Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.28 no.1 Brasília mar. 2019 Epub 12-Mar-2019
http://dx.doi.org/10.5123/s1679-49742019000100013
ORIGINAL ARTICLE
Evaluation of the implantation of the Mortality Information System in Pernambuco state, Brazil, in 2012*
1Universidade Federal de Pernambuco, Programa de Pós-Graduação em Saúde da Criança e do Adolescente, Recife, PE, Brasil
2Instituto de Medicina Integral Prof. Fernando Figueira, Programa de Pós-Graduação em Avaliação em Saúde, Recife, PE, Brasil
3Secretaria Estadual de Saúde de Pernambuco, Secretaria Executiva de Vigilância em Saúde, Recife, PE, Brasil
Objective:
to evaluate the implantation of the Mortality Information System (SIM) in Pernambuco, Brazil.
Methods:
this was an evaluation study; primary data (questionnaires) and secondary data (SIM) were used for the municipalities to estimate the degree of implantation (DI), comparing structure and process indicators with outcome indicators; data were consolidated by region and state.
Results:
SIM was partially implanted in the state (70.6%) and its regions (66.3% to 74.8%); 'management' (75.1%), 'issuing and filling in' (79.1%), and 'processing' (71.7%) were partially implanted; 'collection' (80.7%) was implanted; while 'distribution and control' (49.7%) and 'analysis and dissemination' (58.0%) had incipient implantation; more than 90% coverage was found for deaths with defined underlying causes, as well as for municipalities with monthly data transfer, and death certificates typed and sent on a timely basis; consistency was found between DI and outcome indicators, which improved as DI increased.
Conclusion:
SIM was found to be only partially implanted owing to inadequacies in distribution, control, analysis and dissemination, thus influencing unfavorably the effects observed.
Keywords: Health Evaluation; Health Information Systems; Vital Statistics; Mortality Registries
Introduction
The Mortality Information System (SIM), created in the 1970s, is frequently evaluated by means of quality attributes, with emphasis on reliability, completeness and coverage.1,2 These investigations seek to provide evidence of common obstacles, especially in the less developed regions of Brazil.3-5 However, highlighting specific dimensions of the system limits knowledge on the production of vital data and its level of deployment, with repercussions for information accuracy and use.6
The need for evaluations targeting the generation of information on SIM has been evidenced by studies aimed at identifying difficulties with its operationalization in the institutional environment.7,8 As a result, evaluations that consider the structure and process required to obtain data in the context of health services contribute positively to the use of theoretical and methodological principles of health evaluation in the improvement of information systems that undertake continuous recording.6,9,10
Evaluation of vital information system processes has enabled explanatory factors regardingthe results achieved to be specified. The potential of these analyses was expanded once they began to involve normative aspects as one of their steps.6,9 This methodological procedure has allowed the degree of structure and process adequacy to be determined, based on criteria and standards, as well as to identify whether expected results correspond to those observed in the context of services, in addition to making interventions and their way of operating more understandable.11
Although evaluative experiences have incorporated aspects of the operationalization of health information systems in the organizational environment,6,9 empirical gaps restrict knowledge as to the entire process of SIM data production, its specific problems and deployment implications, with regard to the results achieved. Analyzing the system from the perspective of its deployment may overcome the limitations of evaluations commonly carried out, the focus of which is restricted to results achieved, in addition to guiding actions aimed at improving structural and procedural aspects, with the possibility of having impact on the quality of the system.6,9
This study aimed to evaluate the implantation of SIM in Pernambuco, Brazil, in 2012.
Methods
This was an evaluation study based on implantation analysis, assessing the influence of SIM deployment variation on the results found.12 The strategy we adopted was a single case study13 in Pernambuco, both in relation to the state as a whole and also its health regions.
SIM is in operation in the Health Departments of the 185 municipalities of Pernambuco. These are distributed over 12 political-administrative regions corresponding to the state’s health regions. The municipal health departments are responsible for collecting, processing, transmitting and disseminating information on mortality, which is produced based on 'Death Certificates’ issued. The flow of information is hierarchical: data is sent by municipal SIM managers to the State Health Department and to the Ministry of Health.1
In this study, we included 184 of the state’s municipalities and excluded only one, as it does not have technicians and managers to implement and manage SIM routines. Our evaluation was carried out in four stages:
Stage 1 - Updating the SIM logic model
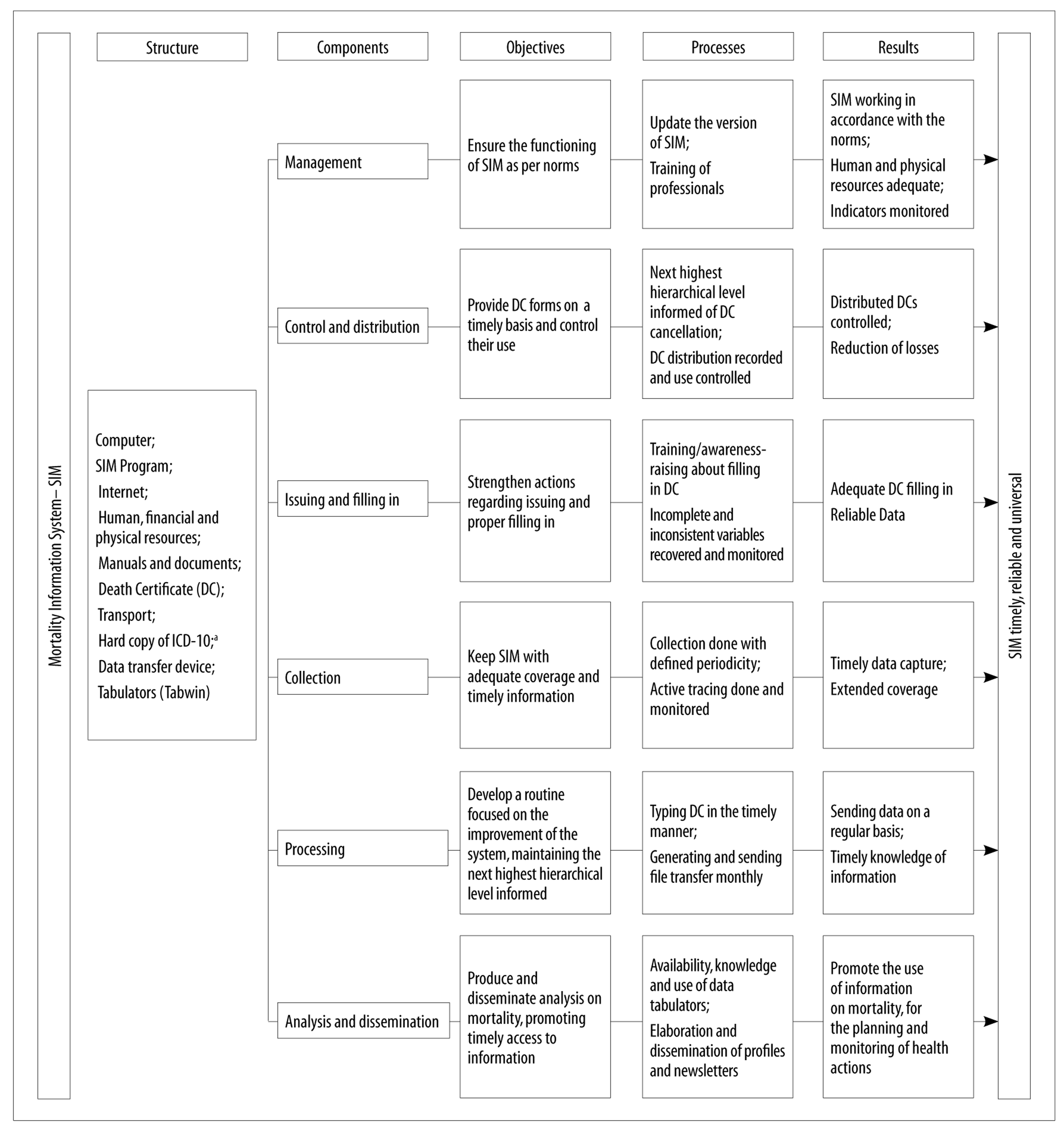
In order to be able to detail the intervention assessed, the previously prepared14 SIM logic model was updated using official system documents in a normative approach that included Ministerial Ordinances No. 116/2009, No. 17082013 and No. 47/2016, Death Certificate procedure and completion manuals, and the planning of actions undertaken in the different spheres of SIM system management. Together these components covered the structure dimension (human and physical resources) and the process dimension (activities performed), divided into six components involved in the generation of information: management; distribution and control; issuing and filling in; collection; processing; and analysis and dissemination (Figure 1).
Stage 2 - Preparation of the matrix of indicators and judgment criteria, and data collection
The indicator matrix and judgment criteria were prepared based on the SIM system logic model. The indicators were selected taking into consideration content validity, its relevance, availability, ease of retrieval, simplicity of calculation and timeliness. Structure and process indicators were established for each component of the logic model expressing the degree of implantation and results. Parameters derived from norms were defined for the indicators of structure and process, when such norms were available in institutional documents of the Ministry of Health and/or the Pernambuco State Health Department. If the norm did not contain a clear definition, the criteria were empirically derived according to the researchers’ judgment and stipulated in accordance with the service routine.
The variables and indicators are shown in (Figure 2), a matrix of 76 indicators distributed according to components: 23 for structure, 33 for process and 20 for the results, with their respective judgment criteria. Based on the indicators selected, we created the data collection instrument according to the SIM system components that were to be evaluated.
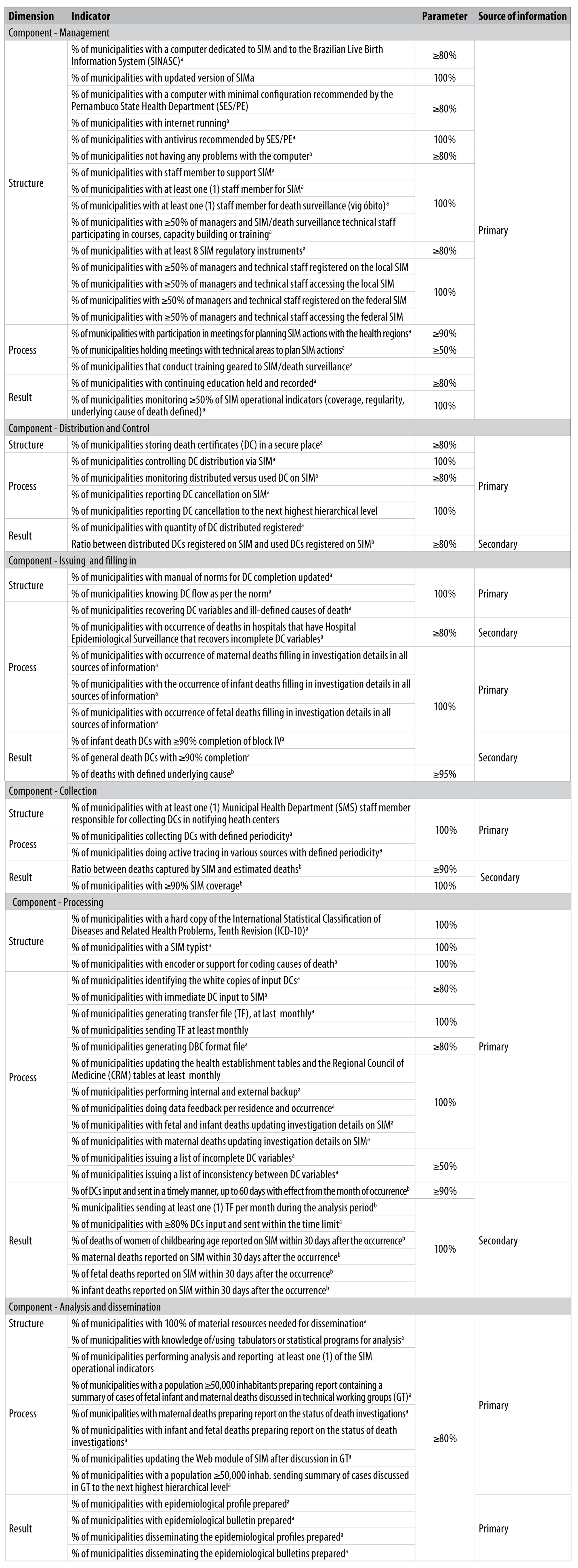
a) Source of empirical verification.
b) Source of normative verification.
Figure 2 - Matrix of Mortality Information System (SIM) indicators and judgment criteria, Pernambuco, 2012
The primary data were collected in November and December 2013 - relating to information for the year 2012 - by administering a structured questionnaire with those responsible for SIM in the municipalities studied, in addition to direct observation of structural and procedural aspects in all the municipal health departments included in the study. The secondary data, relating to deaths occurring in 2012, were retrieved from the Pernambuco state SIM database. The information obtained through the primary and secondary data were consolidated by health region and for the state as a whole, and included in the indicators that informed the evaluation of the degree of SIM implantation and the influence of this on results.
Stage 3 - Classification of degree of implantation
We used structure and process indicators to define the degree of implantation. Each component was classified and, once this had been done, we defined the degree of SIM implantation in the state and its health regions. Each indicator was obtained by calculating the ratio between the scores achieved and scores expected with regard to the number of municipalities having physical or material resources and having carried out activities. The degree of SIM implantation corresponded to the ratio between the sum of the degrees of implantation achieved and expected per system component.
Degree of implantation was classified as being ‘implanted’ when percentages of 80.0 to 100.0% were achieved, ‘partially implanted’ (60.0 to 79.9%), 'incipient' (40.0 to 59.9%) and 'not implanted' (<40.0%), as judged by the authors based on a previous study on SIM.14
Stage 4 - Analysis of the results produced and analysis of the influence of degree of implantation on them
To evaluate the results produced, we calculated the ratio between the scores achieved and those expected for each result indicator. These were analyzed by taking the result for each system component, compared to the indicator matrix (Figure 2). The degree of implantation as classified by SIM component in Stage 3, was compared with the result indicators based on the system logic model, establishing plausible relations for the identification of elements that brought influence to bear on the scope of the results produced.
Considering the control of biases, the strategy used to increase the rigor of the study was the triangulation of information related to the structure and process dimensions, by (i) administering a questionnaire with the participants and (ii) direct observation of SIM operationalization in the municipal health departments by following a checklist.
The study protocol was approved by the Professor Fernando Figueira Institute of Integral Medicine Human Research Ethics Committee: Opinion No. 2,457.367 dated 27 December 2017; Certification of Submission for Ethical Appraisal (CAAE) No. 79846017.3.0000.5201.
Results
SIM was found to be partially implanted in Pernambuco (70.6%), varying between 66.3 and 74.8% according to health region. Similarly, its 'management' (75.1%), 'issuing and filling in' (79.1%) and 'processing' (71.7%) components were found to be partially implanted. The 'collection' component was 'implanted' in the state (80.7%) and in most regions, with the exception of five, three of which were 'partially implanted' and two had 'incipient' implantation. Implantation of the 'distribution and control' component was 'incipient' in the state as a whole (49.7%) and 'not implanted’ in three regions, while the 'analysis and dissemination' component was 'incipient' in the state as a whole (58.0%) and partially implanted in five of its regions (Table 1).
Table 1 - Degree of implantation (%) of the Mortality Information System (SIM) by components and full scope, in the state and its health regions, Pernambuco, 2012
| Component | Health Regions | Pernambuco | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | VII | VIII | IX | X | XI | XII | ||
| Management | 67.4 | 83.9 | 78.0 | 67.9 | 76.7 | 79.5 | 76.2 | 72.2 | 80.3 | 74.3 | 82.2 | 70.0 | 75.1 |
| Distribution and control | 51.0 | 64.0 | 25.5 | 67.5 | 51.0 | 52.3 | 17.1 | 51.4 | 23.6 | 60.0 | 52.0 | 44.0 | 49.7 |
| Issuing and filling in | 88.8 | 77.1 | 89.2 | 72.2 | 78.3 | 75.3 | 78.6 | 81.8 | 80.6 | 75.0 | 75.0 | 73.8 | 79.1 |
| Collection | 63.5 | 80.0 | 100.0 | 83.3 | 75.0 | 51.7 | 61.9 | 93.3 | 100.0 | 91.2 | 57.7 | 96.4 | 80.7 |
| Processing | 74.7 | 67.6 | 71.8 | 75.3 | 68.3 | 70.3 | 68.7 | 69.0 | 81.3 | 75.3 | 66.7 | 64.3 | 71.7 |
| Analysis and dissemination | 70.2 | 53.2 | 52.5 | 61.5 | 50.9 | 50.0 | 68.4 | 61.5 | 66.2 | 50.0 | 51.3 | 56.1 | 58.0 |
| SIM | 70.5 | 73.2 | 71.1 | 70.5 | 69.3 | 69.4 | 67.0 | 70.2 | 74.8 | 71.9 | 70.0 | 66.3 | 70.6 |
Note: Degree of implantation - implanted (80.0 to 100.0%); partially implanted (79.9 to 60%); incipient implantation (40.0 to 59.9%); not implanted (<40.0%).
The 'management' component showed that 69.6% of the state’s municipalities monitored at least 50.0% of the operational indicators; and that 62.0% carried out continuing education, varying between 35.0 and 100.0% between regions (Table 2). The 'distribution and control' component showed that 90.1% of Death Certificates issued and registered were input to SIM, this result being greater than or equal to 79.0% between the health regions. The 'issuing and filling in' component in relation to the state as a whole had 94.9% of deaths with a defined underlying cause, with similar values for all but three health regions. Consolidated Death Certificate completeness for general deaths for the state as a whole was 51.7%; while block IV relating to infant deaths was 66.8% complete, with higher results in three regions. The 'collection' component showed 100% coverage in the state as a whole and also in its regions; the proportion of municipalities with coverage above 90% for this component was 82.1%.
Table 2 - Degree of implantation (%) and result indicators (%) of the Mortality Information System (SIM) by component, in the state and its health regions, Pernambuco, 2012
| DI | Indicator | Health Regions | Pernambuco | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | VII | VIII | IX | X | XI | XII | |||
| Component - Management | ||||||||||||||
| 75.1 | % of municipalities monitoring ≥50% of SIM operational indicators | 90.0 | 45.0 | 45.5 | 100.0 | 15.0 | 100.0 | 85.7 | 85.7 | 72.7 | 100.0 | 100.0 | 10.0 | 69.6 |
| % of municipalities with continuing education held and registered | 35.0 | 70.0 | 95.5 | 50.0 | 50.0 | 61.5 | 100.0 | 57.1 | 54.5 | 75.0 | 70.0 | 50.0 | 62.0 | |
| Component - Distribution and Control | ||||||||||||||
| 49.7 | % of municipalities with quantity of death certificates (DC) distributed registered | 40.0 | 100.0 | 72.7 | 90.6 | 85.0 | 69.2 | 42.9 | 42.9 | 9.1 | 75.0 | 80.0 | 30.0 | 68.5 |
| Ratio between DCs distributed recorded on SIM and DCs used recorded on SIM | 91.4 | 90.9 | 88.1 | 90.2 | 86.4 | 85.9 | 84.4 | 92.1 | 79.0 | 86.5 | 90.1 | 89.7 | 90.1 | |
| Component - Issuing and filling in | ||||||||||||||
| 79.1 | % of child death DCs with ≥90% completion of block IV | 75.7 | 62.7 | 53.5 | 74.0 | 59.3 | 62.0 | 44.4 | 53.3 | 60.2 | 50.0 | 55.8 | 68.2 | 66.8 |
| % of general death DCs with ≥90% completion | 59.6 | 45.8 | 48.5 | 54.4 | 40.9 | 41.8 | 50.1 | 43.3 | 23.9 | 30.8 | 32.5 | 52.2 | 51.7 | |
| % of deaths with defined underlying cause | 98.4 | 96.3 | 95.8 | 93.5 | 86.7 | 84.3 | 90.7 | 79.5 | 94.4 | 96.6 | 94.2 | 94.2 | 94.9 | |
| Component - Collection | ||||||||||||||
| 80.7 | Ratio between deaths captured by SIM and estimated deaths | 98.3 | 103.0 | 97.9 | 99.7 | 105.6 | 105.9 | 96.4 | 92.9 | 104.7 | 99.8 | 97.7 | 102.0 | 100.0 |
| % of municipalities with ≥90% SIM coverage | 95.0 | 75.0 | 81.8 | 75.0 | 90.0 | 92.3 | 42.9 | 85.7 | 81.8 | 83.3 | 70.0 | 100.0 | 82.1 | |
| Component- Processing | ||||||||||||||
| 71.7 | % of municipalities with at least one (1) transfer file sent per month during the period of analysis | 97.1 | 93.3 | 91.7 | 95.3 | 95.4 | 91.0 | 97.6 | 94.0 | 93.9 | 87.5 | 98.3 | 97.5 | 94.3 |
| % of DCs input and sent a in timely manner, up to 60 days with effect from the month of occurrence | 90.0 | 86.1 | 82.4 | 92.1 | 87.3 | 88.7 | 94.0 | 91.9 | 98.6 | 91.5 | 92.2 | 89.0 | 90.1 | |
| % of municipalities with ≥80% of DCs input and sent on time | 85.0 | 50.0 | 54.5 | 75.0 | 80.0 | 69.2 | 71.4 | 85.7 | 90.9 | 83.3 | 90.0 | 80.0 | 73.9 | |
| % of deaths of women of childbearing age reported on SIM within 30 days of occurrence | 31.8 | 39.5 | 32.1 | 51.1 | 32.9 | 47.3 | 78.0 | 75.5 | 56.0 | 54.4 | 57.0 | 29.8 | 40.2 | |
| % of maternal deaths reported on SIM within 30 days of occurrence | 18.8 | NA | 22.2 | - | - | NA | 100.0 | 100.0 | 62.5 | NA | - | - | 26.2 | |
| % of fetal deaths reported on SIM within 30 days of occurrence | 33.1 | 36.0 | 37.6 | 66.7 | 24.7 | 61.5 | 90.6 | 92.1 | 51.6 | 66.7 | 82.9 | 42.2 | 48.1 | |
| % of infant deaths reported on SIM within 30 days of occurrence | 25.5 | 23.2 | 26.8 | 50.2 | 22.2 | 48.8 | 80.9 | 89.2 | 62.5 | 27.5 | 64.9 | 19.7 | 38.6 | |
| Component - Analysis and dissemination | ||||||||||||||
| 58.0 | % of municipalities with epidemiological profile prepared | 75.0 | 10.0 | 18.2 | 62.5 | 25.0 | 38.5 | 14.3 | 28.6 | 36.4 | 25.0 | 20.0 | 10.0 | 34.8 |
| % of municipalities with epidemiological bulletin prepared | 50.0 | 10.0 | 13.6 | 50.0 | 15.0 | 38.5 | 14.3 | 57.1 | 36.4 | 33.3 | 30.0 | 30.0 | 31.5 | |
| % of municipalities disseminating epidemiological profiles prepared | 55.0 | 10.0 | 18.2 | 59.4 | 25.0 | 30.8 | 14.3 | 28.6 | 36.4 | 25.0 | 20.0 | 10.0 | 31.5 | |
| % of municipalities that disseminating epidemiological bulletins prepared | 45.0 | 10.0 | 13.6 | 46.9 | 15.0 | 30.8 | 14.3 | 57.1 | 36.4 | 33.3 | 30.0 | 30.0 | 29.9 | |
Legend:
DI: degree of implantation.
NA: not applicable.
The 'processing' component showed 94.3% of municipalities with monthly data transfer and 90.1% of Death Certificated input and forwarded on a timely basis, with similar results between the regions. The indicators for the notification of deaths of women of childbearing age, maternal, fetal and infant deaths within 30 days after death remained below 50% in the state as a whole. Four regions did not notify maternal death in a timely manner. The 'analysis and dissemination' indicators showed a proportion of less than 40%, in both the state and in most regions (Table 2).
Discussion
SIM was found to be partially implanted in Pernambuco, with variations between the components of the system according to health regions, demonstrating consistency with the results found: the greater the degree of implantation, the better the results. Incomplete achievement of SIM’s objectives arises from inadequacies in the distribution, control, analysis and dissemination of data, although the system has been established for more than 30 years and despite recognition of its relevance for the analysis of the health situation and its monitoring and evaluation.1-3
The fact of state-level management having updated the SIM logic model and prepared the matrix of indicators, without the participation of the federal level of the system, may have bestowed a transitory nature on the judgment criteria so that they may require periodic revisions. In spite of the impossibility of the study results being extrapolated, the internal validity of the logic model of the system is explicit owing to a theoretical construct that shows the relations of interdependence between the historically constructed components and their contents, so that it can be replicated in other contexts, with adjustments.12,13
The 'distribution and control' and 'analysis and dissemination' components showed reduced adherence of procedural indicators to established standards, pointing to a not very satisfactory work process. This finding, while being similar to that found for the Brazilian Live Birth Information System (SINASC) in the municipalities of Minas Gerais,9 is opposite to that found for SISNASC in Pernambuco, where structural problems prevailed.6
Performing analysis by component identified shortcomings, such as municipalities with low control of Death Certificates distributed, used and canceled, which can favor misuse, loss and flow deviation. This insufficient control over the Certificate forms not only increases the cost of production and meeting the needs of the system, but also reveals reduced management capacity. In the same way, studies of active tracing indicate problems with the operationalization of vital information systems, such as inadequate flows and use of non-official forms, reflecting little normative knowledge, signaling the need to enhance the capacity of professionals responsible for the operationalization of these systems.4,6,7,15
Even though inter and intra-regional differences were revealed in SIM coverage in the municipalities evaluated, high system data capture points to an intensive data collection work process. This finding corroborates the evidence about the expansion of SIM coverage in the state of Pernambuco, with repercussions on the reliability of using its data to calculate mortality indicators,16-18 thus allowing adequate monitoring of national and international pacts.19
The better results found for indicators of regular batch transfer and data sending, which are linked to funding being released, to the detriment of timely notification of deaths of women of childbearing age, and maternal, fetal and infant deaths, express the preponderance of financial rationality over the epidemiological situation with regard to SIM processing. These findings are similar to those of a previous study, focused on small-sized municipalities of the state of Rio Grande do Sul.20 Delay in knowledge of reportable events hinders surveillance actions, as well as the reorientation of care and health services to meet the needs of the population,21,22 frequently limiting the scope of municipal actions, inadequately directed towards collection and transmission of data to other health management levels.23
Death Certificate incompleteness, scant dissemination of information and reduced continuing education found in Pernambuco’s health regions, resulting from the overvaluation of data collection and transmission routines, are related to the lack of teams and lack of technical qualification, thus hindering the consolidation of the system.20,23 As expected, the better filling in of Death Certificates, found in more developed areas of the metropolitan region of Recife (the state capital) and its surrounding territories as well as in the state’s larger municipalities, contrasted with Death Certificate completeness found in regions and localities with lower access to health services, lower access to health professional capacity building and lower access to health surveillance services recovering data variables.24-26
The results of the 'issuing and filling in', 'collection' and 'processing' components of the state SIM system are linked to the influence of the degree of implantation achieved, reflecting adherence by municipalities to the system’s operational routines. Conversely, the lower consistency of the 'management', 'distribution and control' and 'analysis and dissemination' components signals restrictions in managerial activities, given the inadequate training of technical staff, inadequate planning and monitoring of actions and information dissemination. These findings reflect the centralizing and fragmented conception of health information systems, historically designed to establish a network of local production of information that respond to national policies.1,27
Notwithstanding the role of executing the actions promoting the empowerment of municipal management,23 such decentralization does not just mean deconcentration of activities but also the sharing of decision-making power, thus promoting management and work process autonomy.27 Empowering health regions and municipalities technically and administratively would be a suitable alternative for consolidating SIM. This procedure, combined with the incorporation of new routines, favors the operationalization of the system, with a reduction of omission, overlap or partial execution of actions.6,28
SIM was found to be partially implemented in the state of Pernambuco, due to inadequacies in the distribution, control, analysis and dissemination of data, negatively influencing the effects observed, while data collection, issuing and filling in obtained the best scores. SIM’s objectives can be achieved by reorganizing the entire data production process, particularly within services, where health care is provided, and where deaths occur. To this end, additional investments are needed in the health service infrastructure, in strengthening of hospital epidemiology hubs and improving the work process. Such initiatives, coupled with periodic evaluations, are indispensable for the qualification of vital information systems and, therefore, for ensuring accuracy in the analysis of the health conditions of the population.29
REFERENCES
1. Mello Jorge MHP, Laurenti R, Gotlieb SLD. Avaliação dos sistemas de informação em saúde no Brasil. Cad Saúde Colet [Internet]. 2010 [citado 2019 jan 14];18(1):7-18. Disponível em: Disponível em: http://www.cadernos.iesc.ufrj.br/cadernos/images/csc/2010_1/artigos/Modelo%20Livro%20UFRJ%201-a.pdf [ Links ]
2. Lima CRA, Schramm JMA, Coeli CM, Silva MEM. Revisão das dimensões de qualidade dos dados e métodos aplicados na avaliação dos sistemas de informação em saúde. Cad Saúde Pública [Internet]. 2009 out [citado 2019 jan 14];25(10):2095-109. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v25n10/02.pdf . Doi: 10.1590/S0102-311X2009001000002 [ Links ]
3. Lima EEC, Queiroz BL. Evolution of the deaths registry system in Brazil: associations with changes in the mortality profile, under-registration of death counts, and ill-defined causes of death. Cad Saúde Pública [Internet]. 2014 Aug [cited 2019 Jan 14];30(8):1721-30. Available from: Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2014000801721 . Doi: 10.1590/0102-311X00131113 [ Links ]
4. Frias PG, Szwarcwald CL, Morais Neto OL, Leal MC, Cortez-Escalante JJ, Souza Júnior PRB, et al. Utilização das informações vitais para a estimação de indicadores de mortalidade no Brasil: da busca ativa de eventos ao desenvolvimento de métodos. Cad Saúde Pública [Internet]. 2017 [citado 2019 jan 14];33(3):e00206015. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v33n3/1678-4464-csp-33-03-e00206015.pdf . Doi: 10.1590/0102-311x00206015 [ Links ]
5. Szwarcwald CL, Frias PG, Souza Júnior PRB, Almeida WS, Morais Neto OL. Correction of vital statistics based on a proactive search of deaths and live births: evidence from a study of the North and Northeast regions of Brazil. Popul Health Metr [Internet]. 2014 Jun [cited 2019 Jan 14];12:16. Available from: Available from: https://www.ncbi.nlm.nih.gov/pubmed/24966804 . Doi: 10.1186/1478-7954-12-16 [ Links ]
6. Pereira CCB, Vidal AS, Carvalho PI, Frias PG. Avaliação da implantação do Sistema de Informações sobre Nascidos Vivos (Sinasc) em Pernambuco. Rev Bras Saúde Matern Infant [Internet]. 2013 jan-mar [citado 2019 jan 14];13(1):39-49. Disponível em: Disponível em: http://www.scielo.br/pdf/rbsmi/v13n1/a05v13n1.pdf . Doi: 10.1590/S1519-38292013000100005 [ Links ]
7. Figueiroa BQ, Vanderlei LCM, Frias PG, Carvalho PI, Szwarcwald CL. Análise da cobertura do Sistema de Informações sobre Mortalidade em Olinda, Pernambuco, Brasil. Cad Saúde Pública [Internet]. 2013 mar [citado 2019 jan 14];29(3):475-84. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v29n3/a06v29n3.pdf . Doi: 10.1590/S0102-311X2013000300006 [ Links ]
8. Almeida WS, Szwarcwald CL, Frias PG, Souza Júnior PRB, Lima RB, Rabello NetoDL, et al. Captação de óbitos não informados ao Ministério da Saúde: pesquisa de busca ativa de óbitos em municípios brasileiros. Rev Bras Epidemiol [Internet]. 2017 abr-jun [citado 2019 jan 14];20(2):200-11. Disponível em: Disponível em: http://www.scielo.br/pdf/rbepid/v20n2/1980-5497-rbepid-20-02-00200.pdf . Doi: 10.1590/1980-5497201700020002 [ Links ]
9. Guimarães EAA, Hartz ZMA, Loyola Filho AI, Meira AJ, Luz ZMP. Avaliação da implantação do Sistema de Informação sobre Nascidos Vivos em municípios de Minas Gerais, Brasil. Cad Saúde Pública [Internet]. 2013 out [citado 2019 jan 14];29(10):2105-18. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v29n10/a26v29n10.pdf . Doi: 10.1590/0102-311X00116312 [ Links ]
10. Minto CM, Alencar GP, Almeida MF, Silva ZP. Descrição das características do Sistema de Informações sobre Mortalidade nos municípios do estado de São Paulo, 2017. Epidemiol Serv Saúde [Internet]. 2017 out-dez [citado 2019 jan 14];26(4):869-80. Disponível em: Disponível em: http://www.scielo.br/pdf/ress/v26n4/2237-9622-ress-26-04-00869.pdf . Doi: 10.5123/S1679-49742017000400017 [ Links ]
11. Hartz ZMA, Cruz M, Craveiro I, Dias S. Estratégia interinstitucional (IHMT/Fiocruz) para fortalecimento da capacidade avaliativa nos países da CPLP: foco nos estudos de implementação para avaliação do PECS. An Inst Hig Med Trop [Internet]. 2016 [citado 2019 jan 14];15(Supl 1):S81-7. Disponível em: Disponível em: https://run.unl.pt/bitstream/10362/36667/2/Estrat_gia_interinstitucional_IHMT_Fiocruz.pdf [ Links ]
12. Champagne F, Brousselle A, Hartz ZMA, Contandriopoulos AP, Denis JL. A análise de implantação. In: Brousselle A, Champagne F, Contandriopoulos AP, Hartz ZMA, organizadores. Avaliação, conceitos e métodos. Rio de Janeiro: Fiocruz; 2011. p. 217-38. [ Links ]
13. Yin RK. Estudo de caso: planejamento e métodos. 5. ed. Porto Alegre: Bookman; 2015. [ Links ]
14. Carvalho PI, Frias PG, Vidal SA. Estudo de avaliabilidade do sistema de informações sobre mortalidade em âmbito estadual. In: Samico I, Felisberto E, Frias PG, Espírito Santo ACG, Hartz Z, organizadores. Formação profissional e avaliação em saúde. Rio de Janeiro: MedBook; 2015. v. 1, p. 283-308. [ Links ]
15. Frias PG, Pereira PMH, Andrade CLT, Szwarcwald CL. Sistema de Informações sobre mortalidade: estudo de caso em municípios com precariedade dos dados. Cad Saúde Pública [Internet]. 2008 out [citado 2019 jan 14];24(10):2257-66. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v24n10/07.pdf . Doi: 10.1590/S0102-311X2008001000007 [ Links ]
16. Almeida WS, Szwarcwald CL. Adequação das informações de mortalidade e correção dos óbitos informados a partir da pesquisa de busca ativa. Ciên Saúde Colet [Internet]. 2017 out [citado 2019 jan 14];22(10):3193-203. Disponível em: Disponível em: http://www.scielo.br/pdf/csc/v22n10/1413-8123-csc-22-10-3193.pdf . Doi: 10.1590/1413-812320172210.12002016 [ Links ]
17. Frias PG, Pereira PMH, Andrade CLT, Lira PIC, Szwarcwald CL. Avaliação da adequação das informações de mortalidade e nascidos vivos no Estado de Pernambuco, Brasil. Cad Saúde Pública [Internet]. 2010 abr [citado 2019 jan 14];26(4):671-81. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v26n4/10.pdf . Doi: 10.1590/S0102-311X2010000400010 [ Links ]
18. Rodrigues M, Bonfim C, Frias PG, Braga C, Gurgel IGD, Medeiros Z. Diferenciais na adequação das informações de eventos vitais nos municípios de Pernambuco, 2006-2008. Rev Bras Epidemiol [Internet]. 2012 jun [citado 2019 jan 14];15(2):275-84. Disponível em: Disponível em: http://www.scielo.br/pdf/rbepid/v15n2/05.pdf . Doi: 10.1590/S1415-790X2012000200005 [ Links ]
19. Abou Zahr C, Savigny D, Mikkelsen L, Setel PW, Lozano R, Nichols E, et al. Civil registration and vital statistics: progress in the data revolution for counting and accountability. Lancet [Internet]. 2015 Oct [cited 2019 Jan 14];386(10001):1373-85. Available from: Available from: https://www.ncbi.nlm.nih.gov/pubmed/25971224 . Doi: 10.1016/S0140-6736(15)60173-8 [ Links ]
20. Vidor AC, Fisher PD, Bordin R. Utilização dos sistemas de informação em saúde em municípios gaúchos de pequeno porte. Rev Saúde Pública [Internet]. 2011 fev [citado 2019 jan 14];45(1):24-30. Disponível em: Disponível em: http://www.scielo.br/pdf/rsp/v45n1/1399.pdf . Doi: 10.1590/S0034-89102011000100003 [ Links ]
21. Mony PK,Varghese B, Thomas T. Estimation of perinatal mortality rate for institutional births in Rajasthan state, India, using capture-recapture technique. BMJ Open [Internet]. 2015;5(3):e005966. Available from: https://bmjopen.bmj.com/content/bmjopen/5/3/e005966.full.pdf. Doi: 10.1136/bmjopen-2014-005966 [ Links ]
22. Oliveira CM, Frias PG, Bonfim CV, Antonino VCS, Nascimento JDT, Medeiros ZM. Rev. Avaliação da vigilância do óbito infantil: estudo de caso. Rev Bras Saúde Matern Infant [Internet]. 2017 out-dez;17(4):817-31. Disponível em: http://www.scielo.br/pdf/rbsmi/v17n4/pt_1519-3829-rbsmi-17-04-0801.pdf. Doi: 10.1590/1806-93042017000400011 [ Links ]
23. Albuquerque AC, Mota ELA, Felisberto E. Descentralização das ações de vigilância epidemiológica em Pernambuco, Brasil. Cad Saúde Pública [Internet]. 2015 abr [citado 2019 jan 14];31(4):861-73. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v31n4/0102-311X-csp-31-04-00861.pdf . Doi: 10.1590/0102-311X00102214 [ Links ]
24. Maia LTS, Souza WV, Mendes ACG. A contribuição do linkage entre o SIM e Sinasc para a melhoria das informações da mortalidade infantil em cinco cidades brasileiras. Rev Bras Saude Matern Infant [Internet]. 2015 jan-mar [citado 2019 jan 14];15(1):57-66. Disponível em: Disponível em: http://www.scielo.br/pdf/rbsmi/v15n1/1519-3829-rbsmi-15-01-0057.pdf . Doi: 10.1590/S1519-38292015000100005 [ Links ]
25. Maia LTS, Souza WV, Mendes ACG, Silva AGS. Uso do linkage para a melhoria da completude do SIM e do Sinasc nas capitais brasileiras. Rev Saúde Pública [Internet]. 2017 [citado 2019 jan 14];51:112. Disponível em: Disponível em: http://www.rsp.fsp.usp.br/artigo/uso-do-linkage-para-a-melhoria-da-completude-do-sim-e-do-sinasc-nas-capitais-brasileiras/ [ Links ]
26. Ramalho MOA, Frias PG, Vanderlei LCM, Macêdo VC, Lira PIC. Avaliação da incompletude da declaração de óbitos de menores de um ano em Pernambuco, Brasil, 1999-2011. Ciên Saúde Colet [Internet]. 2015 set [citado 2019 jan 14];20(9):2891-8. Disponível em: Disponível em: http://www.scielo.br/pdf/csc/v20n9/1413-8123-csc-20-09-2891.pdf . Doi: 10.1590/1413-81232015209.09492014 [ Links ]
27. Santos SSBS, Melo CMM, Costa HOG, Tanaka OY, Ramos FM, Santana MCC, et al. Avaliação da capacidade de gestão descentralizada da vigilância epidemiológica no Estado da Bahia. Ciên Saúde Colet [Internet]. 2012 abr [citado 2019 jan 14];17(4):873-82. Disponível em: Disponível em: http://www.scielo.br/pdf/csc/v17n4/v17n4a10.pdf . Doi: 10.1590/S1413-81232012000400010 [ Links ]
28. Frias PG, Szwarcwald CL, Lira PIC. Estimação da mortalidade infantil no contexto de descentralização do Sistema Único de Saúde (SUS). Rev Bras Saúde Matern Infant [Internet]. 2011 out-dez;11(4):463-70. Disponível em: http://www.scielo.br/pdf/rbsmi/v11n4/v11n4a13.pdf. Doi: 10.1590/S1519-38292011000400013 [ Links ]
29. Contandriopoulos AP, Rey L, Brousselle A, Champagne F. Évaluer une intervention complexe: enjeux conceptuels, méthodologiques, et opérationnels. Can J Program Eval [Internet]. 2011 Jan [cited 2019 Jan 14];26(3):1-16. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4900871/ [ Links ]
*Article derived from the Doctoral thesis entitled “'Evaluation of the effectiveness of intervention for the improvement of the Mortality Information System in Pernambuco: a quasi-experimental study', submitted by Barbara de Queiroz Figueirôa to the Child and Adolescent Health Postgraduate Program of the Federal University of Pernambuco, on 8 June 2018. Study funded by the Brazilian Ministry of Health: Process No 779427/2012.
Received: November 09, 2018; Accepted: December 26, 2018











 texto em
texto em