Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.27 no.1 Brasília mar. 2018 Epub 05-Fev-2018
http://dx.doi.org/10.5123/s1679-49742018000100012
ORIGINAL ARTICLE
Counseling by health professionals and healthy behaviors among the elderly: population-based study in Pelotas, South of Brazil, 2014*
1Universidade Federal de Pelotas, Programa de Pós-graduação em Epidemiologia, Pelotas, RS, Brasil
2Universidade Federal de Pelotas, Departamento de Enfermagem, Pelotas, RS, Brasil
Objective:
to analyze the association between counseling by health care professionals and healthy behaviors among the elderly.
Methods:
population-based, cross-sectional study with elderly individuals (≥60 years) interviewed in 2014; Poisson regression was used to estimate crude and adjusted prevalence ratios (PR) of associations between counseling by health professionals on the reduction of salt, sugar and fat and on the practice of physical activity during the year previous to the interview and healthy behaviors.
Results:
1,281 elderly individuals were interviewed; after adjustments, the elderly who mentioned receiving counseling by health professionals reported reduction in the intake of salt (PR 1.64; 95%CI 1.41;1.91), sugar and sweets (PR 1.21; 95%CI 1.08;1.36) and greater practice of physical activity (PR 1.21; 95%CI 1.06;1.39), when compared to the elderly who had not received any counseling.
Conclusion:
the counseling carried out by health professionals seems to favor the practice of healthy habits among elderly individuals.
Keywords: Health Behavior; Health of the Elderly; Cross-sectional Studies; Counseling; Life Style
Introduction
The process of population aging in Brazil is a phenomenon caused by the demographic transition, which contributed to the epidemiological transition, in addition to being characterized by the absolute and relative increase in the prevalence of chronic diseases.1,2 Data from the 2013 National Health Survey (PNS)3 showed that over 50% of the Brazilian elderly individuals had at least one chronic non-communicable disease (NCD) and used health services in a larger scale.3,4 Health services should be prepared to meet this growing demand,5 and actions to promote disease prevention and health are crucial in order to guarantee a better quality of life for the elderly.1,6
NCDs are considered a health problem worldwide, and have a higher burden in low-income and middle-income countries.7 Even if a large part of the Brazilian elderly are affected by at least one NCD -for example, high blood pressure -, this problem should not be treated simply as a consequence of aging. They are diseases that can be prevented with a healthy lifestyle.5 Health promotion and therapeutic measures have become key strategies which help reduce the burden of NCDs in the health services and contribute to the reduction of conditions caused by them.8-10 In Brazil, the 2010 National Policy for Health Promotion (PNPS) emphasizes the guidelines on healthy habits as an educational process involving all health care professionals and users of the services,2 helping with their own health management,6,11 given the complexity of embracing a healthy lifestyle for each age group.1,2,5
Counseling is an educational practice offered by health care professionals which aims to make individuals active on their health process, concerning their autonomy and valuation of their potential, bringing about a change of behavior and improvement in the quality of life.6,12 The resulting benefits from this guidance which were identified in the individuals' life habits, such as diet care, increase in physical activity and reduction in alcohol intake and smoking, can be found in the literature;8,9,13 people who frequently receive high-quality advice from health care professionals feel more motivated to embrace a healthy lifestyle.14
Studies based on cross-sectional survey data in Canada with hypertensive8 and diabetic9 individuals showed a higher probability of engagement in adopting some healthy habits among those who had received guidance or support from health care professionals. In Brazil, there is a lack of research on this subject.
This study aimed to analyze the association between receiving counseling by health care professionals and healthy behaviors among the elderly.
Methods
This is a cross-sectional, population-based study carried out with individuals aged 60 years or over, residing in the urban area of the municipality of Pelotas, Rio Grande do Sul State, in 2014.
Pelotas is a medium-sized municipality located in the South region of Brazil. It had 305,696 inhabitants in 2010, of which 6,099 were elderly (15.1%). Its 2010 human development index (HDI)19 was 0.739.
The estimated sample size was of 1,119 elderly individuals, considering a 37% prevalence of sufficient physical activity.20 The following parameters were used: 95% confidence interval; four percentage points of sampling error; and a design effect of 2.0. In order to meet the rest of the objectives of the research, we established that about 1,600 elderly individuals would be included into the study.
Sample selection was carried out in two stages: the first one consisted on the selection of the municipality’s census tracts, according to the criteria established by the Brazilian Institute of Geography and Statistics (IBGE) in 2010; and the second stage consisted on the systematic selection of households within each sector. Based on the estimate of 12 elderly individuals per sector and 0.43 per household, 133 sectors and 3,745 households were selected. All individuals aged 60 or over were invited to take part in the survey and were interviewed at their homes. Elderly people living in long-term care institutions, those in enteral nutritional therapy and those unable to answer the food behavior questionnaire, while in the absence of a relative or caregiver were not included in the survey.
The studied outcomes were the report, given by the elderly, of the reduction of salt intake, the frequency of sugar intake (sweets, soft drinks and processed juices) and fried foods, and sufficient physical activity. Fried food intake was used as a proxy for fat intake, because in a previously applied questionnaire on reduced food frequency21 it was not possible to quantify the intake of fats in detail.
The reduction in salt intake was assessed through the following question: “Thinking about the last year, did you reduce the amount of salt you put in your food?”
In order to assess the frequency of sugar and fried foods intake, we used the question “Since [day of the previous week] until now, on how many days did you...” complemented by (i) “eat sweets or have soft drinks and processed juice?” and (ii) “eat fried foods?” Elderly individuals who claimed to have eaten these foods up to two days during the previous week18 were considered to have low frequency of sugar and fried foods intake, a criterion also used in a previous study.18 This recall period was adopted in order to minimize recall bias, as well as the possibility of reverse causality bias, since it concerns events which are not so significant as the reduction of salt intake.
Concerning the recommendation of sufficient physical activity, we considered as active those elderly individuals who practiced ≥150 minutes/week of physical activity, as recommended by the World Health Organization (WHO).22 To achieve such classification, we used the extended version of the International Physical Activity Questionnaire (IPAQ),23 using a global estimate, considering physical activity on commuting and leisure time. Domestic and work activities were disregarded on this study, in order to construct the variable of global estimate of physical activity.
The exposures assessed were the guidance on healthy habits given by health professionals to elderly individuals who had used health services over the previous year, assessed through the following question: “Since [month] of last year until now, did any health care professional advise you...”, complemented by “to reduce salt intake?”, “to reduce sugar and sweets intake”, “to reduce fat intake” and “to practice physical activity?”.1,5,11 These questions were preceded by a filter question: “Since [month] of last year until now, did you visit any health care professional?”, considering every kind of medical care (public and private).
Other independent variables were included, such as demographic: sex (male; female), age group (in years: 60-69, 70-79 or≥80), skin color observed by the interviewer (white, black, brown, Asian or indigenous, later re-categorized as white, other - only one individual classified himself as Asian and another one as indigenous), marital status (married, single, widowed or divorced) and economic classification (A/B; C; D/E).24 We also used self-referred morbidities as variables, according to medical diagnosis (yes; no) for systemic arterial hypertension, diabetes mellitus and hypercholesterolemia. Finally, we asked about the health services visited over the previous year: number of visits with health care professionals (1, 2 or ≥3) and type of financing health insurance and private; Brazilian National Health System [SUS].
Trained interviewers conducted the interviews, and data were typed in netbooks. If, after three or more attempts in different days and times, the individual did not respond to the interview, we considered it missing data; and if the individual stated more than once that he or she would not participate in this study, we considered it a refusal. Interview quality control was performed in 10% of the sample, mostly face-to-face by field work supervisors provided with a reduced questionnaire - 19 questions. Kappa index was 0.64 for the variable (appointment with a health care professional over the previous year).
Data were analyzed using Stata 12.1 software (Stata Corp, College Station, Texas, USA). Initially, we described the outcomes and obtained the prevalence and their respective 95% confidence intervals (95%CI). We used Poisson regression25 on the crude and adjusted analyses, in order to obtain the prevalence ratios (PR) and their respective 95%CI and p values (Wald test for heterogeneity). In order to control confounding factors of the association between receiving guidance from health care professionals and healthy behaviors on the adjusted analysis, at first we included the socioeconomic and demographic variables into the model; then, we considered self-referred morbidities and kept in its level those which presented a p-value <0.20. We considered associations with a p-value <0.05 statistically significant. All analyses were performed using the survey module, for the study sample design.
The study project was approved by the Ethics Research Committee of the Medical College of the Federal University of Pelotas on November 28th, 2013: Protocol No. 201324538513.1.0000.5317. Interviews were performed only after the signing of the Free Informed Term of Consent by the elderly individual or legal guardian.
Results
A total of 1,844 elderly individuals were eligible for this study, of which 1,451 were interviewed. Missing data and refusals accounted 9.7% (n=179) and 11.6% (n=214), respectively; the majority of them were women (59.3%) and aged between 60 and 69 years (59.5%). From all the interviewed, 1,281 (88.3%) had visited a health care professional in the previous year, which constituted this study sample (Figure 1).
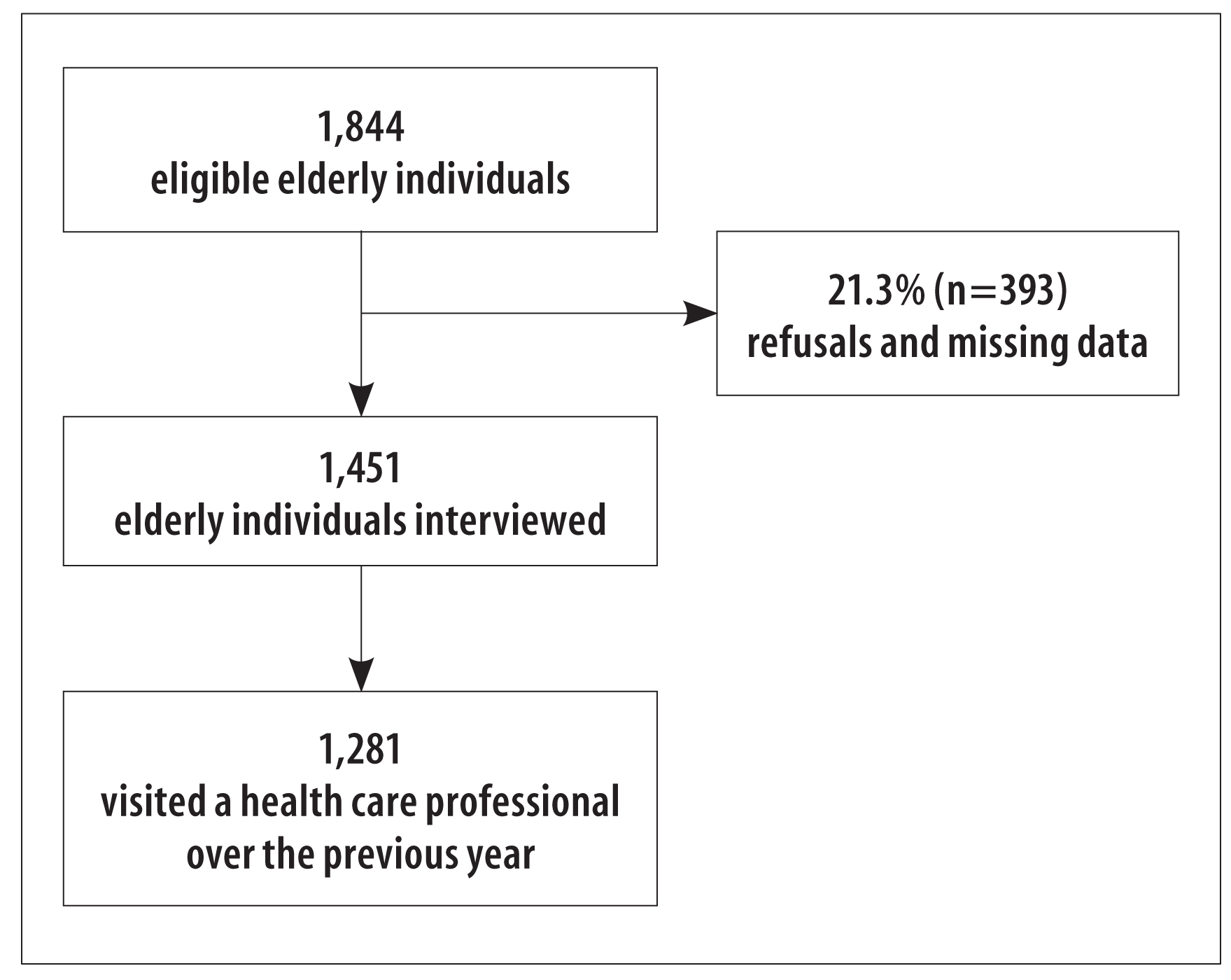
Figure 1 - Flow chart of sample selection for the survey with elderly individuals (n=1,281), Pelotas, Rio Grande do Sul, 2014
Most of the sample was composed of females (64.2%), aged 60-69 years (51.3%), white-skinned (84.4%), with a partner (53.7%) and belonging to economic bracket C (51.7%). The majority (68.2%) of the elderly individuals had a diagnosis of hypertension, 24.9% reported diabetes and 43.4% had high cholesterol. As for the counseling by health care professionals over the previous year, 31.2% of the elderly individuals were advised regarding healthy habits. The elderly interviewed claimed that the main guidance given were reduction of fat (61.7%) and salt intake (61.5%), followed by reduction of sugar intake (50,0%) and practice physical activity (58.2%) (Table 1). About 19.6% of the elderly individuals did not receive any of the researched guidance (data not presented).
Table 1 - Demographic, socioeconomic and health characteristics of elderly individuals (n=1,281) who visited a health care professional over the previous year, Pelotas, Rio Grande do Sul, 2014
| Variable | n (%) | 95%IC a |
|---|---|---|
| Sex | ||
| Male | 459 (35.8) | 33.2;38.5 |
| Female | 822 (64.2) | 61.5;66.8 |
| Age (in complete years) | ||
| 60-69 | 655 (51.3) | 48.5;54.0 |
| 70-79 | 413 (32.3) | 29.7;34.9 |
| ≥80 | 210 (16.4) | 14.4;18.5 |
| Skin color | ||
| White | 1079 (84.4) | 82.4;86.4 |
| Other b | 200 (15.6) | 13.6;17.6 |
| Marital status | ||
| Married/has a partner | 688 (53.7) | 51.1;56.5 |
| Single | 75 (5.9) | 4.6;7.2 |
| Divorced | 111 (8.7) | 7.1;10.2 |
| Widowed | 405 (31.7) | 29.1;34.2 |
| Economic Classification c | ||
| A/B | 483 (37.2) | 34.4;40.0 |
| C | 720 (51.7) | 48.9;54.6 |
| D/E | 169 (11.1) | 9.3;12.8 |
| Arterial Hypertension | ||
| No | 406 (31.8) | 29.2;34.3 |
| Yes | 872 (68.2) | 65.7;70.8 |
| Diabetes mellitus | ||
| No | 960 (75.1) | 72.7;77.5 |
| Yes | 318 (24.9) | 22.5;27.3 |
| High cholesterol | ||
| No | 723 (56.6) | 53.9;59.3 |
| Yes | 554 (43.4) | 40.7;46.1 |
| Number of visits | ||
| 1 | 184 (14.4) | 12.3;16.5 |
| 2 | 239 (18.7) | 16.5;20.8 |
| ≥3 | 857 (66.9) | 64.2;69.7 |
| Type of financing | ||
| Private/ health insurance | 812 (63.4) | 58.8;68.0 |
| SUS | 468 (36.6) | 32.0;41.2 |
| Health care professionals’ guidance | ||
| Salt reduction | 788 (61.5) | 58.8;64.2 |
| Sugar and sweets reduction | 640 (50.0) | 47.2;52.7 |
| Fat reduction | 790 (61.7) | 59.0;64.3 |
| Physical activity | 745 (58.2) | 55.4;60.9 |
a) 95%CI: 95% confidence interval.
b) Skin color: Asian and indigenous with only one case each.
c) Total missing: 71.
Among the interviewed individuals, 92.1% referred having eaten fried foods up to two days a week, more than half of them referred having reduced salt intake over the previous year (57.3%), 51.7% ate sugar and sweets up to two days a week and 40.2% practiced sufficient physical activity (Figure 2).
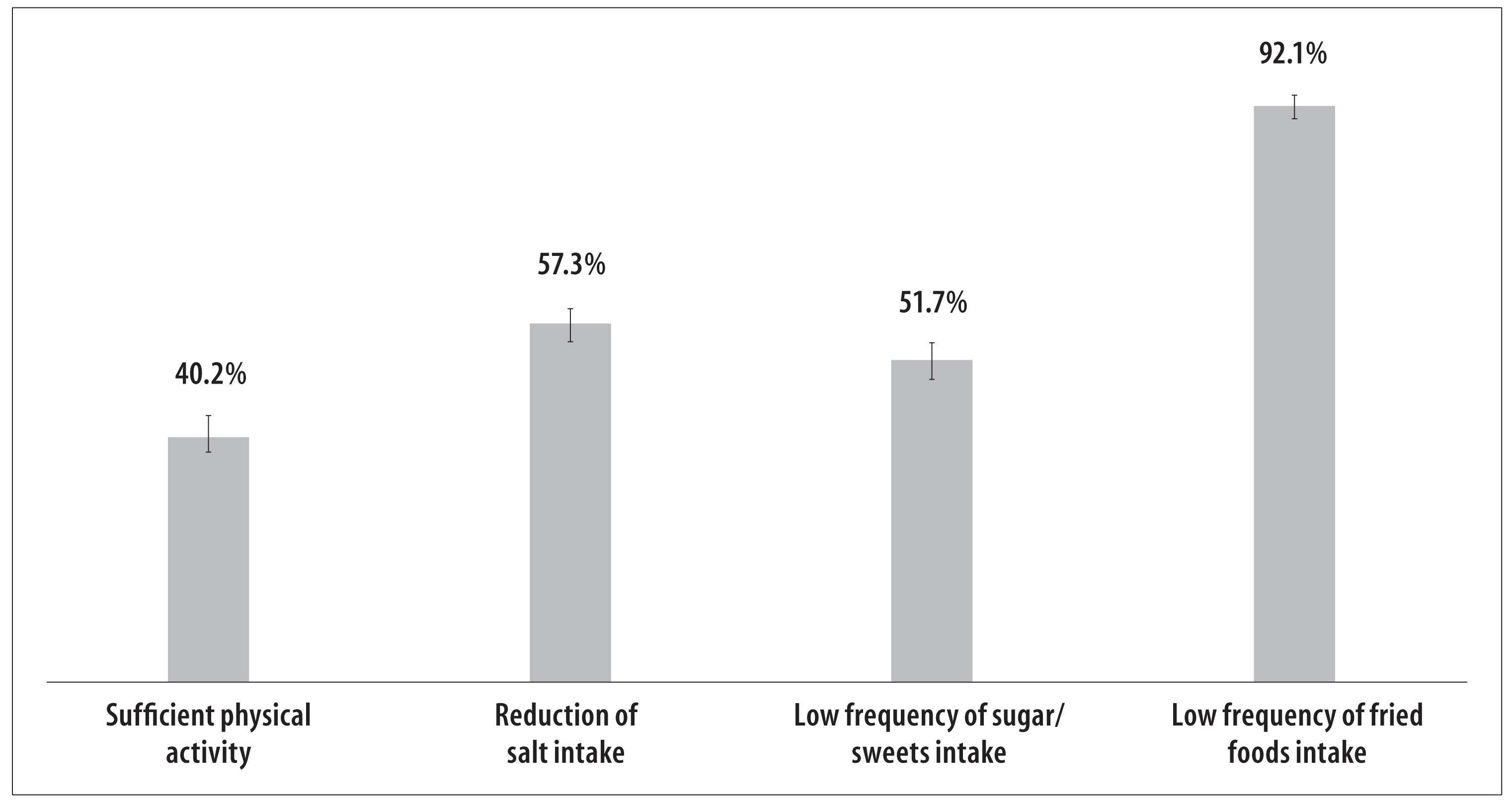
Figure 2 - Prevalence of sufficient physical activity, reduction of salt intake over the previous year and low frequency of sweets and fried foods intake on the previous seven days, among the elderly (n=1,281), Pelotas, Rio Grande do Sul, 2014
Table 2 shows the crude and adjusted analyses of the reports on reduction of salt intake, frequency of sugar and fried foods intake and physical activity in relation to receiving counseling by health care professionals. After the adjustments, elderly individuals who received guidance to reduce salt intake had 63% more probability to actually reduce it over the previous year (PR 1.63; 95%CI 1.40;1.90). Elderly individuals who received guidance on the reduction of sugar and sweets intake had greater prevalence (PR 1.21; 95%CI 1.07;1.36) to refer the consumption of these foods less frequently over the previous seven days, compared to those who did not receive such guidance from health care professionals. Health care professionals’ advice to reduce fat intake was not associated with a lower frequency of fried foods intake over the previous seven days. Sufficient practice of physical activity was higher among elderly individuals who received guidance on this habit (PR 1.18; 95%CI 1.02;1.36).
Table 2 - Crude and adjusted analysis between receiving counseling and healthy behaviors among the elderly (n=1,281) who had visited a health care professional over the previous year, Pelotas, Rio Grande do Sul, 2014
| Guidance | % | Healthy Behaviors a | |||
|---|---|---|---|---|---|
| Crude Analysis | Adjusted analysis b | ||||
| PR c (95%CI) | Valor-p d | PR c (95%CI e ) | p-value d | ||
| Reduction of salt intake | <0.001 | <0.001 | |||
| No | 39.3 | 1.00 | 1.00 | ||
| Yes | 68.4 | 1.74 (1.52;2.00) | 1.63 (1.40;1.90) | ||
| Reduction of sugar and sweets intake | <0.001 | 0.002 | |||
| No | 44.9 | 1.00 | 1.00 | ||
| Yes | 58.4 | 1.30 (1.17;1.44) | 1.21 (1.07;1.36) | ||
| Reduction of fat intake | 0.411 | 0.946 | |||
| No | 91.3 | 1.00 | 1.00 | ||
| Yes | 92.6 | 1.01 (0.98;1.05) | 1.00 (0.96;1.04) | ||
| Physical activity | 0.005 | 0.020 | |||
| No | 35.7 | 1.00 | 1.00 | ||
| Yes | 43.4 | 1.21 (1.06;1.39) | 1.18 (1.02;1.36) | ||
a) Reduction of salt intake over the previous year, sweets/fried food intake up to two days a week and ≥ 150 minutes of physical activity per week.
b) Adjustments for sex, age, ethnicity/skin color, marital status, economic classification according to the Brazilian Market Research Association(ABEP), hypertension, diabetes mellitus, high cholesterol, number of visits and type of medical care.
c) PR: prevalence ratio.
d) Wald test for heterogeneity.
e) 95%CI: 95% confidence interval.
Discussion
In this study, we observed that the frequency of guidance on healthy habits was lower than 65.0%, an inferior percentage compared to those found in developed countries. It is important to point out that the studies were conducted with individuals who had some chronic condition.8,9 The findings of this study suggest that receiving some sort of guidance seems to help reduce salt, sugar and sweets intake and increases the frequency of physical activity among the elderly. However, we could not identify the same influence on the reduction of fat intake.
Considering that elderly people use health services4 a lot and that health care professionals are responsible for health education in every possible opportunity,1,2,5 one can note that guidance is rarely given in the health care context.26 Another challenge is that the elderly population has to achieve these healthy habits, but in many cases they do not have proper access to healthy food and practices.21 Moreover, they find many barriers to engage in healthy habits, such as the guidance by professionals which must be characterized by health education and not simply information.26,27
Guidance on healthy habits given by health care professionals influences people’s habits and can encourage changes in their lifestyle.8,9,13 According to this study, elderly individuals who were advised by health care professionals showed less frequency of sugar intake, reported reduction on salt intake and greater frequency of physical activity, compared to elderly individuals who were not advised. These findings reinforce the hypothesis, present in literature, of the association between guidance by professionals and the possibility of achieving healthy habits.8,9,13,14,18
The effective completion of these recommendations in a personal level is as important as the counseling given by health care professionals on healthy habits.13 Regardless of recognizing the importance of healthy eating and the practice of physical activity, the Brazilian population faces great difficulty trying to maintain a healthier lifestyle,7,11 especially among the elderly. In this study, we were able to identify that just over 90% of the interviewed individuals reported reduction of fried foods intake and only 40% reported practicing physical activity, which shows that the profile of healthy habits is not constant for every behavior. We highlight the need to continuously promote these habits in order to raise more awareness for the population on the importance of a healthy lifestyle.21,27 Besides, the possible problems regarding healthy and quality foods can hinder or stop individuals from following the health care professionals’ guidance.
According to a study conducted in Belo Horizonte with adults and elderly individuals from a primary health care unit (PHU), about 63.0% of the individuals who received guidance on healthy eating and practice of physical activity reported following them.12 In the same study, the most mentioned obstacles to follow these guidance were lack of time, difficulty in changing habits and financial issues;12 these obstacles were also highlighted by Toledo et al.13 When the objective is to educate for health while intervening on people’s behaviors,17 we must consider these obstacles among the aspects to be addressed when the individual is in the health services,13,26,27 helping to achieve such guidance.
Another important issue refers to the guidance by health care professionals. A recent 2014 study performed in the Primary Health Care identified difficulties in the supply of recommendations of physical activity by the evaluated health care professionals. The authors of the study mentioned pointed out the need to invest on these professionals’ training concerning the promotion of a healthy lifestyle.29 Professional training - in every level of health care-needs investments to promote healthy habits and prevent diseases and their injuries. Handicaps in these actions can result in less engagement of the patient in adopting these habits.
It is also important to highlight the possible key factors of the guidance and adoption of healthy behaviors: the first depends on the access to health services and the latter depends on healthy food and life behaviors.21,26-28 Socioeconomic level acts as a decisive factor of this association: individuals with a higher economic level use health services more frequently30 and have healthier life habits.28 Another large study observed that elderly individuals who belong to a social background with a higher economic level had greater probability to receive guidance to practice physical activity and control their weight.27 Also,in a study performed in Primary Health Care, it was clear that individuals who belonged to economic brackets A and B had greater probability to receive every recommendation analyzed herein.26 According to these findings, better socioeconomic conditions help people receive guidance from health care professionals on adopting healthy habits.
This study presents some limitations. Cross-sectional design can hamper the interpretation of associations, such as receiving guidance to reduce sugar and sweets intake and the frequency of intake. However, we did not intend to perform causal inferences, but verify the existence of an association between receiving guidance on healthy habits by health care professionals, such as a more adequate dietary behavior and practice of physical activity among the elderly. It is important to highlight the possibility of social desirability bias, which could lead to changes in the individual’s report: because the elderly individual received guidance before the studied period, in the time of the interview, he or she could report the ideal behavior to engage in a healthy lifestyle. However, we believe that the recall period of the guidance and behaviors (last year) would minimize this possible bias.
Furthermore, the lack of specific parameters in the literature to evaluate behavior after recommendations given by health care professionals hamper comprehension and comparability of the results.13 The frequency of sugar and fried foods intake was used as a proxy of sugar and fat intake, thus it does not constitute a global measurement of these macronutrients, instead, it is an approximation of real diet intake. Reduction of salt intake was assessed according to the perception of the interviewed individual instead of the real amount consumed. Since this study is part of a bigger survey, it was not possible to apply a food log that could evaluate the amount of salt intake with greater accuracy. Besides, the difficulty in evaluating salt intake is reported by other authors.29 The adequacy of behavior to the guidance given by health care professionals was also not examined in long-term, which is perhaps a better indicator of the effectiveness of these actions. Even if this guidance must be reinforced in every contact of the elderly individual with health services, this study can show the recall bias due to the period used in the questions. Since this bias could underestimate the prevalence of exposures, it could also be attenuated, since the median of appointments with health care professionals was 3 (standard deviation=1), allowing frequent contact of the elderly with health services and thus increasing the opportunities to receive guidance on healthy habits. Furthermore, elderly individuals who had three or more appointments over the previous year received more guidance(data not shown in tables).
Regardless of these limitations, the study brought improvements on this subject. Findings evidenced the importance of counseling on healthy habits in relation to the elderly individuals’ lifestyle. The usage of a significant sample in a medium-sized municipality can be considered a positive aspect, since most studies on this subject use baseline samples on the service provision area,13,26 which limits result extrapolation.
The results highlighted that counseling on healthy habits given by health care professionals over the last year was associated with reported reduction of salt intake, low frequency of sugar intake and greater practice of physical activity, which shows that this guidance can be important to promote a healthier lifestyle. Elderly people who received only one guidance, such as reducing salt intake, possible adopted a healthier lifestyle as a whole and not only regarding what was mentioned. That is, even if professionals do not advise as much as they should on reduction of fat intake, it is possible that a simple recommendation to reduce salt intake can influence other health behaviors, such as reduction of fat intake and other unhealthy habits a person had before receiving counseling from a health care professional. Longitudinal studies are necessary to prove this hypothesis.
It is important to emphasize that even though the guidance assessed in this study is of common knowledge, there is a lot of complexity involved so elderly people engage on a healthy lifestyle. Thus, although elderly people who received guidance to reduce salt, consume less sugar and sweets and practice more physical activity, it is recommend that healthy habits be investigated before and after these guidance to have a greater impact on the actions and policies already present in health services.
REFERENCES
1. World Health Organization. Envelhecimento ativo: uma política de saúde [Internet]. Brasília: Organização Pan-Americana da Saúde; 2005 [citado 2017 out 08]. 60 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/envelhecimento_ativo.pdf [ Links ]
2. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Secretaria de Atenção à Saúde. Política nacional de promoção da saúde [Internet]. 3. ed. Brasília: Ministério da Saúde; 2010 [citado 2017 mar 10]. 60 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/politica_nacional_promocao_saude_3ed.pdf [ Links ]
3. Andrade SSA, Stopa SR, Brito AS, Chueri PS, Szwarcwald CL, Malta DC. Prevalência de hipertensão arterial autorreferida na população brasileira: análise da Pesquisa Nacional de Saúde, 2013. Epidemiol Serv Saúde. 2015 abr-jun;24(2):297-304. [ Links ]
4. Lima-Costa MF, Loyola Filho AI, Matos DL. Tendências nas condições de saúde e uso de serviços entre idosos brasileiros: um estudo baseado na Pesquisa Nacional por Amostra de Domicílios (1998, 2003). Cad Saúde Pública. 2007 out;23(10):2467-78. [ Links ]
5. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Envelhecimento e saúde da pessoa idosa [Internet]. Brasília: Ministério da Saúde; 2007 [citado 2017 mar 10]. 192 p. (Série A. Normas e Manuais Técnicos); (Cadernos de Atenção Básica, n. 19). Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/abcad19.pdf [ Links ]
6. Moraes EN. Atenção à saúde do idoso: aspectos conceituais [Internet]. Brasília: Organização Pan-Americana de Saúde; 2012 [citado 2017 out 08]. 98 p. Disponível em: Disponível em: http://apsredes.org/pdf/Saude-do-Idoso-WEB1.pdf [ Links ]
7. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise de Situação de Saúde. Plano de ações estratégicas para o enfrentamento das doenças crônicas não transmissíveis (DCNT) no Brasil 2011-2022 [Internet]. Brasília: Ministério da Saúde; 2011 [citado 2017 jul 27]. 160 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/plano_acoes_enfrent_dcnt_2011.pdf [ Links ]
8. Walker RL, Gee ME, Bancej C, Nolan RP, Kaczorowski J, Joffres M, et al. Health behaviour advice from health professionals to Canadian adults with hypertension: results from a national survey. Can J Cardiol. 2011 Jul-Aug;27(2):446-54. [ Links ]
9. Agborsangaya CB, Gee ME, Johnson ST, Dunbar P, Langlois MF, Leiter LA, et al. Determinants of lifestyle behavior in type 2 diabetes: results of the 2011 cross-sectional survey on living with chronic diseases in Canada. BMC Public Health. 2013 May;13:451. [ Links ]
10. McNaughton SA. Advancing nutrition promotion research and practice. Nutr Diet. 2015 Dec;72(4):305-8. [ Links ]
11. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Guia alimentar para a população brasileira: promovendo a alimentação saudável [Internet]. Brasília: Ministério da Saúde; 2008 [citado 2017 mar 10]. 210 p. (Série A. Normas e Manuais Técnicos). Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/guia_alimentar_populacao_brasileira_2008.pdf [ Links ]
12. Santos RR, Horta PM, Souza CS, Santos CAS, Oliveira HBS, Almeida LMR, et al. Aconselhamento sobre alimentação e atividade física: prática e adesão de usuários da atenção primária. Rev Gaúcha Enferm. 2012 dez;33(4):14-21. [ Links ]
13. Toledo MTT, Abreu MN, Lopes ACS. Adesão a modos saudáveis de vida mediante aconselhamento por profissionais de saúde. Rev Saúde Pública. 2013 jun;47(3):540-8. [ Links ]
14. Kreuter MW, Chheda SG FCB. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000 May;9(5):426-33. [ Links ]
15. Greene GW, Fey-Yensan N, Padula C, Rossi SR, Rossi JS, Clark PG. Change in fruit and vegetable intake over 24 months in older adults: results of the SENIOR project intervention. Gerontologist. 2008 Jun;48(3):378-87. [ Links ]
16. Märki A, Bauer GB, Angst F, Nigg CR, Gillmann G, Gehring TM. Systematic counselling by general practitioners for promoting physical activity in elderly patients: a feasibility study. Swiss Med Wkly. 2006 Jul;136(29-30):482-8. [ Links ]
17. Burke L, Lee AH, Jancey J, Xiang L, Kerr DA, Howat PA, et al. Physical activity and nutrition behavioural outcomes of a home-based intervention program for seniors: a randomized controlled trial. Int J Behav Nutr Phys Act. 2013 Jan;10:14. [ Links ]
18. Andrade KA, Toledo MTT, Lopes MS, Carmo GES, Lopes ACS. Aconselhamento sobre modos saudáveis de vida na Atenção Primária e práticas alimentares dos usuários. Rev Esc Enferm USP. 2012 out;46(5):1117-24. [ Links ]
19. Instituto Brasileiro de Geografia e Estatística. Censo 2010 [Internet]. 2010 [citado 2017 mar 10]. Disponível Disponível em: https://censo2010.ibge.gov.br/ . [ Links ]
20. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância de Doenças e Agravos não Transmissíveis e Promoção da Saúde. Vigitel Brasil 2013: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico [Internet]. Brasília: Ministério da Saúde; 2014 [citado 2017 mar 10]. 164 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2013.pdf [ Links ]
21. Gomes AP, Soares ALG, Gonçalves H. Baixa qualidade da dieta de idosos: estudo de base populacional no sul do Brasil. Ciênc Saúde Coletiva. 2016 nov;21(11):3417-28. [ Links ]
22. World Health Organization. Global recommendations on physical activity for health [Internet]. Geneva: World Health Organization; 2010 [cited 2017 Mar 10]. 58 p. Disponível em: Disponível em: http://www.who.int/dietphysicalactivity/publications/9789241599979/en/ [ Links ]
23. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003 Aug;35(8):1381-95. [ Links ]
24. Associação Brasileira de Empresas de Pesquisa. Critério de classíficação econômica Brasil [Internet]. São Paulo: Associação Brasileira de Empresas de Pesquisa; 2014 [citado 2017 Mar 10]. 6 p. Disponível em: Disponível em: http://www.abep.org/criterio-brasil . [ Links ]
25. Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003 Oct;3:21. [ Links ]
26. Silva SM, Facchini LA, Tomasi E, Piccini R, Thumé E, Silveira DS, et al. Recebimento de orientação sobre consumo de sal, açúcar e gorduras em adultos: um estudo de base nacional. Rev Bras Epidemiol. 2013 dez;16(4):995-1004. [ Links ]
27. Flores TR, Nunes BP, Assunção MCF, Bertoldi AD. Hábitos saudáveis: que tipo de orientação a população idosa está recebendo dos profissionais de saúde? Rev Bras Epidemiol. 2016 jan-mar;19(1):167-80. [ Links ]
28. Soares ALG, França GVA, Gonçalves H. Disponibilidade domiciliar de alimentos em Pelotas (RS): uma abordagem do ambiente obesogênico. Rev Nutr. 2014 mar-abr;27(2):193-203. [ Links ]
29. Castro RSA, Giatti L, Barreto SM. Fatores associados à adição de sal à refeição pronta. Ciênc Saúde Coletiva. 2014 mai;19(5):1503-12. [ Links ]
30. Nunes BP, Thumé E, Tomasi E, Duro SMS, Facchini LA. Desigualdades socioeconômicas no acesso e qualidade da atenção nos serviços de saúde. Rev Saúde Pública. 2014 dez;48(6):968-76. [ Links ]
*This article was based on two Masters’ thesis by Thaynã Ramos Flores and Ana Luiza Gonçalves Soares, defended in November 2014 to the Postgraduate Program in Epidemiology of the Federal University of Pelotas, Rio Grande do Sul, Brazil. Financing: Program of Academic Excellence (PROEX) of the Coordination of Improvement of Higher Education Personnel (CAPES) and Foundation for Research Support of the State of Rio Grande do Sul (FAPERGS).
Received: June 14, 2017; Accepted: September 27, 2017











 texto em
texto em 


