Analysis of mortality from cervical cancer using data from the Mortality Information System in Brazil,21 from 1980 to 2010, shows a trend of increasing mortality rates for cervical cancer in cities outside of the capitals of the North and Northeast regions, in contrast with those found for the other regions of the country. The results of this study reveal also increased mortality from breast cancer in the same regions, contrary to the trend of reduction of mortality observed in the southern and southeastern regions in the same period. These findings are in agreement with the observed in the present study, except for the fact that the women treated in the South region had greater chance of diagnosis in advanced stage, in comparison with the women of the Southeast region. This difference may be related to the search for care by women coming from regions with greater difficulties of access to health services.22
Women with histopathological diagnosis of adenocarcinoma presented lower odds of being diagnosed in more advanced stages than those with squamous tumours. This finding contradicts current notion in the literature, according to which, due to the fact that adenocarcinomas originate more often in the endocervical canal, they would be diagnosed later than the adenocarcinomas.23
The results of this study are consistent with those of work carried out in the United Kingdom, in which 382 women cervical cancer cases diagnosed between 1985 and 1996 were included. The findings showed that women with adenocarcinomas tended to be diagnosed in initial stages more frequently when compared to women with epidermoid tumours. This histological type was also associated with a lower risk of presentation in advanced stage, according to a study based on secondary data about 51.842 women in Brazil, from 2000 to 2009.25 This could explain, at least partially, the fact that screening is, in general, less benefitial for women diagnosed with adenocarcinoma.26
Black and indigenous women, as well as single, divorced and widowed, had greater odds of developing both localized and advanced disease at diagnosis when compared to white women and married women, even after adjustment for the effect of age. This fact, in concordance with evidences found in the literature, indicates the importance of social barriers and family support for adequate attention to women's health.27-29 It is important to consider, however, the possibility of residual confounding in the effect of age over the odds advanced diagnosis: widows tend to be older than married women and, therefore, it is possible that part of the effect found is due to more advanced age.
The associations between the variables studied and the three categories of the outcome mantained the same direction. There were, however, differences in magnitude worthy of note. The effect of the region of the health unit on the chance of developing localized disease was higher than for advanced disease among women treated in all regions analyzed. An explanatory hypothesis for this association would be the application of screening, leading to higher probability of diagnosis in initial stages of the disease.30
As strengths of this work we highlight the large number of cases included representing all states of the country. The methodology used is also noteworthy: the multinomial regression model allowed grouping the staging in uniform categories, aggregating cases with similar prognosis and facilitating the interpretation of the results. These factors, in conjunction with the careful selection of cases that ensured the exclusion of non-invasive tumors, contributed to the accuracy of the results.
The findings point to an association between low socioeconomic level and advanced cervical cancer staging, especially among black, indigenous and low schooling women in Brazil. Specific analysis of the causal chain that guides these relationships, as well as the identication of possible confounding factors not considered in this analysis, would be of great value in the orientation of public health policies, necessary and urgent, aiming to reduce these disparities.
Acknowledgments
Marise Rebelo MD., PhD., for her help in obtaining and analyzing data. Gélcio Quintela Mendes MD.,PhD., and José Bines MD.,PhD., for their valious help during the production process. Andrea Negret MD., for her expert help in translations from the spanish language.
REFERENCES
1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015 Mar;136(5):E359-86. [ Links ]
2. Ministério da Saúde (BR). Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2016: incidência de câncer no Brasil [Internet]. 2016 [citado 2015 nov 13]. Disponível em: Disponível em: http://www.inca.gov.br/estimativa/2016/ . [ Links ]
3. International Agency for Research on Cancer. IARC handbooks of cancer prevention. Lyon: IARC Press; 2005. vol 10. [ Links ]
4. Nascimento MI, Silva GA. Effect of waiting time for radiotherapy on five-year overall survival in women with cervical cancer, 1995-2010. Cad Saúde Pública. 2015 Nov;31(11):2437-48. [ Links ]
5. Murillo R, Almonte M, Pereira A, Ferrer E, Gamboa OA, Jerónimo J, et al. Cervical cancer screening programs in Latin America and the Caribbean. Vaccine. 2008 Aug;26(Suppl 11):L37-48. [ Links ]
6. Brasil. Ministério da Saúde. Portaria GM no 2.439, de 08 de dezembro de 2005. Institui a Política Nacional de Atenção Oncológica: promoção, prevenção, diagnóstico, tratamento, reabilitação e cuidados paliativos, a ser implantada em todas as unidades federadas, respeitadas as competências das três esferas de gestão. Diário Oficial da República Federativa do Brasil, Brasília (DF), 2005 dez 9; Seção 1:80. [ Links ]
7. Medeiros GC, Bergmann A, Aguiar SS, Thuler LCS. Análise dos determinantes que influenciam o tempo para o início do tratamento de mulheres com câncer de mama no Brasil. Cad Saúde Pública. 2015 jun;31(6):1269-82. [ Links ]
8. Thuler LCS, Bergmann A, Casado L. Perfil das pacientes com câncer do colo do útero no Brasil, 2000-2009: estudo de base secundária. Rev Bras Cancerol. 2012 jul-set;58(3):351-7. [ Links ]
9. Ministério da Saúde (BR). Instituto Nacional de Câncer. Registros hospitalares de câncer: planejamento e gestão [Internet]. 2 ed. Rio de Janeiro: Instituto Nacional de Câncer, 2010. 536 p. Disponível em: http://www1.inca.gov.br/inca/Arquivos/INCA2009015_livro_registros_MIOLO.pdf. [ Links ]
10. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009 May;105(2):103-4. [ Links ]
11. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000 Feb;19(3):335-51. [ Links ]
12. Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993 Dec;138(11):923-36. [ Links ]
13. Leifeld P. Conversion of statistical model output in R to LATEX and HTML Tables. J Stat Softw. 2013 Nov;55(8):1-24. [ Links ]
14. Ministério da Saúde (BR). Instituto Nacional de Câncer José Alencar Gomes da Silva. Informação dos registros hospitalares de câncer como estratégia de transformação: perfil do Instituto Nacional de Câncer José Alencar Gomes da Silva em 25 anos [Internet]. Rio de Janeiro: Instituto Nacional de Câncer José Alencar Gomes da Silva; 2012 [citado 2015 maio 3] 100 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/inca/Informacao_dos_registros_hospitalares.pdf [ Links ]
15. Brasil. Presidência da República. Casa Civil. Subchefia para Assuntos Jurídicos. Lei no 12.732, de 22 de novembro de 2012. Dispõe sobre o primeiro tratamento de paciente com neoplasia maligna comprovada e estabelece prazo para seu início. Diário Oficial da República Federativa de Brasília (DF), 2012 nov 23; Seção 1;1. [ Links ]
16. Vargas-Hernández VM, Vargas-Aguilar VM, Tovar-Rodríguez JM. Primary cervical cancer screening. Fetección primaria del cancer cervicouterino. Cir Cir (English Edition). 2015 Sep;83(5):448-53. [ Links ]
17. Sawaya GF, Sung HY, Kearney KA, Miller M, Kinney W, Hiatt RA, et al. Advancing age and cervical cancer screening and prognosis. J Am Geriatr Soc. 2001 Nov;49(11):1499-504. [ Links ]
18. Hu B, Tao N, Zeng F, Zhao M, Qiu L, Chen W, et al. A risk evaluation model of cervical cancer based on etiology and human leukocyte antigen allele susceptibility. Int J Infect Dis. 2014 Nov;28:8-12. [ Links ]
19. Thuler LCS, Aguiar SS, Bergmann A. Determinantes do diagnóstico em estadio avançado do câncer do colo do útero no Brasil. Rev Bras Ginecol Obstet.2014 Jun;36(6):237-43. [ Links ]
20. Lage AC, Pessoa MC, Meléndez JGV. Fatores associados à não realização do Teste de Papanicolaou em Belo Horizonte, Minas Gerais, 2008. REME Rev Min Enferm. 2013 jul-set;17(3):565-70. [ Links ]
21. Girianelli VR, Gamarra CJ, Silva GA. Disparities in cervical and breast câncer mortality in Brazil. Rev Saúde Pública. 2014 Jun;48(3):459-67. [ Links ]
22. Gonzaga CMR, Freitas-Junior R, Barbaresco AA, Martins E, Bernardes BT, Resende PM. Cervical câncer mortality trends in Brazil: 1980-2009. Cad Saúde Pública. 2013 Mar;29(3):599-608. [ Links ]
23. Noh JM, Park W, Kim YS, Kim JY, Kim HJ, Kim J, et al. Comparison of clinical outcomes of adenocarcinoma and adenosquamous carcinoma in uterine cervical cancer patients receiving surgical resection followed by radiotherapy: A multicenter retrospective study (KROG 13-10). Gynecol Oncol. 2014 Mar;132(3):618-23. [ Links ]
24. Herbert A, Singh N, Smith JA. Adenocarcinoma of the uterine cervix compared with squamous cell carcinoma: a 12-year study in Southampton and South-west Hampshire. Cytopathology. 2001 Feb;12(1):26-36. [ Links ]
25. Nogueira-Rodrigues A, Ferreira CG, Bergmann A, de Aguiar SS, Thuler LCS. Comparison of adenocarcinoma (ACA) and squamous cell carcinoma (SCC) of the uterine cervix in a sub-optimally screened cohort: a population-based epidemiologic study of 51,842 women in Brazil. Gynecol Oncol. 2014 Nov;135(2):292-6. [ Links ]
26. Zappa M, Visioli CB, Ciatto S, Iossa A, Paci E, Sasieni P. Lower protection of cytological screening for adenocarcinomas and shorter protection for younger women: the results of a case-control study in Florence. Br J Cancer. 2004 May;90(9):1784-6. [ Links ]
27. Bairros FS, Meneghel SN, Dias-da-Costa JS, Bassani DG, Menezes AMB, Gigante DP, et al. Racial inequalities in access to women’s health care in southern Brazil. Cad Saúde Pública. 2011 Dec;27(12):2364-72. [ Links ]
28. Ferrante JM, Gonzalez EC, Roetzheim RG, Pal N, Woodard L. Clinical and demographic predictors of late-stage cervical cancer. Arch Fam Med. 2000 May;9(5):439-45. [ Links ]
29. Schinkel JK, Zahm SH, Jatoi I, McGlynn KA, Gallagher C, Schairer C, et al. Racial/ethnic differences in breast cancer survival by inflammatory status and hormonal receptor status: an analysis of the surveillance, epidemiology, and end results data. Cancer Causes Control. 2014 Aug;25(8):959-68. [ Links ]
30. Sankaranarayanan R, Budukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bull World Health Organ. 2001 Jan;79(10):954-62. [ Links ]
This article is derived from the Master's thesis entitled 'Access to diagnosis and treatment of patients with breast cancer and cervical cancer in Brazil: an analysis of data from Cancer Hospital Registers', defended by Nelson Luiz Renna Junior to the Postgraduate Program in Collective Health of the Institute of Social Medicine of the State University of Rio de Janeiro (UERJ) in 2016.
Received: August 28, 2017; Accepted: November 30, 2017










 texto en
texto en 


