Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2337-9622
Epidemiol. Serv. Saúde v.26 n.2 Brasília abr./jun. 2017
http://dx.doi.org/10.5123/s1679-49742017000200005
ORIGINAL ARTICLE
Census of the Primary Health Care structure in Brazil (2012): potential coverage estimates*
1Universidade de Brasília, Área de Medicina Social da Faculdade de Medicina, Brasília-DF, Brasil
2Ministério da Saúde, Secretaria de Vigilância em Saúde, Brasília-DF, Brasil
OBJECTIVE:
to estimate and discuss selected indicators of Primary Health Care (PHC) structure in Brazil in 2012.
METHODS:
a descriptive ecological study was carried out using Primary Health Care Centre census data from the National Program for Access and Quality Improvement in Primary Care (PMAQ-AB); potential coverage indicators were estimated for infrastructure, health team composition and services available.
RESULTS:
the results revealed high coverage (≥70%) in Brazil for Community Health Agents (87.6%), teams providing care 5 days or more a week (71.4%), in 2 or more daily periods (70%), with nursing care services (70.9%) and dressing changes (70.4%); on the other hand, coverage is still poor (≤30%) for teams in health centres with adequate external signage (25.4%), delivering care at the weekend (28.4%) and reception of service users by health professionals (10.4%).
CONCLUSION:
the findings of this study point to the great inequalities between Brazilian states in potential coverage as shown by APS structure indicators.
Keywords: Health Evaluation; Structure of Services; Primary Health Care
Introduction
Primary Health Care (PHC) is characterized as the preferential gateway to the health care system, receiving patients and promoting the linking and accountability for the care of their health needs.1 The establishment of mechanisms that ensure the accessibility and reception presuppose a logic for organization and operation of the adequate PHC for the national diversity.1
Since the last decades in Brazil, we can identify many initiatives of the Ministry of Health for the institutionalization of the PHC evaluation.2 Among the most recent, there is the National Program for Access and Quality Improvement in Primary Care (PMAQ-AB),3 introduced in 2011, under the scope of the National Primary Care Policy (PNAB).1 The first cycle of the PMAQ-AB, carried out in 2012, registered an accession of 70% of Brazilian municipalities and included the completion of a census of the structure and organization of PHC services in national territory.
Based on the conceptual milestone of Bárbara Starfield,4 we understand a service provider of PHC when it exhibits four essential features:
i) First contact accessibility between the individual and health care system
ii) Longitudinality
iii) Integrity
iv) Coordination of care
In this scenario, the concept of quality is, therefore, relative and complex and, to a certain extent, demands successive redefinitions.4 Its meaning varies according to historical, political, economic and cultural context and scientific knowledge acquired by a society,5 in which the different points of view of people engaged in health care must be considered.6 Most studies performed in this area have been based on the Donabedian referential, which claims that one of the elements for evaluation of quality is the structure of services, in other words: given a good structure, a better service is more probable (although not certain) of occurring.7
The present study’s objective is to evaluate the indicators of structure of the Primary Health Care - PHC - in Brazil and in the federated unities (FU), in the year of 2012.
Methods
We carried out a research for evaluating coverage, upon outlining of ecological description, whose analysis units were 5,543 (99.5%) Brazilian municipalities (27 [0.5%] of the municipalities denied participation in the study) in the year of 2012. Data from the national base were obtained from the primary healthcare units (PHU) census, carried out by the PMAQ-AB. The national coordination of the project was appointed to the Primary Health Care Department of the Health Care Secretariat of the Ministry of Health, in partnership with education and research institutions from across the country.3
The data collection was managed by consortia formed by the following teaching and research institutions. One of the partner institutions in the consortium coordinated by the University of Pelotas (UFPel) was the University of Brasília (UnB). The project’s coordination in Distrito Federal was entitled to the researcher and first author of this study. Supervisor and interviewer teams used pre-tested data collection instruments constituted of three modules. Module I observed in loco aspects related to infrastructural conditions of PHU (census of structure). Module II characterized the organization of services and the work process, through interviews conducted with health care professional; and Module III consisted of interviews with users about their satisfaction regarding basic health care services. The present analysis make use of results from module I.
The study variables are related to each PHC team described by the census, and were grouped into three subdimensions: infrastructure, composition of the team and available services.
I. Subdimensions of infrastructure
Addresses the number of teams active in PHU that possesses:
i) service available 5 days a week or more, with 2 or more shifts, for 8 hours a day or more, during lunchtime, on weekends and have a vehicle available for external activities;
ii) ‘adequate’ accessibility for people with disabilities, which requires a sidewalk in good condition, or carpet, or non-slip floor, or regular floor, or smooth floor, or an access ramp, or handrail, or entrance door and corridor adapted for wheelchairs;
iii) ‘adequate’ visual identification, which requires disclosure of at least one of the following items to users:
- participation in the Program ‘Saúde Mais Perto de Você’;
- opening hours;
- listing of activities;
- available services;
- schedule of the professionals;
- phone number of the Ministry of Health’s ombudsman;
iv) ‘adequate’ internal signage, with identification of provided services; and
v) ‘adequate’ external signage, which requires the presence of an external totem signage the unit or a sign on the PHU’s façade according to the criteria established by the Ministry of Health.
II. Subdimension of the PHC’s team composition
Addresses the number of teams, which are/have:
i) Family Health Strategy (FHS);
ii) the minimal composition of the FHS teams - doctor, nurse, nursing assitant or technician, and community health agent (CHA);
iii) the minimum composition of the FHS teams - doctor, nurse, nursing assitant or technician, and community health agent (CHA). In addition to these professionals, there are the ones in charge of reception;
iv) parameterized PHC teams, organized differently than the FHS teams and that, to adhere to the PMAQ-AB, meet the set of parameters required by the Ministry of Health;3 and
v) Teams with other configurations, that are not organized like the FHS or the parameterized PHC teams.
III. Subdimension of available services
Addresses the number of teams with selected and available PHC services, which are:
- nursing appointments;
- dressing procedures;
- medical appointments;
- vaccination;
- dispensation of medications by the pharmacy;
- dental appointments; and
- receptivity.
We estimated coverage indicators (%) for Brazil and each federated state. In this study, the concept of coverage refers to potential coverage, as suggested by Soberón in Vieira-da-Silva, that is: coverage corresponding to the capacity and possibility of supply.8
The potential coverage was estimated as the percentage of population that would potentially be covered by a determined PHC service, considering the reference of 3,000 people for each team. This reference is based on the average of people to receive care for each FHS, according to the recommendation of the Ministry of Health.1 To estimate the coverage for the CHA, we considered the reference of one CHA for each 750 people, criterion also established by the Ministry of Health in the National Primary Care Policy (PNAB).1 The medians, and the 1st and 3rd quartiles, of the potential coverage were calculated based on the separatrices (quartiles) of observed distribution for the 27 federated unities. The results were presented in tables and box plots.
To summarize the indicators, we considered low coverages (lower than 30%), intermediary (30 to 69.9%) and high (70% or more).9
The tabulations, figures and analyses were done using the programs Microsoft Office Excel 2007 and Statistics Data Analysis (Stata) version 11.2.
The project for the study, respresentative of a stage in the PMAQ-AB, was approved by the Ethics Commitee in Research of the Medical Faculty of the University of Pelotas: 038/12 CEP/FAMED/UFPel.
Results
In 2012, we identified 38,812 PHU and a total of 49,331 active PHC teams in Brazil, distributed as follows: 39,045 FHS teams (79.1%), 5,459 parameterized PHC teams (11.1%) and 4,827 teams with other configurations (9.8%). These results allowed us to estimate coverages for the PHC of 76.3% of the population, and for FHS, 60.4% of the population (Table 1).
Table 1 - Distribution of potential coverages of indicators of structure available in the Primary Health Care of federated unities, Brazil, 2012
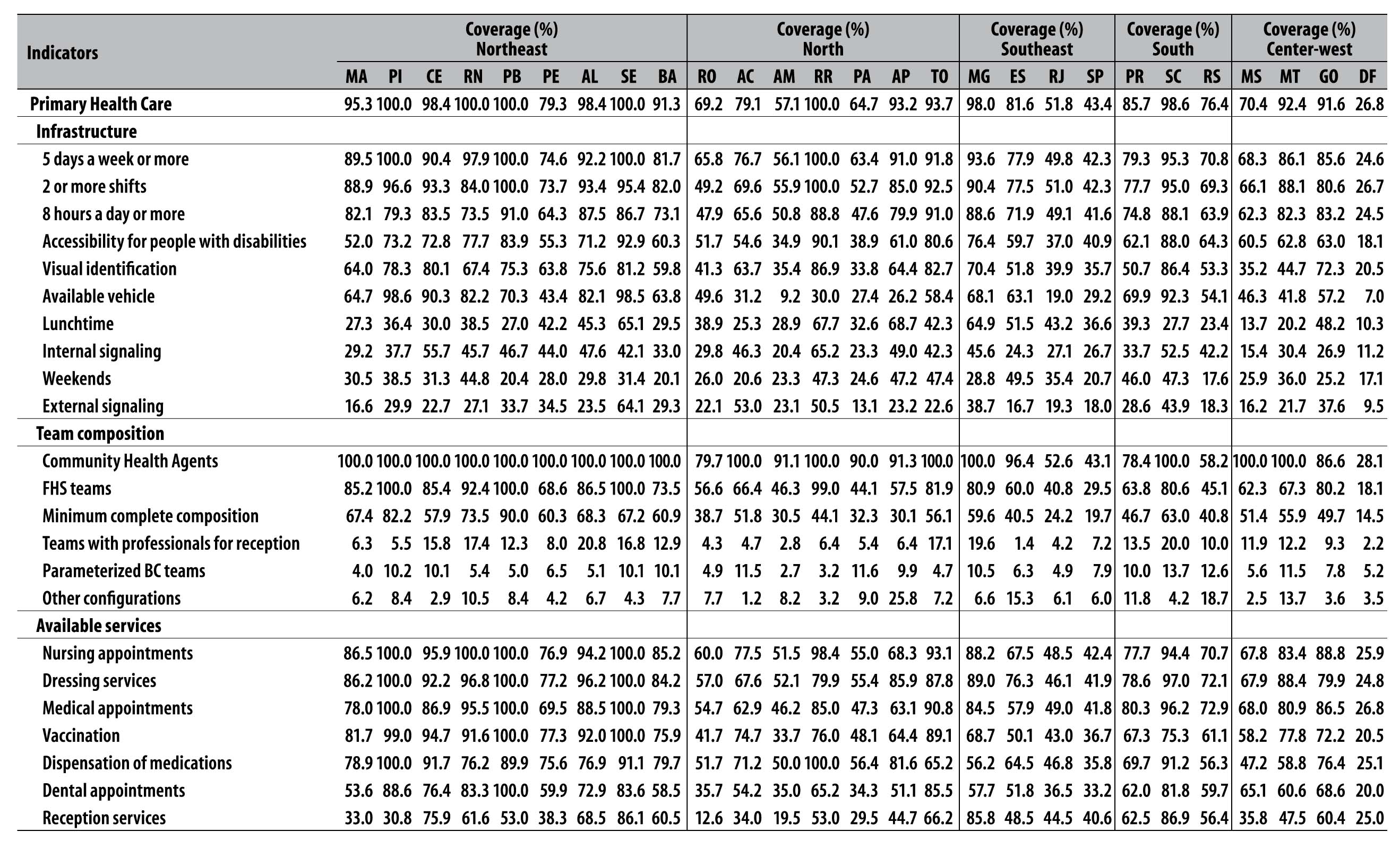
Note: the sum of ‘FHS teams + Parameterized BC teams + Other configurations’ corresponds to the BC coverage. Eventually, this sum is over 100% due to the use of a population base of 3,000 for its estimate. All values that exceeded 100 were adjusted in order to present a maximum limit of 100.0. To calculate the coverage of the Community Health Agents (CHA), we considered the parameter of 1 CHA for 750 people.
Higher coverage was identified for CHA services (87.6%), for teams with service available five days a week or more (71.4%), with two or more shifts (70.0%), with available nursing appointments (70.9%) and with dressing procedure (70.4%). On the other hand, still incipient coverages were observed for teams in PHU with an adequate external signage (25.4%), with service on weekends (28.4%) and whose minimal team composition had professionals for reception (10.4%) (Table 2).
Table 2 - Distribution of potential coverage of indicators of structure available in the Primary Health Care of federated unities, Brazil, 2012
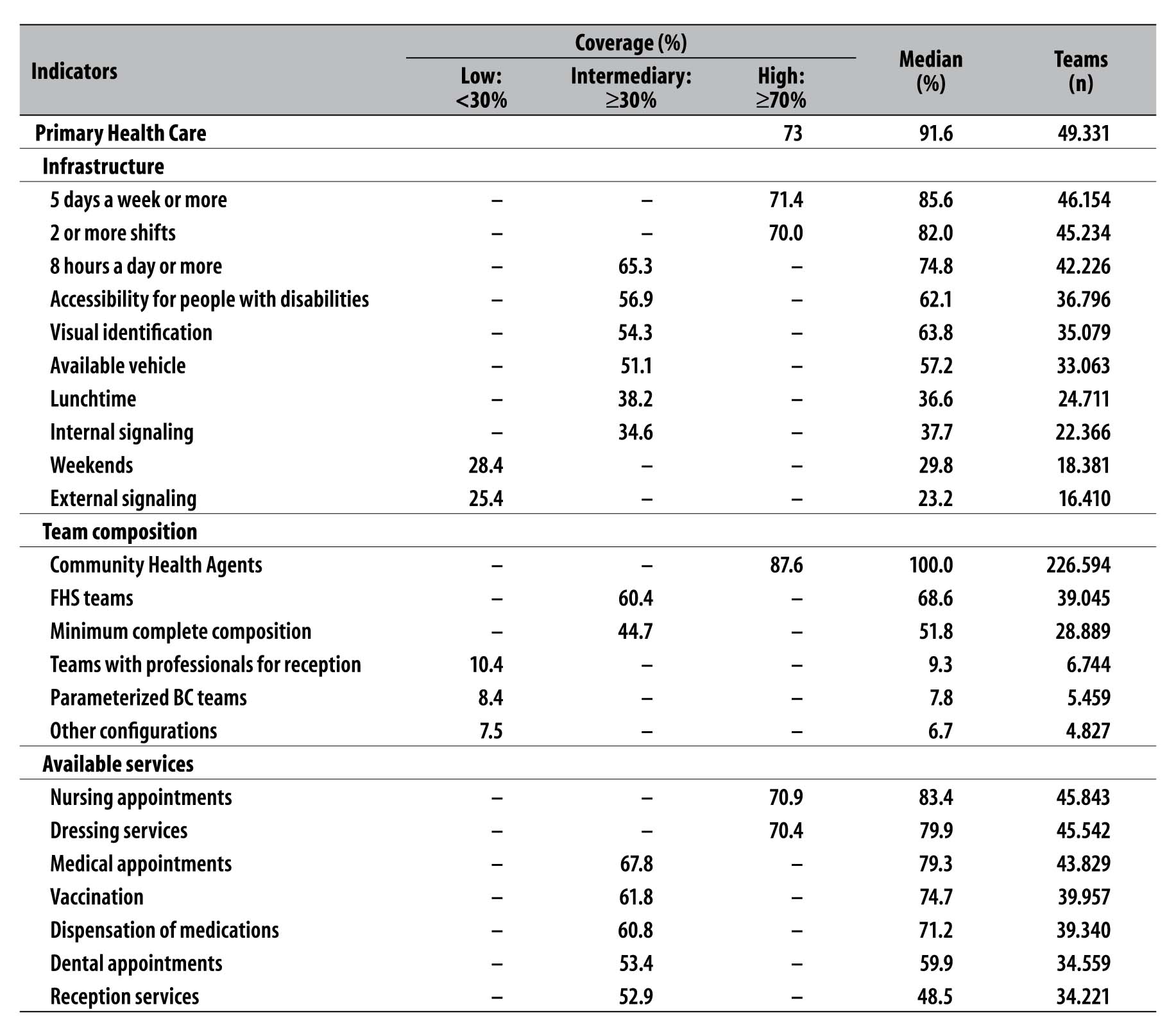
Note: to synthesize the different indicators, the coverage of federation unities were considered low (<30%), intermediary (30-69%) and high (≥70%).
Indicators of infrastructure
Among the 49,331 PHC teams identified in Brazil, a total of 46,154 stated having service available five days a week or more (Table 2 and Figure 1). The coverage for teams with that infrastructure was estimated to be 71.4%, varying from 24.6% in Distrito Federal to 100.0% in Roraima, Piauí, Paraíba and Sergipe states. Regarding service by PHC teams that offered two or more shifts (n=45,234 teams), the coverage was 70.0%, varying from 26.7% in Distrito Federal to 100.0% in Roraima and Paraíba states. The coverage for teams with service available for eight hours a day or more (n=42,226 teams) was 65.3%, varying from 24.5% in Distrito Federal to 91.0% in Tocantins state.
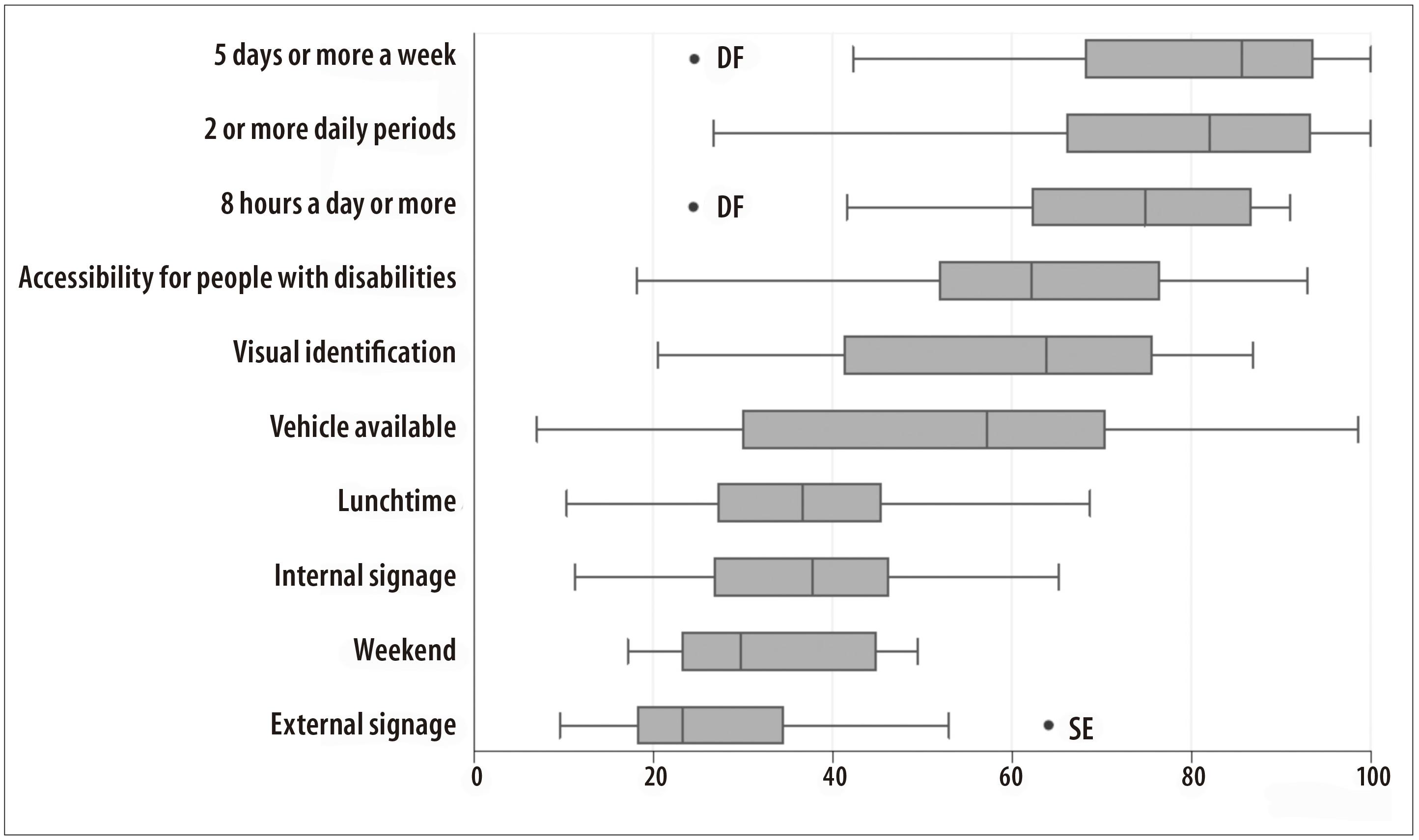
Figure 1 - Distribution of potential coverage (%) of indicators of infrastructure available in the Primary Health Care of federated unities, Brazil, 2012
Teams with an adequate structure for people with disabilities (n=36,796) presented the coverage of 56.9%, varying from 18.1% in Distrito Federal to 92.9% in Sergipe state. The coverage of teams that had a vehicle available for external activities (n=33,063) was 51.1%, varying from 7.0% in Distrito Federal to 98.6% in Piauí state. 24,711 teams offered service during lunchtime, with coverage of 38.2% and variation from 10.3% in Distrito Federal to 68.7% in Amapá state. Regarding teams that had adequate internal signage (n=22,366), the coverage was 34.6%, varying from 11.2% in Distrito Federal to 65.2% in Roraima state.
The lowest coverages were identified on teams that offered service during weekends (28.4%; n=18,381 teams) and that belonged to PHU with adequate external signage (25.4%; n=16,410 teams), with coverage variations from these two indicators, respectively, from 17.1% in Distrito Federal to 49.5% in Espírito Santo state, and from 9.5% in Distrito Federal to 64.1% in Sergipe state.
Indicators of team composition
Among 49,331 PHC teams identified, the CHA coverage (n=226,594 agents) was of 87.6%. In Distrito Federal, it was observed the lowest values: 28.1%. In São Paulo state, 43.1%, in Rio de Janeiro state, 52.6%, and in Rio Grande do Sul state, 58.2% (Table 2 and Figure 2).
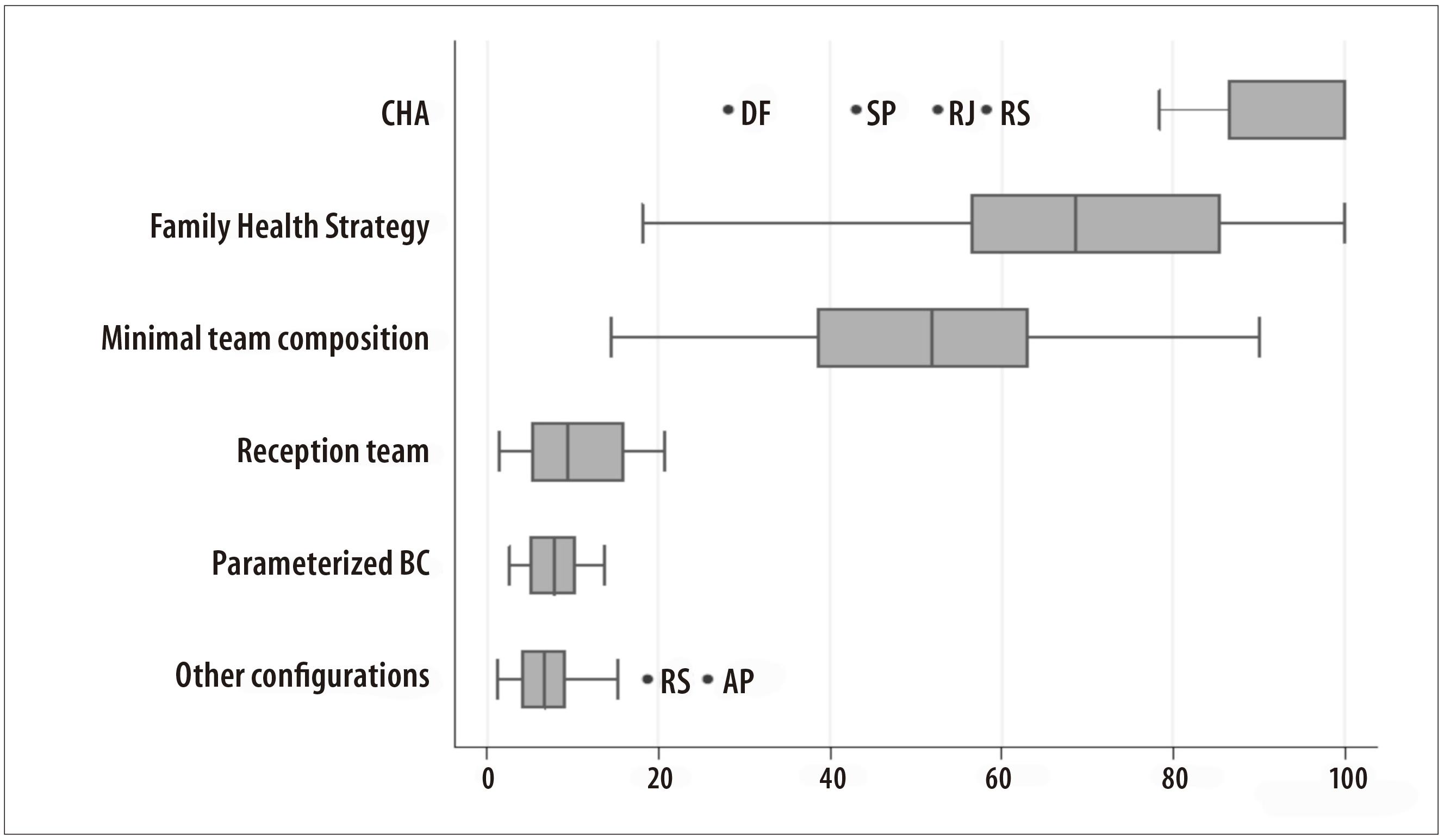
Figure 2 - Distribution of potential coverages (%) of indicators of team composition in the Primary Health Care of the federated unities, Brazil, 2012
The coverage for FHS teams (n=39,045) was 60.4%, varying from 18.1% in Distrito Federal to 100.0% in Piauí, Paraíba and Sergipe states. Regarding the teams that had the minimum composition of health care professionals (n=28,889), the coverage was 44.7% and varied from 14.5% in Distrito Federal to 90.0% in Paraíba state.
For teams that had professionals receiving patients (n=6,744), the coverage was 10.4% and varied from 1.4% in Espírito Santo state to 20.0% in Santa Catarina state.
Regarding the parameterized PHC teams (n=5,459), the coverage was 8.4%, varying from 2.7% in Amazonas state to 13.7% in Santa Catarina state. Only 7.5% of the population were covered by teams with different types of organization (n=4,827), with emphasis on atypical coverages identified in Amapá (25.8%) and Rio Grande do Sul (18.7%) states.
Indicators of available services
Among the 49,331 PHC teams identified in Brazil, the higher coverages were estimated for teams with nursing care appointments (70.9%; n=45,843 teams) and dressing services (70.4%; n=45,542 teams). We emphasize that Distrito Federal has the lower percentages among these coverages: 25.9% and 24.8%, respectively. The population coverage of teams with medical appointments (n=43,829) was 67.8%, reaching the lowest percentage in Distrito Federal (26.8%) among all other federated unities (Table 2 and Figure 3).
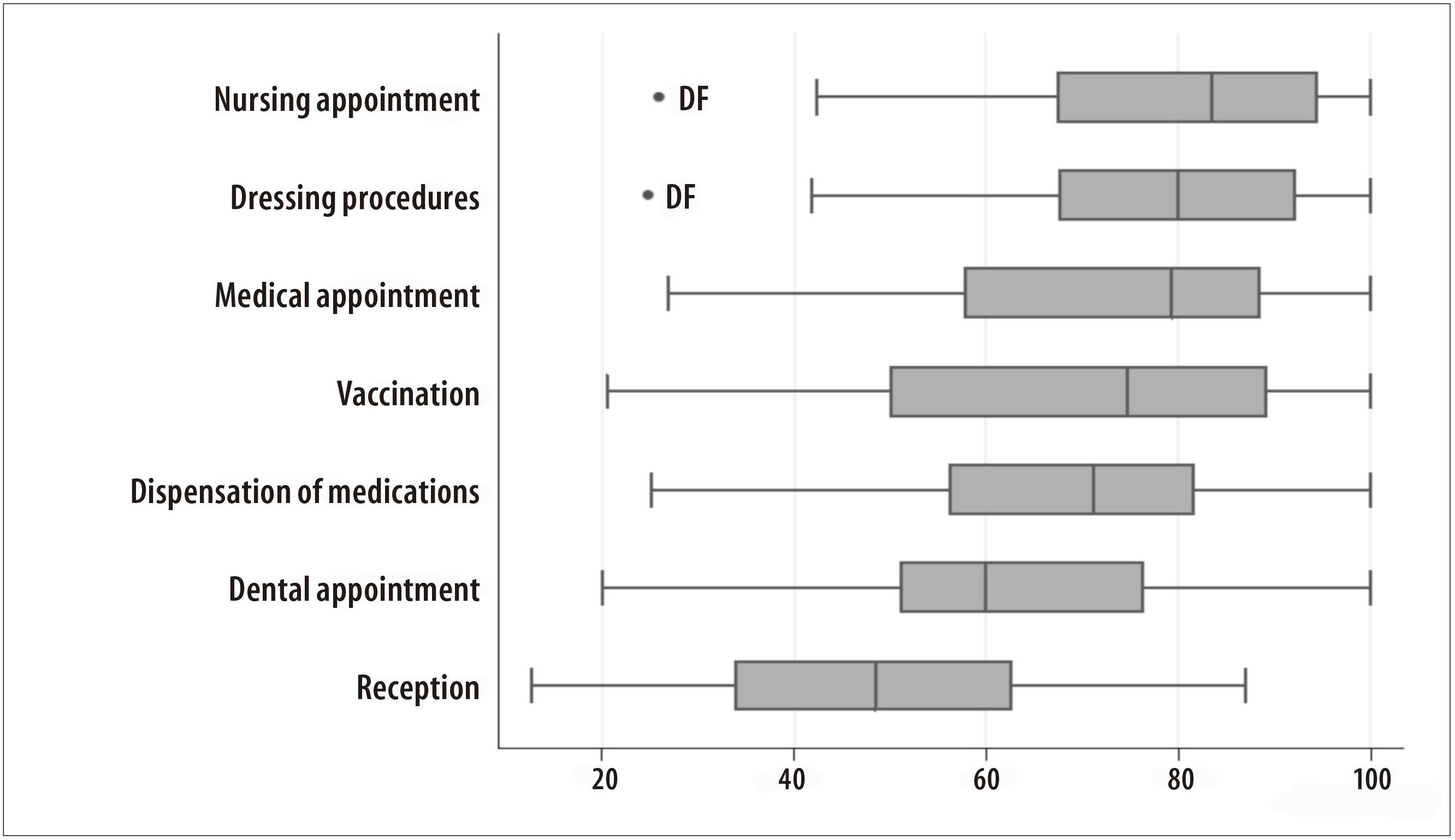
Figure 3 - Distribution of potential coverages (%) of indicators of services available in the Primary Health Care of the federated unities, Brazil, 2012
Teams with vaccination services presented the coverage of 61.8% (n=39,957 teams), with the lowest percentage in Distrito Federal (20.5%) among all other federated unities. For teams with dental care appointments (n=34,559), the coverage was 53.4%, varying from 20.0% in Distrito Federal to 100.0% in Paraíba state.
Regarding teams with dispensation of medications available (n=39,340), the coverage was 60.8%, varying from 25.1% in Distrito Federal to 100.0% in Piauí and Roraima states.
The coverage for receptivity (n=34,221) was 52.9%, and its variation was from 12.6% in Rondônia state to 86.9% in Santa Catarina state.
Discussion
This is the first article that, based on national census data, estimates and discusses potential PHC coverages in Brazil according to selected indicators of structure. Its findings suggest high potential coverages (70.0% or more) for general PHC, as well as for CHA services. Some indicators also stand out with high coverages, in particular: the service in five days a week or more; with two or more shifts; availability of nursing care appointments; and dressing procedures. Nonetheless, other relevant indicators show low potential coverages (<30%), for example, the service on weekends, availability of a reception professional in the PHC teams, and external signage. However, we observed important regional differences in these indicators, with some federated unities, presenting, repeatedly, incipient potential PHC and FHS coverages.
The estimate of potential coverage adopted in this study allowed us to observe that, despite high proportions of PHU possessing some resource or service, a significant portion of the population can still be uncovered if the PHC coverage in the federated unity is incipient. This fact can partially explain the apparently divergent results between the estimated coverages in the present study and, particularly, one recent publication of the Ministry of Health based on the same data of this research.10
In this study, we demonstrated the high PHC coverages in 21 from 27 federated unities. Likewise, it was observed high coverage in 13 from 27 federated unities of the FHS teams, and in 23 from 27 federated unities when considered the CHA services. These results supported the PNAB guidelines which preconizes expansion strategies, qualification and consolidation of the PHC as elements that facilitate the extension, resolution, and promote a favorable cost-effectiveness ratio.1
It is possible to observe the higher PHC coverages overtly oriented towards states and regions less economically developed . For example, we noticed that in the Northeast region, all federated unities showed high PHC coverages of FHS teams and CHA services. The only exception was from Pernambuco state, which had an intermediate coverage of FHS teams. These results indicate the contribution of the FHS for widening to the access to health care services, especially in areas with assistance gaps, outskirts of cities and rural areas from small and medium sized Brazilian municipalities.11 Indeed, Brazil has been mentioned as a successful example of PHC policies involving large scale CHA services.12
In a similar manner, the relative growth of the FHS coverage in the period from 1999 to 2004 was higher in the Northeast than in the Southern region, with the FHS coverage growing 35.0% or more in approximately 65.0% of Northeastern municipalities, while in the South, the growth was of only 5.0%.13
The findings of the present study support the data presented by the Primary Health Care Department of the Health Care Secretariat of the Ministry of Health, indicating that most part of Brazilian municipalities with low Human Development Index (HDI) (75.0%) have a high FHS coverage (70.0% or more).14 As a result of this clear intention of search for equity, studies have suggested that the expansion of FHS in less economically developed regions has contributed to reduction of inequality in health, particularly in health services accessibility and coverage differentials in Brazil..9,15,16
In Brazil, other social policies have been introduced under the principle of social justice and equity. As a consequence of these initiatives, recently, it was observed and described the synergy between these policies, which were positive to health. Example of this was the analysis of the interaction between the FHS and the Bolsa Família Programme (PBF), indicating reductions on risk of infant deaths.16 In this context, it is worth mentioning the induction from PNABand its finantial outline based on equity, which specially benefits municipalities with smaller territories, the poorest condition, higher percentage of poor or extremely poor population and with the lowest population density.
It comes to our attention that states from the Northern region did not have the same performance like the states from the Northeastern region, considering the coverage of these indicators. Considering FHS team coverages, only two of the seven states from Brazil’s Northern region presented high coverages. It is worth to notice that the PNAB induces the conformation of teams with differentiated composition to assist the riverside population of the Legal Amazon region and Pantanal áreas (south of Mato Grosso state). Thus, it is necessary to identify solutions for each of these regions and their real demands.
In general, low potential coverages were estimated, especially regarding the operation of teams during lunchtime and on weekends. This finding suggests the common challenge of access to PHC for the working population with limited negotiation possibilities for absenting the job. Other factors must be considered, for example, the recent effort in Brazil and some federated unities towards the improvement of the emergency and urgent health care network, with the expansion and adaption of Emergency Care Units (UPA). This strategic option of managers can, to a certain extent, conceal the consequences of not offering the PHC services on weekends and during lunchtime. It is a matter worth looking with more depth in further studies.
Another infrastructure result of relevant meaning is the low presence of external and internal signage as a limiting factor of geographical access to the PHU and PHC, which can be a consequence of the use of adapted households to the operation of these units and services. Studies point out signage as promoting conditions of accessibility.17,18 Other researches dedicated to the evaluation of structural aspects of the PHC found similar situations to our study in the physical environment, material resources,13,19,20 and staff,21 as well as inadequate structure characteristics related to the access for the elderly and people with disabilities.22
Access is a condition that can interfere in the relation between the demand and the entry to the service, being the characteristics of supply capable of facilitating or obstructing the use of health services for potential users.23 Information, signage and accessibility are the aspects of ambience defined for the Brazilian National Health System (SUS) by the National Humanization Policy (NHP).24
We observed favorable results for Brazil regarding teams with nursing appointments and dressing services. Intermediate coverages were identified for essential services, such as: medical appointments, vaccination, dispensation of medications, dental appointments and receptivity.
The results point out to great inequalities of the potential coverages related to the PHC indicators of structure amongst Brazilian federated unities . Two situations should be discussed. The first one concerns the federated unities that, although had intermediate or high potential PHC coverages, presented poor indicators of structure, with a considerable amount of the population not being covered. Examples of this group are Mato Grosso do Sul, Rondônia and Pará states. The second situation concerns the federated unities with low or intermediate potential PHC coverages. In some way, they limit the possible extent of coverage that could be assumed by all the analyzed indicators. In this group, there are Distrito Federal, and the states of São Paulo and Rio de Janeiro. Distrito Federal has reported the lowest coverage percentages for virtually every researched criteria. Although the poor structure indicators are, to a certain extent, conditioned by the PHC coverage values in these states, still, they indicate that a significant amount of the population is potentially not covered by these services, something that administrators should give attention to.
Presently in Brazil, the PHC, especially the FHS, is heterogeneous in its implementation in different geographical areas, not only in terms of coverage, but also in relation to the extent of the PHC attributes. Based on the SUS interfederative relationships and on the guidelines for the implementation of the FHS from the federal level,the Primary Health Care System becomes concrete at local level. Its conditions - and interpretation - will define its singularity, resulting in adiversity of structures, team compositions, operations, offer of services and characteristics of what we presently call the Primary Health Care and Family Health Strategy.
It is possible that in contexts of smaller scope, other studies can detail the diversity and the characteristics of the PHC, searching to explain its specific quality. The permanent challenges to face are the theoretical deepening and the combination of methodologies capable of measuring the quality of the PHC in the nationwide perspective, and also in the contexts of interpretation and reinterpretation of the FHS.
The present study also presents some limitations. There is a risk of extrapolating meaning boundaries due to the use of a set of indicators of structure like proxis of direct measure of access and utilization. Such indicators of structure, however, can facilitate or hamper the extent of these PHC attributes, equally dependent on other indicators.
Another limitation can be related to the accuracy of the population base, defined in 3,000 people (average set by PNAB) for the estimate of the potential coverage indicators. Still, we believe that our methodology is more informative than others adopted to describe the offer of services only based on PHU numbers.
The determination of the causal networks which attribute the structure of health services to their results are complex, it assumes the consideration of many dimensions for its identification.20 The findings of this work contribute to shed light on the structure indicators to evaluate health care services and to discuss its relation with the quality of processe indicators and the achievement of results, in the contexto osindividual and population health. The present study shows the heterogeneity in the implantation of Primary Health Care in the country, and the challenges for its evaluation.25
The methodology used in this research can be adapted to monitor the distribution of resources in health services in many levels. The evaluation conducted in smaller geographical units will benefit by a bigger homogeneity, contributing to future analyses to be conducted in collaboration, aiming to institutionalize the evaluation in the services and the accomplishment of a universal and an equitativehealth system.
REFERENCES
1. Brasil. Ministério da Saúde. Portaria nº 2.488, de 21 de outubro de 2011. Aprova a Política Nacional de Atenção Básica, estabelecendo a revisão de diretrizes e normas para a organização da Atenção Básica, para a Estratégia Saúde da Família (ESF) e o Programa de Agentes Comunitários de Saúde (PACS). Diário Oficial da República Federativa do Brasil, Brasília (DF), 2011 out 24; Seção 1:48. [ Links ]
2. Felisberto E. Da teoria à formulação de uma Política Nacional de Avaliação em Saúde: reabrindo o debate. Cienc Saude Coletiva. 2006 jul-set;11(3):553-63. [ Links ]
3. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Saúde mais perto de você: acesso e qualidade: Programa Nacional de Melhoria do Acesso e da Qualidade da Atenção Básica (PMAQ): manual instrutivo [Internet]. Brasília: Ministério da Saúde; 2012 [citado 2016 dez 23]. (Série A. Normas e Manuais Técnicos). Disponível em: Disponível em: http://189.28.128.100/dab/docs/publicacoes/geral/manual_instrutivo_pmaq_site.pdf [ Links ]
4. Starfield B. Atenção primária: equilíbrio entre necessidades de saúde, serviços e tecnologia. Brasília: Organização das Nações Unidas para a Educação, a Ciência e a Cultura: Ministério da Saúde; 2004. [ Links ]
5. Cazarin G, Poças KC, Mendes M. Avaliação e qualidade em saúde: fonte de inovações e reflexões. Rev Bras Saude da Família. 2011;29:51-8. [ Links ]
6. Uchimura KY, Bosi MLM. Qualidade e subjetividade na avaliação de programas e serviços em saúde. Cad Saude Publica. 2002 nov-dez;18(6):1561-9. [ Links ]
7. Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005 Dec;83 (4):691-729. [ Links ]
8. Silva LMV. Conceitos, abordagens e estratégias para a avaliação em saúde. In: Hartz ZMA, Vieira-da-Silva LM, organizadoras. Avaliação em Saúde: dos modelos teóricos à prática na avaliação de programas e sistemas de saúde. Salvador: UFBA; Rio de Janeiro: Fiocruz; 2005. [ Links ]
9. Aquino R, Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009 Jan;99(1):87-93. [ Links ]
10. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Retratos da atenção básica no Brasil 2012: características das Unidades Básicas de Saúde [Internet]. Brasília: Ministério da Saúde ; 2015 [citado 2016 dez 23]. (Gestão da Atenção Básica; v. 1). Disponível em: Disponível em: http://189.28.128.100/dab/docs/portaldab/publicacoes/retratos_ab_2_vol_1.pdf [ Links ]
11. Sousa MF. A reconstrução da saúde da família no Brasil: diversidade e incompletude. In: Sousa MF, Franco MS, Mendonça AVM. Saúde da Família nos municípios brasileiros: os reflexos dos 20 anos no espelho do futuro. Campinas: Saberes Editora; 2014. [ Links ]
12. World Health Organization. The world health report 2008: primary health care now more than ever [Internet]. Geneva: World Health Organization; 2008 [cited 2016 Dec 23]. Available from: Available from: http://www.who.int/whr/2008/whr08_en.pdf [ Links ]
13. Facchini LA, Piccini RX, Tomasi E, Thumé E, Silveira DS, Siqueira FV, et al. Desempenho do PSF no Sul e no Nordeste do Brasil: avaliação institucional e epidemiológica da Atenção Básica à Saúde. Cien Saude Coletiva. 2006 jul-set;11(3):669-81. [ Links ]
14. Ministério da Saúde (BR). Secretaria de Gestão Estratégica e Participativa. Departamento de Monitoramento e Avaliação da Gestão do SUS. Painel de indicadores do SUS nº4. v.2. Brasília: Ministério da Saúde; 2008. [ Links ]
15. Macinko J, Guanais FC, Souza MF. Evaluation of the impact of the Family Health Program on infant mortality in Brazil, 1990-2002. J Epidemiol Community Health. 2006 Jan;60(1):13-9. [ Links ]
16. Rasella D, Aquino R, Santos CAT, Paes-Sousa R, Barreto ML. Effect of a conditional cash transfer programme on childhood mortality : a nationwide analysis of Brazilian municipalities. Lancet 2013 Jul;382(9886):57-64. [ Links ]
17. Ribeiro JP, Mamede SN, Souza MR, Souza MM, Rosso CFW. Acessibilidade aos serviços de saúde na Atenção Básica do estado de Goiás. Rev Eletr Enf. 2015 jul-set;17(3):1-11 [ Links ]
18. Garcia ACP, Andrade MAC, Contarato PC, Tristão FI, Rocha EMS, Rabello AE, et al. Ambiência na Estratégia Saúde da Família. Vigil Sanit Debate. 2015;3(2):36-41. [ Links ]
19. Silveira DS, Santos IS, Costa JSD. Atenção pré-natal na rede básica: uma avaliação da estrutura e do processo. Cad Saude Publica. 2001 jan-fev;17(1):131-9. [ Links ]
20. Moura BLA, Cunha RC, Fonseca ACF, Aquino R, Medina MG, Vilasbôas ALQ, et al. Atenção primária à saúde: estrutura das unidades como componente da atenção à saúde. Rev Bras Saude Matern Infant. 2010 nov;10 supl 1:s69-81. [ Links ]
21. Niquini RP, Bittencourt SA, Lacerda EMA, Saunders C, Leal MC. Avaliação da estrutura de sete unidades de saúde da família para a oferta da assistência nutricional no pré-natal no município do Rio de Janeiro, Brasil. Rev Bras Saude Matern Infant. 2010 nov;10 supl 1:s61-8. [ Links ]
22. Siqueira FCV, Facchini LA, Silveira DS, Piccini RX, Thumé E, Tomasi E. Barreiras arquitetônicas a idosos e portadores de deficiência física: um estudo epidemiológico da estrutura física das unidades básicas de saúde em sete estados do Brasil. Cien Saude Coletiva. 2009 jan-fev;14(1):39-44. [ Links ]
23. Travassos C, Castro MSM. Determinantes e desigualdades sociais no acesso e na utilização de serviços de saúde. In: Giovanella L, Escorel S, Lobato LVC, Noronha JC, Carvalho AI, organizadores. Políticas e sistema de saúde no Brasil. Rio de Janeiro: Fiocruz; 2008. [ Links ]
24. Ministério da Saúde (BR). Secretaria Executiva. Núcleo Técnico da Política Nacional de Humanização. HumanizaSUS: Política Nacional de Humanização: documento base para gestores e trabalhadores do SUS. 2. ed. Brasília: Ministério da Saúde; 2004.(Série B. Textos Básicos de Saúde) [ Links ]
25. Cardoso MO, Vieira-da-Silva LM. Avaliação da cobertura da atenção básica à saúde em Salvador, Bahia, Brasil (2000 a 2007). Cad Saúde Pública 2012; 28:1273-84. [ Links ]
* The present article is part of the doctoral thesis of Katia Crestine Poças, entitled ‘Evaluation of the Primary Health Care in Distrito Federal’, qualified together with the Programa de Pós-Graduação em Saúde Coletiva of the Faculdade de Ciências da Saúde of the University of Brasília in 2016. The manuscript’s research is financed by the Ministry of Health - Proposal 922420800001110-04; Process 25000.187078/2011-11 - and is registered in the Sistema de Convênios e Contratos de Repasse da Administração Pública Federal (SICONV) under the number 760463/11. There were also stages of the study that were backed by the Fundação de Apoio à Pesquisa do Distrito Federal (FAPDF) - Edital FAPDF 10/2012, Research program for the SUS: shared management in health PPSUS. FAP/DF/SESDF/MS/CNPQ.
Received: July 08, 2016; Accepted: October 11, 2016











 texto en
texto en 


