INTRODUCTION
It is estimated that approximately 13% of all cancer cases worldwide - excluding non-melanoma skin cancer - are related to infections.1 Among the infectious agents causing the disease, the human papillomavirus (HPV) stands out, with infections linked to several types of cancers, such as cervical cancer, anus, penis, vulva and oropharyngeal.2
Cervical cancer is the fourth most common cancer in women globally and the third in Brazil, with a high associated mortality rate.3 In 2020, over 600,000 cases of cervical cancer were estimated worldwide, with an incidence of 13.3 cases per 100,000 women and a mortality rate of 7.2 deaths per 100,000 women per year. The highest incidence is concentrated in populous countries such as Indonesia, India, Russia and Brazil.4
HPV vaccination is the primary means of preventing cervical cancer, with efficacy already demonstrated in several studies.5),(6 In Brazil, a large study showed a 56.8% reduction in the prevalence of HPV genotypes identified as HPV 6, 11, 16 and 18 among vaccinated women aged 16 to 25 years.7
Quadrivalent HPV vaccine, aimed at adolescents aged 9 to 14 years and immunocompromised people, regardless of age, has been offered by the National Immunization Program (Programa Nacional de Imunizações - PNI) since 2014, in Brazil. The quadrivalent vaccine provides protection against HPV types 16 and 18, which have high oncogenic potential; in addition to types 6 and 11, which pose low oncogenic risk, despite being the main cause of anogenital warts.8
Following the inclusion of the HPV vaccine in the Brazilian immunization schedule, additional strategies were implemented over time, aimed to achieve the national coverage target of 80%. Among these strategies are (i) the provision of the vaccine in school settings, (ii) the inclusion of male children and adolescents as the target population, with a gradual reduction of the minimum age to 9 years, and (iii) the inclusion of specific population groups, such as the immunocompromised individuals, who receive the vaccine in a three-dose schedule.8
However, little information is available about the impact of these actions on the temporal evolution of vaccination coverage in each Federative Unit, which makes it difficult to formulate specific strategies for each population and geographic region.8 Furthermore, studies show highly heterogeneous vaccination coverage in the country, with high dropout rates after the first dose and greater difficulty accessing some locations, including the state of Goiás.6),(7),(9
The objective of this study was to analyze the temporal trend of HPV vaccination coverage among the female population aged 10 to 14 years, living in the state of Goiás, Brazil, between 2014 and 2022.
METHODS
This was an ecological time series study conducted in Goiás state, Brazil. The state of Goiás, located in the Midwest region of the country, covers an area of 340,242.859 km² and had an estimated population of 7,056,495 inhabitants (2022), 50.9% of whom were female.10
The study participants were comprised of females, aged 10 to 14 years, living in Goiás state from 2014 to 2022. The study variables were: the number of second doses of the HPV vaccine administered each year between 2014 and 2022; and the number of females aged 10 to 14 years, living in Goiás in each year of the study.
The number of second doses administered/year in the study population was retrieved from the National Immunization Program Information System (Sistema de Informações do Programa Nacional de Imunizações - SI-PNI), linked to the Brazilian National Health System Information Technology Department (Departamento de Informática do Sistema Único de Saúde - DATASUS), using an online data tabulator and spreadsheet generator tool: TabNet - Health Care module. The target population was obtained from the population estimates of the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística - IBGE), filtering the data by location and year.11 The databases were accessed on February 20, 2023.
As for the calculation of the vaccination coverage rate, the methodology proposed by the Pan American Health Organization/World Health Organization (PAHO/WHO) was used: as numerator, the number of second doses administered in the target population, and as denominator, the size of the target population, multiplied by 100.12
Regarding trend analysis, the Prais-Winsten model, proposed by Antunes & Cardoso, was used, considering time as the independent variable; and the annual vaccination coverage rate transformed into a base-10 logarithmic function as the dependent variable.13 The annual percentage change (APC) was obtained using the formula:
[(vaccination coverage rate in the following year ÷ vaccination coverage rate in the previous year) - 1] × 100
The value of which can indicate an increasing, decreasing, or stationary trend in the time series.13
The Durbin-Watson test was applied to check for the presence of serial autocorrelation, with values close to two indicating the absence of serial autocorrelation. The data were tabulated and analyzed using Excel and Stata 17.0 software, respectively.
Taking into consideration its observational nature and the use of data in the public domain, this study did not require ethical review.14 The drafting of the article followed the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) and The Reporting of Studies Conducted Using Observational Routinely Collected Health Data (RECORD).15),(16
RESULTS
Between 2014 and 2022, a total 407,217 second doses of the quadrivalent HPV vaccine were administered to the female population aged between 10 and 14 years in the state of Goiás. The highest vaccination coverage rates were observed in 2015 and 2014, as shown in Table 1.
Table 1 Annual coverage rate of the quadrivalent HPVa vaccine among the female population aged 10 to 14, state of Goiás, Brazil, 2014-2022
| Year | Target population | Number of second doses administered | Coverage rate (%) |
|---|---|---|---|
| 2014 | 270,137 | 80,569 | 29.8 |
| 2015 | 269,899 | 80,902 | 30.0 |
| 2016 | 266,135 | 33,215 | 12.5 |
| 2017 | 262,407 | 44,172 | 16.8 |
| 2018 | 258,769 | 35,140 | 13.6 |
| 2019 | 255,268 | 31,486 | 12.3 |
| 2020 | 251,945 | 36,900 | 14.6 |
| 2021 | 248,854 | 32,239 | 13.0 |
| 2022 | 246,013 | 32,594 | 13.2 |
| Total | 2,329,427 | 407,217 | 17.3 |
a) HPV: Human papillomavirus.
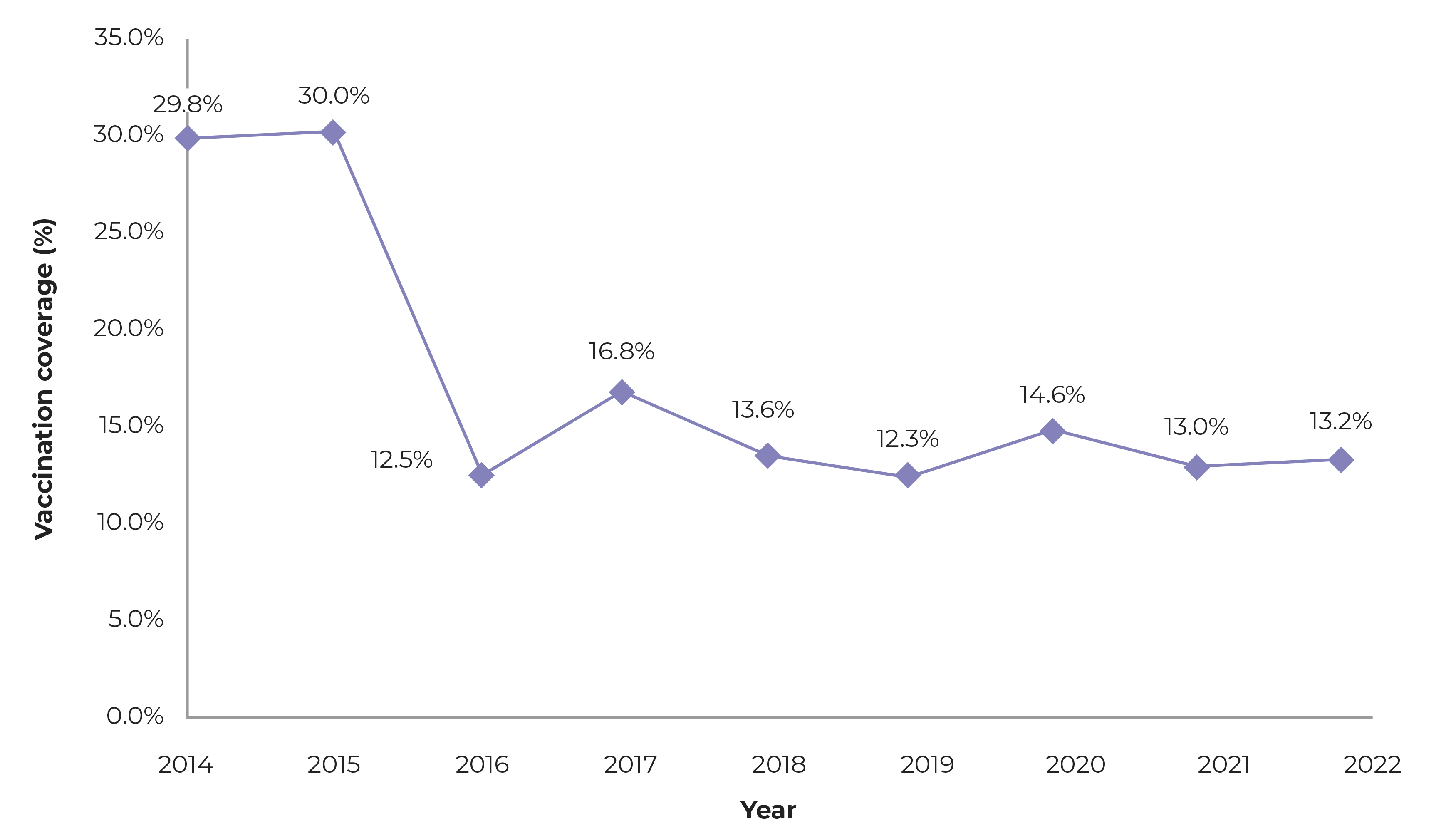
The annual vaccination coverage rate ranged from 12.3% in 2019 to 30.0% in 2015. The APC was 0.7% (95%CI 0.9; 0.2; p-value = 0.030), and the temporal trend was considered stationary (Figure 1).
a) HPV: Human papillomavirus.
Figure 1 The evolution of HPVa vaccine coverage rates among the female population aged 10 to 14, state of Goiás, Brazil, 2014-2022
The Durbin-Watson test showed a coefficient of 2.98, excluding the hypothesis of serial autocorrelation: there was no correlation between the current vaccination coverage rate and the vaccination coverage rate in previous years. Thus, it is assumed that the findings occurred randomly and independently.
DISCUSSION
This study showed low HPV vaccine coverage among female adolescents in the state of Goiás, with a stationary trend in the time series. This scenario is concerning and demands careful attention from local management, based on the target set by the WHO for the elimination of cervical cancer worldwide, aiming to achieve a vaccination coverage of 90% by 2030.17
Low HPV vaccination coverage is a global reality, especially in developing countries. There is a significant disparity in vaccination rates between developed and least developed countries, as well as variations in the quality of vaccination records.18 The estimated global HPV vaccination coverage in 2018 was only 12.2%.17 According to WHO estimates, the Region of the Americas showed the highest percentage of girls vaccinated by age 15, with vaccination coverage reaching 64% in 2021 and 66% in 2022; for the same periods, respectively, this coverage was 28% and 29%, in Europe, 18% and 19%, in Africa, and below 2% in Asia and the Middle East, reflecting a possible cultural determinant impacting the differences observed in the demand for and availability of the HPV vaccine, according to regions and continents.19
In Canada, HPV vaccination coverage in 2021 ranged from 57.1 to 91.3% depending on the region, while in the United States it remained around 76.9% in the same year.20),(21 In Latin American countries, however, vaccination coverage in 2020 ranged from 7% to 77% among female populations in the Dominican Republic and Costa Rica, respectively; in some countries in the region, such as Cuba, Venezuela, and Nicaragua, at the time this report was completed, there was no HPV vaccination plan among public immunization policies.22 In Brazil, vaccination coverage rates vary according to region, socioeconomic factors, and age group, although they remain below the national target of 80% in all regions of the country.9
In addition to the low adherence to HPV vaccination in Goiás, the results of this study show a decrease of over 50% in the rates of administration of the second dose of the HPV vaccine between 2015 and 2016, a period corresponding to the second year, post-introduction of the quadrivalent HPV vaccine into the Brazilian immunization schedule. From that point onwards, vaccination coverage maintains a stationary trend until the end of the time series evaluated. Corroborating these results, another Brazilian study showed a reduction of almost 30% in the number of doses of the HPV vaccine administered between 2014 and 2018, with an even sharper decline from 2015 onwards. In the Midwest region, for example, 596,777 doses were administered in 2014 and 176,935 in 2018, specifically in Goiás, this number dropped from 244,285 to 70,915 doses during the same period.23 This sharp decline after 2015 is possibly related to the cessation of the initial efforts for dissemination and expansion of supply, which were undertaken during the stage of the implementation of the vaccine into the recommended immunization schedule.23
Low adherence to the HPV vaccine is multifactorial. Studies demonstrate that income, race/skin color, education level, and geographic conditions can constitute barriers to the population access to the vaccine.9),(24),(25 Lack of knowledge, fear of adverse events, traditional beliefs and values, and the association of the vaccine with early sexual initiation can also lead to its refusal, both by adolescents and by their parents, resulting in low HPV vaccination coverage rates.26),(27 In this context, there is a need to expand access to the vaccine, especially in less-developed regions, in addition to the implementation of educational actions, communication campaigns, and specific policies aimed at increasing engagement and acceptance of vaccination. Dialogues with community and/or religious leaders can be effective strategies for achieving the immunization targets.
Another interesting aspect addressed in the literature is the difference in coverage between the first and second doses, indicating that a portion of the population initiates the HPV vaccination schedule but does not complete it. This phenomenon, known as vaccine dropout, has been reported more frequently in the child population, with regard to the essential vaccines in the schedule, and may be associated with a drop in immunobiological coverage of up to 40%.28),(29 Although evidence of this phenomenon in HPV vaccination is scarce, it is likely that the low vaccination coverage found is related to high rates of vaccination dropout, given that this analysis only took into consideration adolescents who had received the second dose of the vaccine. Currently, the effectiveness of the one-dose HPV vaccine for the prevention of cervical cancer is being studied, a measure that could result in increased supply and greater population adherence.30
The data presented in this study are of great regional interest, given the scarcity of research on HPV vaccine coverage among the female population living in the state of Goiás. The stationary trend in coverage rates, observed for most of the time series, suggests a possible inefficiency in vaccination strategies, associated with low interest and knowledge of the population about the importance of the vaccine. It was expected that the COVID-19 pandemic would influence the vaccination trend in recent years, which was not confirmed.
This study has limitations related to the use of secondary data, due to the possibility of poor quality of records and consequent discrepancy in available information. In addition, no stratified analysis was conducted by age and municipalities, nor were possible vaccination patterns in males investigated. For further studies, it is suggested to investigate the local factors leading to the refusal or voluntary delay in HPV vaccination, as well as seasonal analyses during vaccination campaigns and their impact on the vaccination rates achieved.
It can be concluded that the coverage rate of the quadrivalent vaccine against the HPV in Goiás state was below the national target between 2014 and 2022, showing a stationary trend in this time series. As additional measures to address the issue, it is suggested that (i) the opportunity for “extramural” vaccination activities - in schools, churches and other places with a large concentration of adolescents - be provided, as well as (ii) the active search for those who are missing vaccinations, based on data concerning vaccination dropout after the first dose.











 texto em
texto em 


