Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.1 Brasília 2020 Epub 14-Feb-2020
http://dx.doi.org/10.5123/s1679-49742020000100005
ORIGINAL ARTICLE
Sociodemographic and health care profile of maternal death in Recife, PE, Brazil, 2006-2017: a descriptive study*
1Instituto de Medicina Integral Prof. Fernando Figueira, Programa de Pós-Graduação em Medicina Integral, Recife, PE, Brazil
2Secretaria Estadual de Saúde de Pernambuco, Secretaria Executiva de Vigilância em Saúde, Recife, PE, Brazil
Objective:
to describe the sociodemographic and health care characteristics of women dying due to maternal causes in Recife, Pernambuco, Brazil.
Methods:
this was a descriptive study using the Mortality Information System, case investigation sheets and summary sheets of early and late maternal deaths occurring between 2006 and 2017, with avoidability assessed by the Municipal Maternal Mortality Committee.
Results:
we identified 171 deaths, of which 133 were in the puerperium; most deaths occurred among Black women (68.4%), women without partners (60.2%), women who had prenatal care (77.2%), during maternity hospital/general hospital delivery (97.1%), women attended to by obstetricians (82.6%);10.4% of women with puerperal complications had no health care; avoidable/probably avoidable deaths corresponded to 81.9%, for indirect causes (n=80), and direct causes (n=79).
Conclusion:
deaths occurred mainly in the postpartum period, among Black women; care failures were frequent; improved health service surveillance and follow-up is needed in the pregnancy-puerperal period, in Recife.
Keywords: Maternal Mortality; Pregnancy Complications; Mortality Registries; Health Information Systems; Epidemiology, Descriptive
Introduction
Maternal death continues to be an important health problem in many of the world’s regions, especially in those that are less developed.1,2 In 2015, the global maternal death ratio was estimated to be 216 per 100,000 live births (LB), varying between 542 per 100,000 LB in Africa and 16 per 100,000 LB in Europe.2
A study conducted in the United States covering the period 2011-2015 identified higher maternal death ratios among Black women (42.8 per 100,000 LB), women without partners (22.8 per 100,000 LB) and women with low schooling.1 Institutional conditions also contributed to these deaths, such as health teams having little experience of obstetric emergencies, absence of specialized staff or services, delayed diagnosis and lack of continuing care, among others.1
Reducing maternal mortality is a global guideline owing to its avoidable nature.2,3 It was part of the Millennium Development Goals for 2015 and has been reiterated in the Sustainable Development Goals for 2030.3 Brazil did not achieve the Millennium Development Goals target as its maternal death ratio in 2015 was 44 per 100,000 LB, this being higher than the ratios recorded in the poorest Latin American countries, such as Cuba (39 per 100,000 LB), Costa Rica (25 per 100,000 LB) and Uruguay (15 per 100,000 LB).2
In the three-year period comprising 2009-2011, Brazil’s Northeast region, especially Pernambuco state, had maternal death ratios of 80.8 per 100,000 LB and 63.3 per 100,000 LB, respectively, these being higher than the national average; and owing to underreporting they may have been even higher.4
In Brazil, risk of maternal death from direct obstetric causes was 40.7 per 100,000 LB, this being approximately double the risk of death from indirect obstetric causes (19.4 per 100,000 LB) in 2012. In the same year, the most frequent direct causes of maternal death were arterial hypertension (19.6%), hemorrhage (11.6%) and puerperal infection (7.1%), while the main indirect obstetric causes of death were diseases of the circulatory system with complications during pregnancy, childbirth or puerperium (7,1%). In Pernambuco, also in 2012, maternal death cause distribution was similar to that found nationally.5
Previous Brazilian studies have revealed causes of maternal mortality and its sociodemographic characteristics without detailing the clinical, epidemiological and health care aspects of the pregnancy-puerperal cycle, restricting themselves to the variables available on Death Certificates (DCs).5-8 Evaluation of information forming part of epidemiological investigation of maternal deaths in hospital, outpatient services and at home, as regulated by the Ministry of Health in 2008, would add relevant information.9 These investigations would provide additional input, contributing to explaining the epidemiological and sociodemographic profile of the victims, clarifying the circumstances of death, identifying health care problems and proposing changes to women’s health care.1,9
The objective of this study was to describe the sociodemographic and health care characteristics of women dying due to maternal causes in Recife, Pernambuco, Brazil.
Methods
This is a descriptive study based on records held on DCs, Confidential Maternal Death Investigation Sheets and Summarized Maternal Death Investigation Sheets. DCs are filled in by doctors at the service where death occurs or at autopsy services; confidential investigation sheets are filled in by means of interviews with family members, examining medical records and autopsy reports; the summary investigation sheet is filled in following discussions by the maternal death technical group based on multiple sources.10
Recife is located on the coast of Pernambuco’s Zona da Mata region. It covers an area of 218.435km2 and in 2010 it had a population of 1,537,704 inhabitants, of whom 522,120 were women of childbearing age (10-49 years old), resident in 94 exclusively urban neighborhoods.11 According to the National Health Establishments Register, the municipality has the state’s largest health care network, with seven public and nine private maternity hospitals where 50,000 live births take place every year, 23,000 of whom are resident in Recife; the care network also includes 130 primary health care centers, 276 Family Health Strategy (ESF) teams and 2,100 community health agents (ACS) to cover 51% of the population.12 Maternal death surveillance was implanted with effect from 1994. The technical discussion groups include Primary Care professionals and professionals from health establishments where women were cared for until the time of death.13
This study assessed all maternal deaths of women resident in Recife, including those classified as late deaths (from 43 days to one year following childbirth), investigated and discussed by the Recife Health Department maternal mortality technical group which reports to the Municipal Maternal Mortality Committee. Inclusion of late maternal deaths aimed to broaden the study’s scope, by extending the period for detecting and including maternal deaths delayed by the advance of health technologies.
The following is a description of the variables considered in the study:
a) Sociodemographic variables
- age (in years: 10-19, 20-34, 35-49);
- race/skin color (White, Black [including black and brown skin color], unknown);
- marital status (had partner, did not have partner [includes single, widowed and separated women], unknown);
- schooling (no schooling, primary and middle school education, high school education, higher education, unknown); and
- occupation (housewife, worked in trade/business, student, housekeeper, teacher, other, unknown).
b) Reproductive, pregnancy and prenatal history
- previous pregnancy (none, 1, 2 or more, unknown);
- attempted abortion (yes, no, unknown);
- tetanus vaccination (complete, incomplete, not immunized, unknown);
- ACS visit (yes, no, unknown);
- complications during pregnancy (yes, no, unknown);
- treatment of complications during pregnancy (yes, no, unknown);
- prenatal monitoring (yes, no, unknown);
- number of prenatal consultations (1-3, 4-6, 7 or more, unknown);
- type of prenatal health establishment (Family Health center, public/philanthropic hospital/polyclinic, private hospital/consulting rooms, unknown);
- gestational age at first prenatal consultation (in weeks: 1-13, 14-26, 27-42, unknown);
- prenatal card, or Pregnancy Card (yes, no, unknown);
- blood pressure at first prenatal consultation (normal, high, unknown);
- referral to high risk prenatal service (yes, no, unknown);
- consultation at high risk prenatal service (yes, no, unknown);
- type of high risk prenatal service establishment (public/philanthropic hospital/polyclinic, private consulting rooms, unknown).
c) Delivery and abortion (gestational age <20 weeks)
- place of delivery/abortion (maternity hospital, general hospital, home, Urgent Mobile Care Service [SAMU], unknown);
- type of establishment where delivery/abortion took place (private hospital, public/philanthropic hospital/polyclinic /SAMU, unknown);
- municipality of establishment where delivery/abortion took place (Recife, other);
- gestational age at delivery/abortion (in weeks: ≤22, 23-36, 37-41, ≥42, unknown);
- transfer during delivery/abortion (yes, no, not hospitalized);
- type of abortion (miscarriage, induced by patient, silent miscarriage);
- procedures used in induced abortion (homemade herb tea, misoprostol, other);
- had complications resulting from abortion (yes, no, unknown);
- complications resulting from abortion (infection, hemorrhage, embolism, uterine perforation, other);
- type of delivery (vaginal, cesarean, vaginal and cesarean [when both types occurred, in the same pregnancy]);
- duration of labor (in hours: ≤3, 4-12, >12, unknown);
- professional who performed the delivery (obstetrician, other, unknown);
- anamnesis filled in (yes, no, unknown);
- partogram filled in (yes, no, unknown);
- companion during labor (yes, no, unknown);
- had complications during labor (yes, no, unknown); and
- complications during labor (hemorrhage; fetal distress; pre-eclampsia; stillborn fetus; eclampsia; hemolysis, elevated liver enzymes and low platelets [HELLP] syndrome; other).
d) Puerperium and circumstances of death
- had complications during puerperium (yes, no, unknown);
- treatment of complications during puerperium (yes, no, unknown);
- complications during puerperium (infection, hemorrhage, cardiovascular problems, eclampsia, embolism, neoplasms, uterine atony, other);
- time of death (during pregnancy, during labor, early puerperium, late puerperium);
- place of death (hospital, other health establishments, at home);
- municipality where death occurred (Recife, others);
- death avoidability criterion, as per the Maternal Death Epidemiological Surveillance Guide, which is not limited to analysis of therapeutic measures but also considers factors related to the community and to the patient, as well as professional, institutional, social and intersectoral factors, and which following individual analysis of each case by the Maternal Mortality Committee, classifies death as avoidable, probably avoidable, probably unavoidable, inconclusive or unknown;10
- autopsy performed (yes, no, unknown);
- analysis of uterus and appendages during autopsy (yes, no, unknown);
- direct obstetric causes, defined as resulting from complications during pregnancy, childbirth or puerperium, due to interventions, omissions, incorrect treatment, or to the chain of events arising from any of these causes10 (hypertension, embolism, hemorrhage, puerperal infection, abortion, pregnancy ending in abortion, other complications related to labor and delivery, infection of genitourinary tract during pregnancy, cardiomyopathy during puerperium, other causes);
- indirect obstetric causes, resulting from a mother’s previous disease or developing during pregnancy, not due to direct obstetric causes but exacerbated by the physiological effects of pregnancy10 (circulatory system diseases, specified diseases and disorders, respiratory system diseases, HIV/AIDS, pre-existing hypertension, communicable and parasitic diseases causing complications during pregnancy, childbirth and puerperium, mental disorders, digestive system diseases, other hematologic diseases, endocrine system diseases);
- obstetric death from unspecified cause;
- death from any late obstetric cause (43 days to 1 year); and
- ill-defined cause.
The causes of death considered here are catalogued in chapter XVIII of the International Statistical Classification of Diseases and Related Health Problems - Tenth Revision (ICD-10).
The data used in the study were collected in the second semester of 2018 from the Mortality Information System (SIM), Confidential Maternal Death Investigation Sheets and Summarized Maternal Death Investigation Sheets,10 in relation to deaths occurring between January 1st 2006 and December 31st 2017, made available by the Pernambuco State Health Department and the Recife Health Department.
Data obtained from SIM were tabulated using TabWin32, while the Summary Sheet data were retrieved from the maternal death surveillance database. Both datasets were input to Epi Info version 3.6.3, using the ‘make view’ and ‘enter data’ modules. The variables from the Confidential Maternal Death Investigation Sheets formed an Excel® 2007 electronic spreadsheet database. The deterministic linkage technique enabled consolidation in a single Excel® 2007 database, taking the death certificate (DC) number as the key variable. Missing information on DCs and maternal death investigation sheets was complemented by the Recife Health Department which sought this information via several sources (hospital, patient’s home and outpatient services).
The study included women who died from notified early and late maternal causes, as well as those identified following investigation of deaths of women of childbearing age within the study period.
We used descriptive statistics shown according to distribution by absolute and relative frequencies for the total number of years in the period. We calculated the proportion of maternal deaths for the study variables.
The study project was approved by the Professor Fernando Figueira Comprehensive Medicine Institute Research Ethics Committee: Report No. 2.277.245, dated 15/9/2017; Certification of Submission for Ethical Appraisal CAAE) No. 72815317.4.0000.5201
Results
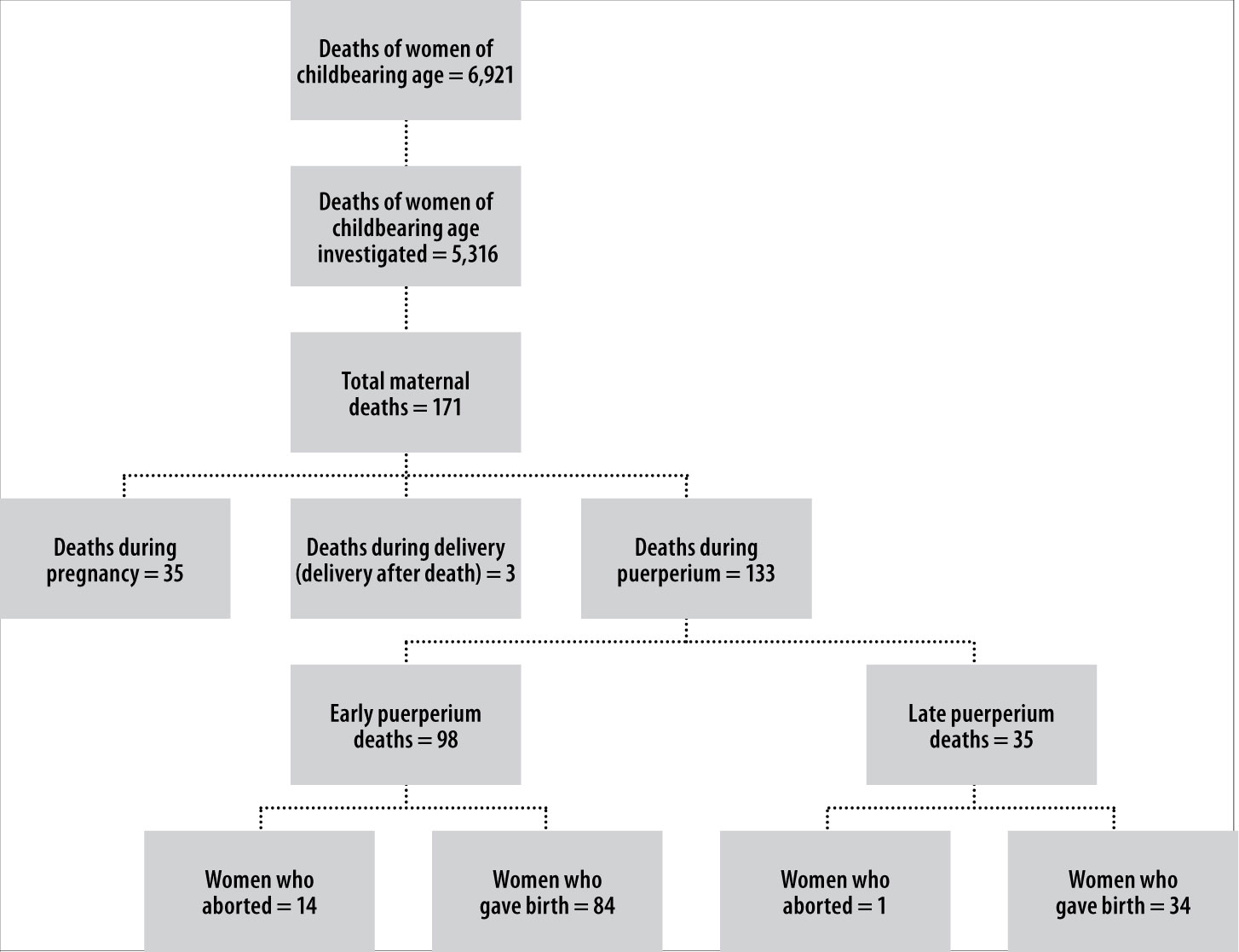
Of the 6,921 deaths of women of childbearing age resident in Recife, 76.8% were investigated and 171 (3.2%) of these deaths were classified as maternal deaths following technical discussion. Thirty-five occurred during pregnancy, three during labor and 133 in the puerperium (Figure 1).
Among the women who died, 84.2% (n=144) were 20 to 39 years old, 68.4% (n=117) were Black, 60.2% (n=103) did not have a partner, 34.5% (n=59) had middle or high school education and 46.2% (n=79) were housewives. No maternal deaths were recorded in relation to indigenous women or women of Asian descent (‘yellow’ skin color) (Table 1).
Table 1 - Frequency of sociodemographic characteristics of women who died from maternal causes (n=171), Recife, Pernambuco, 2006-2017
| Characteristics | n | % |
|---|---|---|
| Age (in years) | ||
| 10-19 | 14 | 8.2 |
| 20-34 | 118 | 69.0 |
| 35-49 | 39 | 22.8 |
| Race/skin color | ||
| White | 51 | 29.8 |
| Black | 117 | 68.4 |
| Unknowna | 3 | 1.8 |
| Marital status | ||
| Had partner | 65 | 38.0 |
| Did not have partner | 103 | 60.2 |
| Unknowna | 3 | 1.8 |
| Schooling | ||
| No schooling | 15 | 8.8 |
| Primary and middle school education | 59 | 34.5 |
| High school education | 59 | 34.5 |
| Higher education | 20 | 11.7 |
| Unknowna | 18 | 10.5 |
| Occupation | ||
| Housewife | 79 | 46.2 |
| Worked in trade/business | 20 | 11.7 |
| Student | 16 | 9.4 |
| Housekeeper | 16 | 9.4 |
| Teacher | 6 | 3.5 |
| Other | 30 | 17.5 |
| Unknowna | 4 | 2.3 |
a) Corresponds to the alternatives ‘Unknown’ and ‘Blank’ regarding the answers available on the instruments used.
Thirty-five (20.5%) of these women did not have prenatal monitoring and 19 of them died during the puerperium. Among the women who did have prenatal care, 35 (26.5%) attended at least three appointments; five of these women died during pregnancy. The majority of prenatal consultations (59.1%; n=78) took place in ESF health centers, 34.8% (n=46) began prenatal monitoring during the first trimester of pregnancy, 64.4% (n=85) received a prenatal card (Pregnancy Card) and 7.6% (n=10) had high arterial pressure at their first consultation. Complications during pregnancy occurred in 73.1% (n=125) of the women and 46.4% (n=58) received treatment for these complications; 42.4% (n=56) of the women were referred to a high risk prenatal service, 85.7% (n=48) of whom attended appointments there and 87.4% (n=42) attended appointments at a public/philanthropic hospital/polyclinic. We found 67.8% (n=116) unknown information about immunization against tetanus and 54.4% (n=93) unknown information about attempted abortion during current pregnancy (Table 2).
Table 2 - Frequency of reproductive, pregnancy and prenatal characteristics of women who died from maternal causes (n=171), Recife, Pernambuco, 2006-2017
| Characteristics | n | % |
|---|---|---|
| Previous pregnancy | ||
| None | 49 | 28.7 |
| 1 | 43 | 25.1 |
| 2 or more | 74 | 43.3 |
| Unknowna | 5 | 2.9 |
| Attempted abortion | ||
| Yes | 5 | 2.9 |
| No | 73 | 42.7 |
| Unknowna | 93 | 54.4 |
| Tetanus vaccination | ||
| Complete | 40 | 23.4 |
| Incomplete | 13 | 7.6 |
| Not immunized | 2 | 1.2 |
| Unknowna | 116 | 67.8 |
| Community health agent visit | ||
| Yes | 57 | 33.3 |
| No | 45 | 26.3 |
| Unknowna | 69 | 40.4 |
| Complications during pregnancy | ||
| Yes | 125 | 73.1 |
| No | 21 | 12.3 |
| Unknowna | 25 | 14.6 |
| Treatment of complications during pregnancyb | ||
| Yes | 58 | 46.4 |
| No | 35 | 28.0 |
| Unknowna | 32 | 25.6 |
| Prenatal monitoring | ||
| Yes | 132 | 77.2 |
| No | 35 | 20.5 |
| Unknowna | 4 | 2.3 |
| Number of prenatal consultationsc | ||
| 1-3 | 35 | 26.5 |
| 4-6 | 40 | 30.3 |
| 7 or more | 39 | 29.6 |
| Unknowna | 18 | 13.6 |
| Type of prenatal health establishmentc | ||
| Family Health Strategy (ESF) center | 78 | 59.1 |
| Public/philanthropic hospital/polyclinic | 27 | 20.4 |
| Private hospital/consulting rooms | 24 | 18.2 |
| Unknowna | 3 | 2.3 |
| Gestational age at first prenatal consultation (in weeks)c | ||
| 1-13 | 46 | 34.8 |
| 14-26 | 45 | 34.1 |
| 27-42 | 3 | 2.3 |
| Unknowna | 38 | 28.8 |
| Prenatal card (Pregnancy Card)c | ||
| Yes | 85 | 64.4 |
| No | 7 | 5.3 |
| Unknowna | 40 | 30.3 |
| Blood pressure at first prenatal consultationc | ||
| Normal | 84 | 63.6 |
| High | 10 | 7.6 |
| Unknowna | 38 | 28.8 |
| Referral to high risk prenatal servicec | ||
| Yes | 56 | 42.4 |
| No | 54 | 40.9 |
| Unknowna | 22 | 16.7 |
| Consultation at high risk prenatal serviced | ||
| Yes | 48 | 85.7 |
| No | 6 | 10.7 |
| Unknowna | 2 | 3.6 |
| Type of high risk prenatal service establishmente | ||
| Public/philanthropic hospital/polyclinic | 42 | 87.4 |
| Private consulting rooms | 3 | 6.3 |
| Unknowna | 3 | 6.3 |
a) Corresponds to the alternatives ‘Unknown’ and ‘Blank’ regarding the answers available on the instruments used.
b) n = 125 women died from complications during pregnancy.
c) n =132 women who had prenatal consultations.
d) n = 56 women who were referred to high risk prenatal services.
e) n = 48 women who had consultations at high risk prenatal services.
The main place of delivery and abortion, for 92.7% (n=126) of the women, were maternity hospitals, 90.2% (n=120) of which were located in Recife; 19.5% (n=26) of these procedures occurred in private health establishments. Of the 171 maternal deaths studied, 121 women gave birth and 105 of these had live-born babies. Among the 15 abortions registered, nine were miscarriages and four were induced by the patient. Complications occurred in ten of the abortions, six due to infection and four due to hemorrhage. Gestational age at the time of delivery for 46.3% (n=63) of the women was between 23 and 36 weeks. The majority of deliveries were performed by obstetricians (82.6%; n=100), 61.2% (n=74) of which were surgical deliveries (Table 3).
Table 3 - Frequency of delivery and abortion characteristics of women who died from maternal causes (n=171), Recife, PE, 2006-2017
| Characteristics | n | % |
|---|---|---|
| Place of delivery/abortiona | ||
| Maternity hospital | 126 | 92.7 |
| General hospital | 6 | 4.4 |
| At home | 2 | 1.5 |
| Urgent Mobile Care Service (SAMU) | 1 | 0.7 |
| Unknownb | 1 | 0.7 |
| Type of establishment where delivery/abortion took placec | ||
| Private hospital | 26 | 19.5 |
| Public/philanthropic hospital/polyclinic/SAMU | 104 | 78.2 |
| Unknownb | 3 | 2.3 |
| Municipality of establishment where delivery/abortion took placec | ||
| Recife | 120 | 90.2 |
| Other | 13 | 9.8 |
| Gestational age at delivery/abortion (in weeks)a | ||
| ≤22 | 11 | 8.1 |
| 23-36 | 63 | 46.3 |
| 37-41 | 42 | 30.9 |
| ≥42 | 2 | 1.5 |
| Unknownb | 18 | 13.2 |
| Transfer during delivery/abortiona | ||
| Yes | 21 | 15.4 |
| No | 113 | 83.1 |
| Not hospitalized | 2 | 1.5 |
| Type of abortiond | ||
| Miscarriage | 9 | 60.0 |
| Induced by patient | 4 | 26.7 |
| Silent miscarriage | 2 | 13.3 |
| Procedures used in induced abortione | ||
| Homemade herb tea | 1 | 25.0 |
| Misoprostol | 1 | 25.0 |
| Others | 2 | 50.0 |
| Had complications resulting from abortiond | ||
| Yes | 10 | 66.7 |
| No | 3 | 20.0 |
| Unknownb | 2 | 13.3 |
| Complicationsf resulting from abortiong | ||
| Infection | 6 | 60.0 |
| Hemorrhage | 4 | 40.0 |
| Embolism | 1 | 10.0 |
| Uterine perforation | 1 | 10.0 |
| Other | 4 | 40.0 |
| Type of deliveryb | ||
| Vaginal | 45 | 37.2 |
| Cesarean | 74 | 61.2 |
| Vaginal and cesarean (in the same pregnancy) | 2 | 1.6 |
| Duration of labor (in hoursh) | ||
| ≤3 | 10 | 8.3 |
| 4-12 | 12 | 9.9 |
| >12 | 8 | 6.6 |
| Unknownb | 91 | 75.2 |
| Professional who performed the deliveryh | ||
| Obstetrician | 100 | 82.6 |
| Other | - | - |
| Unknownb | 21 | 17.4 |
| Anamnesis filled inh | ||
| Yes | 45 | 37.2 |
| No | 28 | 23.1 |
| Unknownb | 48 | 39.7 |
| Partogram filled inh | ||
| Yes | 9 | 7.4 |
| No | 72 | 59.5 |
| Unknownb | 40 | 33.1 |
| Companion during laborh | ||
| Yes | 30 | 24.8 |
| No | 22 | 18.2 |
| Unknownb | 69 | 57.0 |
| Had complications during laborh | ||
| Yes | 46 | 38.0 |
| No | 58 | 47.9 |
| Unknownb | 17 | 14.1 |
| Complicationsi during laborj | ||
| Hemorrhage | 14 | 30.4 |
| Fetal distress | 10 | 21.7 |
| Pre-eclampsia | 9 | 19.6 |
| Stillborn fetus | 6 | 13.0 |
| Eclampsia | 5 | 10.9 |
| HELLP syndromel | 3 | 6.5 |
| Other | 47 | 102.2 |
a) n = 136 women who had delivery/abortion.
b) Corresponds to the alternatives ‘Unknown’ and ‘Blank’ regarding the answers available on the instruments used.
c) n = 133 women whose delivery/abortion took place in a health establishment.
d) n = 15 women who had an abortion.
e) n = 4 women who induced abortion.
f) On the investigation form, the ‘Type of complications due to abortion’ variable allows more than one answer.
g) n = 10 women who had complications due to abortion.
h) n = 121 women who gave birth.
i) On the investigation form, the ‘Type of complications during childbirth’ variable allows more than one answer.
j) n = 46 women who had complications during childbirth.
l) HELLP: hemolysis, elevated liver enzymes and low platelets.
Anamnesis was not recorded on 28 medical records (23.1%), and there was no record of a partogram on 72 medical records (59.5%). We found that 38.0% (n=46) had complications during delivery, the main ones being hemorrhage (30.4%; n=14) and fetal distress (21.7%; n=10). No companion was present at 18.2% (n=22) of deliveries (Table 3).
Most maternal deaths occurred in the early puerperium (57.3%; n=98), during pregnancy and the late puerperium (both: 20.5%; n=35), and during labor (1.7%; n=3). Complications during the puerperium occurred in 94% (n=125) of these deaths, due above all to infection (24.0%; n=30), hemorrhage (23.2%; n=29) and cardiovascular problems (19.2%; n=24). 10.4% (n=13) of cases of complications during the puerperium did not receive treatment. Almost half (47.4%; n=81) the corpses were submitted to autopsies, 69.2% (n=56) of which involved examination of the uterus and appendages (Table 4).
Table 4 - Frequency of the characteristics of puerperium and circumstances of death of women who died from maternal causes (n=171), Recife, Pernambuco, 2006-2017
| Characteristics | n | % |
|---|---|---|
| Had complications during puerperiuma | ||
| Yes | 125 | 94.0 |
| No | 2 | 1.5 |
| Unknownb | 6 | 4.5 |
| Treatment of complications during puerperiumc | ||
| Yes | 108 | 86.4 |
| No | 13 | 10.4 |
| Unknownb | 4 | 3.2 |
| Complicationsd during puerperiumc | ||
| Infection | 30 | 24.0 |
| Hemorrhage | 29 | 23.2 |
| Cardiovascular problems | 24 | 19.2 |
| Respiratory problems | 18 | 14.4 |
| Eclampsia | 16 | 12.8 |
| Embolism | 9 | 7.2 |
| Neoplasms | 8 | 6.4 |
| Uterine atony | 6 | 4.8 |
| Other | 27 | 21.6 |
| Time of death | ||
| During pregnancy | 35 | 20.5 |
| During labor | 3 | 1.7 |
| Early puerperium | 98 | 57.3 |
| Late puerperium | 35 | 20.5 |
| Place of death | ||
| Hospital | 163 | 95.3 |
| Other health establishments | 2 | 1.2 |
| At home | 6 | 3.5 |
| Municipality where death occurred | ||
| Recife | 160 | 93.6 |
| Others | 11 | 6.4 |
| Death avoidability criterion | ||
| Avoidable | 80 | 46.8 |
| Probably avoidable | 60 | 35.1 |
| Probably unavoidable | 24 | 14.0 |
| Inconclusive | 5 | 2.9 |
| Unknownb | 2 | 1.2 |
| Autopsy performed | ||
| Yes | 81 | 47.4 |
| No | 89 | 52.0 |
| Unknownb | 1 | 0.6 |
| Analysis of uterus and appendages during autopsye | ||
| Yes | 56 | 69.2 |
| No | 4 | 4.9 |
| Unknownb | 21 | 25.9 |
| Causes of death | ||
| Direct obstetric causes | 79 | 46.2 |
| Arterial hypertension | 17 | 9.9 |
| Embolism | 12 | 7.0 |
| Hemorrhage | 10 | 5.8 |
| Infection puerperal | 9 | 5.3 |
| Abortion | 8 | 4.7 |
| Pregnancy ending in abortion | 8 | 4.7 |
| Other complications related to labor and delivery | 5 | 2.9 |
| Infection of genitourinary tract during pregnancy | 3 | 1.8 |
| Cardiomyopathy during puerperium | 3 | 1.8 |
| Other causes | 4 | 2.3 |
| Indirect obstetric causes (complicating pregnancy, childbirth and puerperium) | 80 | 46.8 |
| Circulatory system diseases | 21 | 12.4 |
| Specified diseases and disorders | 18 | 10.5 |
| Respiratory system diseases | 14 | 8.2 |
| HIV/AIDS | 7 | 4.1 |
| Pre-existing hypertension | 5 | 2.9 |
| Communicable and parasitic diseases | 4 | 2.3 |
| Mental disorders | 4 | 2.3 |
| Digestive system diseases | 4 | 2.3 |
| Other hematologic diseases | 2 | 1.2 |
| Endocrine system diseases | 1 | 0.6 |
| Obstetric death from unspecified cause | 3 | 1.8 |
| Death from any late obstetric cause (43 days to 1 year) | 8 | 4.7 |
| Ill-defined cause | 1 | 0.6 |
a) n = 133 women who died during puerperium.
b) Corresponds to the alternatives ‘Unknown’ and ‘Blank’ regarding the answers available on the instruments used.
c) n = 125 women who had complications during puerperium.
d) On the investigation form, the ‘Type of complications due to abortion’ variable allows more than one answer.
e) n = 81 women on whom an autopsy was performed.
81.9% (n=140) of maternal deaths were classified as avoidable and probably avoidable, with indirect obstetric causes accounting for 46.8% (n=80) and direct obstetric causes accounting for 46.2% (n=79). Among the indirect obstetric causes, diseases of the circulatory system complicating pregnancy, childbirth and puerperium (CID-10: O99.4) led to the death of 21 women (12.4%). Among the direct obstetric causes, arterial hypertension (CID-10: O11/O14/O15) was responsible for 17 of maternal deaths (9.9%) (Table 4).
Discussion
Maternal deaths were most frequent among Black women, women without formal employment, women who did not have a partner, those who started prenatal monitoring late, and those who had four to six prenatal consultations. Not all the women who had complications during pregnancy received care at high risk prenatal services, and part of those who had complications during the puerperium did not receive treatment. Most deliveries/abortions took place in public or philanthropic maternity hospitals and were performed by obstetricians. The majority of complications related to abortion were infection and hemorrhage; while during the puerperium, circulatory and respiratory problems were recorded in addition to these. The majority of maternal deaths were avoidable, with arterial hypertension, embolism and hemorrhage standing out among direct obstetric causes; and with diseases of the circulatory system complicating pregnancy, childbirth and puerperium standing out among indirect obstetric causes.
Use of secondary data results in limitations: (i) possibility of underrecorded cause of maternal death on death certificates (DC), (ii) incomplete filling in of DCs and investigation sheets, as well as (iii) problems regarding the reliability of information contained on DCs and Confidential Maternal Death Investigation Sheets, thus limiting the validity of the results shown. These limitations were minimized by Recife Health Department retrieving variables from the health establishments, as well as through case discussions by the technical group of the Recife Municipal Maternal Mortality Committee. Despite problems with information quality, it is the only source of data available for monitoring maternal mortality.
The socio-economic profile we found is similar to that of Brazil as a whole, in particular with regard to characteristics that make women vulnerable, such as poverty and race/skin color.13-15 Data on ethnicity/race exposes inequalities within society, socio-economic status and unequal access to health services faced by this population.15 Black women are even more likely to be living in unfavorable contexts, in which socio-historic disadvantages are potentialized by gender violence, stigma, poverty and human rights violations.14 The consequences of higher rates of arterial hypertension, diabetes mellitus, tobacco smoking and syphilis include greater prevalence of maternal death outcomes in this specific female group.14,15
A cross-sectional study conducted with women of childbearing age in Brazilian state capital cities in the first semester of 2002 identified greater risk of maternal death among those with less than four years of schooling.16 Studies of maternal death published more recently have shown increased levels or years of schooling in relation to these deaths,6-8 and this was also identified in our study. Few years of schooling and not having a partner contribute to low family income, making it hard to break the poverty cycle, restricting access to health information and health services, as well as lack of emotional support provided by a partner, these being fundamental factors for a healthy pregnancy and recognition of women as citizens who have rights.1,17-19
In this study, the majority of women had prenatal care at Family Health centers and some of them who were referred to high risk prenatal services were not cared for accordingly. Municipalities with high Primary Health Care coverage favor prenatal care being provided close to home,20,21 even though household visits by community health agents to measure blood pressure were not found for all women in the study. Shortcomings such as these in the prenatal period prevent early diagnosis and favor the occurrence of complications during pregnancy and childbirth. A national survey of child delivery and childbirth in Brazil found that 11.5% of women referred to high risk antenatal services had difficulty in receiving care there.20
We found that some women did not have a prenatal card. Although it is an instrument of communication between the different levels of health care and is fundamental for clinical monitoring of maternal health care, the percentage of women who had a Pregnancy Card in our study was below that found by the survey on child delivery and childbirth in Brazil, according to which 90% of women stated having received the Card and 72% provided their Card to staff at the time of childbirth.20 Comprehensive health care can operate as a compensatory policy, capable of ensuring that women have adequate monitoring during pregnancy, childbirth and during the puerperium.1,19
Death of women with high-risk pregnancies is a marker of successive failures, ranging from inadequate prenatal care, to the not always successful quest for more specialized childbirth services, lack of diagnosis and lack of linkage between prenatal care services and the place where childbirth takes place.1,4,22,23 In our study we found that many women had been transferred and some of them had undergone several transfers at the time of delivery/abortion. In many cases, absence of referral by prenatal services to the place where childbirth occurs results in women seeking delivery/abortion services that are not duly equipped to provide adequate care. This fact was also identified by a qualitative study conducted in South Sudan.22 This peregrination by pregnant women was associated with severe maternal morbidity according to the 2012 survey of child delivery and childbirth: 19% of mothers who had a maternal near miss had had at least one clinical or obstetric complication during pregnancy, childbirth or in the postpartum period.24
Nearly all the deliveries of the women who died included in this study were performed in maternity hospitals by obstetricians, despite no partogram having been filled in for most of them, as well as the high proportion of cesarean sections. An international review of partogram use that included 95 studies identified that doctors were resistant to filling in partograms and were apparently indifferent to its importance as an instrument for measuring the impact of their work; another conclusion of that review was the need to establish new strategies for partogram implementation, so as to improve, among other aspects, information about indication of cesarean sections performed.25 Despite childbirth and the puerperium period resulting in physiological conditions that require basic care for the majority of women, emergencies may occur that require quick and adequate responses by qualified and more complex services prepared to deal with the risk of maternal death.1,23 Obstetric transition in Brazil is characterized by institutionalization of child delivery, following the global trend of medicalization and increased interventions at times unnecessary.21
We found that most deaths occurred in the early puerperium, a period that requires particular attention. Fortnightly household surveillance of women at risk who have recently given birth should take place up to two months following childbirth, in order to ensure timely diagnosis, referral and treatment of complications.26
The lower number of late maternal deaths we found may possibly be due to difficulties in measuring them as a result of incorrect filling in of DCs and, consequently, shortcomings in determining causa mortis.23,26 These difficulties could be minimized by increasing the surveillance period of at-risk puerperal women to one year, as well as by investigating deaths of women of childbearing age.27 Moreover, autopsy analysis of the uterus and appendages of women of childbearing age would contribute to knowledge of the real magnitude of the problem. In this study, autopsies were performed on less than half the cases and even so uterus and appendages were not examined in all these cases.
The direct obstetric causes of death we analyzed corroborated earlier studies conducted in Recife.6,13 Four out of the total number of deaths due to abortion were reported as being induced by the women in question, possibility related to unsafe practices which are a consequence of abortion being illegal in Brazil. This, however, does not prevent abortions from taking place and results in many of these deaths not being classified as maternal deaths.29,30
The leading indirect causes of death found by our study were ‘Circulatory system diseases’, ‘Respiratory system diseases’, ‘Other specified diseases and disorders’ and, in fourth place, ‘HIV/AIDS’, all of which were responsible for ‘complicating pregnancy, childbirth and puerperium’.13 ‘Other specified diseases’ have stood out in the Northeast region and in Brazil as a whole.30
This study suggests that the gains for maternal health arising from scientific and technological advances were not ensured for the women in question. The more these advances are incorporated in the Brazilian National Health System (SUS), the lower the incidence will be of diseases related to reproduction and more deaths will be avoided.1,22,25 The socio-demographic and health care profile found expresses society’s “consent” to maternal deaths, by violating women’s basic rights to sexual and reproductive health, quality and timely health care, in accordance with their needs.14,15
The majority of maternal deaths in Recife occurred in the puerperium among Black women and women who did not have a partner. We found a high proportion of avoidable deaths among the maternal deaths. Given their importance for maternal health services, we highlight the presence of shortcomings in health care in the prenatal period, during childbirth and in the puerperium: difficulty in accessing health services, insufficient monitoring, lack of timely detection of complications, low adherence to interventions based on evidence and good practices, in addition to issues related to women’s social and individual vulnerability. Our findings indicate the urgent need to enhance health surveillance and health care, as well as to develop studies with robust designs that evaluate services and make explicit social and health care inequities between different groups of the population.
REFERENCES
1. Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, et al. Vital signs: pregnancy-related deaths, United States, 2011-2015, and strategies for prevention, 13 States, 2013-2017. MMWR Morb Mortal Wkly Rep [Internet]. 2019 May [cited 2019 Oct 2];68(18):423-9. Available from: Available from: https://www.cdc.gov/mmwr/volumes/68/wr/mm6818e1.htm [ Links ]
2. World Health Organization. United Nations Children's Fund. World Bank. United Nations. United Nations Population Division. Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division [Internet]. Geneva: World Health Organization; 2015 [cited 2019 Apr 10]. 77 p. Available from: Available from: https://apps.who.int/iris/bitstream/handle/10665/194254/9789241565141_eng.pdf;jsessionid=90B5E6FF8F4F1E08DFD3D62AF9F07B62?sequence=1 [ Links ]
3. Organização das Nações Unidas. Transformando nosso mundo: a agenda 2030 para o desenvolvimento sustentável [Internet]. Rio de Janeiro: Nações Unidas; 2015 [citado 2016 fev 18]. 41 p. Disponível em: Disponível em: https://www.undp.org/content/dam/brazil/docs/agenda2030/undp-br-Agenda2030-completo-pt-br-2016.pdf [ Links ]
4. Szwarcwald CL, Escalante JJC, Rabello Neto DL, Souza Junior PRB, Victora CG. Estimação da razão de mortalidade materna no Brasil, 2008-2011. Cad Saúde Pública [Internet]. 2014 [citado 2019 out 2];30(Suppl 1):S71-S83. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v30s1/0102-311X-csp-30-s1-0071.pdf . doi: 10.1590/0102-311X00125313 [ Links ]
5. Zoca B, Escalante JJC, Viola RC, Lecca RCR. Morbimortalidade materna: tendências, causas e investigação de óbitos. In: Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise de Situação em Saúde. Saúde Brasil 2013: uma análise da situação da saúde e das doenças transmissíveis relacionadas à pobreza [Internet]. Brasília: Ministério da Saúde; 2014 [citado 2018 nov 15]. 41-64 p. Disponível em:Disponível em:http://bvsms.saude.gov.br/bvs/publicacoes/saude_brasil_2013_analise_situacao_saude.pdf [ Links ]
6. Correia RA, Araújo HC, Furtado BMA, Bonfim C. Características epidemiológicas dos óbitos maternos ocorridos em Recife, PE, Brasil (2000-2006). Rev Bras Enferm [Internet]. 2011 jan-fev [citado 2019 out 2];64(1):91-7. Disponível em: Disponível em: http://www.scielo.br/pdf/reben/v64n1/v64n1a14.pdf . doi: 10.1590/S0034-71672011000100014 [ Links ]
7. Martins ACS, Silva LS. Epidemiological profile of maternal mortality. Rev Bras Enferm [Internet]. 2018 [cited 2019 Oct 2];71(Suppl 1):677-83. Available from: Available from: http://www.scielo.br/pdf/reben/v71s1/0034-7167-reben-71-s1-0677.pdf . doi: 10.1590/0034-7167-2017-0624 [ Links ]
8. Biano RKC, Souza PCB, Ferreira MBG, Silva SR, Ruiz MT. Mortalidade materna no Brasil e nos municípios de Belo Horizonte e Uberaba, 1996 a 2012. Rev Enferm Centro-Oeste Mineiro [Internet]. 2017 [citado 2019 out 2];7:e1464. Disponível em: Disponível em: http://www.seer.ufsj.edu.br/index.php/recom/article/view/1464/1575 . doi: 10.19175/recom.v7i0.1464 [ Links ]
9. Brasil. Ministério da Saúde. Portaria MS/GM nº 1.119, de 5 de junho de 2008. Regulamenta a vigilância de óbitos maternos [Internet]. Diário Oficial União, Brasília (DF), 2008 jun 06 [citado 2019 out 2]; Seção1: 48. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2008/prt1119_05_06_2008.html [ Links ]
10. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise de Situação em Saúde. Guia de vigilância epidemiológica do óbito materno [Internet]. Brasília: Ministério da Saúde ; 2009 [citado 2019 out 2]. 84 p. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/guia_vigilancia_epidem_obito_materno.pdf [ Links ]
11. Instituto Brasileiro de Geografia e Estatística. Censo demográfico 2010 [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2010 [citado 2018 nov 10]. Disponível em: Disponível em: https://cidades.ibge.gov.br/brasil/pe/recife/pesquisa/23/25888?detalhes=true%2Fhttps:%2F%2Fwww.ibge.gov.br%2Festatisticas-novoportal%2Fsociais%2Fpopulacao%2F9662-censo-demografico-2010.html [ Links ]
12. Ministério da Saúde (BR). Departamento de Informática do SUS. Cadastro nacional de estabelecimentos de saúde: consulta profissional [Internet]. Brasília: Ministério da Saúde ; 2019 [citado 2019 abr 1]. Disponível em: Disponível em: http://cnes.datasus.gov.br/pages/profissionais/consulta.jsp [ Links ]
13. Leite RMB, Araújo TVB, Albuquerque RM, Andrade ARS, Duarte Neto PJ. Fatores de risco para mortalidade materna em área urbana do Nordeste do Brasil. Cad Saúde Publica [Internet]. 2011 out [citado 2019 out 2];27(10):1977-85. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v27n10/11.pdf . doi: 10.1590/S0102-311X2011001000011 [ Links ]
14. Taquette Stella R. Interseccionalidade de gênero, classe e raça e vulnerabilidade de adolescentes negras às DST/aids. Saúde Soc [Internet]. 2010 [citado 2019 out 2];19(Suppl 2):51-62. Disponível em: Disponível em: http://www.scielo.br/pdf/sausoc/v19s2/06.pdf . doi: 10.1590/S0104-12902010000600006 [ Links ]
15. Pícoli RP, Cazola LHO, Lemos EF. Mortalidade materna segundo raça/cor, em Mato Grosso do Sul, Brasil, de 2010 a 2015. Rev Bras Saúde Matern Infant [Internet]. 2017 out-dez [citado 2019 out 2];17(4):739-47. Disponível em: Disponível em: http://www.scielo.br/pdf/rbsmi/v17n4/pt_1519-3829-rbsmi-17-04-0729.pdf . doi: 10.1590/1806-93042017000400007 [ Links ]
16. Laurenti R, Mello Jorge MHP, Gotlieb SLD. A mortalidade materna nas capitais brasileiras: algumas características e estimativa de um fator de ajuste. Rev Bras Epidemiol [Internet]. 2004 dez [citado 2019 out 2];7(4):449-60. Disponível em: Disponível em: http://www.scielo.br/pdf/rbepid/v7n4/08.pdf . doi: 10.1590/S1415-790X2004000400008 [ Links ]
17. Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards millennium development goal 5. Lancet [Internet]. 2010 Apr [cited 2019 Oct 2];375:1609-23. Available from: Available from: https://www.thelancet.com/article/S0140-6736(10)60518-1/abstract . doi: 10.1016/S0140-6736(10)60518-1 [ Links ]
18. United Nations. Millennium development goals and beyond 2015 [Internet]. New York: United Nations; 2013 [cited 2016 Dec 7]. Available from: Available from: https://www.un.org/millenniumgoals/pdf/Goal_5_fs.pdf [ Links ]
19. Dias JMG, Oliveira APS, Cipolotti R, Monteiro BKSM, Pereira RO. Mortalidade materna. Rev Med Minas Gerais [Internet]. 2015 [citado 2019 out 2];25(2):173-9. Disponível em: Disponível em: http://www.rmmg.org/artigo/detalhes/1771 . doi: 10.5935/2238-3182.20150034 [ Links ]
20. Viellas EF, Domingues RMSM, Dias MAB, Gama SGN, Theme Filha MM, Costa JV, et al. Assistência pré-natal no Brasil. Cad Saúde Pública [Internet]. 2014 [citado 2019 out 2];30(Supl1):S85-S100. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v30s1/0102-311X-csp-30-s1-0085.pdf . doi: 10.1590/0102-311X00126013 [ Links ]
21. Leal MC, Szwarcwald CL, Almeida PVB, Aquino EML, Barreto ML, Barros F, et al. Saúde reprodutiva, materna, neonatal e infantil nos 30 anos do Sistema Único de Saúde (SUS). Ciênc Saúde Coletiva [Internet]. 2018 jun [citado 2019 out 2];23(6):1915-28. Disponível em: Disponível em: http://www.scielo.br/pdf/csc/v23n6/1413-8123-csc-23-06-1915.pdf . doi: 10.1590/1413-81232018236.03942018 [ Links ]
22. Elmusharaf K, Byrne E, AbuAgla A, AbdelRahim A, Manandhar M, Sondorp E, et al. Patterns and determinants of pathways to reach comprehensive emergency obstetric and neonatal care (CEmONC) in South Sudan: qualitative diagrammatic pathway analysis. BMC Pregnancy Childbirth [Internet]. 2017 Aug [cited 2019 Oct 2];17:278. Available from: Available from: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-017-1463-9 [ Links ]
23. Vega CEP, Soares VMN, Nasr AMLF. Late maternal mortality: comparison of maternal mortality committees in Brazil. Cad Saúde Publica [Internet]. 2017 [cited 2019 Oct 2];33(3):e00197315. Available from: Available from: http://www.scielo.br/pdf/csp/v33n3/1678-4464-csp-33-03-e00197315.pdf . doi: 10.1590/0102-311x00197315 [ Links ]
24. Domingues RM, Dias MA, Schilithz AO, Leal MD. Factors associated with maternal near miss in childbirth and the postpartum period: findings from the birth in Brazil National Survey, 2011-2012. Reprod Health [Internet]. 2016 Oct [cited 2019 Oct 2];13(Suppl 3):115. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5073804/ . doi: 10.1186/s12978-016-0232-y [ Links ]
25. Bedwell C, Levin K, Pett C, Lavender DT. A realist review of the partograph: when and how does it work for labour monitoring? BMC Pregnancy Childbirth [Internet]. 2017 Jan [cited 2019 Oct 2];17:31. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5237234/ . doi: 10.1186/s12884-016-1213-4 [ Links ]
26. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Pré-natal e puerpério: atenção qualificada e humanizada [Internet]. Brasília: Ministério da Saúde ; 2006 [citado 2019 out 2]. 163 p. (Série A. Normas e Manuais Técnicos); (Série Direitos Sexuais e Direitos Reprodutivos - Caderno no 5). Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/manual_pre_natal_puerperio_3ed.pdf [ Links ]
27. Jentoft S, Nielsen VO, Roll-Hansen D. Adjusting maternal mortality data for international comparisons: The case of vital registration systems. Statistics Norway [Internet]. 2014 Mar [cited 2019 Oct 2];773. Available from: Available from: https://www.ssb.no/en/forskning/discussion-papers/_attachment/168855 . [ Links ]
28. Victora CG, Aquino EML, Leal MC, Monteiro CA, Barros FC, Szwarcwald CL, et al. Maternal and child health in Brazil: progress and challenges. Lancet [Internet]. 2011 May [cited 2019 Oct 2];377(9780):1863-76. Available from: Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(11)60138-4/fulltext . doi: 10.1016/S0140-6736(11)60138-4 [ Links ]
29. Martins EF, Almeida PFB, Paixão CO, Bicalho PG, Errico LSP. Causas múltiplas de mortalidade materna relacionada ao aborto no Estado de Minas Gerais, Brasil, 2000-2011. Cad Saúde Pública [Internet]. 2017 [citado 2019 out 2];33(1):e00133115. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v33n1/1678-4464-csp-33-01-e00133115.pdf . doi: 10.1590/0102-311x00133116 [ Links ]
30. Silva BGC, Lima NP, Silva SG, Antúnez SF, Seerig LM, Restrepo-Méndez MC, et al. Mortalidade materna no Brasil no período de 2001 a 2012: tendência temporal e diferenças regionais. Rev Bras Epidemiol [Internet]. 2016 jul-set [citado 2019 out 2];19(3):484-93. Disponível em: Disponível em: http://www.scielo.br/pdf/rbepid/v19n3/1980-5497-rbepid-19-03-00484.pdf . doi: 10.1590/1980-5497201600030002 [ Links ]
*Article derived from data collected for the Ph.D. dissertation entitled ‘Maternal mortality in Pernambuco: magnitude, health care trajectory and social cost’, to be submitted by Patrícia Ismael de Carvalho to the Postgraduate Program in Comprehensive Medicine/Ph.D. Course at the Professor Fernando Figueira Comprehensive Medicine Institute in 2020.
Received: May 30, 2019; Accepted: September 21, 2019










 texto en
texto en