Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2337-9622
Epidemiol. Serv. Saúde v.26 n.2 Brasília abr./jun. 2017
http://dx.doi.org/10.5123/s1679-49742017000200003
ORIGINAL ARTICLE
Syphilis in pregnancy and congenital syphilis in Palmas, Tocantins State, Brazil, 2007-2014*
1Centro Universitário Luterano de Palmas, Programa de Residência Multiprofissional em Saúde Coletiva com Ênfase em Vigilância em Saúde, Palmas-TO, Brasil
2Centro Universitário Luterano de Palmas, Departamento de Enfermagem e Saúde Coletiva,
3Universidade Federal do Tocantins, Departamento de Nutrição, Palmas-TO, Brasil
OBJECTIVE:
to describe the epidemiological profile of reported cases of syphilis in pregnant women and congenital syphilis in the period 2007-2014 in Palmas-TO, Brazil.
METHODS:
this is a descriptive study with data from the Information System for Notifiable Diseases (Sinan).
RESULTS:
171 pregnant women with syphilis (4.7/1,000 live births [LB]) and 204 cases of congenital syphilis (5.6/1,000 LB) were identified; most women were brown-skinned (71.3%), had low education level (48.0%) and received late diagnosis during prenatal care (71.9%); the incidence of congenital syphilis varied from 2.9 to 8.1/1,000 LB in the period; the predominant maternal characteristics were age from 20 to 34 years (73.5%), having up to complete high school (85.3%), attending prenatal care (81.4%), diagnosis of syphilis during prenatal care (48.0%), and untreated partners of mothers who attended prenatal care (83.0%), reaching almost 80% of live births with congenital syphilis.
CONCLUSION:
it is necessary to adopt new strategies for the effectiveness of the prenatal care provided, and, consequently, to reduce the incidence of congenital syphilis.
Keywords: Pregnant Women; Prenatal Care; Congenital Syphilis; Syphilis; Epidemiology, Descriptive
Introduction
Syphilis is still a serious Public Health issue, at global level, despite the availability of low-cost diagnostic methods and the effective treatment since the decade of 1950. The disease shows a scenario worse than the vertical transmission of human immunodeficiency virus (HIV) and is a determinant factor in the rise of maternal and perinatal morbidity and mortality indicators.1
In 2011, the World Health Organization (WHO) estimated that 2 million cases of syphilis in pregnant women occur each year. About 25% of untreated cases, or treated inappropriately, would result in miscarriage or stillbirths.2
Infection's surveillance of syphilis in pregnant women aims to meet the serological status and start maternal therapy early, aiming to strengthen planning and evaluation of prevention and control measures, particularly the vertical transmission of the Treponema pallidum.3
The effective control of syphilis has as its fundamental premise the serological screening and treatment of pregnant women and sexual partners, since the quality of prenatal and delivery assistance are important determinants in reducing mother-to-child transmission. Penicillin is the drug of first choice in the treatment of syphilis and the only indicated for pregnant women: it presents 98% effectiveness in preventing congenital syphilis, acting at all stages of the disease. There is no report on the resistance of Treponema pallidum to penicillin.3,4 Notwithstanding, the high incidence of syphilis in pregnant women and congenital syphilis are still a challenge to health services.
From 2007 to 2013, 685 cases of syphilis in pregnant women and 535 cases of congenital syphilis were registered in individuals resident in Tocantins State.5 According to an agreement between the Ministry of Health and the Pan-American Health Organization (PAHO), the target for 2015 was to reduce the incidence to 0.5 cases per 1,000 live births.1,3
Primary Health Care is essential in tackling congenital syphilis, since it is the main entrance to health services. Family Health teams are the closest bond between the health professional and the patient and may help change the epidemiological picture of this disease. The professionals who work directly with pregnant women need technical qualification and an interdisciplinary look, given the difficulties in diagnosis and assistance for this disease.4
In Brazil, there are several discussions over this subject. However, there are few studies on the epidemiological characteristics of congenital syphilis in several places.6 This fact justifies the conduction of studies that may contribute to a better knowledge and understanding of syphilis epidemiology, enabling a (i) better planning of education and prevention measures in most vulnerable groups and (ii) assessment of the action to reduce the mother-to-child transmission of syphilis.
This study aimed to describe the epidemiological profile of reported cases of syphilis in pregnant women and congenital syphilis in the period 2007-2014 in Palmas, Tocantins State, Brazil.
Methods
This is a descriptive study with data from the Information System for Notifiable Diseases (Sinan), which is fed by forms of compulsory notification; these files are standardized forms that contain sociodemographic and clinical information, and are filled in by health professionals.
The place of study was Palmas, the capital of Tocantins State, located in the central region of that state; it occupies an area of 2,218.943 km² and, in 2015, it had a population of 272,726.7
We included in this study all the cases of syphilis during pregnancy and congenital syphilis in residents of Palmas, registered on Sinan, from 2007 to 2014, which fit the definition criterion of confirmed case, according to the Brazilian Ministry of Health.8 The duplicate cases identified after analysis on Sinan were excluded. The variables studied were related to the notification files of syphilis during pregnancy and congenital syphilis, as follows:
a) Maternal sociodemographic
- age (in years: 10 to 14; 15 to 19; 20 to 34; 35 to 49)
- ethnicity/skin color (white; black; Asian; brown; indigenous)
- education level (illiterate; 1st to 4th grade of elementary school incomplete; 4th grade of elementary school complete; 5th to 8th grade of elementary school incomplete; complete elementary school; incomplete high school; higher education degree; unknown)
b) Prenatal care (yes; no; unknown/blank)
c) Obstetric and treatment
- moment of maternal diagnosis (1st, 2nd, 3rd trimester or gestational age ignored)
- clinical classification of the disease (primary; secondary; tertiary; latent; unknown/blank)
- treponemal test (reactive; nonreactive; not conducted; unknown/blank)
- nontreponemal test (reactive; nonreactive; not conducted)
- treatment scheme prescribed to the pregnant woman (penicillin G benzathine 2,400,000 IU; penicillin G benzathine 4,800,000 IU; penicillin G benzathine 7,200,000 IU; other scheme; not conducted; unknown/blank)
- partner’s treatment (yes; no; unknown/blank)
d) Newborn’s clinical and laboratory information
- VDRL test (venereal disease research laboratory) in peripheral blood (positive, negative, not conducted, unknown/blank)
- CSF VDRL test (positive; negative; not conducted, unknown/blank)
- long bone radiography (yes; no; not conducted; unknown/blank)
- case evolution (alive; death due to congenital syphilis; death due to other causes; miscarriage; stillbirths)
To calculate the prevalence rate of syphilis during pregnancy, we used the number of notified cases per year, divided by the number of live births in the same year, multiplied by 1,000. To calculate the incidence of congenital syphilis, we used the number of new cases per year, divided by the number of live births in the same year, multiplied by 1,000.9 The number of live births was obtained at the Information System on Live Births (Sinasc).
The statistics softwares - open distribution - used to conduct the analyses were BioEstat 5.0 and Epi Info 3.5.2; data were tabulated with Tabwin 32.
The research project was approved by the Ethics in Research Committee of the Centro Universitário Luterano de Palmas, under the report No. 985.502, dated March 13th, 2015; the project was conducted according to the Resolution of the National Health Council (CNS) No. 466, dated December 12th, 2012.
Results
From 2007 to 2014, 171 cases of syphilis in pregnant women and 204 cases of congenital syphilis were identified. The year of 2014 presented the highest number of notified cases of syphilis in pregnant women (n=39; 23.0%), with a prevalence rate of 7.5/1,000 live births (Figure 1), which is equivalent to an increase of 38.8% when compared to the previous year and of 78.5% in relation the average of the previous years (4.2/1,000 live births).
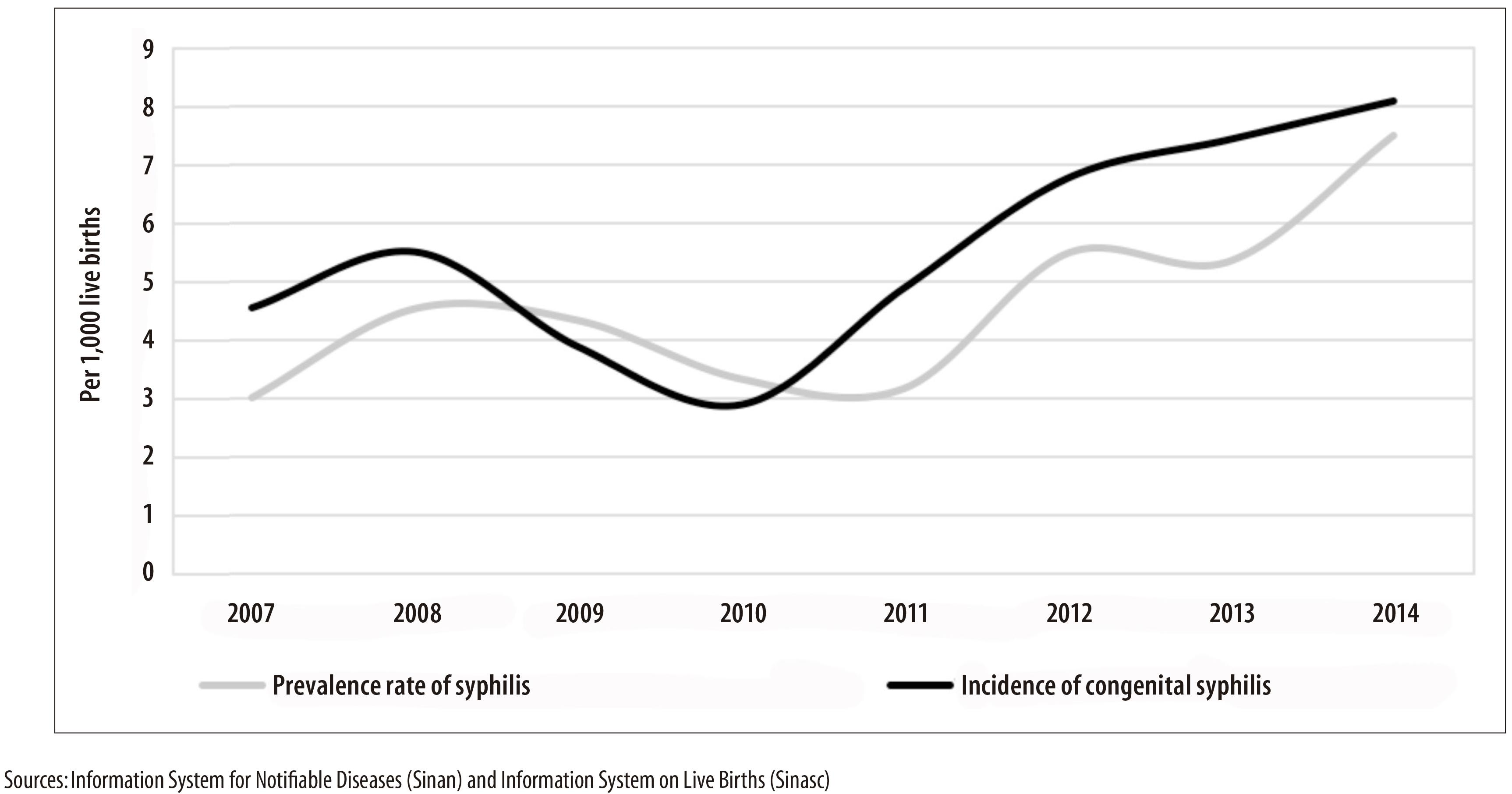
Figure 1 - Annual incidence of congenital syphilis and prevalence rate of syphilis during pregnancy (per 1,000 live births) in the municipality of Palmas, Tocantins, 2007-2014
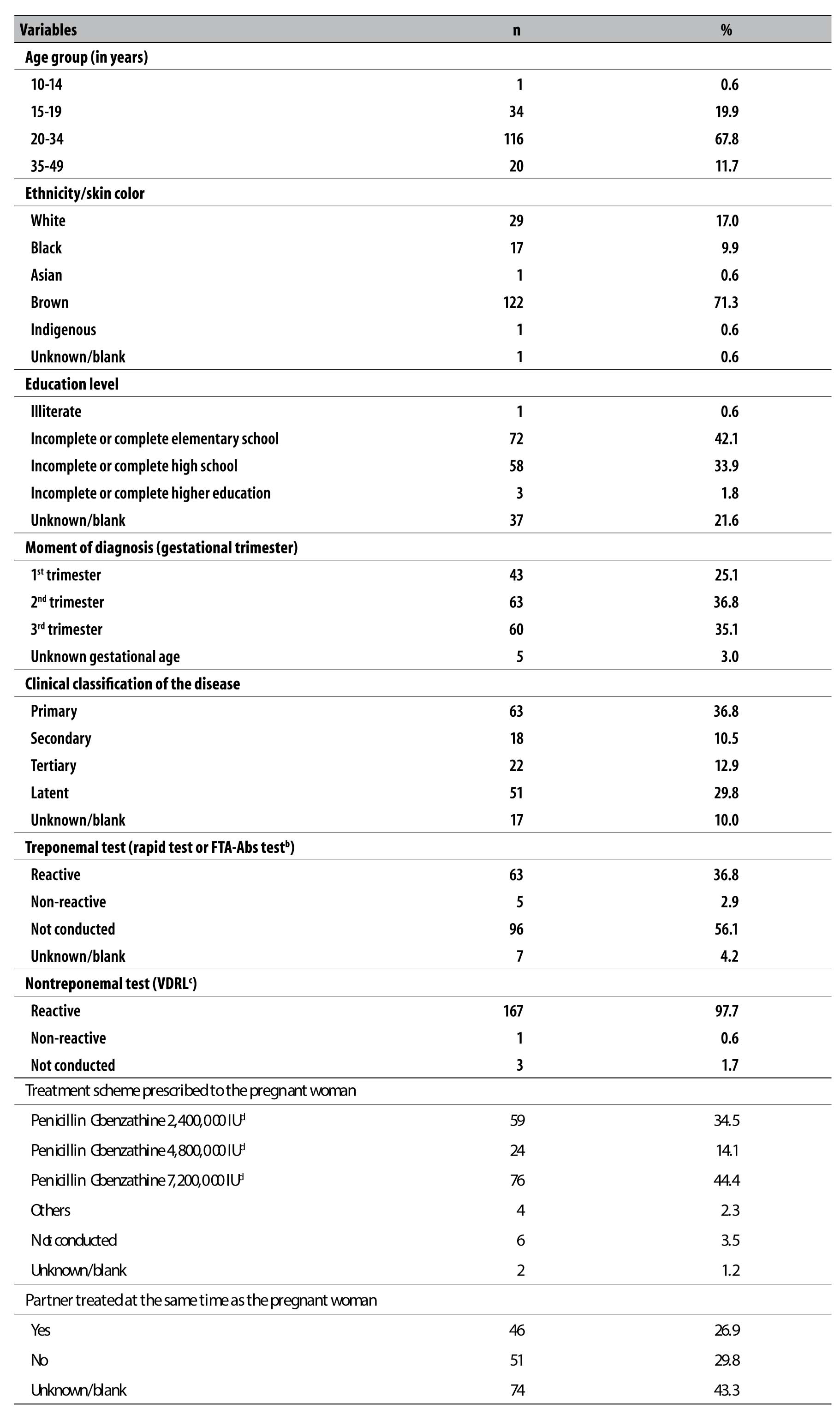
The majority of the 116 pregnant women with syphilis (67.8%) were in the age group of 20-34 years old (average age of 25 years; range from 13 to 43 years) (Table 1). More than two thirds of those women (71.3%) were brown-skinned and 76.0% had from incomplete elementary school to complete high school. In 51 (29.8%) cases, the partner did not receive treatment (Table 1).
Table 1 - Distribution of pregnant women with syphilis (n=171), according to sociodemographic, obstetric, and partners’ information, notified on Sinana in the municipality of Palmas, Tocantins, 2007-2014
a) Sinan: Information System for Notifiable Diseases
b) Fluorescent treponemal antibody-absorption
c) VDRL: Venereal disease research laboratory
d) International Units
In 47.3% of the cases syphilis was primary and/or secondary. In 93.0% of cases, we could identify the VDRL test, which varied between 1:1 and 1:128, with median of 1:4 and mode of 1:2. In 11 (7.0%) cases, the VDRL was informed with inexistent titles.
Of the 167 pregnant women with positive VDRL, 36.8% tested positive in the treponemal test (fluorescent treponemal antibody-absorption [FTA-ABS]); and 2.9% tested negative, being, thus, discarded for syphilis.
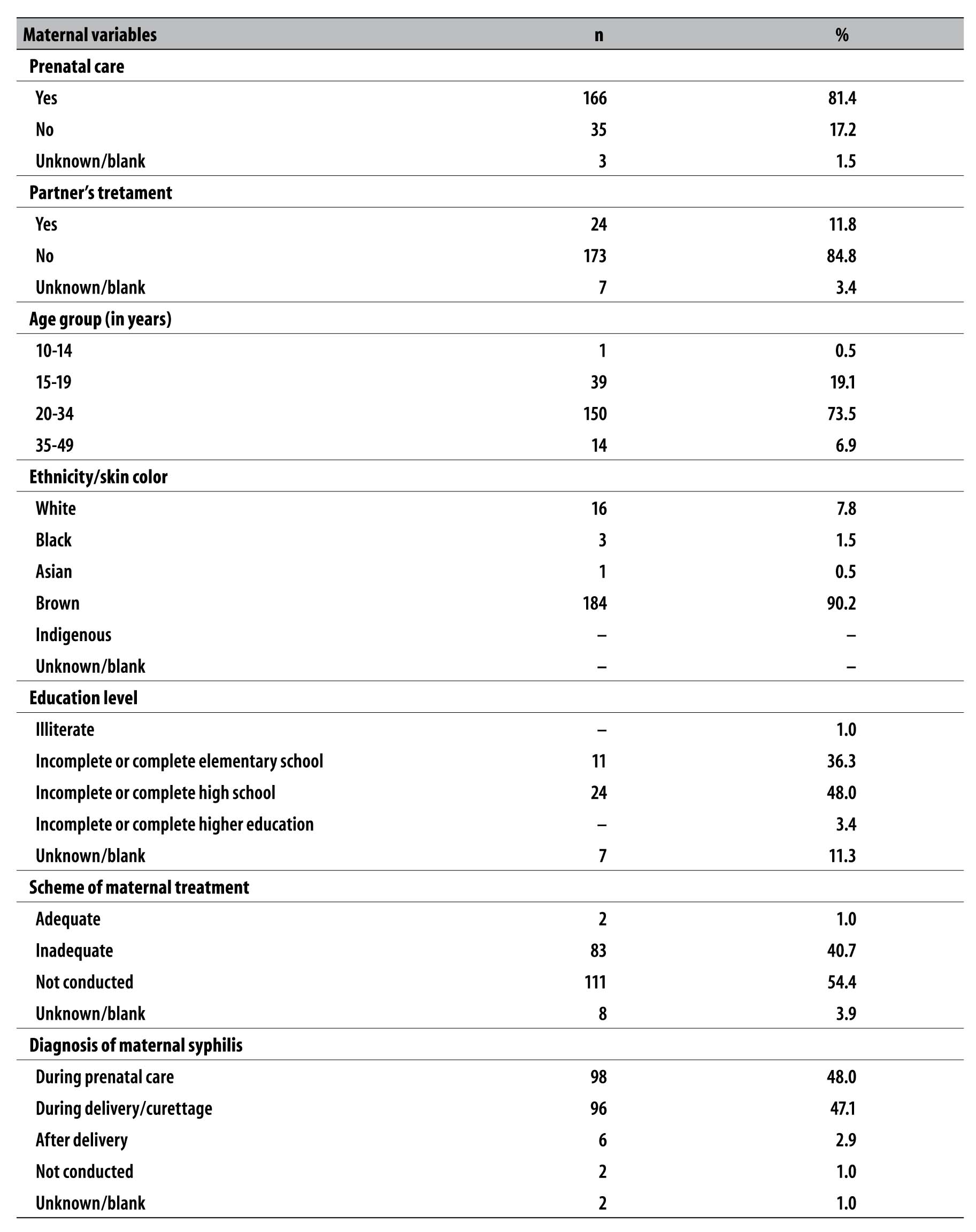
From 2007 to 2014, the annual incidence rate of congenital syphilis raised from 2.9 to 8.1 cases per 1,000 live births. Among the mothers of cases that fit into the criteria of definition for congenital syphilis, most were brown-skinned (90.2%), in the age group from 20 to 34 years old (73.5%), with incomplete or complete high school (48.0%) (Table 2).
Table 2 - Sociodemographic and clinical characteristics of mothers of live births with congenital syphilis (n=204), notified on Sinana in the municipality of Palmas, Tocantins, 2007-2014
a) Sinan: Information System for Notifiable Diseases
Of the total of cases of congenital syphilis, 81.4% of the mothers attended prenatal care during pregnancy and 48.0% were diagnosed during prenatal care (Table 2). The partners of 83.0% of the mothers who attended prenatal care were not treated for the disease.
Most of mothers of notified cases of congenital syphilis did not receive treatment (54.4%), and many of them received inadequate treatment (40.7%). The performance of adequate treatment for pregnant women during the historical series was low (1.0%) (Table 2).
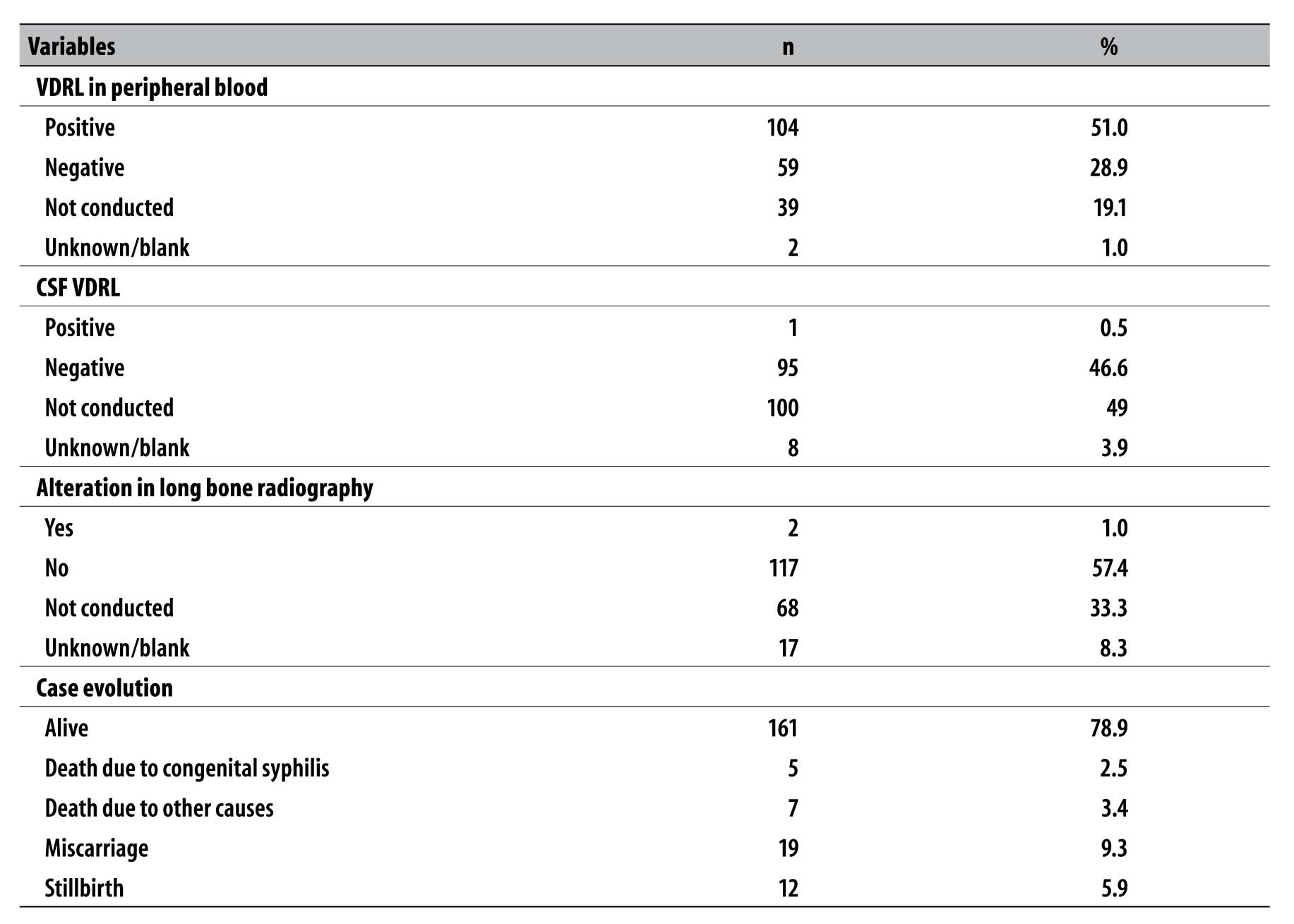
Among the live births with congenital syphilis, 51.0% presented VDRL in peripheral blood positive and only 1.0% presented changes in the long bone radiography; however, this latter was not performed in 68 cases (33.3%) (Table 3).
Table 3 - Diagnosis characteristics of cases of congenital syphilis (n=204), notified on Sinana in the municipality of Palmas, Tocantins, 2007-2014
a) Sinan: Information System for Notifiable Diseases
b) VDRL: venereal disease research laboratory
By analyzing the evolution of cases of congenital syphilis, we could observe: 78.9% of cases were alive; 2.5% died due to syphilis; 3.4% died due to other causes; 9.3% were miscarriages; and 5.9% were stillbirths (Table 3).
Discussion
An increase in the prevalence of syphilis during pregnancy and raising incidence of congenital syphilis were observed in Palmas-TO, Brazil. This increase has also been reported in other Brazilian municipalities9 and around the world.10 Women with syphilis are mainly young, brown-skinned, with low education level and who attended prenatal care, a profile similar to other studies.11-15
It is important to highlight that the low education level is considered a marker of greater risk of exposition to sexually transmitted diseases, due to the little knowledge on the importance of prevention.16 In this study, we can notice that most of mothers of notified infants had low education level. This finding is similar to a research conducted between 2010 and 2013, in Belo Horizonte, capital of Minas Gerais State,17 and to results of other studies that confirmed higher occurrence of syphilis in pregnant women with low education level.12,13,18
We could also observe a high frequency of syphilis diagnosis in the 2nd and 3rd trimesters of pregnancy,19 possibly related to the (i) late search for prenatal care and (ii) low sensibility and quality of pregnant women health care. These results reaffirm the importance of the timely detection of cases of syphilis in pregnant women, as well as the offer of correct treatment for those women and their partners: the adequate prenatal care is essential for the maternal-infant health and, consequently, for the reduction of congenital syphilis. Similar results were found in some studies conducted in municipalities from the states of Rio de Janeiro (1994 to 1999), and Ceará (2000 to 2005), as well as in the Federal District (2005 to 2009).18,19,20 The improvement in timely diagnose in pregnant women from Palmas may be related to the implementation of rapid tests in the primary health care units (PHU), since 2013.21
According to the Ministry of Health, there are some difficulties in the clinical diagnose for syphilis in pregnant women, because the chancre does not present symptoms and is usually located in areas of limited view: vaginal wall, cervix or perineum.22 This study showed that many pregnant women were misclassified, regarding the disease stage, given the high number of women on the primary and tertiary stages, which is different from what is expected during screening, when the latent stage is more common.22 It is important to highlight that the mistakes in interpretations and classification of the clinical stage of syphilis may lead to inadequate treatments, and cases in which it is not possible to find out the evolution of the disease or those with absence of clinical signs, must be classified as of syphilis with unknown duration, and, in those cases, the treatment advised are three doses of benzathine penicillin.3,22
In São Paulo, 40% of congenital syphilis cases lead to fetal death (miscarriage, stillbirths) or early neonate death.23 In this study, in almost one fifth of miscarriage cases, mothers were diagnosed with syphilis only during delivery and curettage. For almost all live births (symptomatic or not), the mothers were diagnosed during prenatal care, which proves that prenatal care enables a more favorable outcome of cases.
In Palmas, we observed a high percentage of exams not performed on newborns with congenital syphilis (CSF VDRL test and long bone radiography). The long bone radiography may offer diagnose assistance and present, as more frequent alteration, periostitis, osteomyelitis and osteochondritis.22,24 Other studies conducted in Belo Horizonte-MG, Caxias do Sul-RS and Natal-RN, from 2001 to 2013,17,25,26 also observed a prevalence of information absence regarding the radiological diagnosis and the CSF VDRL test, which may hamper the effective follow-up of cases.
This study presented some limitations, which are common in researches with secondary data - limited to coverage and registers quality -, given the possibility of underreporting and the low quality of the information registered.
The results presented help understand the fragility of health services, regarding the control of congenital syphilis. Several important failures were found, with influence over diagnose and follow-up, for both the pregnant women during prenatal care, and the infants, and the non- compliance of an adequate treatment for the mothers and their partners stands out.
The Primary Health Care is essential in tackling the vertical transmission of syphilis, considering it is the main entrance to health services, whilst the Family Health teams are the closest bond between the health professional and the patient, and can help change the epidemiological picture of congenital syphilis. Health professionals who work directly with pregnant women need to get involved with the cause, besides receiving technical qualification and having an interdisciplinary look, given the difficulties in diagnosis and assistance for this disease. The health professionals should be aware, in order to minimize a totally avoidable risk with timely diagnose, adequate treatment and education in health for pregnant women and their partners.
REFERENCES
1. Organización Pan-Americana de la Salud. Análisis de la situación al año 2010: eliminación de la transmisión maternoinfantil del VIH y de la sífilis congénita en la Región de las Américas [Internet]. Washington: Organización Pan-Americana de la Salud; 2012 [citado 2016 dic 19]. Disponible en: http://www.paho.org/clap/index.php?option=com_docman&task=doc_download&gid=273&Itemid= [ Links ]
2. World Health Organization. Methods for surveillance and monitoring of congenital syphilis elimination within existing systems. Geneva: World Health Organization; 2011 [ Links ]
3. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para prevenção da transmissão vertical de HIV, sífilis e hepatites virais. Brasília: Ministério da Saúde; 2015. 120 p. [ Links ]
4. Grumach AS, Matida LH, Heukelbach J, Coêlho HLL, Ramos Júnior AN. A (des)Informação relativa à aplicação da penicilina na rede do sistema de saúde do Brasil: o caso da sífilis. J Bras Doencas Sex Transm. 2007:19(3-4):120-7. [ Links ]
5. Ministério da Saúde (BR). Departamento de Informática do SUS [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2016 dez 19]. Disponível em: Disponível em: http://datasus.gov.br [ Links ]
6. Silva LSR, Rocha SS, Silva TA, Andrade WL, Silva WMP. Análise dos casos de sífilis congênita nos últimos 20 anos: uma revisão da Literatura. In: Anais do 18º Congresso Brasileiro dos Conselhos de Enfermagem. 2015 set 15-18; João Pessoa. Brasília: Conselho Federal de Enfermagem; 2015. [ Links ]
7. Instituto Brasileiro de Geografia e Estatística. Cidades@ [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2016 [citado 2016 dez 19]. Disponível em: http://www.cidades.ibge.gov.br/xtras/perfil.php?lang=&codmun=172100&search=tocantins|palmas [ Links ]
8. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Programa Nacional de DST e Aids. Diretrizes para controle da sífilis congênita. Brasília: Ministério da Saúde; 2005. 72p. (Manuais; 62) [ Links ]
9. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de DST, Aids e Hepatites Virais. Bol Epidemiol Sif. 2015;4(1):1-28 [ Links ]
10. Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis: United States of America, 2012-2014. MMWR Morb Mortal Wkly Rep. 2015 Nov;64(44):1241-5. [ Links ]
11. Campos ALA, Araujo MAL, Melo SP, Goncalves MLC. Epidemiologia da sífilis gestacional em Fortaleza, Ceará, Brasil: um agravo sem controle. Cad Saude Publica. 2010 set;26(9):1747-55. [ Links ]
12. Gonzales GF, Tapia V, Serruya SJ. Sífilis gestacional y factores asociados en hospitales públicos del Perú en el periodo 2000-2010. Rev Peru Med Exp Salud Publica. 2014 Apr;31(2):211-21. [ Links ]
13. Lima MG, Santos RFR, Barbosa GJA, Ribeiro GS. Incidência e fatores de risco para sífilis congênita em Belo Horizonte, Minas Gerais, 2001-2008. Cien Saude Colet. 2013 fev;18(2):499-506. [ Links ]
14. Carvalho IS, Brito RS. Sífilis congênita no Rio Grande do Norte: estudo descritivo do período 2007-2010. Epidemiol Serv Saude. 2014 jun; 23(2):287-94. [ Links ]
15. Almeida MFG, Pereira SM. Caracterização epidemiológica da sífilis congênita no município de Salvador, Bahia. DST - J Bras Doencas Sex Transm. 2007;19(3-4):144-56. [ Links ]
16. Serafim AS, Moretti GP, Serafim GS, Niero CV, Rosa MI, Pires MMS, et al. Incidence of congenital syphilis in the South Region of Brazil. Rev Soc Bras Med Trop. 2014 Apr;47(2):170-8. [ Links ]
17. Nonato SM, Melo APS, Guimarães MDC. Sífilis na gestação e fatores associados à sífilis congênita em Belo Horizonte-MG, 2010-2013. Epidemiol Serv Saude. 2015 out-dez;24(4):681-94. [ Links ]
18. Sá RAM, Bornia RBG, Cunha AA, Oliveira CA, Rocha GPG, Giordano EB. Sífilis e gravidez: avaliação da prevalência e fatores de risco nas gestantes atendidas na Maternidade Escola - UFRJ. DST -J Bras Doencas Sex Transm. 2001;13(4):6-8. [ Links ]
19. Araújo MAL, Silva DMA, Silva RM, Gonçalves MLC. Análise da qualidade dos registros nos prontuários de gestantes com exame de VDRL reagente. Rev APS. 2008 jan-mar;11(1):4-9. [ Links ]
20. Leitão EJL, Canedo MCM, Furiatti MF, Oliveira LRS, Diener LS, Lobo MP, et al. Sífilis gestacional como indicador da qualidade do pré-natal no Centro de Saúde n.º 2 Samambaia-DF. Com Cienc Saude. 2009;20(4):307-14. [ Links ]
21. Secretaria Municipal de Saúde (Palmas). Diretoria de Vigilância em Saúde. Área Técnica DST, Aids e Hepatites Virais. Bol Epidemiol HIVAids Síf Hep Virais. 2015 jan-dez;1(1):1-33 [ Links ]
22. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para atenção integral às pessoas com infecções sexualmente transmissíveis. Brasília: Ministério da Saúde; 2015. [ Links ]
23. Secretaria de Estado da Saúde (São Paulo). Coordenadoria de Controle de Doenças. Centro de Referência e Treinamento DST/Aids - SP. Programa Estadual DST/Aids de São Paulo. Guia de bolso para manejo da sífilis em gestantes e sífilis congênita. 2. ed. São Paulo: Secretaria de Estado da Saúde; 2016. [ Links ]
24. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Programa Nacional de DST e Aids. Protocolo para a prevenção de transmissão vertical de HIV e sífilis: manual de bolso. Brasília: Ministério da Saúde; 2007. 180p. (Série B. textos básicos de saúde) ; (Série manuais; vol. 80) [ Links ]
25. Lorenzi DRS, Madi JM. Sífilis congênita como indicador de assistência pré-natal. RBGO. 2001 nov-dez;23(10):647-52. [ Links ]
26. Holanda MTCG, Barreto MA, Machado KMM, Pereira RC. Perfil epidemiológico da sífilis congênita no Município do Natal, Rio Grande do Norte - 2004 a 2007. Epidemiol Serv Saude. 2011 abr-jun;20(2):203-12. [ Links ]
* This article is part of the Final Project of the Multiprofessional Residency in Public Health with emphasis in Health Surveillance, by Patrícia Alves de Mendonça Cavalcante, presented to the Fundação Escola de Saúde Pública e Centro Universitário Luterano de Palmas, in 2015. This study was funded by the Fundação Escola de Saúde Pública/Fundo Municipal de Saúde: Report No. 413017193.
Received: April 21, 2016; Accepted: November 30, 2016











 texto en
texto en 


