Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.28 no.3 Brasília set. 2019 Epub 22-Out-2019
http://dx.doi.org/10.5123/s1679-49742019000300012
EXPERIENCE REPORT
Gestational risk classification based on maternal death profile 2008-2013: an experience report from the municipality of Porto Seguro, Bahia, Brazil
1Universidade Federal do Sul da Bahia, Centro de Formação em Saúde, Teixeira de Freitas, BA, Brasil
2Secretaria Municipal de Saúde, Porto Seguro, BA, Brasil
3Universidade Federal da Bahia, Maternidade Climério de Oliveira, Salvador, BA, Brasil
Objective:
to portray the creation of a gestational risk classification based on the profile of maternal deaths in a municipality where the rate of these deaths is high, and its use in prenatal care.
Methods:
the profile was prepared using records of maternal deaths that occurred between 2008 and 2013, considering age, schooling, race/skin color, place of residence, pre-existing disease, reproductive history.
Results:
maternal death was most frequent in women of brown/black skin color, aged 30-39, with low schooling, living in socially vulnerable districts and with heart disease as the main pre-existing disease; gestational risk was classified based on this profile, whereby points (1-3) were assigned to each lowest/highest frequency and care priorities (P) were defined - PI=regular risk (4-9pt: routine consultation/examination), PII=high risk (10-16pt: reduce waiting time for consultation/examination by 50%), and PIII=very high Risk (≥17pt: access to consultation/examination within 7 days).
Conclusion:
the new classification improved healthcare professionals’ awareness of determinants surrounding maternal death and the need to prioritize access to prenatal care according to risk.
Keywords: Maternal Mortality; Risk Factors; Prenatal Care; Health Services Accessibility; Cross-Sectional Studies
Introduction
Maternal Mortality (MM) is still one of the biggest Public Health problems. In 2000, the United Nations (UN) defined it as an indicator of one of the main issues to be faced at the turn of new millennium, with the aim of promoting social and human development and ending extreme poverty worldwide. One of the Millennium Development Goals (MDG) proposed by the UN was to reduce MM by 75% by 2015. Brazil did not achieve this goal, and the MDG were replaced by the Sustainable Development Goals. In Brazil’s case, the current target consists of reducing the MM ratio to 20/100,000 live births (LB) by 2030.1
When we study MM and investigate its causes, what draws our attention is the high potential for avoiding these deaths if timely actions are taken. In order to really improve maternal health, the focus should not only be on the causal link. The need exists to identify and eliminate obstacles to accessing quality health services, at all health system levels.2 Studies have provided evidence that access to health services is essential for reducing high MM rates, and that social, cultural and economical determinants, as well as health policies, have a close relationship with these deaths.3,4
McCarthy and Maine classify maternal death determinants as “general”, “intermediate” and “proximal”.5 General determinants refer to macro-social processes, related to socioeconomic inequalities, ethnic and racial discrimination and lack of social policies for less privileged segments of the female population. Standing out among intermediate determinants is restricted access to social assets, while proximal determinants are represented by women’ sociodemographic characteristics and their health conditions, besides those related to access to care, ease of reproductive planning, timely and quality care during the prenatal period, at childbirth and in the puerperium.
In this sense, Primary Health Care professionals have the opportunity to implement many practices that are able to contribute to MM prevention, operating on proximal determinants. It is known that prenatal care may not prevent the main complications occurring during childbirth and which are important MM causes, however certain prenatal care interventions may favor maternal prognosis and prevent MM.6
Prenatal care can control risk factors that lead to complications during pregnancy, besides allowing early detection and treatment, thus contributing to a favorable perinatal and maternal outcome.7 It is also necessary to recall that 15% of pregnancies are characterized as being high risk, and that early recognition of these cases, associated with the existence of more complex support services and adequate monitoring, are decisive for keeping these women alive.8
Technical materials produced by the Ministry of Health regarding pregnant women’s health,9,10 recommend that risk classification should be done during the first and subsequent medical appointments, so as to favor access to quality services, by identifying these factors as early as possible and in a dynamic way, besides enabling recognition of situations that contribute to potentially avoidable deaths.
Although these instruments are used by Family Health Strategy (FHS) teams in decision making related to caring for and monitoring pregnant women with regard to regular risk in the prenatal period, knowledge of determinants related to maternal death in a municipality may add important information to gestational risk classification, prioritizing health care actions, in a timely manner, contributing to MM prevention according to local reality. Morse et al. highlight that research into MM determinants is still weak in Brazil, being comprised mostly of descriptive studies identifying underlying causes, while making little progress with investigating the determinant factors of these deaths.11
In 2013, the fact of the MM ratio having remained high since 2009 in the municipality of Porto Seguro-BA led the local epidemiological surveillance of deaths (ESD) service to create the Target 35 Project, with the mission of expanding integration with Primary Care and promoting greater interaction with the local hospital network in order to achieve the project’s main objective: to intervene in avoidable MM causes based on the investigation reports of these deaths, with the target of reducing the MM ratio to approximately 35/100,000 LB by 2015, in line with the MDG.
The purpose of this report was to portray the experience of creating a gestational risk classification based on maternal death profile and its use in prenatal care by Family Health Strategy teams in Porto Seguro, Bahia, Brazil.
Methods
In order to obtain the profile of MM determinants, we selected reports on maternal deaths occurring and investigated by the municipal ESD service between 2008 and 2013. We decided to start with 2008 as that was the year in which death investigations began. The investigation reports follow templates recommended by the Ministry of Health for hospital, outpatient and household information, as well as the ESD conclusion report.12
General maternal characteristics evaluated were: age, education level, occupation, ethnicity/skin color, district of residence, marital status and monthly family income. For health conditions and access to health services, we evaluated: presence of underlying disease; number of pregnancies; past reproductive history; usual access to prenatal care medical appointments; access to higher risk prenatal care (HRPC) and to medical exams; gestational age at the first medical appointment; type of childbirth; cause of death; and newborn/fetus birth conditions. Data were tabulated using an Excel Office spreadsheet and were described according to frequencies. The death investigation reports are the ESD technicians’ daily work instruments. They produce annual reports with aggregated information, whereby it is not possible to identify individual patients. These reports are provided to the epidemiological surveillance service, the Municipal Primary Health Care services, service coordinators and managers and to the death committees. The reports are available to the public. For these reasons, the study was not submitted to a Research Ethics Committee.13
Results
In the period studied there were 23 maternal deaths, 73.9% of which were from direct/indirect obstetric causes, while the remaining (26.1%) were cases of late maternal death. The selection of the variables that formed the risk classification was based on the most prominent determinants, besides those that characterize vulnerabilities within the municipality, such as health region or health district (Table 1).
Table 1 - Maternal death characteristics according to age, years of schooling, ethnicity/skin color, health district and number of prenatal care medical appointments, in the municipality of Porto Seguro, Bahia, Brazil, 2008-2013
| Characteristics | N |
|---|---|
| Maternal age (in years) | |
| 10 to 14 | - |
| 15 to 19 | 5 |
| 20 to 29 | 6 |
| 30 to 39 | 12 |
| 40 to 49 | - |
| Years of schooling | |
| 1 to 3 | 2 |
| 4 to 7 | 9 |
| 8 to11 | 10 |
| 12 or more | - |
| Illiterate | - |
| Unknown | 2 |
| Ethnicity/skin color | |
| White | 2 |
| Indigenous | 3 |
| Brown | 12 |
| Black | 5 |
| Unknown ethnicity/skin color | 1 |
| Health Region (health districts) | |
| Centro | 3 |
| Frei Calixto | 8 |
| Litoral Sul | 8 |
| Rural area | 1 |
| Indigenous villages | 3 |
| Prenatal care medical appointments | |
| 1 to 3 | 5 |
| 4 to 6 | 13 |
| 7 or more | 4 |
| No prenatal care | 1 |
Note: ( - ) Indicates numerical data equal to zero, not resulting from rounding.
Regarding total maternal deaths, Table 1 shows higher frequency for the 30-39 years age group (52.2%), women with less than eight years of schooling (47.8%) and black/brown skin color (73.9%). The prevalent health districts were those corresponding to areas of higher social vulnerability. These findings represent results similar to those found in other studies evaluating MM determinants.11,14-16
We found that 56.3% of women had some underlying disease with heart disease being the most frequent. Of the 23 deaths, 13 women had reproductive history of a disease or condition, representing an expressive number of women who need more individualized care (Table 2). Nonetheless, more than half of them (56.5%) had only 4 to 6 medical appointments during prenatal care (Table 1).
Table 2 - Maternal death characteristics according to underlying disease and reproductive history, in the municipality of Porto Seguro, Bahia, Brazil, 2008-2013
| Characteristics | N |
|---|---|
| Underlying disease/condition | |
| Cardiac | 5 |
| Chemical/alcohol dependency | 2 |
| Neurological | 2 |
| Digestive | 1 |
| Endocrinal | 1 |
| Hematological | 1 |
| Respiratory | 1 |
| No previous disease | 6 |
| Unknown | 4 |
| Total | 23 |
| Reproductive history | |
| Miscarriage | 8 |
| Perinatal death | 2 |
| Hemorrhagic syndrome | 1 |
| Preeclampsia | 1 |
| Depression | 1 |
| Total | 13 |
Note: The difference between the sum of the items and the total expressed as a percentage is due to the rounding criteria.
Main direct obstetric causes were hemorrhages and puerperal infections; and the main indirect causes of maternal deaths were circulatory system diseases complicated by pregnancy, labor and puerperium.
Based on the profile results, we selected six prominent variables to build the municipality gestational risk classification: maternal age, education level, ethnicity/skin color, health district, underlying disease and past reproductive history.
A score of 1 to 3 was given to the frequencies obtained for each category. A score of 3 was given to the larger frequency range and a score of 1 to the smaller frequency range. (Table 3). In the “years of study” category, although there were no records in the “illiterate” range, the applicable score was the same score given to the “1 to 3 years” range, due to the relevance of this condition as a determinant of maternal death. The difficulty the teams had in placing value on pregnant women’s reproductive history led to this category being considered to be of isolated importance, and it received the maximum score (3 points) for any result.
Table3 - Category distribution and scores for calculating gestational risk in the municipality of Porto Seguro, Bahia, Brazil
| Categories | Score | Categories | Score |
|---|---|---|---|
| Maternal age (in years) | Underlying disease/condition | ||
| 10 to 14 | 1 | Cardiac | 3 |
| 15 to 19 | 2 | Chemical/alcohol dependency | 2 |
| 20 to 29 | 2 | Neurological | 2 |
| 30 to 39 | 3 | Digestive | 2 |
| 40 to 49 | 1 | Endocrinal | 2 |
| Years of schooling | Hematological | 2 | |
| Illiterate | 3 | Respiratory | 2 |
| 1 to 3 | 3 | Other | 2 |
| 4 to 7 | 2 | Smoking | 1 |
| 8 to 11 | 1 | ||
| 12 or more | 1 | ||
| Ethnicity/skin color | Reproductive history | ||
| White | 1 | Miscarriage | 3 |
| Indigenous | 2 | Perinatal death | 3 |
| Brown | 3 | Hemorrhagic syndrome | 3 |
| Black | 3 | Preeclampsia | 3 |
| Health Region (health districts) | Depression | 3 | |
| Other | 3 | ||
| Centro | 2 | ||
| Frei Calixto | 3 | ||
| Litoral Sul | 3 | ||
| Rural area | 1 | ||
| Indigenous villages | 2 |
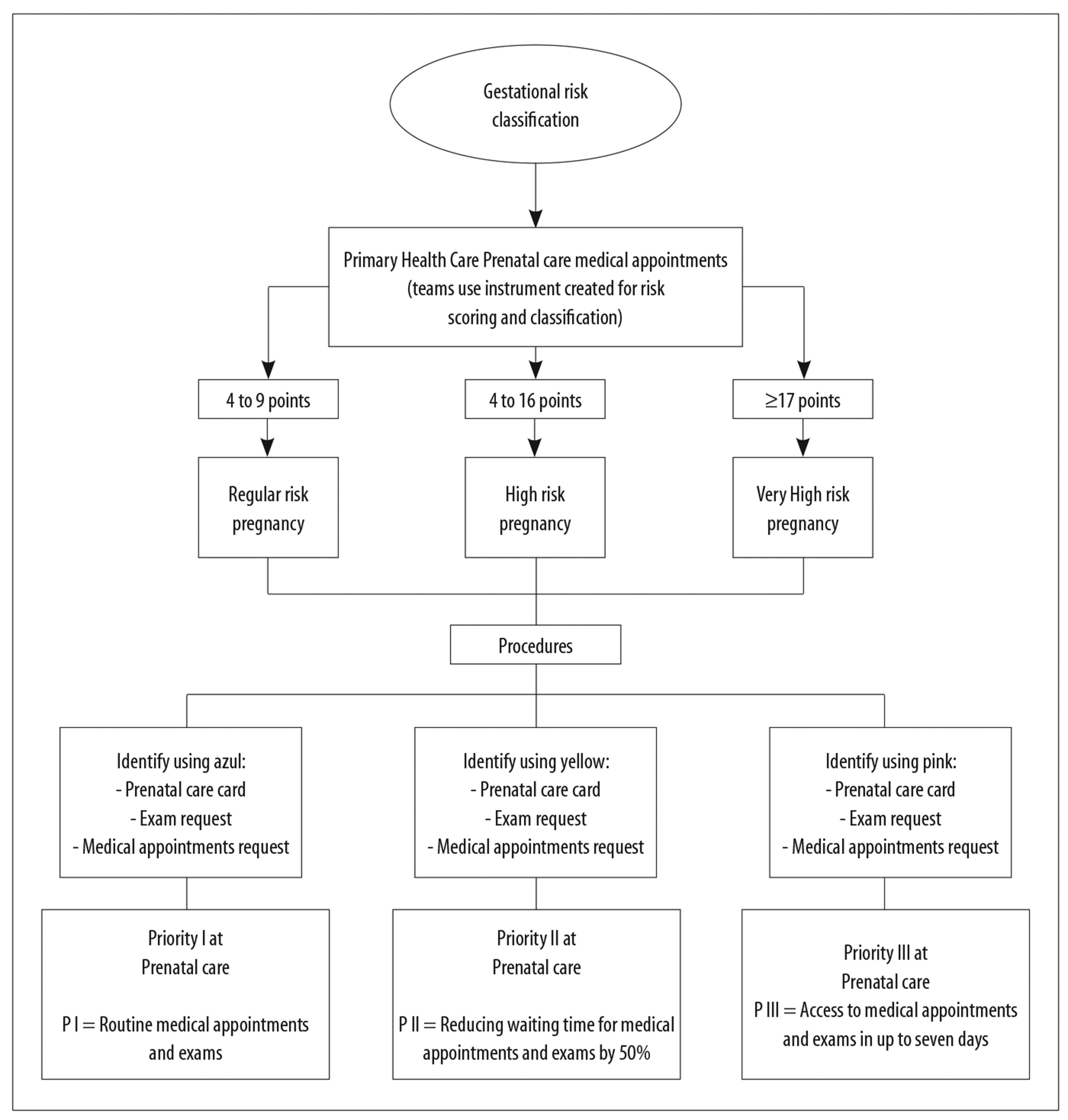
The final score was represented by the sum of the scores of the six categories analyzed. Therefore, gestational risk was classified as regular (4 to 9 points), High (10 to 16 points) or very high (17 points or more) (Figure 1).
Based on this new classification, prenatal care priority was determined according to the gestational risk level found. Priority I was attributed to regular risk, meaning that the pregnant woman should follow the team’s routine for medical appointments and exams. In the case of Priority II, waiting time for a medical appointment and prenatal care exams should be reduced to 50%, and in the case of Priority III, access to medical appointments and exams should not take longer than seven days (Figure 1).
Before the risk classification and priority instrument was distributed, we had meetings with the Primary Health Care coordinators and Ambulatory Care waiting list coordinators to agree on deadlines for medical appointments with focal specialists and medical exams, according to the priorities established.
Health teams underwent awareness-raising as to the maternal death situation in the municipality, including a presentation of the results of the study on the MM determinant profile. They were also informed about the way the gestational risk classification had been built and were trained in the correct use of the instrument. The color-coded instrument was printed on sheets of A4 paper with plastic covers for distribution to the teams. It provided instructions and guidance on how to score the listed categories, establish risk level and priority for health care.
During Primary Health Care prenatal care medical appointments, pregnant women were evaluated for gestational risk based on the instrument, receiving a final score, classification and health care priority definition.
In order to avoid pregnant women being identified by the term “risk”, care was taken to color code prenatal care cards and requisition forms for medical appointments and exams, using blue, yellow or pink, meaning regular, high or very high risk, respectively (Figure 1). The care network for pregnant woman also received guidance on the meaning of the colors.
With regard to cases referred to other services, care was taken to ensure comprehensive health care, so that these pregnant women were monitored even after being effectively attended to at the referral service.
Discussion
With effect from the first meetings with the teams, we could see that the instruments provided by the Ministry of Health were little used in the prenatal care service routine. However, following the presentation of the new classification, professionals were more aware and careful with regard to using available tools to help to improve care for pregnant women.
The teams showed awareness of the importance of recognizing determinants involved in maternal death. The practice of registering data about education level and ethnicity/skin color was not part of the team routine. The 2016 version of the Expectant Mother’s Notebook prepared and published by the Ministry of Health,17 does not contain the item “education level” as part of the identification data of pregnant women. Professionals pointed out the need to require this information as being a marker of the importance of medical record data completeness.
From the accounts given by the teams, we noted that cardiological evaluation was insufficient. Referrals to the cardiologist were made when pregnant women knew they had a cardiovascular system disease prior to pregnancy, or when there was a clinical condition involving cardiac decompensation. With the new classification, the clinical approach to heart conditions began to be more detailed and access to electrocardiograms became easier for pregnant women.
Importance had not been given to pregnant women’s reproductive history, leading to shortcomings in identifying assumed risk situations regarding obstetric complications. With the new classification and greater awareness, professionals started to place more importance on this topic during obstetric anamnesis and to collect information in more detail about previous obstetric and gynecological history.
Setting priorities for prenatal health care, according to the pregnant women’s profile and risk level, had positive effects on the teams. They reported that they found (i) greater certainty of dealing with cases in a timely manner and (ii) guaranteed access to medical examinations and appointments, thus overcoming weaknesses in referrals.
The persistence of a high MM ratio in the municipality since 2009 motivated the development of this experience. The Target 35 Project represented a call to health professionals and managers involved in the care of pregnant women, in the light of the information described in the maternal death investigation reports that showed the need to invest in actions with greater emphasis on Primary Care. It was a challenging project, in view of the delicate situation of maternal deaths in the municipality.
Since 2007, ESD has been working in an integrated way with Primary Care in preventing maternal and child mortality, and considers this partnership to be of fundamental importance for carrying out actions to prevent disease and promote health. The teams’ awareness, their integration with death surveillance as well as management support were all fundamental for the success of the experience.
Obtaining the epidemiological profile and exposing/clarifying the situation of maternal mortality, highlighting specific determinants in the municipality, was a relevant part of the project. The complexity of determinants involved in maternal deaths represents an important challenge for health service management, owing to the need to articulate intersectoral actions. However, when we consider the high percentage of deaths from avoidable causes, we recognize not only the possibility, but also the need to build strategies to help to change this scenario. The prevalence of low levels of schooling, brown or black ethnicity/skin color and living in areas of greater social vulnerability are evidence of continuing inequalities related to MM.
Most of the studies on obstetric causes of MM point to direct causes (hypertensive disorders, hemorrhages, and puerperal infections) as being most frequent.11,15,18,19 In this study, after hemorrhages indirect causes corresponded to an important proportion of deaths. Nonetheless, regardless of their cause, the potential avoidability of these deaths draws attention. When analyzing the profile of maternal deaths, Martins and Silva found that 73% of these deaths were avoidable, or would probably have been avoidable if interventions had been carried out in a timely manner.19
Risk classification was built based on the MM profile of the municipality of Porto Seguro, as was the definition of health care priorities, with the aim of improving care for pregnant women.
According to a recent study of hospitalizations due to obstetric complications during pregnancy and maternal and perinatal outcomes in the municipality of São Paulo, pregnant women who had obstetric complications had more unfavorable pregnancy outcomes, such as postpartum hospitalization and MM, in addition to higher levels of newborn babies being readmitted to hospital. That study concluded that these events should be considered to be sentinel events for monitoring childbirth and newborn health care in the population served by the Brazilian National Health System (SUS).20
For the epidemiological surveillance of deaths service, the experience described by this report reaffirmed work processes based on building and sharing information and recommending procedures, thus contributing to the practices of Primary Health Care professionals being articulated with health surveillance actions. In 2013, the year in which the Target 35 Project started, the third and last maternal death recorded in Porto Seguro occurred in June. In 2014, the municipality did not record any maternal deaths, breaking the sequence of 3 or 4 deaths a year.21
It is known that responding to and eliminating maternal mortality is an urgent task and requires considerable efforts. There is also an evident need to promote women’s well-being and better survival rates and quality of life for their children. Small actions, carried out every day by each health professional, can bring solid results in changing this uncertain but avoidable scenario.
Referências
1. Organização das Nações Unidas. Transformando nosso mundo: a agenda 2030 para o desenvolvimento sustentável [Internet]. Brasília: Organização das Nações Unidas; 2015 [citado 2019 fev 9]. Disponível em: Disponível em: https://nacoesunidas.org/pos2015/agenda2030/ [ Links ]
2. Silveira, MMP. Influência do tempo de remoção da paciente para a maternidade de alta complexidade e desfecho desfavorável [dissertação]. Salvador: Escola Bahiana de Medicina e Saúde Pública; 2015. Disponível em: http://www7.bahiana.edu.br/jspui/bitstream/bahiana/234/1/Dissertação.%20Silveira.%20Márcia%20Maria%20Pedreira%20da.%202015.001.BAHIANA.pdf [ Links ]
3. Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med [Internet]. 1994 Apr [cited 2018 Dec 8];38(8):1091-110. Available from: Available from: http://www.ncbi.nlm.nih.gov/pubmed/804205 . [ Links ]
4. Gabrysch S, Campbell OMR. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth [Internet]. 2009 Jan [cited 2019 Jan 26];9:34. Available from: Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2744662&tool=pmcentrez&rendertype=abstract . doi: 10.1186/1471-2393-9-34 [ Links ]
5. Mccarthy J, Maine D. A framework for analyzing the determinants of maternal mortality. Stud Fam Plann [Internet]. 1992 Jan-Feb [cited 2019 Jul 8];23(1):23-33. Available from: Available from: https://www.jstor.org/stable/1966825 . doi: 10.2307/1966825 [ Links ]
6. Calderón IMP, Cecatti JG, Vega CEP. Intervenções benéficas no pré-natal para prevenção da mortalidade materna. Rev Bras Ginecol Obs [Internet]. 2006 maio [citado 2018 nov 9];28(5):310-5. Disponível em: Disponível em: http://www.scielo.br/pdf/rbgo/v28n5/a08v28n5.pdf . doi: 10.1590/S0100-72032006000500008 [ Links ]
7. Domingues RMSM, Hartz ZMA, Dias MAB, Leal MC. Avaliação da adequação da assistência pré-natal na rede SUS do Município do Rio de Janeiro, Brasil. Cad Saúde Pública [Internet]. 2012 mar [citado 2018 dez 6];28(3):425-37. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v28n3/03.pdf . doi: 10.1590/S0102-311X2012000300003 [ Links ]
8. Ministério da Saúde (BR). Secretaria de Políticas de Saúde, Área Técnica da Saúde da Mulher. Urgências e emergências maternas: guia para diagnóstico e conduta em situações de risco de morte materna [Internet]. 2. ed. Brasília: Ministério da Saúde; 2000 [citado 2019 jul 8]. 119 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/0105urgencias.pdf [ Links ]
9. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Atenção ao pré-natal de baixo risco [Internet]. Brasília: Ministério da Saúde ; 2012 [citado 2019 jul 8]. 318 p. (Série A. Normas e Manuais Técnicos) (Cadernos de Atenção Básica, n° 32). Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/cadernos_atencao_basica_32_prenatal.pdf [ Links ]
10. Ministério da Saúde (BR). Instituto Sírio-Libanês de Ensino e Pesquisa. Protocolos da atenção básica: saúde das mulheres [Internet]. Brasília: Ministério da Saúde; 2016 [citado 2019 jul 8]. 230 p. Disponível em: Disponível em: http://189.28.128.100/dab/docs/portaldab/publicacoes/protocolo_saude_mulher.pdf [ Links ]
11. Morse ML, Fonseca SC, Barbosa MD, Calil MB, Eyer FPC. Mortalidade materna no Brasil: o que mostra a produção científica nos últimos 30 anos? Cad Saúde Pública [Internet]. 2011 abr [citado 2018 nov 12];27(4):623-38. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v27n4/02.pdf . doi: 10.1590/S0102-311X2011000400002 [ Links ]
12. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise de Situação em Saúde. Guia de vigilância epidemiológica do óbito materno [Internet]. Brasília: Ministério da Saúde; 2009 [citado 2019 jul 8]. 84 p. (Série A. Normas e Manuais Técnicos). Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/guia_vigilancia_epidem_obito_materno.pdf [ Links ]
13. Brasil. Ministério da Saúde. Resolução MS/CNS nº 510, de 7 de abril de 2016. Dispõe sobre as normas aplicáveis a pesquisas em Ciências Humanas e Sociais cujos procedimentos metodológicos envolvam a utilização de dados diretamente obtidos com os participantes ou de informações identificáveis ou que possam acarretar riscos maiores do que os existentes na vida cotidiana [Internet]. Diário Oficial da União, Brasília (DF), 2016 maio 24 [citado 2019 jul 8];Seção 1:44-6. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/cns/2016/res0510_07_04_2016.html [ Links ]
14. Faria DR, Sousa RC, Costa TJNM, Leite ICG. Mortalidade materna em cidade-polo de assistência na região Sudeste: tendência temporal e determinantes sociais. Rev Med Minas Gerais [Internet]. 2012 [citado 2018 nov 12];22(1):1-128. Disponível em: Disponível em: http://www.rmmg.org/artigo/detalhes/121 . [ Links ]
15. Teixeira NZF, Pereira WR, Barbosa DA, Vianna LAC. Mortalidade materna e sua interface com a raça em Mato Grosso. Rev Bras Saúde Mater Infant [Internet]. 2012 [citado 2019 fev 12];12(1):27-35. Disponível em: Disponível em: http://www.scielo.br/pdf/rbsmi/v12n1/03.pdf . doi: 10.1590/S1519-38292012000100003 [ Links ]
16. Leite RMB, Araújo TVB, Albuquerque RM, Andrade ARS, Duarte Neto PJ. Fatores de risco para mortalidade materna em área urbana do Nordeste do Brasil. Cad Saúde Pública [Internet]. 2011 out [citado 2019 jan 31];27(10):1977-85. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v27n10/11.pdf . doi: 10.1590/S0102-311X2011001000011 [ Links ]
17. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Coordenação Geral da Saúde das Mulheres. Departamento de Atenção Básica. Caderneta da gestante [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2019 jul 8]. Disponível em: Disponível em: http://portalarquivos2.saude.gov.br/images/pdf/2018/agosto/31/Caderneta-da-Gestante-2018.pdf [ Links ]
18. Silva BGC, Lima NP, Silva SG, Antúnez SF, Seerig LM, Restrepo-Méndez MC, et al. Mortalidade materna no Brasil no período de 2001 a 2012: tendência temporal e diferenças regionais. Rev Bras Epidemiol [Internet]. 2016 jul-set [citado 2019 jan 27];19(3):484-93. Disponível em: Disponível em: http://www.scielo.br/pdf/rbepid/v19n3/1980-5497-rbepid-19-03-00484.pdf . doi: 10.1590/1980-5497201600030002 [ Links ]
19. Martins ACS, Silva LS. Epidemiological profile of maternal mortality. Rev Bras Enferm [Internet]. 2018 [cited 2019 Mar 15];71(Suppl 1):677-83. Available from: Available from: http://www.scielo.br/pdf/reben/v71s1/pt_0034-7167-reben-71-s1-0677.pdf . doi: 10.1590/0034-7167-2017-0624 [ Links ]
20. Moura BLA, Alencar GP, Silva ZP, Almeida MF. Internações por complicações obstétricas na gestação e desfechos maternos e perinatais, em uma coorte de gestantes no Sistema Único de Saúde no município de São Paulo, Brasil. Cad Saúde Pública [Internet]. 2018 [citado 2019 mar 19];34(1):e00188016. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v34n1/1678-4464-csp-34-01-e00188016.pdf . doi: 10.1590/0102-311x00188016. [ Links ]
21. Secretaria de Saúde do Estado da Bahia. Informações em saúde [Internet]. Salvador: Secretaria de Saúde do Estado da Bahia; 201- [citado 2019 jul 8]. Disponível em: Disponível em: http://www.saude.ba.gov.br/suvisa/diretoria-de-informacao-em-saude-dis [ Links ]
Received: February 19, 2019; Accepted: June 28, 2019











 texto em
texto em