Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2337-9622
Epidemiol. Serv. Saúde v.26 n.2 Brasília abr./jun. 2017
http://dx.doi.org/10.5123/s1679-49742017000200020
ECONOMIC EVALUATION
Budget impact analysis
1Universidade de Sorocaba, Programa de Pós-Graduação em Ciências Farmacêuticas, Sorocaba-SP, Brasil
2Universidade de Brasília, Faculdade de Ceilândia, Brasília-DF, Brasil
3Universidade de Brasília, Faculdade de Medicina, Brasília-DF, Brasil
Introduction
The budget impact analyses estimate the financial consequences of the adoption and diffusion of a new strategy or technology in a health system.1 When these analyses are adequately conducted, they can predict how the changes in the offer of inputs or services may influence the future costs of a health problem. For example, when a new drug is introduced in the treatment for rheumatoid arthritis by the Brazilian National Health System (SUS), it is possible to determine how much of additional resources the health manager will have to provide to cover the expenses of this inclusion. The budget impact analysis provides this information through the comparison of costs before and after the change. This type of study is indicated for the analysis of interventions that proved to be efficient, safe and cost-effective.2 Consequently, the budget impact analysis does not focus on matters of efficacy or effectiveness, but on costs, i.e., how these resources may vary with the incorporation of new technologies.
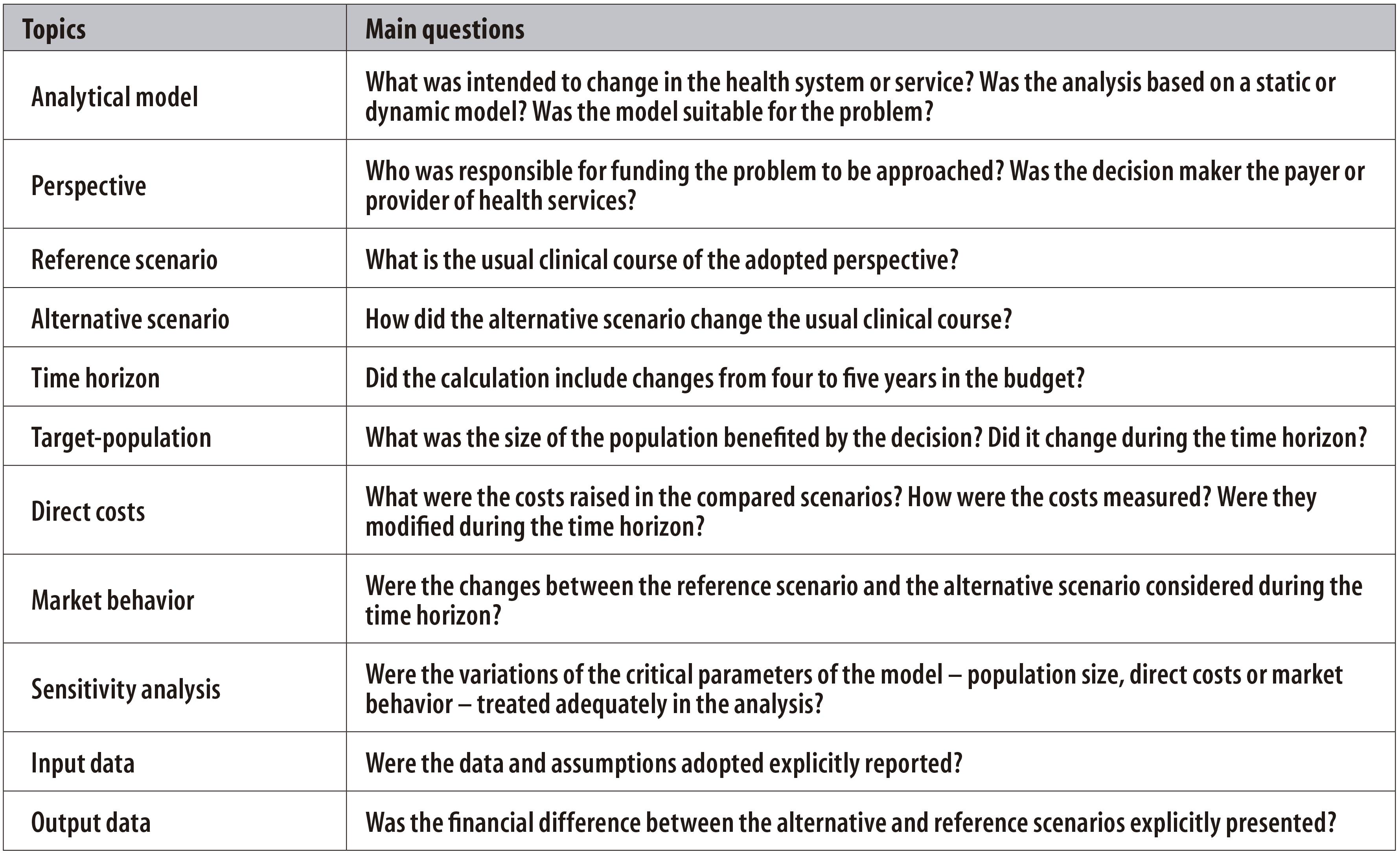
A considerable international effort, with some benefits to Brazil, has been made in order to produce methodological recommendations for budget impact analyses. They present topics to be assessed in this type of study (Figure 1). This article aims to present some of the main elements of those recommendations, and the references presented allow a deeper understanding on the subject.
Model structure
Budget impact relates to the financial changes that take place in a new scenario, in relation to the reference scenario. The reference scenario covers the financial consequences of the current management of the studied problem. The new, or alternative, scenario contains expenses from the adoption of the new offer on inputs and services.
It is necessary to specify in the model the perspective of the analysis. In general, the perspective used is the one of the payer, i.e., the service provider or the health system.1,3 The direct costs related to the problem of interest are also included here.4-5 The set of information allows the use of static or dynamic models.6 These models vary in the electronic spreadsheet, which enable the construction of models of decision analysis, to specific softwares, which formulate dynamic models and more complex ones.
Usually, several scenarios are built in order to increase the validity of the prediction.4-5
Time horizon
Budget impact analyses include four to five years in the comparison scenarios.4-5 This time horizon will influence the remaining parameters, such as: (i) the target population - will it reduce or increase during the period?; (ii) the costs in the studied context - will they be modified throughout time?; (iii) will the potential stakeholders for the alternative scenarios influence on decision making during the whole period?
Population characteristics and size
Most of times, changes in the set of procedures affect a group of individuals covered by the service provider or the health system. Thereby, estimating the beneficiary population with regard to their characteristics and size will scale out the costs in line with future perspectives. There are two common approaches related to the perspectives of the service provider or health services:4-5 (i) historical series of the population being assisted; and (ii) calculation of the prevalence of the problem adjusted for access capacity.
The challenge lies on dealing with variables with difficult behavioral prediction throughout time, such as incidence and prevalence of the health problem, the level of improvement of diagnostic procedures and the off label use, i.e., the use of technology with objectives that are different from those previously specified.7 A common problem, and of difficult solution, is the fact that the new scenario modifies the natural history of the disease during the time horizon, increasing or reducing morbidity and mortality.
Disease-related costs
Once the perspective is defined, the next step is to identify the financial path of the health problem in the reference scenario. Based on the most common clinical course, the direct costs are estimated in parts, for example, medical appointments, hospitalizations and medication intake.8 Data on the costs are weighed in relation to the population size, in order to obtain the value of the reference scenario.
Based on the better scientific evidence, changes in the clinical courses are estimated, and, consequently, in the direct costs of alternative scenarios.9 According to the target-population size, the value of each alternative scenario is calculated. After the estimates are ready, it is possible to calculate the differences between the alternative scenarios and the reference scenario, in order to estimate the incremental budget impact. Usually, the budget impact is presented in percentage, in order to make the outcomes communication easier.
Preferences and market behavior
It is important to highlight that the changes in procedure tables and reimbursement hardly happen at a sudden. Several factors influence on the dissemination of the change, such as the interest of users, adoption of the input by the health professionals, external influence and logistics matters. Simultaneously, unexpected consequences of the alternative scenario come out and may influence in the access to the new strategy to be adopted.
Theoretically, the migration of the reference scenario to the alternative one happens gradually within the time horizon. However, there are few studies that assess the impact of those changes.10 Considering the perspective of the Brazilian Ministry of Health, some analyses involving medications show that this migration is influenced by the available alternatives, by the combination with other products and by the therapeutic innovation.11
Sensitivity analysis
The possible variations on the parameters included in the budget impact analyses should be verified. First, all the elements included in the model should be assessed, particularly the population size, the direct costs and the market behavior. The procedure is similar to what is conducted in cost-effectiveness studies, including univariate analysis and tornado diagrams.12
Moreover, the most useful studies are those that introduce clinically valid information (reflect the context), are transparent (guarantee the calculation repetition) and have flexibility (allow adaptation).7
Concluding remarks
Health care is marked by periods of financial crisis and budget restrictions. However, even in periods of financial instability, there are more health needs than resources to tackle them. The good use of the available resources will allow more benefits to be achieved per costs unit. Budget impact analyses help managers to make decision, because they estimate the financial feasibility of a strategy in a health service or system.
Referências
1. Mauskopf J, Earnshaw S. A methodological review of us budget-impact models for new drugs. Pharmacoeconomics. 2016 Nov;34(11):1111-31. [ Links ]
2. Silva EN, Silva MT, Pereira MG. Estudos de avaliação econômica em saúde: definição e aplicabilidade aos sistemas e serviços de saúde. Epidemiol Serv Saude. 2016 jan-mar;25(1):205-7. [ Links ]
3. van de Vooren K, Duranti S, Curto A, Garattini L. A critical systematic review of budget impact analyses on drugs in the EU countries. Appl Health Econ Health Policy. 2014 Feb;12(1):33-40. [ Links ]
4. Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health. 2014 Jan-Feb;17(1):5-14. [ Links ]
5. Ferreira-Da-Silva AL, Ribeiro RA, Santos VCC, Elias FTS, d'Oliveira ALP, Polanczyk CA. Diretriz para análises de impacto orçamentário de tecnologias em saúde no Brasil. Cad Saude Publica. 2012 jul;28(7):1223-38. [ Links ]
6. Silva EN, Silva MT, Pereira MG. Modelos analíticos em estudos de avaliação econômica. Epidemiol Serv Saude. 2016 out-dez;25(4):855-8. [ Links ]
7. Watkins JB, Danielson D. Improving the usefulness of budget impact analyses: a U.S. payer perspective. Value Health. 2014 Jan-Feb;17(1):3-4. [ Links ]
8. Silva EN, Silva MT, Pereira MG. Identificação, mensuração e valoração de custos em saúde. Epidemiol Serv Saude. 2016 abr-jun;25(2):437-9. [ Links ]
9. Silva MT, Silva EN, Pereira MG. Desfechos em estudos de avaliação econômica em saúde. Epidemiol Serv Saude. 2016 jul-set;25(3):663-6. [ Links ]
10. Garuoliene K, Godman B, Gulbinovic J, Schiffers K, Wettermark B. Differences in utilization rates between commercial and administrative databases: implications for future health-economic and cross-national studies. Expert Rev Pharmacoecon Outcomes Res. 2016;16(2):149-52. [ Links ]
11. Schneiders RE, Ronsoni RM, Sarti FM, Nita ME, Bastos EA, Zimmermann IR, et al. Factors associated with the diffusion rate of innovations: a pilot study from the perspective of the Brazilian Unified National Health System. Cad Saude Publica. 2016 Oct;32(9):e00067516. [ Links ]
12. Silva EN, Silva MT, Pereira MG. Incerteza em estudos de avaliação econômica. Epidemiol Serv Saude. No prelo 2017. [ Links ]











 texto em
texto em 
 Curriculum ScienTI
Curriculum ScienTI