Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2337-9622
Epidemiol. Serv. Saúde v.26 n.1 Brasília jan./mar. 2017
http://dx.doi.org/10.5123/s1679-49742017000100009
ORIGINAL ARTICLE
Cesarean sections in Piauí State: trend and associated factors in the period 2000-2011, Brazil
1Universidade Estadual do Piauí, Núcleo de Pesquisa e Extensão em Saúde da Mulher, Teresina-PI, Brasil
OBJECTIVE:
to analyze trends in cesarean sections proportion and associated factors in Piauí State, Brazil, from 2000 to 2011.
METHODS:
this is a time series and cross-sectional study, with data of all institutional childbirths in primiparous, recorded on the Information System on Live Births (Sinasc).
RESULTS:
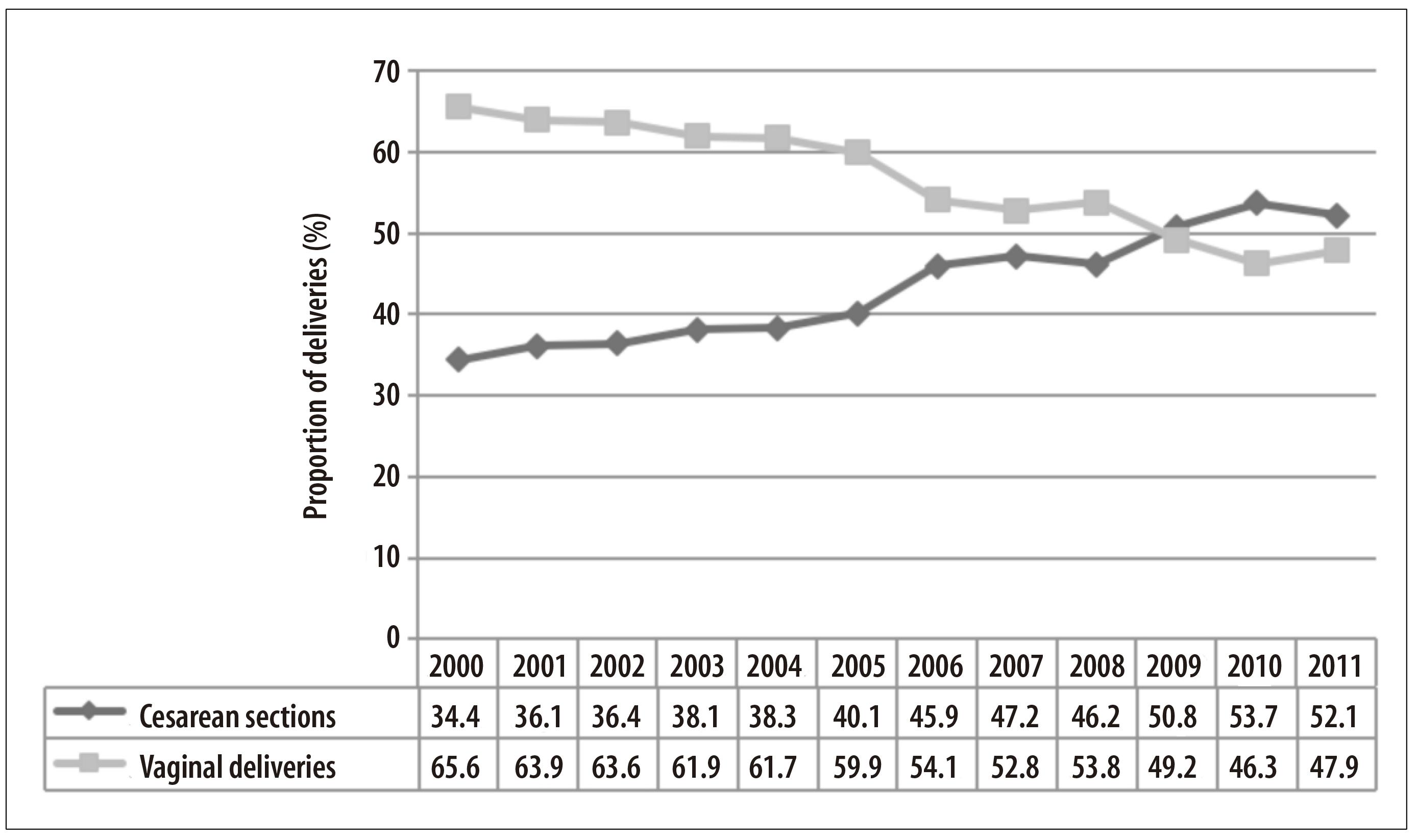
cesarean sections proportion increased from 34.4% in 2000 to 52.1% in 2011 (annual percentage change +4.4; 95%CI 3.6;5.1); white-skinned women (PR=1.72; 95%CI 1.63;1.86), over 40 years (PR=2.17; 95%CI 2.09;2.28), with more than 12 years of schooling (PR=1.86; 95%CI 1.77;1.96), who attended 7 or more prenatal care appointments (PR=2.08; 95%CI 1.97;2.18), residents in municipalities with over 300,000 inhabitants (PR=1.68; 95%CI 1.62;1.80) and with higher Human Development Index (PR=1.61; 95%CI 1.51;1.73) presented the highest cesarean sections proportion.
CONCLUSIONS:
the occurrence of cesarean sections was high and more frequent in women with low obstetric risk.
Key words: Cesarean Section; Trends; Risk Factors; Health Inequalities; Time Series Studies; Cross-Sectional Studies
Introduction
The proportion of cesarean sections in Brazil is one of the highest in the world, much higher than the 15% limit recommended by the World Health Organization (WHO) to ensure good fetal-maternal results.1,2 In all regions of Brazil, the percentage of cesarean sections had a relative growth, from 15% in 1970 to 48.8% in 2008,3 and in 2009 it surpassed for the first time the percentage of vaginal deliveries.4 In 2010, whilst the Northeast and North regions had a proportion of cesarean sections of 41% and 44%, respectively, the South and Southeast regions had higher proportions: 58.1% and 58.2%, respectively.4
The cesarean section is an effective intervention to reduce maternal and neonatal morbidity and mortality, in the presence of adequate clinical indication. However, non-clinical factors are associated with the high number of cesarean sections, such as the relation between purchasing power and the health services accessibility which provide the surgical procedure.5 This hypothesis is reinforced when we verify that the most important factors for its occurrence are socioeconomic characteristics, higher number of prenatal care appointments and deliveries carried out in the private sector.5-8 These factors have a direct association with the organization of obstetric care, often guided by the convenience of a scheduled intervention, and to physicians’ and patients’ preference for cesarean section.9-11
In Brazil, many researches have shown that, according to physicians, most women prefer the cesarean section. They suggest that the reasons for this preference are related to fear of pain during vaginal delivery, concerns over injuries on the pelvic floor, the belief that vaginal delivery is riskier than cesarean section, and also the possibility of undergoing tubectomy in the same surgery.12,13 However, studies on the women’s preference do not corroborate with this argument.12,14 A national hospital-based survey inquired 23,940 puerperal women between 2011 and 2012 and revealed that the proportion of cesarean sections was three times higher than the initial preference reported by women, especially in the private sector. The most cited factor in preference for cesarean delivery was the fear of pain during delivery, however there was no reference of choosing cesarean section to prevent injuries on the pelvic floor.11
In Brazil, the private sector is the main contributor to the high proportion of cesarean sections. In 2006, the percentage of cesarean deliveries in the public health system and the private health services was of 33.2% and 77.2%, respectively.15 National surveys suggest that, although most women desire a vaginal delivery at the beginning of their pregnancy, in the private sector they undergo cesarean sections before going into labor, 90% of the times without an adequate medical justification.10,11,14,15 Furthermore, the prevalence of prematurity in cesarean sections is higher in private health services that assist women with higher socioeconomic and education levels when compared to those of public health services.1,16 The high frequency of elective cesarean sections without an adequate clinical recommendation could be the main factor for a higher percentage of low weight newborns among the population with better socioeconomic level.17
Although there is still some debate about an adequate proportion of cesarean sections for each country, both very high and low rates are considered unsatisfactory. A low percentage of cesarean sections demonstrates women’s difficulty to access health services with appropriate technology. On the other hand, a high percentage of cesarean sections can determine negative consequences such as maternal and neonatal morbidity and mortility.18,19 Data from Asian and African countries reveal that the frequency of cesarean sections is higher among wealthier urban women and lower among poorer women from rural zones.20 This pattern of inequality demonstrates the low usage of cesarean sections in low-income countries, where women would most need it, and the excess of cesarean sections in middle and high-income countries, where the obstetric risk is lower.6,7
Little is known about birth methods practiced in the state of Piauí. A research that evaluated the time trends of cesarean sections in Brazil from 1994 to 2009 showed that Piauí, just like the other states, had an increasing trend in this period with an average percentage variation of 2% per year.21 However, maternal and regional characteristics which can be related to the cesarean section procedures have not been investigated. The objective of this study was to analyze the trends in cesarean sections proportion and associated factors in Piauí State, Brazil, from 2000 to 2011.
Methods
This is a time series and cross-sectional study with data from the Information System on Live Births (Sinasc) of the Health Surveillance Secretariat of the Ministry of Health. The data refer to the period from 2000 to 2011.
Piauí State is located in the mid-northern of Brazil’s Northeast region and is composed by 224 municipalities, covering an area of 251,611km2. In 2015, the estimated population of Piauí was of 3,204,028 inhabitants, and 65.9% lived in urban areas. Although there have been advances in the development indicators in the past few years, the state still has one of the lowest income distribution and education level in the country.22
All hospital childbirths of primiparous women residing in Piauí, with single gestation and gestational age equal to or over 22 weeks, and whose newborns weighted 500g or more were included in the study. The proportion of cesarean sections was calculated by dividing the number of cesarean sections by the total number of childbirths, and then multiplying it by 100. This proportion was calculated for the whole period (2000-2011) and for four year periods: 2000-2003, 2004-2007 and 2008-2011.
The independent variables taken from Sinasc were: maternal age (in years: less than 20; 20-29; 30-39; ≥40), education level (in complete schooling years: none; 1-3; 4-7; 8-11; ≥12), ethnicity/skin color (white; black; yellow; brown; indigenous), number of prenatal care appointments (0; 1-6; ≥7) and pregnancy duration (in weeks: 22-36; 37-41; ≥42). The municipality’s size (in number of inhabitants: up to 20,000; from 20,001 to 50,000; from 50,001 to 100,000; from 100,001 to 300,000; and more than 300,000) and the Municipal Human Development Index (M-HDI) (classified in quartiles: from 0.485 to 0.546; from 0.547 to 0.565; from 0.566 to 0.591; and from 0.592 to 0.751) were provided by the Brazilian Institute of Geography and Statistics (IBGE).
The proportion trends for cesarean sections and vaginal deliveries were assessed based on segmented linear regression, per inflection point - joinpoint -, considering each year from 2000 to 2011. The annual percentage change (APC) and its respective 95% confidence intervals (95%CI) were calculated. We considered that there was an increase in proportions when the trend was increasing and the minimum value of the 95%CI was higher than 0. In turn, we considered that there was a decrease when the trend was decreasing and the maximum value of the 95%CI was below 0. Stability was set when, regardless of the trend, the 95%CI was equal to 0.
The analysis of the factors associated with the cesarean sections was calculated using the crude and adjusted prevalence ratios (PR) and their respective 95%CI, through Poisson regression with robust adjustment of variance.23 The dependent variable was the type of delivery (cesarean section or vaginal delivery). The adjusted analysis was carried out with the hierarchical model in two levels: the first level included age, education level, ethnicity/skin color and duration of pregnancy; and the second level included the number of prenatal care appointments, the municipality size and the M-HDI. The categories chosen as reference were those considered less risky to the occurrence of cesarean sections.
This study was approved by the Ethics Committee in Research of the State University of Piauí (CAAE No. 15524213.2.0000.5209) on July 16, 2013.
Results
Over the 12 years studied, 651,587 live births were registered in Piauí, from which 215,594 (33.1%) corresponded to hospital childbirths, of primiparous women, with single gestation. The proportion of cesarean sections for this subgroup was of 43.9%. Figure 1 shows that since 2009 the proportion of cesarean sections is higher than the proportion of vaginal deliveries. There was a significant increasing trend of cesarean sections in the studied period (APC: +4.4; 95%CI 3.6;5.1) (Table 1).
Table 1 - Trends in proportion (%) of cesarean sections, according to variables and period, in Piauí, 2000-2011

a) APC: annual percentage change, calculated for each year, by segmented linear regression, by inflection point or joinpoint.
b) 95%CI: 95%confidence interval
c) Missing data in 1,513 (1.6%) cases
d) Missing data in 7,757 (8.2%) cases
e) Missing data in 851 (0.9%) cases
f) Missing data in 757 (0.8%) cases
The proportion of cesarean sections increased in all groups of maternal age, education level, ethnicity/skin color, number of prenatal care appointments, gestational age, municipality size and M-HDI, from the 2000-2003 to the 2008-2011 period. The highest increase occurred among women with less than 20 years old (+44%; APC: +5.3; 95%CI 4.1;6.8), with education level equal or higher than 12 schooling years (+48.5%; APC: +5.1; 95%CI 4.3;7.1), white-skinned (+67.7%; APC: +5.8; 95%CI 4.7;7.2), with more than seven prenatal care appointments (+50.4%; APC; +3.9; 95%CI 2.2;5.1), gestational age from 37 to 41 weeks (+79.3%; APC: +2.8: 95%CI 2.0;4.2), residents in municipalities with more than 300 thousand inhabitants (+49%; APC: +4.2; 95%CI 2.8;5.9) and with a high M-HDI (+51%; APC: +3.4; 2.6;4.3) (Table 1).
Women aged 40 or older showed a higher proportion of cesarean sections (PRadj=2.17; 95%CI 2.09;2.28) when comparing to those with less than 20 years old for all the periods. The proportion of cesarean sections was higher among women with more than 12 years of schooling (PRadj=1.86; 95%CI 1.77;1.96) than among illiterate women. White women (PRadj=1.72; 95%CI 1.63;1.86) and those who attended seven or more prenatal care appointments (PRadj=2.08; 95%CI 1.97;2.18) also had greater proportions of cesarean sections. Municipalities with more than 300 thousand inhabitants (PRadj=1.68; 95%CI 1.62;1.80) and those with higher M-HDI (PRadj=1.61; 95%CI 1.51;1.73) had more cesarean sections in all the periods. Except for maternal age and municipality size, all variables showed higher prevalence ratios in the 2008-2011 period (Table 2).
Table 2 - Crude and adjusted prevalence ratios of the relation between cesarean sections and maternal and municipalities characteristics, according to period, in Piauí, 2000-2011

a) PRc: crude prevalence ratio
b) 95%CI: 95% confidence interval
c) PRadj: adjusted prevalence ratio, calculated by Poisson regression with robust adjustment of the variance - the adjustment variables considered were age, education level, ethnicity/skin color, pregnancy duration (1st level); and number of prenatal care appointments, municipality size and M-HDI (2nd level).
Discussion
The proportion of cesarean sections among primiparous women with a single gestation has shown increasing trend in Piauí. This growth has occurred in all groups, but it was predominant among white women with more years of schooling, who attended more prenatal care appointments, residents of municipalities with more than 300 thousand inhabitants and with a higher M-HDI. These data suggest some inequalities in women’s profile with access to cesarean sections in the state; and the decision for the procedure was probably not only based on technical criteria, which is similar to other studies’ findings.5,6,8,10,14
The proportion of cesarean sections in Piauí is nearly three times higher than the amount recommended by WHO.2,18 This pattern is similar to Brazil as a whole and its macroregions, even though there are some exceptions.15,24 In 2012, for instance, proportions between 30.0% and 45.0% have been found in the North and Northeast regions, whereas in the South, Southeast and Midwest, the proportions varied between 55.0% and 65.0%, showing a higher frequency of cesarean sections in wealthier states with higher amount of inhabitants and deliveries.3,15,24 Many factors have been pointed out as determinants for the growth in the proportion of cesarean sections in Brazil. Many studies have mentioned the importance of non-clinical variables, such as women’s age and schooling, their ethnic origin, region of residence, prenatal care, and also the influence of the professional who assists the prenatal care and delivery.7,8,11,12,14,15,20
In this study, maternal age equal or higher than 40 years old was associated with higher prevalence of cesarean sections, as observed in other researches.8,14 The older maternal age is classically considered one of the important factors for increasing the proportion of cesarean sections.25 The higher incidence of chronic diseases in this age group (such as hypertension and diabetes) and myometrium function (due to the lower amount of oxytocin receptors), which reduces with aging, could lead to a higher risk of complications during gestation or labor, and the surgical intervention is used to minimize this risk.25 Although this association cannot be assessed in this study, some authors have demonstrated that obstetric complications themselves do not explain the high proportion of cesarean sections in older women. In addition, the anxiety of women and physicians for considering these pregnancies as “high risk” could overcome the true existence of maternal morbidity in cesarean section recommendation.26
With regard to the impact of gestational age in cesarean section, smaller proportions were verified between the 37th and 41st weeks of pregnancy with little association between post-term gestational age and cesarean sections. Among nulliparous women, the proportions of cesarean sections are lower when the gestational age is between 37 and 40 weeks and labor starts spontaneously.27
Other Brazilian studies have also verified positive association between cesarean sections and maternal education level.8,10,14,15 Rising proportions of cesarean sections were also observed in all groups of maternal education level, suggesting better access to health services for the delivery. In other countries, women with more years of schooling are three to four times more likely to have a cesarean section when compared to illiterate women.6,16,27 In 2009, according to an ethnographic study carried out with 80 puerperal women in Pelotas, Rio Grande do Sul, the women believed that the best quality childbirth care was associated with the technology used in cesarean sections.10 Therefore, women with higher education level would rather request the surgical delivery because they believed it was safer than vaginal delivery, besides being less painful and more convenient.11,14-16,24
The disparity in proportions of cesarean sections per ethnicity/skin color not only can arise from sociocultural characteristics, but also from deficiencies in medical care.27 With results similar to those in this present study, another research with primiparous Brazilians, carried out in 2003 and 2004, revealed that white women had higher proportions of cesarean sections than other skin color groups.8 This pattern is not found in every country, for example, in the United States of America and England, the highest proportions of cesarean sections are among black and Asian women.28,29 Besides the inaccurate definition for skin color, the discrepancy between data can be originated in biological factors, preference of women, family income, and maternal education level, which can influence access and quality of the obstetric care in different places.5,20,29
Since 1980, there has been an increase in the frequency of pregnant Brazilians with an early start of prenatal care, who attended six or more appointments and underwent several subsidiary examinations.3 Thus, in quality prenatal care services, it is expected that health professionals encourage vaginal delivery whenever there is no contraindication. However, consistently with national literature,8,14-16 in Piauí, the proportions of cesarean sections were higher among women who went to more prenatal care appointments. There are at least two reasons for this result. First, the higher number of appointments could be explained by the presence of diseases such as hypertension and diabetes - which, because of the high obstetric risk, would lead to a higher frequency of cesarean sections.6,29 Second, it is possible that some information provided by the physician during the prenatal period could influence pregnant women’s decision on the type of delivery when recommending the cesarean section as the safest option.10,11
We observed that municipalities with more than 300 thousand inhabitants and with higher M-HDI have a higher proportion of cesarean sections. On one hand, these data reflect the fact that hospitals located in more developed urban areas are usually better equipped and have more qualified healthcare teams, which are strong characteristics in performing surgical procedures. On the other hand, the lower frequency of cesarean sections in less populous and less developed areas, which are generally poorer, leads to the assumption that women with high obstetric risk have less access to surgical delivery, when necessary. National and international data support the idea that the socioeconomic characteristics of the women’s residence region are more determinant in the proportion of cesarean sections than the pregnant women’s individual and familiar socioeconomic factors.8,20
This study presents some limitations to be considered, especially related to the use of secondary data from the Information System on Live Births (Sinasc), due to its restrictions of coverage and quality.30 It is important to highlight that the research was limited to hospital childbirths of primiparous women. Due to the impossibility to assess the influence of previous cesarean sections when choosing the subsequent delivery method, we opted for including only primiparous women. Furthermore, the variables available in the database did not allow us to differentiate all situations that could determine cesarean sections, precluding the separation of cesarean sections by clinical indication from those carried out for convenience.
Even with those limitations, this is the first assessment study on the overview of child deliveries in Piauí covering a 12 year period. Factors related to deliveries of primiparous women should be prioritized regarding the approach and implementation of measures to decrease the frequency of cesarean sections repetition.
Although there is no knowledge on the ideal proportion of cesarean sections for each population, the amount of surgical deliveries has been considered excessive throughout the world. Data from Piauí support observations from other national studies, which demonstrate that, besides the increasing trends during the last decades, the proportion of cesarean sections are marked by social inequalities. In practice, it is likely that women who need cesarean sections the most lack the technology, and, on the other hand, its frequency may be abusive to women with less pregnancy risks. This scenario of delivery support can have an impact on the prevalence of high occurrence of maternal and fetal morbidity and mortality, both due to the lack or excess of cesarean sections.
There is a duality in the current model of childbirth care in Brazil. On one hand, the public health services are characterized by higher frequency of vaginal deliveries, generally with little pain control and more unnecessary interventions. On the other hand, the private health services display the cesarean sections as a practically universal type of delivery, with conveniently scheduled procedures, fastest type of delivery, and upheld as safer than vaginal delivery. If we consider that the cesarean section is an essential procedure in the obstetric care, which is capable of saving maternal and fetal lives when adequately recommended, the debate about equality of access to childbirth care should be centered on offering the cesarean section to women who really need it. The increasing proportion of cesarean sections and its highest occurrence among women with low obstetric risk in Piauí suggest the need for intervention focusing on health care professionals, women, and on the organization and structure of health services. Measures such as continuous medical education, quality prenatal care appointments and access to good practices during childbirth care can contribute to the decrease on the proportion of unnecessary cesarean sections.
Referências
1. Villar J, Valadares E, Wojdyla D, Zavaleta N, Carroli G, Velazco A, et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006 Jun;367(9525):1819-29. [ Links ]
2. World Health Organization. Appropriate technology for birth. Lancet. 1985 Aug;326(8452):436-7. [ Links ]
3. Victora CG, Aquino EML, Leal MC, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet 2011 May;377(9780):1863-76. [ Links ]
4. Ministério da Saúde (BR). Departamento de Informática do Sistema Único de Saúde [Internet]. Brasília: Ministério da Saúde; 2010 [citado 2015 jun 20]. Disponível em: Disponível em: http://www.datasus.gov.br . [ Links ]
5. Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol. 2012 Apr;206(4):331.e1-19. [ Links ]
6. Linwattananon S, Tangcharoensathien V, Sirilak S. Trends and inequities in where women delivered their babies in 25 low-income countries: evidence from Demographic and Health Surveys. Reprod Health Matters. 2011 May;19(11):75-85. [ Links ]
7. Kyu HH, Shannon HS, Georgiades K, Boyle MH. Caesarean delivery and neonatal mortality rates in 46 low- and middle-income countries: a propensity-score matching and meta-analysis of Demographic and Health Survey data. Int J Epidemiol. 2013 Jun;42(3):781-91. [ Links ]
8. Freitas PF, Drachler ML, Leite JC, Marshall T. Inequalities in cesarean delivery rates by ethnicity and hospital accessibility in Brazil. Int J Gynecol Obstet. 2009 Dec;107(3):198-201. [ Links ]
9. Patah LEM, Malik AM. Modelos de assistência ao parto e taxas de cesárea em diferentes países. Rev Saude Publica. 2011 fev;45(1):185-94. [ Links ]
10. Béhague DP, Victora CG, Barros FC. Consumer de¬mand for caesarean sections in Brazil: informed decision making, patient choice or social inequal¬ity? A population based birth cohort study linking ethnographic and epidemiological methods. BMJ. 2002 Apr;324(7343):942-5. [ Links ]
11. Domingues RMSM, Dias MAB, Nakamura-Pereira M, Torres JA, d’Orsi E, Pereira APE, et al. Processo de decisão pelo tipo de parto no Brasil: da preferência inicial das mulheres à via de parto final. Cad Saude Publica 2014;30 supl 1:101-16. [ Links ]
12. Faúndes A, Pádua KS, Osis MJD, Cecatti JG, Souza MH. Opinião de mulheres e médicos brasileiros sobre a preferência pela via de parto. Rev Saude Publica 2004 ago;38(4):488-94. [ Links ]
13. Potter JE, Berquó E, Perpétuo IHO, Leal OF, Hopkins K, Souza MR. Unwanted caesarean sections among public and private patients in Brazil: prospective study. BMJ. 2001 Nov;323(7322):1155-8. [ Links ]
14. Mendoza-Sassi RA, Cesar JA, Silva PR, Denardin G, Rodrigues MM. Risk factors for cesarean section by category of health service. Rev Saude Publica. 2010 Feb;44(1):80-9. [ Links ]
15. Rebelo F, Rocha CM, Cortes TR, Dutra CL, Kac G. High cesarean prevalence in a national population-based study in Brazil: the role of private practice. Acta Obstet Gynecol Scand. 2010 Jul;89(7):903-8. [ Links ]
16. Barros AJD, Santos IS, Matijasevich A, Domingues MR, Silveira M, Barros FC, et al. Patterns of deliveries in a Brazilian birth cohort: almost universal cesarean sections for the better-off. Rev Saude Publica. 2011 Aug;45(4):635-43. [ Links ]
17. Bettiol H, Rona RJ, Chinn S, Goldani M, Barbieri MA. Factors associated with preterm births in southeast Brazil: a comparison of two birth cohorts born 15 years apart. Paediatr Perinat Epidemiol. 2000 Jan;14(1):30-8. [ Links ]
18. Ye J, Betrán AP, Vela MG, Souza JP, Zhang J. Searching for the optimal rate of medically necessary cesarean delivery. Birth. 2014 Sep;41(3):237-44. [ Links ]
19. Althabe F, Sosa C, Belizán JM, Gibbons L, Jacquerioz F, Bergel E. Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: an ecological study. Birth. 2006 Dec;33(4):270-7. [ Links ]
20. Cavallaro FL, Cresswell JA, França GVA, Victora CG, Barros AJD, Ronsmans C. Trends in caesarean delivery by country and wealth quintile: cross-sectional surveys in southern Asia and sub-Saharan Africa. Bull World Health Organ. 2013 Dec;91(12):897-972. [ Links ]
21. Höfelmann DA. Tendência temporal de partos cesáreos no Brasil e suas regiões: 1994 a 2009. Epidemiol Serv Saude. 2012 out-dez;21(4):561-68. [ Links ]
22. Instituto Brasileiro de Geografia e Estatística. Estados: Piauí [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2015 [citado 2016 jun 14]. Disponível em: Disponível em: http://www.ibge.gov.br/estadosat/perfil.php?sigla=pi [ Links ]
23. Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003 Oct;3:21. [ Links ]
24. Ramires de Jesus G, Ramires de Jesus N, Peixoto-Filho FM, Lobato G. Caesarean section rates in Brazil: what is involved? BJOG. 2015 Apr;122(5):606-9. [ Links ]
25. Bayrampour H, Heaman M. Advanced maternal age and the risk of cesarean section: a systematic review. Birth . 2010 Sep;37(3):219-26. [ Links ]
26. Janoudi G, Kelly S, Yasseen A, Haman H, Moretti F, Walker M. Factors associated with increased rates of caesarean section in women of advanced maternal age. J Obstet Gynaecol Can. 2015 Jun;37(6):517-26. [ Links ]
27. Heffner LJ, Elkin E, Fretts RC. Impact of labor induction, gestational age, and maternal age on cesarean delivery rates. Obstet Gynecol. 2003 Aug;102(2):287-93. [ Links ]
28. Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetrical outcomes and care: prevalence and determinants. Am J Obstet Gynecol . 2010 Apr;202(4):335-43. [ Links ]
29. Edmonds JK, Yehezkel R, Liao X, Simas TA. Racial and ethnic differences in primary, unscheduled cesarean deliveries among low-risk primiparous women at an academic medical center: a retrospective cohort study. BMC Pregnancy Childbirth. 2013 Sep;13:168. [ Links ]
30. Oliveira MM, Andrade SSCA, Dimech GS, Oliveira JCG, Malta DC, Rabello Neto DL, et al. Avaliação do Sistema de Informações sobre Nascidos Vivos. Brasil, 2006-2010. Epidemiol Serv Saude. 2015 out-dez;24(4):629-40. [ Links ]
Received: February 21, 2016; Accepted: June 30, 2016











 texto em
texto em