Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2337-9622
Epidemiol. Serv. Saúde v.26 n.1 Brasília jan./mar. 2017
http://dx.doi.org/10.5123/s1679-49742017000100002
ORIGINAL ARTICLE
Guillain-Barré syndrome and other neurological manifestations possibly related to Zika virus infection in municipalities from Bahia, Brazil, 2015
1Ministério da Saúde, Programa de Treinamento em Epidemiologia Aplicada aos Serviços do Sistema Único de Saúde, Brasília-DF, Brasil
2Ministério da Saúde, Programa Nacional de Controle da Dengue, Brasília-DF, Brasil
3Secretaria de Estado da Saúde da Bahia, Salvador-BA, Brasil
Objective:
to describe the reported cases of Guillain-Barré Syndrome (GBS) and other neurological manifestations with a history of dengue, chikungunya or Zika virus infections, in the Metropolitan Region of Salvador and in the municipality of Feira de Santana, Brazil.
Methods:
this is a descriptive study with data of an investigation conducted by the epidemiological surveillance from March to August 2015; to confirm the neurological manifestations, medical diagnosis records were considered, and to prior infection, clinical and laboratory criteria were used.
Results:
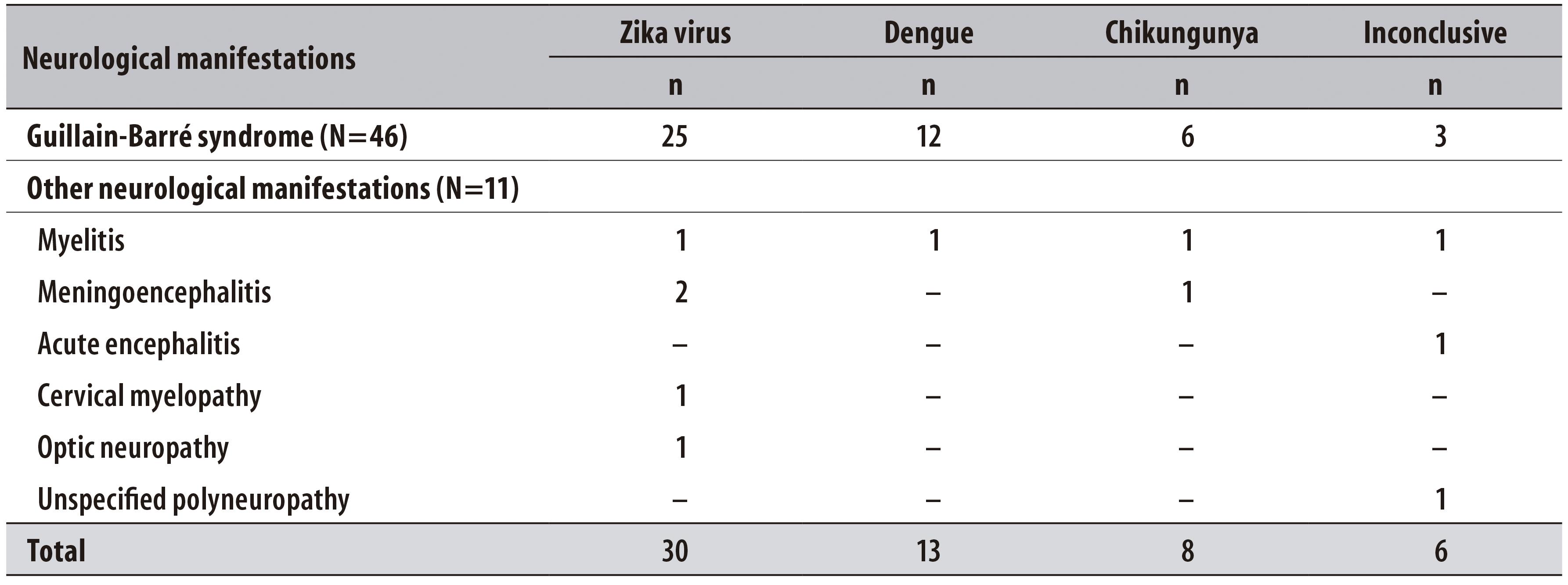
138 individuals were investigated, 57 reported infectious process up to 31 days before neurological symptoms - 30 possibly due to Zika, 13 to dengue, 8 to chikungunya and 6 were inconclusive -; GBS was the most frequent neurological condition (n=46), with predominance of male sex (n=32) and the median age was 44.
Conclusion:
most cases reported a clinical picture consistent with acute Zika virus disease, which preceded the occurrence of neurological symptoms.
Key words: Guillain-Barré Syndrome; Neurological Manifestations; Zika Virus; Epidemiology, Descriptive
Introduction
At least nine pathogenic arboviruses circulated in Brazil in 2015, and three of them with sustainable urban circulation stood out: dengue, chikungunya and Zika virus.1 Reemergence of dengue in Brazil has been observed since the mid-1980s, whereas chikungunya and Zika virus emergencies are more recent, and their autochthony was confirmed in 2014 and 2015, respectively.
Some reports confirm the relation between infection due to those arboviruses and problems in the central and peripheral nervous system. The increase in the number of encephalitis and meningoencephalitis in patients with dengue had been reported in Brazil during the 1997 and 2002 epidemics. Besides that, many studies from countries with dengue epidemics observed an association between this condition and other neurological manifestations, such as Guillain-Barré syndrome (GBS), peripheral neuropathy, peripheral facial paralysis, encephalitis and myelitis.2
In regions with chikungunya epidemics, some atypical conditions involving the nervous system were found, including myelopathy, encephalitis, GBS, flaccid paralysis and neuropathy.3
Zika virus infection has also been connected to the occurrence of neurological manifestations. In Micronesia, during an outbreak of Zika virus in 2007, 40 cases of GBS were diagnosed, which represented an incidence 20 times higher than the previous period: about five cases/year. A similar situation was identified in French Polynesia, in 2013, and, more recently, in Brazil, in 2015.4,5
GBS, a neurological manifestation frequently associated to those arboviruses, is a probable autoimmune neurological condition in which approximately 60% of cases can be attributed to recent infection process.6,7 It is the most frequent occurrence of flaccid paralysis in the world, with annual incidence from 0.81 to 1.89 per 100 thousand inhabitants, striking mainly the population aged between 20 and 40, of both sexes. Usually, most of cases occur sporadically and do not seem to present any seasonality, with a fatality rate varying between 5 and 15%.4,6,8
In 2015, the National Program for Dengue Control, of the Brazilian Ministry of Health, registered an increase in the number of hospitalizations due to GBS in the Brazilian National Health System (SUS). The state with the highest number of hospitalizations was Bahia, located in the Northeast region, where, from January to July 2015, there was a 66% increment in the number of hospitalization due to GBS, when comparing with the average of the same period, from 2008 to 2014.5 Moreover, the circulation of Zika virus in Brazil had been first confirmed in that state,9 where there is also concurrent circulation of dengue and chikungunya. Such epidemiological situation justified the conduction of a case investigation in municipalities from Bahia.
The objective of this study was to describe the reported cases of Guillain-Barré Syndrome (GBS) and other neurological manifestations with a history of dengue, chikungunya or Zika virus infections, in the Metropolitan Region of Salvador and in the municipality of Feira de Santana, Brazil.
Methods
This is a descriptive study of GBS cases and other neurological manifestations with history of prior infection with dengue, chikungunya or Zika virus, notified to the Center for Strategic Information on Health Surveillance of Bahia (CIEVS/BA), of the State Health Department of Bahia. All cases notified from March, 1st to August 31st 2015 and cases investigated in August and September 2015 of residents and hospitalized individuals in the Metropolitan Region of Salvador and in the municipality of Feira de Santana were included. The Metropolitan Region of Salvador, capital of Bahia State, is composed by the following municipalities: Camaçari, Candeias, Dias d’Ávila, Itaparica, Lauro de Freitas, Madre de Deus, Mata de São João, Pojuca, Salvador, São Francisco do Conde, São Sebastião do Passé, Simões Filho and Vera Cruz. In 2015, that region had 3,953,288 inhabitants.10 Feira de Santana, located 108km from the state capital, had 617,528 inhabitants in 2015.10
The data used in this study were collected through actions of surveillance and rapid response to this unexpected event. In this situation, for convenience, we opted for selecting municipalities close to Salvador that gathered the highest number of GBS cases and other neurological manifestations - object of notification, to widen the research.
The following case definitions were used:
a) Suspect - individuals notified to CIEVS/BA diagnosed with GBS or other neurological manifestations (encephalitis, meningoencephalitis, myelitis, optic neuropathy) from March to August 2015, hospitalized in public or private hospitals from the Metropolitan Region of Salvador or in the municipality of Feira de Santana.
b) Probable - suspect case with history of prior virus infection with an arbovirus (dengue, chikungunya Zika virus) up to 60 days before the beginning of neurological symptoms, without laboratory confirmation or virus isolation (or through cell culture or molecular biology), which met any of the following criteria:
- Zika virus - presence of maculopapular rash, in addition to two or more of the following signs or symptoms: fever, polyarthralgia, conjunctival hyperemia, joint swelling or pruritus.
- Dengue - presence of fever, in addition to one or more of the following signs and symptoms: nausea, vomit, rash, myalgia, headache, retro-orbital pain, petechiae and/or positive serology (presence of IgM).
- Chikungunya - presence of fever and arthralgia, not explained by other conditions and/or positive serology (presence of IgM).
c) Confirmed for arbovirus infection - suspect case with laboratory confirmation through virus isolation for dengue, chikungunya or Zika virus.
d) Discarded for arbovirus infection - suspect case of neurological manifestation with history of prior virus infection, confirmed for etiologic agent other than dengue, chikungunya or Zika virus.
d) Discarded for arbovirus infection - suspect case of neurological manifestation with history of prior virus infection, confirmed for etiologic agent other than dengue, chikungunya or Zika virus.
In order to confirm the neurological manifestations of suspect cases, we considered the register of the diagnose in the hospitalization medical records. The specific cases of GBS were evaluated: clinical symptoms and analysis of the cerebrospinal fluid (CSF), in which the albuminocytologic dissociation was observed, with an elevation of proteins, with no increase in the count of white blood cells, though.
A search for results of laboratory exams was conducted in Bahia SmartLab system and in the Laboratory Environment Manager, of the Ministry of Health, in order to confirm the suspect of prior virus infection; blood and cerebrospinal fluid (CSF) samples were obtained while they were still stored in the notifier hospitals. The samples obtained were analyzed at the State Central Laboratory (Lacen/BA) and at the Evandro Chagas Institute/Pará (IEC/PA), being tested for dengue, chikungunya and Zika virus. The serologic diagnose for dengue and chikungunya was performed through the enzyme-linked immunosorbent assay (MAC-ELISA); for detecting Zika virus in the CSF samples, the polymerase chain reaction (PCR) was adopted.
The selection of cases to be investigated was based on the spreadsheet of Sesab epidemiological surveillance, and all the suspect cases were included. Medical records of the notifier hospitals were consulted and interviews with the individuals were conducted through the use of a semi-structured questionnaire, especially designed for this investigation, covering the following variables: sociodemographic, epidemiological history, neurological manifestations, treatment and evolution, prior virus infection and laboratory exams. The interviews with suspect cases were conducted by telephone. The absence of telephone number or the impossibility of conducting the interview after four attempts, in alternate days and times were considered as losses.
The following variables were included in the interview:
- sex (male; female)
- age (in years);
- municipality of residence;
- date of initial symptoms of GBS or other neurological manifestations;
- date of initial symptoms of prior virus infection;
- diseases such as diabetes and hypertension (presence; absence);
- influenza vaccination in the previous immunization campaign (yes, no);
- history of surgery intervention in the 90 days prior to the date of initial symptoms (yes, no);
- history of pregnancy in the 90 days prior to the date of initial symptoms (yes, no);
- hospitalization (yes, no);
- hospitalization period (in days);
- administration of intravenous immunoglobulin (yes, no);
- case evolution (recovery and hospital discharge; referral; death; recurrence); and
- presence or absence of the following signs and symptoms: rash, fever, polyarthralgia, pruritus, myalgia, headache, joint swelling, retro-orbital pain, conjunctival hyperemia, nausea.
The data were analyzed using the programs Epi InfoTM 7.1.5.0 and QGIS 2.6.1. The probable cases of infection with arbovirus with diagnose of neurological manifestations were described using measures of frequency, central tendency and dispersion. In order to calculate the incidence of GBS and other neurological manifestations, we considered the number of cases in 2015 divided by the number of inhabitants10, multiplied by 100 thousand; then, to calculate the incidence rate for the outbreak period, we divided the annual incidence rate / (Number of the epidemiological week of the year - 52 / Number of epidemiological week when the outbreak occurred).
The distribution of the number of probable cases of dengue, chikungunya and Zika virus per epidemiological week was also presented, and they were obtained on the Information System for Notifiable Diseases (Sinan) and on FormSUS. Only the probable cases were considered in this study, and the discarded cases were excluded.
At the moment of the telephone interview, a Free Informed Term of Consent was read by the interviewer. After the term was read, the individual to be interviewed could agree or not in taking part of the study, through a verbal permission. The confidentiality of information was ensured, according to the Resolution of the National Health Council (CNS) No. 466, dated December 12th, 2012. The project was not submitted to the approval of an Ethics Research Committee, since this is a case investigation within epidemiological surveillance actions.
Results
A total of 138 medical records were revised, from 24 public and private hospitals, one health care center and one primary health care unit (PHU): 60 medical records (43.5%) met the definition for probable case, and three of them (2;2%) were considered losses. Among the suspect cases, the median of time between the virus infection and the neurological manifestations was of 10 days, with a range from 1 to 31 days.
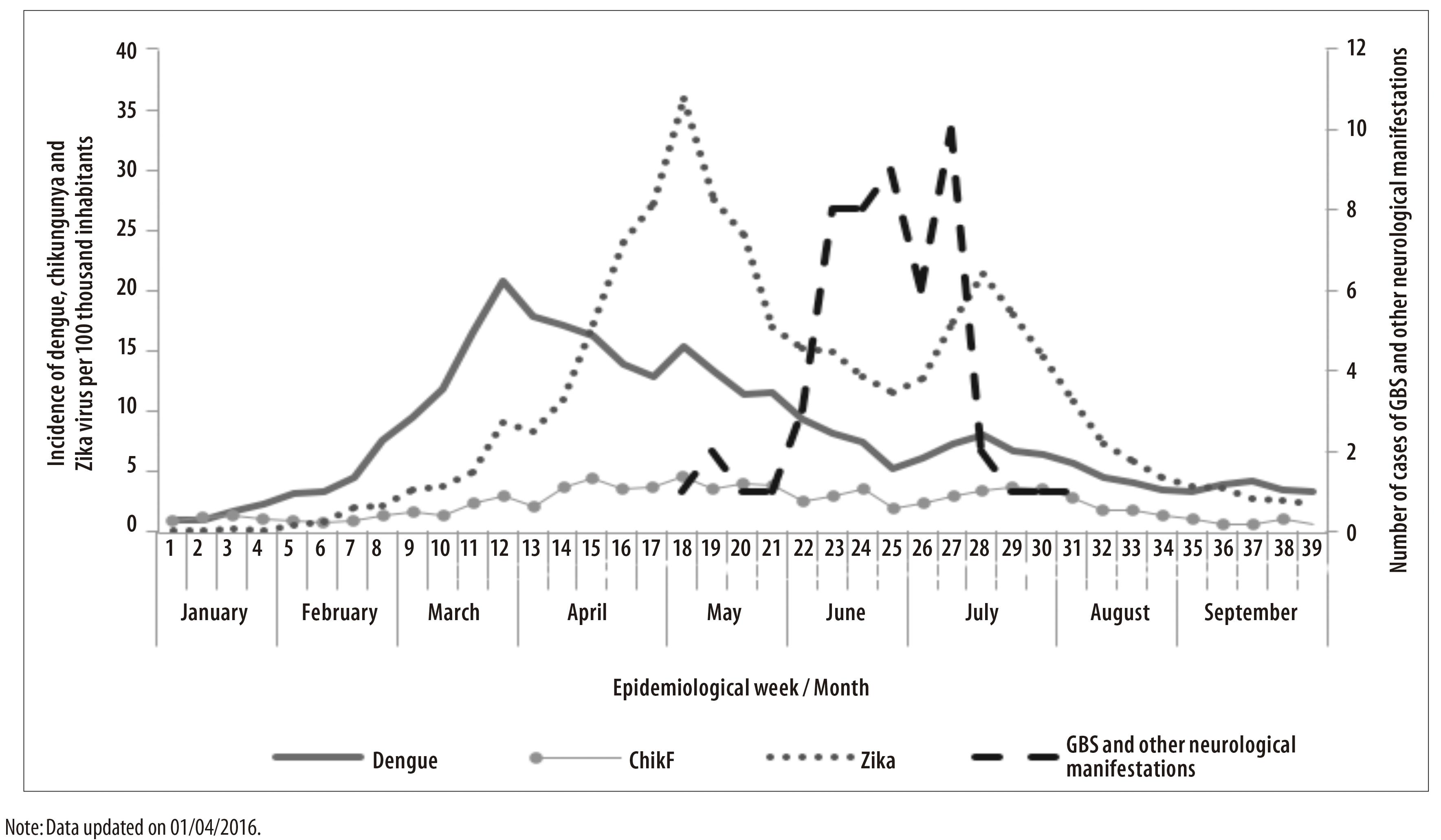
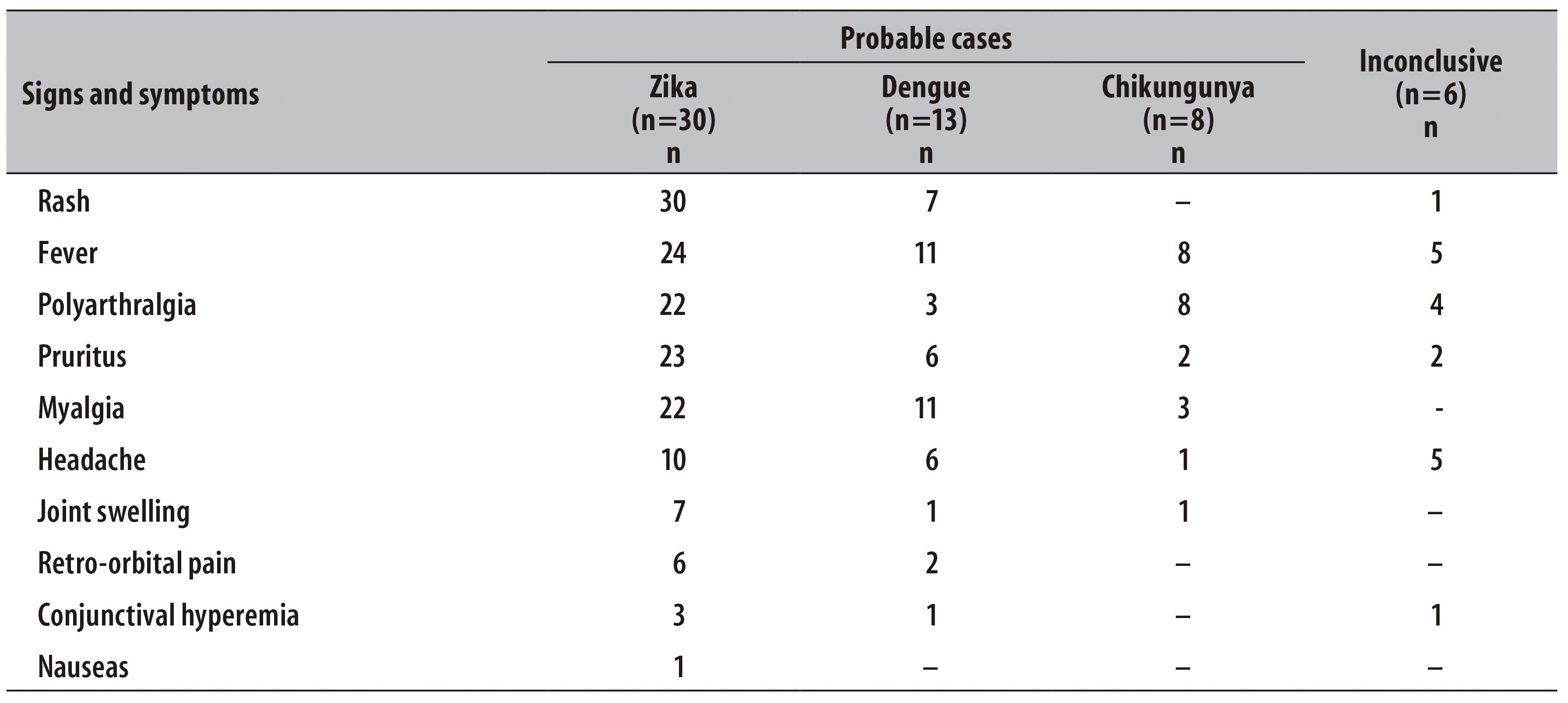
Of the 57 probable cases, the date of initial symptoms was mostly concentrated between the epidemiological weeks 15 and 31, with a peak on the 27th week, in July 2015 (Figure 1). Of these cases, 46 were diagnosed for GBS and 11 for other neurological manifestations. With regard to history of prior virus infection, 30 of them were classified as probable cases of infection with Zika virus, 13 with dengue, 8 with chikungunya and 6 were considered inconclusive (Table 1). Of the 21 cases tested for dengue, eight had serology IgM reagent.
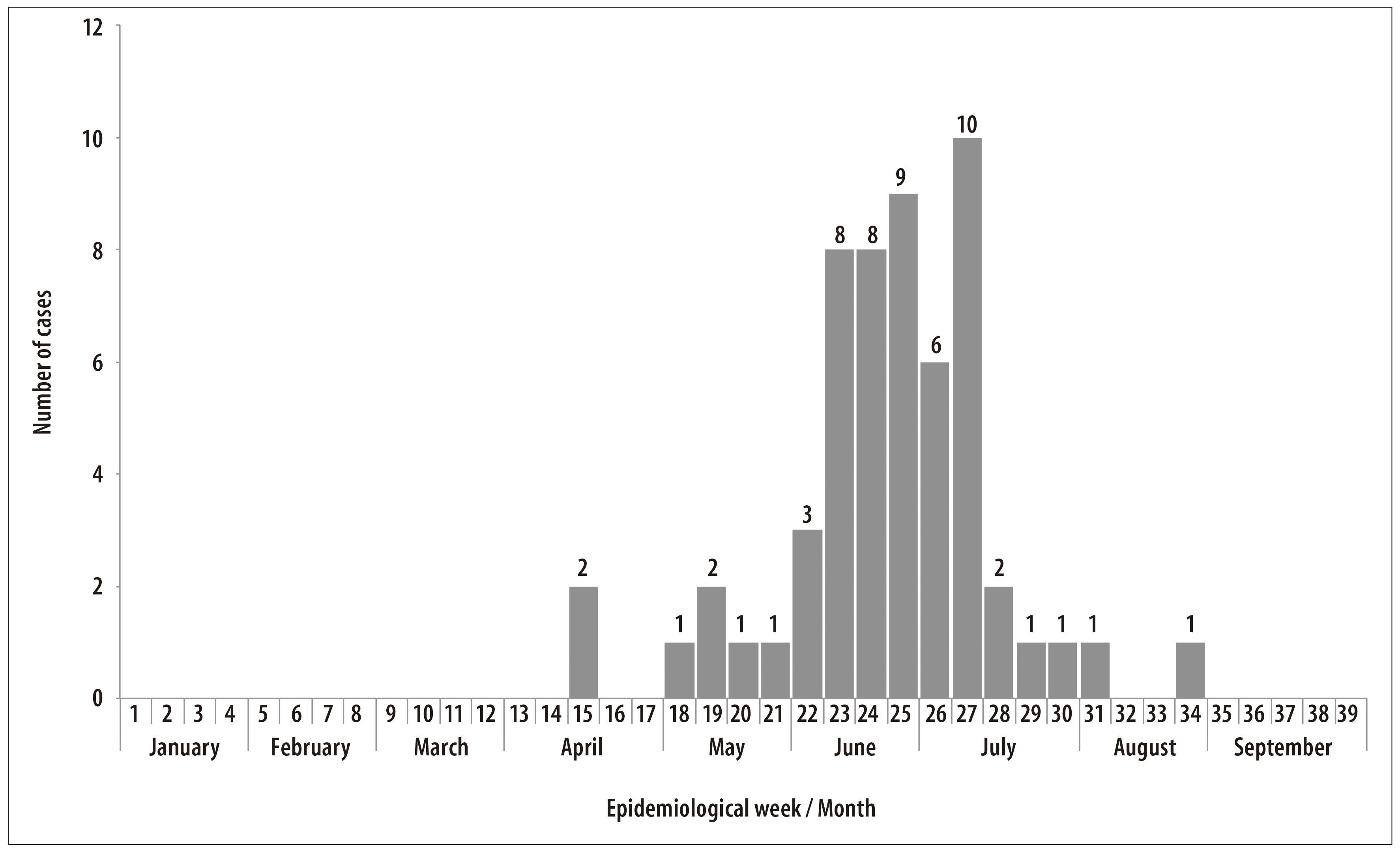
Figure 1 - Distribution of the frequency of cases of Guillain-Barré syndrome and other neurological manifestations with probable prior infection with Zika virus, dengue or chikungunya (n=57), according to the epidemiological week of initial symptoms, Bahia, January to September 2015
Table 1 - Distribution of the frequency of probable cases of arbovirus infection, according to the classification of neurological manifestations, Bahia, March to August 2015
Regarding demographic characteristics, 32/57 probable cases were males and the median of age was 44 years old (interquartile range of 1 and 3: 31-59 years - amplitude: 2-83 years). Most suspect cases were residents in the municipality of Salvador (n=35 cases), followed by Feira de Santana (n=4) (Figure 2).
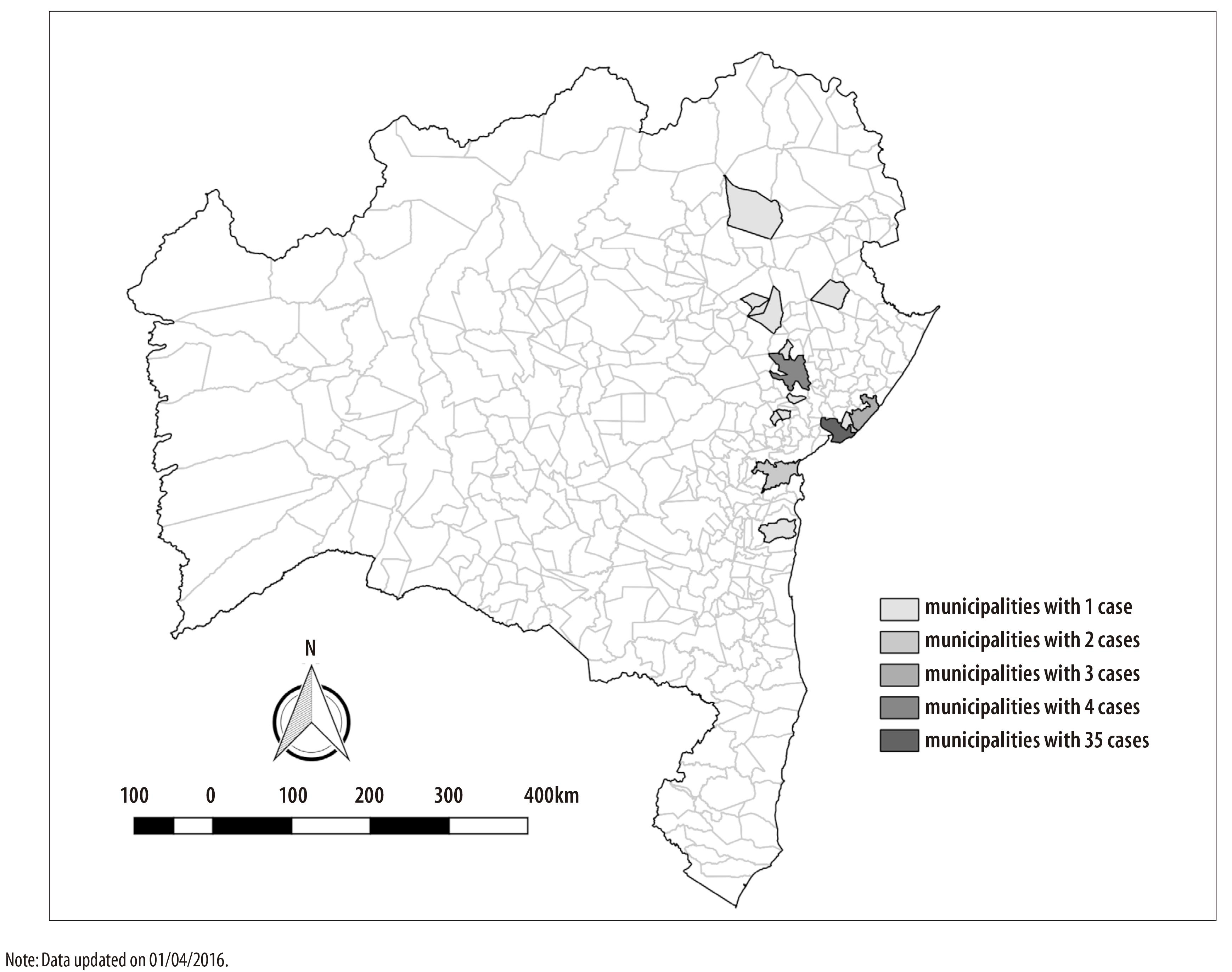
Figure 2 - Number of cases of Guillain-Barré syndrome and other neurological manifestations with probable prior infection with Zika virus, dengue or chikungunya, according to municipality of residence, Bahia, March to August 2015
Other exposures probably linked to neurological manifestations were also researched. With regard to the presence of associated diseases, 26 suspect cases reported having at least one disease - hypertension and diabetes were the most frequent; 13 cases had received influenza vaccine in the previous campaign, which took place from 4 to 22 May, 2015. There was no case with history of surgery intervention, and none of the women presented history of pregnancy in the 90 days prior to the date of initial symptoms.
All the 57 cases of GBS and other neurological manifestations were hospitalized and 20 of them were assisted in an Intensive Care Unit (ICU). The treatment with intravenous immunoglobulin was administered in 41/46 cases of GBS; the median of time between the beginning of neurological symptoms and the beginning of administration of intravenous immunoglobulin was of 8 days (interquartile range of 1 and 3: 6-14 days, amplitude: 1-45 days).
With regard to the evolution of cases of GBS and other neurological manifestations, 48 were discharged after recovery, and 6 were referred to other health facilities; 2 cases of GBS evolved to death: one case with history of prior virus infection with dengue and another one with Zika virus. One case of acute encephalitis, after clinical recovery, presented recurrence. The hospitalization period of suspect cases had a median of 11 days, varying from 1 to 73 days (median: 11 days).
Through laboratory search, 10 CSF samples of suspect cases were identified; however, due to the condition of the samples, only 6 were processed. The median of time between the prior virus infection and the CSF collection was of 20 days, varying from 12 to 30 days. These samples were stored for six months, until they were processed, and all of them presented negative results for Zika virus.
When the clinical picture before neurological manifestations was analyzed, most of the 30 cases of GBS or other neurological manifestations classified as probable infection with Zika virus presented rash, fever, polyarthralgia, pruritus and myalgia. Among the 13 cases of GBS and other neurological manifestations with probable infection with dengue, most of the individuals presented fever, myalgia, rash, pruritus and headache. With regard to the 8 cases of GBS and other neurological manifestations with probable infection with chikungunya, most of the individuals presented fever, polyarthralgia and myalgia. Among the 6 inconclusive cases for arbovirus infection, most of the individuals presented fever, headache and polyarthralgia (Table 2).
Table 2 - Distribution of the frequency of signs and symptoms occurrence among cases of Guillain-Barré syndrome and other neurological manifestations with probable prior infection with Zika virus, dengue or chikungunya, or inconclusive, Bahia, March to August 2015
During the period of epidemic outbreak, the general incidence of GBS and other neurological manifestations was of 4.4 cases per 100 thousand inhabitants in the studied population, and 4.2 per 100 thousand inhabitants residents in Salvador. The incidence of GBS and other neurological manifestations was of 5.0/100 inhabitants among men and 3.8/100 inhabitants among women.
The distribution of probable cases of dengue, chikungunya and Zika virus in Bahia State, according to the initial date of symptoms, shows a higher number of dengue notified on Epi week 12 and Zika virus on Epi week 18. The peak of cases notified of GBS and other neurological manifestations (between June and July, 2015) occurred after the first identification of Zika virus in Bahia and Brazil, after the period of higher transmission of dengue and Zika virus (between April and May, 2015) (Figure 3).
Discussion
The epidemiological investigation identified an outbreak of GBS and other neurological manifestations, with higher number of cases in June and July, after the introduction and rapid spread of Zika virus in Bahia, as well as the simultaneous circulation of dengue and chikungunya viruses. Most of the cases were males and aged less than 50.
The time range between the date initial symptoms of the prior virus infection and the neurologic picture observed in the present study (median: 10 days) corroborates with what is found on literature.11,12
There are records of neurological manifestations after infection processes with dengue and chikungunya since the 1960s.13 A study of 41 cases, conducted in a public hospital from Recife-PE, described 7 cases of neurological manifestations with history of dengue in the 1997 epidemics and 34 cases in 2002, among which some brain and peripheral nerves problems have been registered in both periods.2
There are reports of neurological complications after Zika virus infection since 2007, after outbreaks occurred in the regions of Micronesia and French Polynesia.14 In Bahia, an increase in the number of dengue cases was identified in the epidemiological week 12; after this period, no cases of neurological manifestations with prior virus infection were recorded, taking into consideration the maximum range since the date of initial symptoms of the acute infection and the neurological manifestations: 31 days. The increase in the notification of cases of GBS and other neurological manifestations with history of prior virus infection was observed after the first identification of Zika virus, confirmed in Brazil on April 29th 2015, in the Metropolitan Region of Salvador.15 It seems that the reduction in the number of notified cases due to the triple epidemics - dengue, chikungunya and Zika - was followed by a reduction in the number of cases of GBS and other neurological manifestations.
Half of the cases of neurological manifestations that were diagnosed for dengue by laboratory criteria, IgM reagent, did not meet the definition of dengue case. However, two cases did not present fever and other two presented other symptoms suggesting Zika virus; these cases may be false-positive for dengue, once the serology for dengue is characterized by the low diagnose specificity, which may present crossed reaction with other flavivirus.16
A study conducted in a university hospital in Rio de Janeiro State, from December 2015 to March 2016, identified 20 cases of GBS, 17 of them with history of virus disease with clinical picture consistent with Zika virus.17
According to a study conducted in French Polynesia with 42 patients who presented clinical picture of GBS and most with history of an exanthematous syndrome, 41 of them (98%) presented IgM or IgG markers and neutralizing antibodies against Zika virus.18
There is also the possibility of a co-detection among the arboviruses during the prior acute disease, based on a case report of GBS in which Zika and CHIKV (chikungunya virus) were detected in the serum and cerebrospinal fluid.19
From the epidemiological point of view, the event of neurological manifestations with history of virus infection is already expected, due to the rapid spread of the Zika virus in the country. However, the etiology for this increase in the number of cases remains under investigation.
Among the study's limitations we must mention the lack of information of the laboratory component that did not allow the confirmation of the infection and the identification of the etiologic agent for all the cases, mainly due to the lack of opportunity of collecting samples following the initial symptoms of prior virus infection. A possible recall bias from the interviewed individuals should be considered, because of the time span between the prior virus infection and the moment the interview was conducted. The telephone interviews did not present any interference: the individuals seemed attentive and available to answer to the questions.
We suggest the conduction of prospective studies, aiming the opportunity of collection and case confirmation, samples viability and collection for virus diagnose in cases of neurological manifestations with history of prior virus infection in the hospitals, and the conduction of an analytic study to identify and establish the possible relation and factors associated to the development of GBS and other neurological manifestations and Zika virus infection.
This is a pioneer study in Brazil, dedicated to document the highest number of cases that developed Guillain-Barré syndrome and other neurological manifestations after prior virus infection possibly caused by Zika, dengue or chikungunya viruses. Most of individuals reported clinical picture consistent with acute disease by Zika virus that preceded the occurrence of neurological symptoms. This epidemiological scenario coincided with the increase in the number of dengue cases, the introduction and rapid spread of Zika virus and increase of chikungunya cases in Bahia State. In view of this result, states and municipalities should be qualified to timely notify and investigate suspect cases of neurological manifestations, possibly related to arboviruses, adopting the adequate clinical management, and providing intensive care beds for better tackling these diseases and conditions.
Referências
1. Figueiredo LTM. The recent arbovirus disease epidemic in Brazil. Rev Soc Bras Med Trop. 2015 May-Jun;48(3):233-4. [ Links ]
2. Ferreira MLB, Cavalcanti CG, Coelho CA, Mesquita SD. Manifestações neurológicas de dengue: estudo de 41 casos. Arq Neuro-Psiquiatr. 2005 jun;63(2B):488-93. [ Links ]
3. Azevedo RSS, Oliveira CS, Vasconcelos PFC. Chikungunya risk for Brazil. Rev Saude Publica. 2015 Sep;49:58. [ Links ]
4. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância das doenças transmissíveis. Protocolo de vigilância e resposta à ocorrência de microcefalia e/ou alterações do sistema nervoso central (SNC) [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2016 set 12]. Disponível em: Disponível em: http://combateaedes.saude.gov.br/images/sala-de-situacao/Microcefalia-Protocolo-de-vigilancia-e-resposta-10mar2016-18h.pdf [ Links ]
5. Leite PL. Síndrome de Guillan-Barré e manifestações neurológicas relacionadas a doença exantemática anterior [Apresentação realizada para o Comitê Técnico Assessor do Programa Nacional de Controle da Dengue do Ministério da Saúde (CTA-PNCD/MS); 2015 set 30; Brasília, Brasil]. [ Links ]
6. Sejvar JJ, Baughman AL, Wise M, Morgan OW. Population incidence of Guillain-Barré syndrome: a systematic review and meta-analysis. Neuroepidemiology. 2011;36(2):123-33. [ Links ]
7. Hugh JW, Bart CJ, Pieter AVD. Guillain-Barré syndrome: a systematic review. Lancet. 2016 Aug;388(10045):717-27. [ Links ]
8. Sejvar JJ, Kohl KS, Gidudu J, Amato A, Bakshi N, Baxter R, et al. Guillain-Barré syndrome and Fisher syndrome: case definitions and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine. 2011 Jan;29(3):599-612. [ Links ]
9. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Confirmação do Zika vírus no Brasil [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2016 set 12]. Disponível em: Disponível em: http://portalsaude.saude.gov.br/index.php/o-ministerio/principal/secretarias/svs/noticias-svs/17702-confirmacao-do-zika-virus-no-brasil [ Links ]
10. Instituto Brasileiro de Geografia e Estatística. Estimativas de população para 1º de julho de 2015 [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2016 [citado 2016 set 12]. Disponível em: Disponível em: http://www.ibge.gov.br/home/estatistica/populacao/estimativa2015/estimativa_tcu.shtm [ Links ]
11. Newswanger DL, Warren CR. Guillain-Barré syndrome. Am Fam Physician. 2004 May;69(10):2405-10. [ Links ]
12. Kuwabara S. Guillain-Barré Syndrome: Epidemiology, Pathophysiology and Management. Drugs. 2004;64(5):1-14. [ Links ]
13. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância das Doenças Transmissíveis. Protocolo de vigilância dos casos de manifestações neurológicas com histórico de infecção viral prévia [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2016 set 13]. Disponível em: Disponível em: http://portalsaude.saude.gov.br/images/pdf/2016/janeiro/15/Protocolo-de-vigila--ncia-de-manifestac--a--o-neurolo--gica-Vers--o-FINAL.pdf [ Links ]
14. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Febre pelo vírus Zika: uma revisão narrativa sobre a doença. Bol Epidemiol. 2015;46(26):1-7. [ Links ]
15. Cardoso CW, Paploski IAD, Kikuti M, Rodrigues MS, Silva MMO, Campos GE, et al. Outbreak of exanthematous illness associated with Zika, Chikungunya, and Dengue viruses, Salvador, Brazil. Emerg Infect Dis. 2015 Dec;21(12):2274-6. [ Links ]
16. Dejnirattisai W, Supasa P, Wongwiwat W, Rouvinski A, Barba-Spaeth G, Duangchinda T, et al. Dengue virus sero-cross-reactivity drives antibody- dependent enhancement of infection with Zika virus. Nat Immunol. 2016 Sep;17(9):1102-8. [ Links ]
17. Silva IRF, Fontera JA, Nascimento OJM. News from the battlefront: Zika Virus associated Guillain-Barré syndrome in Brasil. Neurology. 2016 Sep. [ Links ]
18. Cao-Lormeau V, Blake A, Mons S, Lastère S, Roche C, Vanhomwegen J, et al. Guillain-Barré Syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet. 2016 Apr;387(10027):1531-9. [ Links ]
19. Zambrano H, Waggoner JJ, Almeida C, Rivera L, Benjamin JQ, Pinsky BA. Zika virus and Chikungunya virus co-infections: a series of three cases from a single center in Ecuador. Am J Trop Med Hyg. 2016 Jul. [ Links ]
Received: July 25, 2016; Accepted: September 05, 2016











 texto em
texto em