Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2337-9622
Epidemiol. Serv. Saúde v.26 n.1 Brasília jan./mar. 2017
http://dx.doi.org/10.5123/s1679-49742017000100004
ORIGINAL ARTICLE
Hospitalization due to road traffic injuries in Brazil, 2013: hospital stay and costs*
1Ministério da Saúde, Departamento de Vigilância de Doenças e Agravos Não Transmissíveis e Promoção da Saúde, Brasília-DF, Brasil
2Universidade de São Paulo, Faculdade de Saúde Pública, São Paulo-SP, Brasil
Objetivo:
to describe hospitalization rates and to estimate hospital costs and time spent in hospital due to road traffic accidents (RTA) in Brazil, in 2013.
Methods:
this is an ecological study conducted using data from the Brazilian National Hospital Information System.
Results:
in 2013, 170,805 hospitalizations due to RTA were funded by the Brazilian National Health System; 78.2% of the individuals were male, 48.6% were from 20 to 39 years old, and 51.9% were motorcyclists; RTA hospitalization rate was of 85.0 hospitalizations/100,000 inhabitants; total cost was BRL 231,469,333.13, with 1,072,557 hospital inpatient days and average stay of 6.3 days in hospital.
Conclusion:
the magnitude of hospitalization due to RTA was high; victims hospitalized were mainly men, young adults and motorcyclists; average stay in hospital was almost a week, implying significant costs.
Key words: Accidents, Traffic; Morbidity; Hospitalization; Costs and Cost Analysis; Epidemiology, Descriptive
Introduction
According to the World Health Organization’s (WHO) estimates, concerning the year 2013, 1.25 million deaths due to road traffic accidents (RTA) occurred annually. According to WHO data from 1998, the number of people with non-fatal injuries due to these conditions would vary from 20 to 50 million per year.1,2
RTA affects about 1 to 2% of the gross domestic product (GDP) of low and middle-income countries, reflecting a cost that exceeds 100 billion dollars per year.2 In 1997, RTA estimated cost was of $18.9 billion in Latin America, and $453.3 billion worldwide.3
A literature review published in 1997 describes that, in low and middle-income countries, from 30 to 86% of trauma hospitalizations occurred due to RTA.4 RTA victims represented 13 to 31% of all external causes’ hospital care, and 48% of beds in surgical wards. In addition, these individuals required more care than other patients hospitalized due to other external causes in surgical centers, intensive care units (ICU), radiological centers and physiotherapy and rehabilitation services.4
In 2003, the number of hospitalizations due to external causes was 6.2 times higher than the number of deaths from this same group of causes. Furthermore, data analysis from the National Traffic Department showed that in 2002, in Brazil, there were 337,190 accidents with victims, and 94.4% of them were non-fatal. Each RTA involved 1.5 victim on average, and for each fatal victim there were 17 cases of non-fatal victims, stressing that RTA morbidity is much higher than RTA mortality.5
RTA victims’ hospitalization depicts the severity of the event and constitutes a considerable portion of expenditures due to this condition.6 In general, health costs can be categorized as direct, indirect or intangible. The study of direct cost in health aims to quantify, in monetary values, the amount of resources directly used in the treatment/intervention of a patient, and can be subdivided into medical costs (hospitalization, medicines, fees etc.) and non-medical costs (patient transport, food, etc.). Indirect costs, in turn, refer to the loss of working time suffered by the patient or by their relatives as a consequence of the disease/condition or their treatment, and can be measured, for example, in terms of loss of productivity.7,8 Intangible costs are harder to measure and involve health gain, pain or distress associated with the treatment.
Health cost analysis may vary, depending on the adopted approach; e.g. from society, health service, government, among others. Under this perspective, the source of relevant costs is described based on the purpose of the study.7,8 Mello Jorge and Koizumi reported that hospital expenditures with care to road traffic victims are much higher than those with patients admitted for treatment of diseases.9 Economic loss, which is represented by both direct and indirect medical costs of RTA, is even higher amongst poor households, having a greater impact on the family budget.2
We must also consider the social costs associated with the use of motor vehicles related to the occurrence of deaths and injuries resulting from RTA, to air pollution, to the "barrier effect" (difficulty in social relationships of residents from a certain area attributed to vehicles transit), and to traffic jam.10
Accordingly, the objective of this study was to describe hospitalization rates due to road traffic accidents - RTA - in Brazil in 2013, to estimate hospital costs and length of hospital stay owing to RTA in the Brazilian National Health System (SUS).
Methods
A descriptive study was conducted with data on RTA hospitalizations, recorded in the Brazilian National Hospital Information System (SIH/SUS), available at the website of SUS IT Department (Datasus).11
SIH/SUS, a financial management system of SUS hospital component, covers both the hospital network itself and the network formed by the private hospitals which are partners of the public health sector.12 SIH/SUS exclusively provides data on hospitalizations funded by the public sector, so data concerning injured patients who did not require hospitalization and patients admitted to private health care not linked to the SUS or insured by health insurances are missing from the system.13
For this study, hospitalizations occurred in 2013 and registered under the codes of the International Classification of Diseases - 10th Revision (ICD-10)14 related to road traffic injuries, chapter XX, categories V00 to V89 (external causes of morbidity and mortality) were selected.
Hospitalization rates were calculated considering as numerator the number of hospitalizations in 2013, obtained from SIH/SUS, and, as denominator, the estimated population for Brazil and its macroregions - North, Northeast, Midwest, Southeast and South -, in the same year, estimated by the Brazilian Institute of Geography and Statistics (IBGE).15 Hospitalization rates in Brazilian macroregions were standardized by age, through direct method, employing the Brazilian population in 2013 as default. The age standardization method aims to minimize the effect of the differences in age structure between regions on the indicators, allowing comparisons between them.
Hospitalization rates for Brazil were calculated according to sex (male; female), age (in years: 0 to 9; 10 to 19; 20 to 39; 40 to 59; 60 and over) and type of victim (pedestrian; cyclist; motorcyclist; car occupant; truck occupant; bus occupant; other).
SUS expenditure with hospitalizations due to RTA were also projected (amounts in Brazilian currency): total costs, hospital and professional services costs, and average cost per hospitalization), length of hospital stay and average of inpatient days, all relating 2013.
The software used for the analyses was Microsoft Excel for Mac 2011, version 16.6.2.
The study was dismissed from consideration by an Ethics Research Committee for using only anonymous publicly available data. Ethical guidelines for research with human beings were complied, as recommended by the Resolution No. 466 of the National Health Council (CNS) dated December 12, 2012.
Results
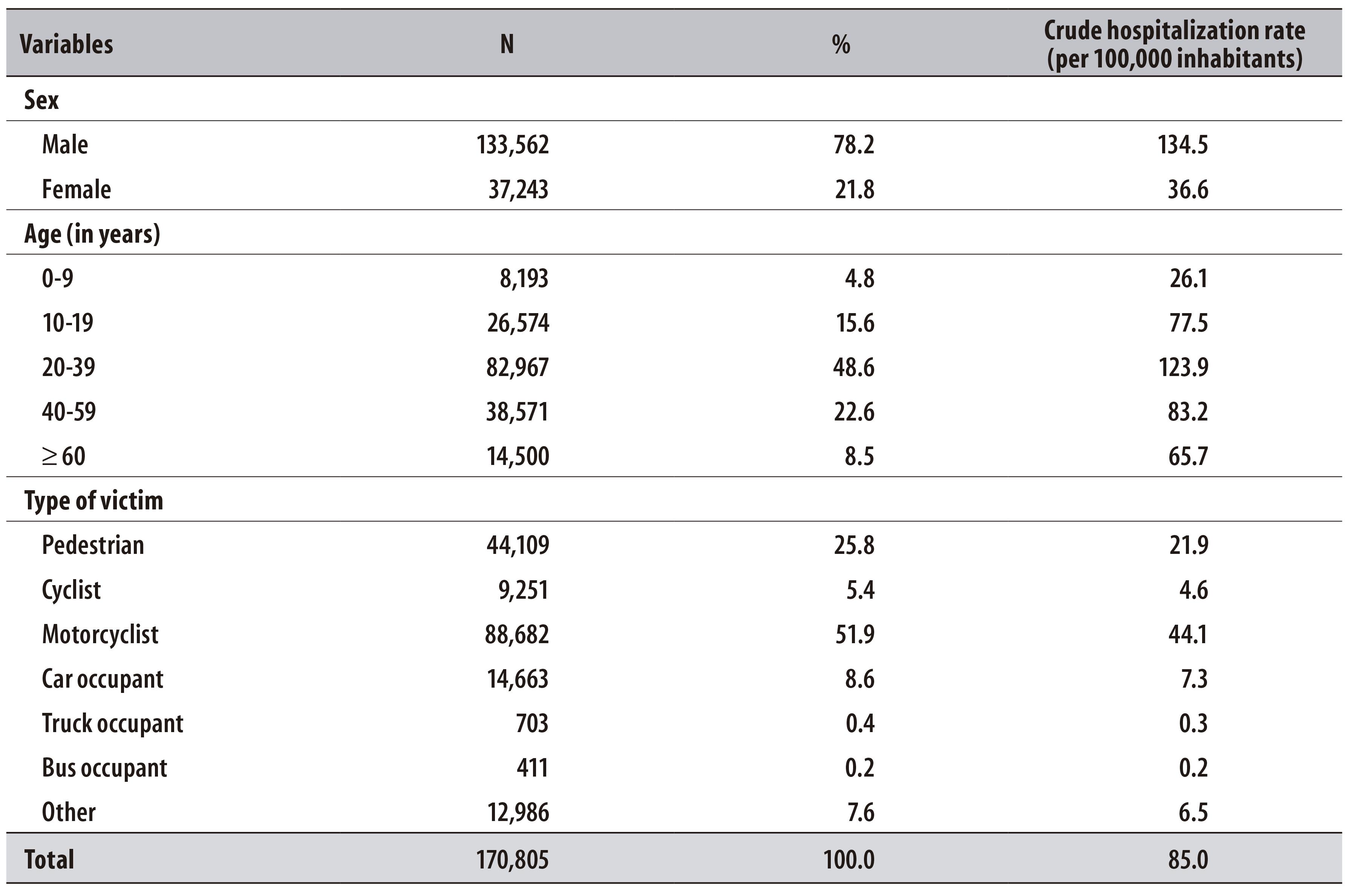
In Brazil, in 2013, 170,805 hospitalizations due to RTA were recorded on SIH/SUS, which represents a rate of 85.0 hospitalizations per 100,000 inhabitants. The highest hospitalization rates due to RTA were observed among male individuals (134.5 hospitalizations per 100,000 men), in the age group from 20 to 39 years old (123.9 hospitalizations per 100,000 inhabitants in this age group). More than half of the hospitalizations due to RTA involved motorcyclists (51.9%; 44.1 hospitalizations per 100,000 inhabitants), followed by pedestrians (25.8%; 21.9 hospitalizations per 100,000 inhabitants) (Table 1).
Table 1 - Absolute number, percentage and crude hospitalization rate of road traffic accidents according to sex, age and type of victim, Brazil, 2013
The highest crude and standardized rates of hospitalizations due to RTA (both per 100,000 inhabitants) were found in the Midwest (98.0 and 96.6, respectively) and Northeast (89.1 and 90.2, respectively) regions (Table 2).
Table 2 - Absolute number, crude and standardized hospitalization rates of road traffic accidents, Brazil and macrorregions, 2013

a) Standardized by age through direct method, employing the Brazilian population in 2013 as default.
Total costs with hospitalizations due to RTA in 2013, within the National Health System, were of BRL 231,469,333.13, of which BRL 188,025,095.94 corresponded to hospital services costs and BRL 43,361,377.01 to professional services. The average hospitalization cost per RTA in the studied period was BRL 1,355.17. A total of 1,072,557 inpatient days were accounted for all hospitalized victims, with an average length of hospital stay of 6.3 days per patient (Table 3).
Table 3 - Number of hospitalizations due to road traffic accidents, costs (in Brazilian Reais (R$)) and time and average stay (in days) according to the type of victim, Brazil, 2013
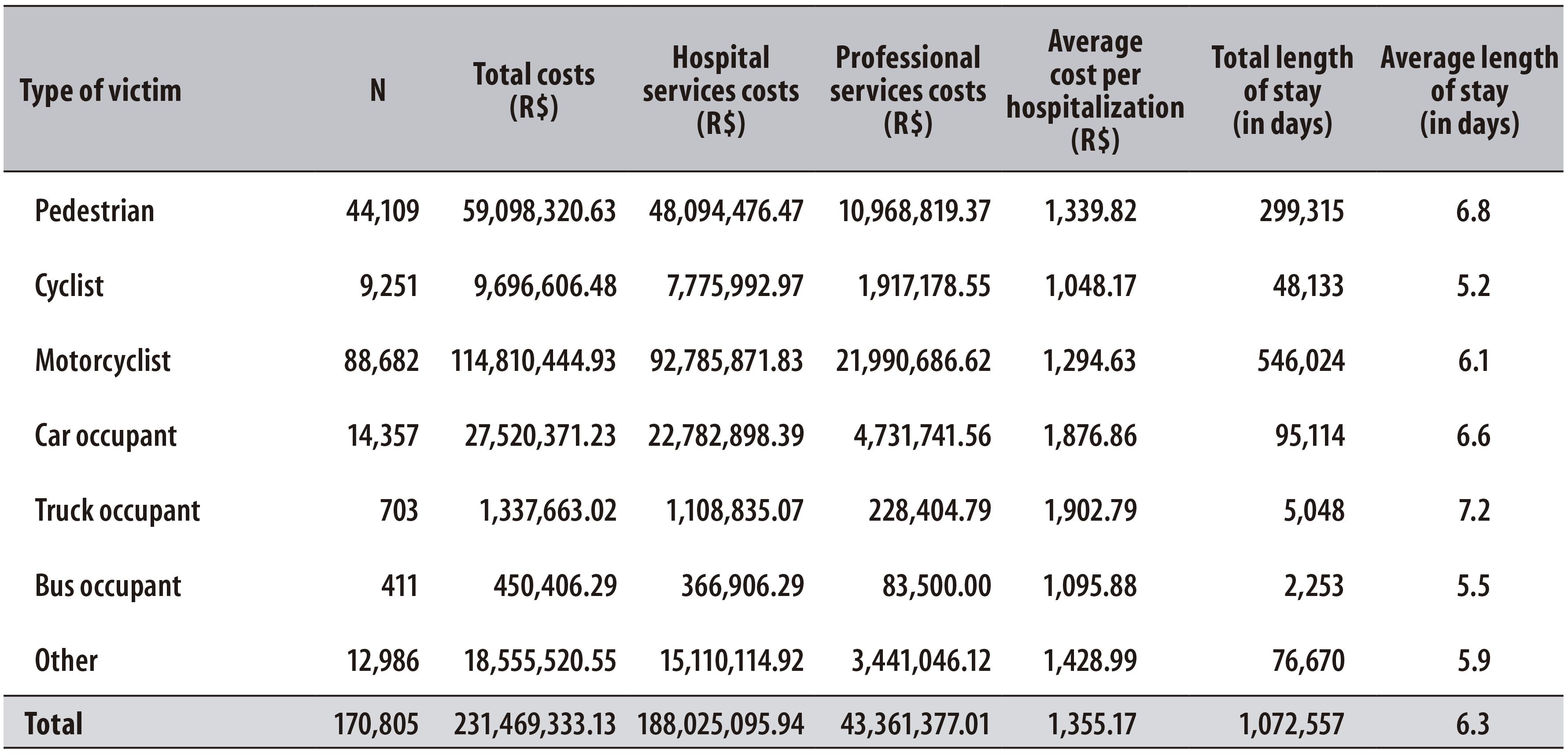
Motorcyclists were the victims with the longest hospital stay (546,024 days) and the highest total costs (BRL 114,810,444.93). However, the highest average hospitalization cost was represented by truck occupants (BRL 1,902.79), who also responded to the highest average length of hospital stay (7.2 days), followed by pedestrians (6.8 days) (Table 3).
Discussion
Male individuals, young adults and motorcyclists residing in the Midwest and Northeast regions of Brazil were dominant among RTA victims admitted to public hospitals or to private hospitals insured by SUS. Total hospitalization costs due to RTA exceeded BRL 230 million, and the average length of hospital stay of each RTA victim was of almost one week.
The main determinants of hospitalization due to RTA are: male sex; pedestrian, cyclist and motorcyclist; age group over 50 years; accident involving collision with heavy transport or bus; and the event having occurred late at night or during the afternoon.6,16-18 Literature points that males and the age group from 20 to 39 years as the most vulnerable groups to RTA.2,6,17-19
According to the National Household Sample Survey (PNAD), conducted by IBGE in 2008, 2.5% of Brazilians (approximately 4.8 million people) reported having suffered any RTA within 12 months preceding the survey; male individuals had 2.3 times more involvement in this type of accident than females; and an increased RTA frequency was observed amongst individuals in the age group from 18 to 24 and from 25 to 34 years.20
A likely explanation for this finding is the fact that men culturally expose themselves more often to dangerous situations, such as drink-driving. Data from National Health Survey (PNS), representative of Brazilian adults, and from the Surveillance System of Risk and Protective Factors for Chronic Diseases by Telephone Survey (Vigitel), representative of adults residing in 26 Brazilian state capitals and the Federal District, pointed out that both the attitude of driving a vehicle after drinking alcoholic beverages (29.3% [Vigitel]; 24.4% [PNS]) and the habit of drunk driving (9.4% [Vigitel]; 7.4% [PNS]) were higher among male individuals.21
In 2005, 118,122 hospitalizations due to RTA were recorded in SIH/SUS, which corresponded to a hospitalization rate of 64.1 per 100,000 inhabitants.19 In 2012, there were 159,251 hospitalizations due to RTA, with hospitalization rate of 82.0 per 100,000 inhabitants.15 According to data from Violence and Accidents Survey (VIVA), conducted in urgent and emergent health services of 11 Brazilian municipalities from September to October 2011, RTA were responsible for 4,413 health assistances, of which about one quarter evolved to emergency hospitalization within the first 24 hours.17
An analysis on the hospitalizations trends due to RTA between 2002 and 2012 showed an increase in these rates, with higher increment (250%) in hospitalizations of motorcyclists: 1.2 hospitalizations per 10,000 inhabitants in 2002 and 4.2 per 10,000 inhabitants in 2012.16
According to this study, the highest hospitalization rates were observed in the Midwest and Northeast regions. According to PNAD, Brazilian Midwest presented the highest proportion of people involved in RTA (3.3%), in 2008, whereas the Northeast showed the lowest percentages (1.9%).20 In 2012, the crude rate of hospitalizations due to RTA in the Midwest region was the highest in the country (10.0 hospitalizations per 10,000 inhabitants), followed by the Southeast (8.7 hospitalizations per 10,000 inhabitants).16
The Midwest region also presented the highest mortality rate due to RTA in 2011 (30.8 deaths per 100,000 inhabitants). The high hospitalization rates in the Midwest and Northeast regions are possibly attributed to drink-driving, and to the little use of security equipment.21,22 Another possible explanation for the regional differences identified was the implementation of traffic laws in the Southeast region before the Brazilian Traffic Code, besides a more effective surveillance and more intense use of speed control strategies.23
The first estimate on SUS hospital expenditures due to external causes was conducted in 1994, showing a cost of BRL 23,923,861.94 with hospitalizations due to external causes only in November of that year.24 In the period from 1998 to 2006, considering only RTA involving motorcyclists, the cost was of BRL 5.3 billion, or BRL 1,400.00 per motorcycle circulating in the country.10
Hospital expenditures exceeded BRL 230 billion in 2013, with the highest percentage concerning costs related to hospital services, and the average hospitalization cost exceeded BRL 1,300.00, whereas the average length of hospital stay was of almost one week. In 2012, BRL 193,328,361.76 were spent in the hospitalization of RTA victims attended by SUS, and the average length of hospital stay ranged from 4.8 (cyclists) to 9.7 (pedestrians) days, depending on the type of victim.16 Certainly, the factors that influence both the length of hospital stay and the hospital expenditures due to RTA include trauma severity, the need of life support equipment and stay in intensive care units.
A limitation of this study is the fact that data refer only to hospitalizations funded by the Brazilian National Health System (SUS). However, SIH/SUS covers about 70% of hospitalizations throughout the country and represents the best available source of data on RTA.25-28 Furthermore, social costs for hospitalizations due to RTA were not evaluated, or their impact on injured individuals, on their relatives and on society. Another limitation of this research lies on the possibility of hospitalization costs having been underestimated, as there is an additional funding on SIH/SUS table of values, intended to these services:29 states and municipalities can pay for these hospitalizations, so they may exceed the values presented on SUS procedure table, which paid directly by the federal government.
A literature review that covers the period from 1998 to 2010 describes the Brazilian situation when it comes to RTA as alarming, especially in relation to the increase in the total number of deaths and mortality rates, expanded fleet of motorcycles, and the practice of the binomial ‘drink-driving’. Measures adopted by the Government to deal with the issue of RTA have been incipient and unsatisfactory.23
Both the effect of legal actions on the behavior of the population and the Project Life in Traffic are punctual actions which, added to other factors such as the obligation to inform speed radar locations, reduced penalties and lack of education programs for transit, act as negative determinants for not achieving the goals for a sustainable way over time as proposed by the Global Road Safety Plan which aims at the reduction on the number of RTA.23
Hospitalizations due to RTA have a huge impact on society, especially when involving young and economically active population, and justify immediate interventions. In addition to the measures adopted by the health sector, intersectoral and multi-institutional actions must become part of the Government plans in order to tackle morbidity and mortality due to RTA, breaking with the centralization of preventive actions directed to the victim.26
The magnitude of hospitalizations due to road traffic accidents was high in 2013, demonstrating significant expenses. These hospitalizations have a significant social and economic impact, increasing costs of the families’ budgets and of Social Security, as they affect predominantly men and young people. Brazil has a wide and challenging way to go in order to reverse this scenario.
REFERENCES
1. Organização das Nações Unidas. Resolution adopted by the General Assembly [Internet]. Genebra: Organização Mundial de Saúde; 2010 [cited 2016 Aug 10]. 349 p. Available from: http://www.who.int/violence_injury_prevention/publications/road_traffic/UN_GA_resolution-54-255-en.pdf [ Links ]
2. Organização Mundial de Saúde. Relatório global sobre o estado da segurança viária 2015. Genebra: Organização Mundial de Saúde ; 2015 [citado 2016 ago 10]. Disponível em: Disponível em: http://www.who.int/violence_injury_prevention/road_safety_status/2015/en/ [ Links ]
3. Organização Pan-Americana da Saúde. Organização Mundial da Saúde. Ministério da Saúde (BR). Relatório mundial sobre prevenção de lesões causadas pelo trânsito: resumo. Brasília: Organização Pan-Americana da Saúde; 2012. [ Links ]
4. Odero W, Garner P, Zwi A. Road traffic injuries in developing countries: a comprehensive review of epidemiological studies. Trop Med Int Health. 1997 May; 2(5):445-60. [ Links ]
5. Souza ER, Lima MLC. Panorama da violência urbana no Brasil e suas capitais. Cienc Saude Coletiva. 2006; 11 supl:1211-22. [ Links ]
6. Soares DFPP, Barros MBA. Fatores associados ao risco de internação por acidentes de trânsito no Município de Maringá-PR. Rev Bras Epidemiol. 2006 jun;9(2):193-205. [ Links ]
7. Folland S, Goodman AC, Stano M. A economia da saúde. 5. ed. Porto Alegre: Bookman; 2008. [ Links ]
8. Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005. [ Links ]
9. Jorge MHPM, Koizumi MS. Gastos governamentais do SUS com internações hospitalares por causas externas: análise no Estado de São Paulo, 2000. Rev Bras Epidemiol. 2004 jun;7(2):228-38. [ Links ]
10. Vasconcellos EA. O custo social da motocicleta no Brasil. Rev Transp Publicos. 2008:127-42. [ Links ]
11. Ministério da Saúde (BR). Departamento de Informática do Sistema Único de Saúde. Informações de Saúde (TABNET) [Internet]. Brasília: Ministério da Saúde; 2016 [citado 2016 ago 10]. Disponível em: Disponível em: http://www2.datasus.gov.br/DATASUS/index.php?area=02 [ Links ]
12. Carvalho DM. Grandes sistemas nacionais de informação em saúde: revisão e discussão da situação atual. IESUS. 1997 out-dez;4:7-46. [ Links ]
13. Bastos YGL, Andrade SM, Soares DA. Características dos acidentes de trânsito e das vítimas atendidas em serviço pré-hospitalar em cidade do Sul do Brasil, 1997/2000. Cad Saude Publica. 2005 maio-jun;21(3):815-22. [ Links ]
14. Organização Mundial da Saúde. Classificação estatística internacional de doenças e problemas relacionados à saúde: CID 10. São Paulo: Edusp; 1994. [ Links ]
15. Instituto Brasileiro de Geografia e Estatística. Estimativas populacionais para os municípios brasileiros em 01.07.2013 [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2013 [citado 2016 ago 10]. Disponível em: Disponível em: http://www.ibge.gov.br/home/estatistica/populacao/estimativa2013/default.shtm [ Links ]
16. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise de Situação de Saúde. Saúde Brasil 2012: uma análise da situação de saúde e dos 40 anos do Programa Nacional de Imunizações. Brasília: Ministério da Saúde; 2013. [ Links ]
17. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Doenças e Agravos Não Transmissíveis e Promoção da Saúde. Sistema de Vigilância de Violências e Acidentes (Viva): 2009, 2010 e 2011. Brasília: Ministério da Saúde; 2013. [ Links ]
18. Andrade SM, Jorge MHPM. Características das vítimas por acidentes de transporte terrestre em município da Região Sul do Brasil. Rev Saude Publica. 2000 abr;34(2):149-56. [ Links ]
19. Jorge MHPM, Koizumi MS. Acidentes de trânsito no Brasil: um atlas de sua distribuição. Rev Abramet. 2008;26(1):52-8. [ Links ]
20. Malta DC, Mascarenhas MDM, Bernal RTI, Silva MMA, Pereira CA, Minayo MCS, et al. Análise das ocorrências das lesões no trânsito e fatores relacionados segundo resultados da Pesquisa Nacional por Amostra de Domicílios (PNAD) Brasil, 2008. Cienc Saude Coletiva. 2011 set;16(9):3679-87. [ Links ]
21. Malta DC, Bernal RTI, Mascarenhas MDM, Silva MMA, Szwarcwald CI, Morais Neto OL. Consumo de bebidas alcoólicas e direção de veículos nas capitais brasileiras e no Distrito Federal, segundo dois inquéritos nacionais de saúde. Rev Bras Epidemiol. 2015 dez;18 supl 2:214-23. [ Links ]
22. Malta DC, Andrade SSCA, Gomes N, Silva MMA, Morais Neto OL, Reis AAC, et al. Lesões no trânsito e uso de equipamento de proteção na população brasileira, segundo estudo de base populacional. Cienc Saude Coletiva. 2016 fev;21(2):399-410. [ Links ]
23. Bacchieri G, Barros AJD. Traffic accidents in Brazil from 1998 to 2010: many changes and few effects. Rev Saude Publica. 2011 Sep;45(5):949-63. [ Links ]
24. Iunes RF. Impacto econômico das causas externas no Brasil: um esforço de mensuração. Rev Saude Publica .1997 ago;31(4)supl:38-46. [ Links ]
25. Reichenheim ME, Souza ER, Moraes CL, Jorge MHPM, Silva CMFP, Minayo MCS. Violence and injuries in Brazil: the effect, progress made, and challenges ahead. Lancet. 2011 Jun;377(9781):1962-75. [ Links ]
26. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise de Situação de Saúde. Saúde Brasil 2011: uma análise da situação de saúde e a vigilância da saúde da mulher. Brasília: Ministério da Saúde ; 2012. [ Links ]
27. Silva ZP, Ribeiro MCSA, Barata RB, Almeida MF. Perfil sociodemográfico e padrão de utilização dos serviços de saúde do Sistema Único de Saúde (SUS), 2003 - 2008. Cienc Saude Coletiva. 2011 set;16(9):3807-16. [ Links ]
28. Bittencourt SA, Camacho LAB, Leal MC. O Sistema de informação hospitalar e sua aplicação na saúde coletiva. Cad Saude Publica. 2006 jan;22(1):19-30. [ Links ]
29. Gonçalves MA, Ferreira BP, Alemão MM. Risco operacional no setor saúde: financiamento pelo SUS paralelo aos gastos na fundação hospitalar do Estado de Minas Gerais. Rev Gestao Tecnol. 2014 jan-abr;14(1):126-50. [ Links ]
*Article based on Silvânia Suely Caribé de Araújo Andrade's PhD thesis entitled ‘A perspective on traffic accidents in Brazil: from hospitalizations and sequelae to death: a contribution to their surveillance’, presented to the Postgraduate Program on Public Health of the University of São Paulo (USP) in 2015.
Received: April 21, 2016; Accepted: July 19, 2016











 texto em
texto em 
 Curriculum ScienTI
Curriculum ScienTI

