Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.1 Brasília 2020 Epub 13-Mar-2020
http://dx.doi.org/10.5123/s1679-49742020000100016
ORIGINAL ARTICLE
Temporal trend of HIV/AIDS cases in the state of Minas Gerais, Brazil, 2007-2016*
1Universidade de São Paulo, Programa de Pós-Graduação Stricto Sensu em Saúde na Comunidade, Ribeirão Preto, SP, Brasil
2Universidade Federal do Triângulo Mineiro, Programa de Pós-Graduação Strictu Sensu em Inovação Tecnológica, Uberaba, MG, Brasil
3Universidade de Uberaba, Faculdade de Odontologia, Uberaba, MG, Brasil
4Faculdade Alfredo Nasser, Faculdade de Medicina, Aparecida de Goiânia, GO, Brasil
Objective:
to analyze the temporal trend of Human Immunodeficiency Virus (HIV) and Acquired Immune Deficiency Syndrome (AIDS) incidence, detection and mortality coefficients in the state of Minas Gerais between 2007 and 2016.
Methods:
this was a time series study of data held on the Notifiable Health Conditions Information System (Sinan) using Prais-Winsten regression.
Results:
in the period studied, 35,349 cases were notified, with predominance of sexually transmitted cases (81.7%), 50.3% of which were heterosexual cases and 22.8% were homosexual cases. AIDS incidence increased (annual change 1.6%; 95%CI 0.0;3.3) as did HIV detection (annual change 60.3%; 95%CI 22.9;109.0). The mortality rate was stationary; HIV+ notifications increased from 3.8% in 2007 to 65.1% in 2016.
Conclusion:
the growing trend of HIV+ detection coincided with the government strategy to identify cases. AIDS incidence increased.
Keywords: Acquired Immunodeficiency Syndrome; HIV; Time Series Studies; Notification
Introduction
Acquired Immune Deficiency Syndrome (AIDS) is an important public health problem, considering its severity, its pandemic nature, discrimination and high costs of prevention and treatment. With the increase of survival time and quality of life,1 as well as the implementation of public policies that ensure testing and treatment,2,3 the disease is now considered to be a chronic condition, with epidemiological implications and challenges for global public health.4,5 Countries face challenges to increasing social equality and access to tests for diagnosis of human immunodeficiency virus (HIV) infection,6 and incidence rates vary substantially.
Forty percent of the 35,000 new cases of HIV infection occurring every year in Brazil are diagnosed late.3 In order to alter this reality, notification of infected people became compulsory nationwide with effect from the implementation of Health Ministry Ordinance No. 1271 in June 2014.7 This notification supports the policy of provision of antiretroviral treatment following HIV diagnosis, regardless of CD4 cell count or stage of the disease.8 Moreover, advertising campaigns have been intensified encouraging the population to test for HIV. Nevertheless, early testing is still a national challenge.
Early diagnosis contributes to reducing morbidity and mortality, as does adherence to antiretroviral therapy (ART). According to the HIV/AIDS Epidemiological Bulletin (2017),9 882,810 HIV/AIDS cases had been recorded in Brazil as at July 2017, with 65.3% of cases in males and case concentration in the Southeast region (52.3%). With effect from the early 2000s, there has been a reduction in the population that has never tested and an increase in adherence to treatment.
With effect from 2009, there has been a reduction in AIDS cases among females and an increase among males, especially among males aged 13-19 and those in the category of men who have sex with men (MSM). A 30% increase in the detection rate among pregnant women also occurred between 2004 and 2014. Several transformations in the epidemiological profile of the disease have been observed since its emergence, including virus transmission outside risk groups, so that the possibility of all people being infected has expanded.10
Updating knowledge about epidemiological dynamics in different regions, in diverse cultures, including specificities with regard to public policies and access to health services for people living with HIV/AIDS (PLWHA), contributes to revealing the regional behavior of the disease with a view to improving prevention and control strategies. Access to diagnosis and treatment, adherence to antiretroviral therapy and forms of contagion/transmission can have regional specificities.2,7
The temporal trend of HIV/AIDS incidence, detection and mortality rates assists with evaluation of infection prevention and control strategies in the country’s diverse regions. As such, the purpose of this study was to analyze the temporal trend of HIV/AIDS incidence, detection and mortality rates in the state of Minas Gerais between 2007 and 2016.
Methods
This was an ecological study using a time series analysis approach.
We used anonymized data from the Notifiable Health Conditions Information System (Sinan), provided by the Minas Gerais State Health Department (SES/MG), for the period 2007-2016, containing notified cases of HIV/AIDS in people aged 13 years and over resident in the state.
Minas Gerais has 853 municipalities and is Brazil’s second most populous state. The state’s Human Development Index (HDI) was 0.731 in 2010, although sharp inequalities exist between the state’s regions.11
The variables used in the study were age range (13-19 years, 20-29 years, 30-39 years, 40-49 years, 50-59 years, 60 years and over), sex (male or female), skin color/race (white, brown, black, yellow, indigenous), schooling (illiterate, elementary education, high school education, higher education), zone of residence (urban, rural), exposure category (heterosexual, bisexual, homosexual, drug use, accident involving biological material, other), laboratory test result (positive, negative, inconclusive), pregnant (yes, no, does not apply), case definition criteria (Adapted CDC, Rio de Janeiro/Caracas, HIV, death from HIV/AIDS),12 disease progression (alive, death from AIDS, death from other causes) and concomitant infections/diseases (cytomegalovirus, intestinal isosporidiosis, intestinal cryptosporidiosis, disseminated histoplasmosis, disseminated mycobacteriosis, invasive cervical cancer, salmonella infections, Chagas disease reactivation, primary cerebral lymphoma, cachexia, asthenia, anemia, lymphopenia, thrombocytopenia, oral candidiasis, encephalopathy, lymphadenopathy, hairy leukoplakia, temperature above 38ºC for more than a month, diarrhea for one month or more, persistent dermatitis, persistent cough or pneumonia, central nervous system dysfunction, CD4+ T count <350cells/mm3, esophageal candidiasis, Pneumocystis jirovece pneumonia, cerebral toxoplasmosis, herpes simplex, extrapulmonary cryptococcosis, tracheobronchial/esophageal candidiasis, chronic intestinal leukoencephalopathy, mucocutaneous herpes simplex for more than 1 month, herpes zoster in <60 year-olds, Kaposi’s sarcoma, tuberculosis).
The following indictors were used for the study: AIDS incidence rate (number of new AIDS cases notified in the period and region/population >13 years old x 105), HIV/AIDS mortality rate (number of HIV/AIDS deaths notified in the period and region/population >13 years old x 105) and HIV+ detection rate (number of HIV+ cases notified in the period and region/population >13 years old x 105). These indicators were calculated for each year comprising the period 2007-2016. Population estimates provided by the Brazilian Institute of Geography and Statistics (IBGE) were used as the denominators.
For the temporal trend analyses, we used generalized and standardized Prais-Winsten linear regression models to quantify annual percentage change (APC) in the indicators, with their respective 95% confidence intervals. Positive APC indicated that the series was considered to be increasing; while negative APC indicated decreasing series; and, when no statistically significant difference was found, the trend was considered to be stationary.13 The analyses were performed using IBM SPSS Statistics, version 20.
This study was approved by the Triângulo Mineiro Federal University (UFTM) Research Ethics Committee on June 5th 2017, as per approval report number 2.099.176. The database was provided with no variables capable of enabling identification of the research subjects.
Results
Between 2007 and 2016, 35,349 HIV/AIDS cases were recorded in the state of Minas Gerais. The AIDS incidence rate increased from 12.4 cases/100,000 inhabitants in 2007 to 14.0 cases/100,000 inhab. in 2016, while the HIV+ detection rate increased from 0.5 cases/100,000 inhab. in 2007 to 27.2 cases/100,000 inhab. in 2016.
The time series analysis (Figure 1) reveals an increase in the HIV+ detection rate, with percentage annual change of 60.3% (95%CI 22.9;109.0; p=0.005). The AIDS incidence rate also showed an increasing trend, with percentage annual change of 1.6% (95%CI 0.0;3.3; p=0.039). The mortality rate remained stationary, with -2.5% annual change (95%CI -10.4; 6.1; p=0.521). The increase in the HIV/AIDS incidence coefficient was found in all age ranges (Figure 2).

Figure 1 - Temporal progression of AIDS incidence, HIV detection and HIV/AIDS mortality coefficients, Minas Gerais, 2007-2016
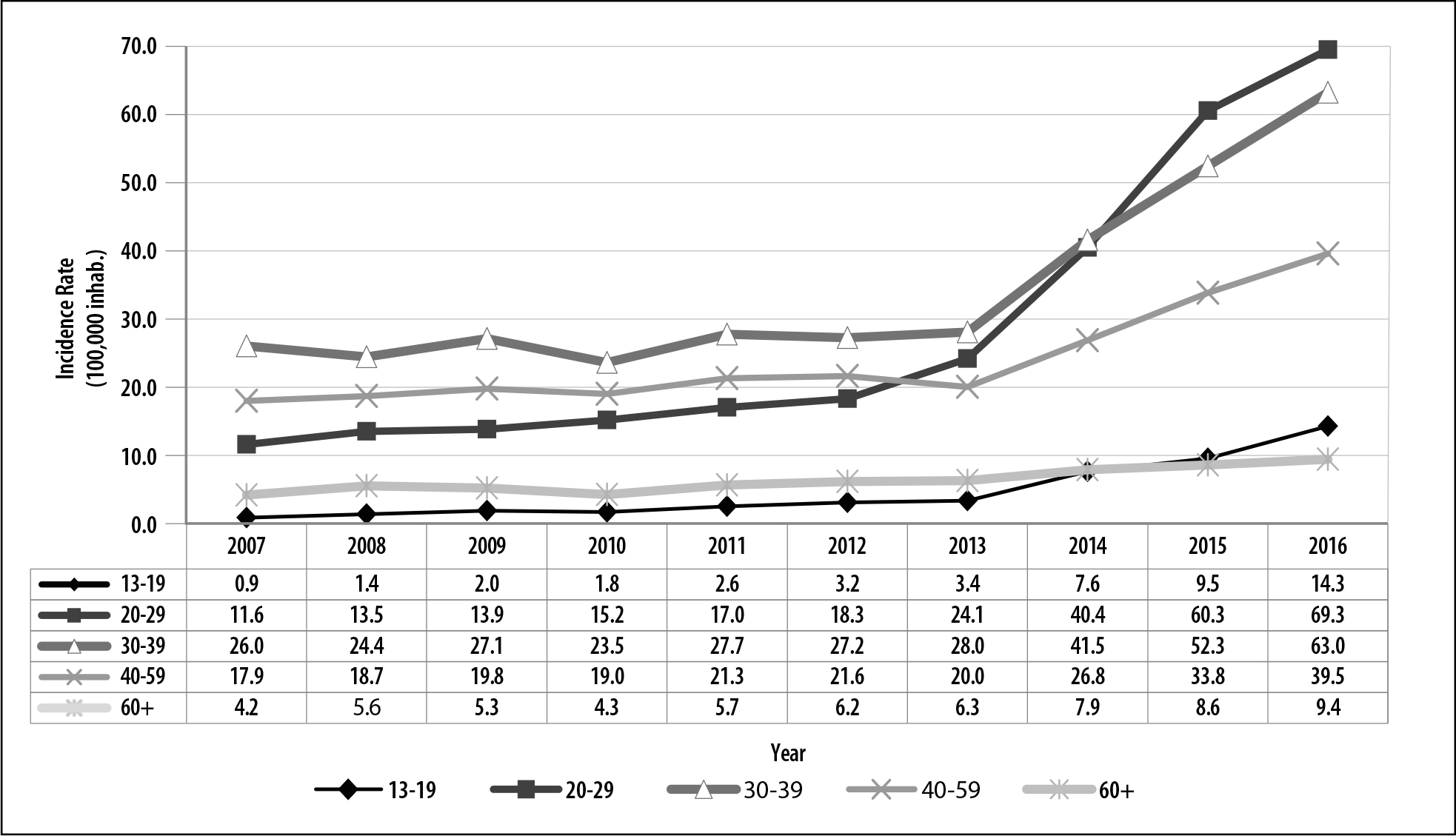
Figure 2 - Distribution of HIV/AIDS incidence/detection coefficients (per 100,000 inhabitants) by age range, Minas Gerais, 2007-2016
The average age of HIV/AIDS cases was 37.3 years (SD 11.9 years), with median age of 35.6 years and the interquartile rage was [28.1; 45.0]. Case concentration was greater in the 20-29, 30-39 and 40-59 years age groups, being 30.8% on average in each of them. The majority of cases were male (n=23,982; 67.8%), of white (n=13,921; 39.4%) or brown (n=11,094; 31.4%) skin color/race, had elementary schooling (n=11,244; 31.8%) and lived in the urban zone (n=32,800; 92.8% - data not shown in tables).
Transmission was predominantly sexual (81.7% of cases), followed by blood-borne transmission owing to drug use (3.4% of cases). Infection was most predominant in heterosexuals (50.3%), followed by homosexuals (22.8%) and bisexuals (5.4%) (Table 1). 89.5% of HIV/AIDS infected cases were identified by screening tests, 84.1% of which had reactive/positive confirmatory test results. This test was not performed in 7.2% of cases.
Table 1 - HIV/AIDS case distribution by case definition criteria, progression, pregnancy and exposure category, Minas Gerais, 2007-2016 (N= 35,349)
| Case definition criteria | N | % |
|---|---|---|
| Adapted CDCa | 21,431 | 60.6 |
| HIV+b | 11,116 | 31.4 |
| Rio de Janeiro/Caracas | 1,979 | 5.6 |
| HIVc/AIDS death | 823 | 2.4 |
| Progression | ||
| Alive | 30,369 | 85.9 |
| AIDS death | 3,836 | 10.9 |
| Unknown | 788 | 2.2 |
| Death from other causes | 356 | 1.0 |
| Pregnant woman | ||
| Yes | 541 | 1.5 |
| No | 7,820 | 22.1 |
| Does not apply | 25,767 | 72.9 |
| Unknown | 1,221 | 3.5 |
| Exposure category (not exclusive) | ||
| Heterosexual | 17,784 | 50.3 |
| Homosexual | 8,051 | 22.8 |
| Unknown | 6,102 | 17.3 |
| Bisexual | 1,918 | 5.4 |
| Drugs | 1,463 | 4.1 |
| Perinatal | 255 | 0.7 |
| Other | 41 | 0.1 |
| Accident involving biological material and seroconversion | 6 | 0.0 |
a) CDC: AIDS case definition criterion for notification adapted from Centers for Disease Control and Prevention - CDC.
b) HIV+: case definition criterion for notification being infected with HIV.
c) HIV: human immunodeficiency virus.
The case definition criterion used for notifying the majority of HIV/AIDS cases was the Centers for Disease Control and Prevention criterion adapted to Brazil (Adapted CDC), accounting for 60.6% of cases, although this gradually reduced after 2014, and was replaced by the being HIV+ criterion. In turn, notifications using the being HIV+ criterion accounted for 31.4% of cases and increased in the period, from 3.8% in 2007 to 65.1% in 2016. A reduction of 54.7% was found in cases notified using the Rio de Janeiro/Caracas criterion. The AIDS-related death notification criterion accounted for 827 cases (2.3%), meaning that death was certified as being AIDS or HIV-related and that cause of death was associated with immunodeficiency, and was not classified according to other criteria following investigation. With regard to case progression, 30,369 cases (85.9%) were alive at the time of notification. Only 1.5% of cases were pregnant women (Tables 1 and 2).
Table 2 - Proportional HIV/AIDS case distribution by case definition criteria per annum, Minas Gerais, 2007-2016
| Year | Adapted CDCa | HIV+b | Rio de Janeiro/Caracasc | Criterion death | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| 2007 | 1,702 | 81.9 | 78 | 3.7 | 196 | 9.4 | 103 | 5.0 |
| 2008 | 1,848 | 83.7 | 89 | 4.0 | 167 | 7.6 | 103 | 4.7 |
| 2009 | 2,133 | 89.0 | 47 | 2.0 | 151 | 6.3 | 65 | 2.7 |
| 2010 | 2,017 | 87.3 | 89 | 3.8 | 128 | 5.5 | 76 | 3.3 |
| 2011 | 2,349 | 86.9 | 99 | 3.7 | 164 | 6.1 | 91 | 3.4 |
| 2012 | 2,365 | 84.1 | 183 | 6.5 | 192 | 6.8 | 72 | 2.6 |
| 2013 | 2,231 | 74.1 | 571 | 19.0 | 157 | 5.2 | 53 | 1.8 |
| 2014 | 2,269 | 49.9 | 2,010 | 44.2 | 211 | 4.6 | 60 | 1.3 |
| 2015 | 2,407 | 39.7 | 3,252 | 53.6 | 305 | 5.0 | 100 | 1.6 |
| 2016 | 2,110 | 29.2 | 4,698 | 65.1 | 308 | 4.3 | 100 | 1.4 |
| Total | 21,431 | 60.6 | 11,116 | 31.5 | 1,979 | 5.6 | 823 | 2.3 |
a) Adapted CDC: AIDS case definition criterion for notification adapted from Centers for Disease Control and Prevention - CDC.
b) HIV+: case definition criterion for notification being infected with HIV.
c) Rio de Janeiro/Caracas: case definition for notification according to the Rio de Janeiro/Caracas Criterion.
The most frequent infections in AIDS cases defined using the Adapted CDC criterion were: CD4+ T lymphocyte count <350 cells/mm3 (14.8%), esophageal candidiasis (10.4%), Pneumocystis jiroveci pneumonia (6.8%), cerebral toxoplasmosis (5.8%) and mucocutaneous herpes simplex for more than one month (2.6%) (Table 3).
Table 3 - Distribution of notified HIV/AIDS cases by Adapted CDCa and Rio de Janeiro/Caracas Criteria, Minas Gerais, 2007-2016
| Rio de Janeiro/Caracas Criterion* | N | % |
|---|---|---|
| Cachexia with weight loss >10 | 9,996 | 28.3 |
| Asthenia >1 month | 8,469 | 24.0 |
| Anemia and/or lymphopenia and/or thrombocytopenia | 6,071 | 17.2 |
| Oral candidiasis or hairy leukoplakia | 5,996 | 17.0 |
| Temperature >38ºC for >1 month | 5,348 | 15.1 |
| Diarrhea for 1 month or more | 5,115 | 14.5 |
| Persistent dermatitis | 4,126 | 11.7 |
| Persistent cough or any form of pneumonia | 3,160 | 8.9 |
| Lymphadenopathy >1cm, >2 extrainguinal sites for >1 month | 3,038 | 8.6 |
| Central nervous system dysfunction | 2,385 | 6.7 |
| Herpes zoster in <60 year-olds | 1,694 | 4.8 |
| Pulmonary cavitary or unspecified tuberculosis | 1,364 | 3.9 |
| Disseminated/extrapulmonary/non-cavitary tuberculosis | 924 | 2.6 |
| Kaposi’s sarcoma | 402 | 1.1 |
| Adapted CDC Criteriona,b | ||
| CD4+ T lymphocyte count <350cells/mm3 | 5,225 | 14.8 |
| Esophageal candidiasis | 3,667 | 10.4 |
| Pneumocystis carinii pneumonia | 2,412 | 6.8 |
| Cerebral toxoplasmosis | 2,038 | 5.8 |
| Mucocutaneous herpes simplex (>1month) | 933 | 2.6 |
| Extrapulmonary cryptococcosis | 425 | 1.2 |
| Cytomegalovirus (except liver, spleen or lymph nodes) | 345 | 1.0 |
| Tracheobronchial/esophageal candidiasis | 263 | 0.7 |
| Progressive multifocal leukoencephalopathy | 228 | 0.6 |
| Non-Hodgkin lymphoma and other lymphomas | 192 | 0.5 |
| Chronic intestinal isosporiasis (>1month) | 151 | 0.4 |
| Chronic intestinal cryptosporidiosis (>1 month) | 150 | 0.4 |
| Disseminated histoplasmosis | 126 | 04 |
| Disseminated mycobacteriosis (except tuberculosis and leprosy) | 98 | 0.3 |
| Invasive cervical cancer | 69 | 0.2 |
| Salmonella infections (recurrent non-typhoidal septicemia) | 53 | 0.1 |
| Chagas disease reactivation | 45 | 0.1 |
| Primary cerebral lymphoma | 41 | 0.1 |
a) Adapted CDC: AIDS case definition criterion for notification adapted from Centers for Disease Control and Prevention - CDC.
b) Criteria not mutually exclusive.
The Rio de Janeiro/Caracas criterion defined 5.6% of AIDS cases, with the following being most frequent: cachexia (28.3%), asthenia for more than one month (24.0%), anemia and/or lymphopenia and/or thrombocytopenia (17.2%), oral candidiasis or hairy leukoplakia (17,0%), temperature above 38ºC for more than one month (15.13%), diarrhea for one month or more (14.5%) and persistent dermatitis (11.7%) (Table 3).
Discussion
The number of PLWHA increased in the state of Minas Gerais, as did the AIDS incidence rate and the HIV detection rate. This indicates that the strategy of identifying HIV positive people and strengthening the epidemiological surveillance system has been successful in the state. Corroborating this, there was a reduction in the proportion of notifications made according to the Adapted CDC and Rio de Janeiro/Caracas criteria, stabilization in AIDS-related deaths and an increase in notifications using the being HIV+ criterion.
AIDS is treated as a chronic disease, and quality of life and life expectancy is better in countries that provide access to ART. Brazil has provided antiretroviral drugs free of charge to all diagnosed PLWHA since 2013,14,15 and the effects of this can be perceived in reduced hospitalizations, mortality, mother-to-child transmission and opportunistic infections.4,16 Approaching AIDS as a chronic disease may be reflected in the reduction in people’s fear of testing, so that there may be a gradual increase, as indicated in this study, following obligatory notification of HIV cases. It should be noted that notification is not restricted to newly identified cases, since health services can also record HIV cases identified before notification became compulsory.
According to Greco15 and Maksud et al.,14 making antiretroviral therapy available regardless of the number of CD4 T lymphocytes should be evaluated carefully.16,14 In the case of PLWHA with CD4 counts above 500, presumably asymptomatic, the need may exist for early 2nd and 3rd line treatment regimens; on the other hand, risk of severe disease or death in patients starting treatment early is reduced by 53.0% when compared to those who start treatment late.16
Ever since the beginning of the epidemic in Brazil, the country’s response has included local condom and antiretroviral production and distribution, human rights defense, laboratory networks and specialized services.3,16 The challenges facing monitoring and control of the epidemic include increased access to diagnostic tests5 - since approximately half of all PLWHA are not aware of their serological status - as well as the elimination of discrimination related to HIV infection.6
Failure to use condoms in all sexual intercourse is a reality found in many countries. New prevention technologies now available should be seen as methods to assist with reducing HIV incidence, since some aspects of these strategies have not yet been evaluated in depth, as is the case of medicalization of HIV prevention, which may result in unsafe sexual practices and potential adverse effects in the long term.14
Deaths showed a stationary trend in Minas Gerais. Stabilization of deaths may be related to use of ART, which results in greater survival time and deaths not attributed to HIV. In Minas Gerais the Notifiable Health Conditions Information System (Sinan) is updated when people who have HIV become classified as AIDS cases or when their death is related to HIV infection, and this has contributed to the system’s greater sensitivity in relation to deaths.
A study conducted in relation to the period 1997-2012 using inpatient medical records from 31 hospitals located in the interior part of São Paulo state, following ART introduction, found that 54.5% of PLWHA hospitalizations were due to communicable diseases, especially opportunistic infections that define AIDS cases (32.7%), and that deaths were 42% higher and average number of inpatient days was greater (11.2 days) among hospitalized males than among hospitalized females, indicating the limited effect of antiretroviral drug use on reducing the occurrence of opportunistic infections, which may also be attributed to low adherence to ARV therapy.17 It should be highlighted that the period 1997-2012 is prior to obligatory HIV notification regardless of CD4 cell levels. This may have influenced the frequency and severity of opportunistic infections attributed to AIDS and to hospitalizations. New studies on the profile of hospitalizations and adherence to ARV therapy need to be conducted in relation to the period after which HIV notification became compulsory, in order to evaluate the cost-benefit and impact of this government strategy on ARV use by all HIV positive cases as well as use of pre-exposure prophylaxis. In this study it was not possible to formally evaluate conditions before and after the start of obligatory HIV notification, given that the study covered a period of eight years prior to this and only three years following this.
A higher proportion of males was found among notified cases (67.8%), and this was also found in several reports in the literature.18-20 A study conducted with females in 2003/2004, in state capitals and large cities, found that spontaneous serological testing was low (12.7%); the majority of them sought testing when AIDS symptoms appeared (24.6%), having a spouse with AIDS (24.7%) or found out during antenatal care (19.5%),21 which may contribute to the higher proportion of male cases identified. Based on Brazilian and international literature, however, these findings do not suggest that low spontaneous serological testing among women represents a change in the epidemiological profile of the disease.
In this study, sexual transmission and transmission between heterosexuals were predominant. A study of 4,666 AIDS cases conducted in the state of Rio Grande do Norte covering the period 1980-2013, found that male heterosexuals were the most frequent exposure category (66.6%), which is similar to the results of our study.22 A study conducted in Anápolis/GO for the period 2009-2013, found that 61.3% of cases were heterosexual, 24.5% were homosexual and that sexual transmission accounted for 61.3%,23 this percentage being lower than that found in our study. However, Grangeiro et al.15 indicate that between 2004 and 2013 cases began to increase once more among homosexuals and to decrease among heterosexuals in Brazil as a whole. This fact was also found in a study conducted by Kundro et al.5 in a Buenos Aires hospital between 2002 and 2014.5
Average age was 37.3 years and infection was predominant in adults aged 20-59 years. A similar average was found by Silva et al.23 in a study conducted in a city in Goiás state, and also by Silva et al.22 in a study conducted in Rio Grande do Norte state.
Individuals of white and brown skin color/race and who had elementary schooling were predominant in this study. A study conducted with elderly people with AIDS in municipalities in the Belo Horizonte health macro-region covering the period 1986-2010 and using Sinan data, also found relevant percentages of white skin color/race (26.2%), followed by brown (19.5%).24 Another study conducted in Rio Grande do Norte state found higher AIDS prevalence among individuals of brown skin color and with low schooling.22 Skin color/race and schooling are social determinants of health. Historically, individuals of brown skin color and with low schooling have had less access to health services and education, which is directly related to information regarding disease transmission routes and prevention methods.25,26
In the state of Minas Gerais, 1.5% of cases were pregnant women, and, between 2007 and 2016, there was a 240% increase in cases. According to the Minas Gerais Epidemiological Bulletin,8 1,977 cases of pregnant women were notified between 2010 and 2015 and a slight decrease in cases was seen during the period. This diverges from the findings of our study. It should be highlighted that many women discover they have HIV when having antenatal examinations during pregnancy; hence the importance of early diagnosis and health workers trained to provide support to these women. It should be noted that there is a specific HIV notification form for pregnant women and this generates a separate database on Sinan.
Gender inequalities interfere in the HIV/AIDS epidemic and are also expressed in the dynamics of health service practices, which separate provision of contraceptives from HIV prevention, leading to shortcomings in counseling before and after serological testing. Women’s lack of sexual autonomy reveals itself in the dynamics of interpersonal relationships and in health service practices, whereby these services are not always trained to provide means by which women can enjoy their sexuality while minimizing risks.27,28
As injecting drug use has decreased, a gradual reduction in this HIV transmission route is expected. However, among blood-borne transmission, transmission due to drug use (3.4%) was most frequent. This was also found by a study in Buenos Aires for the period 2002-2014 (2.0%).5 A cohort study of PLWHA in Aids between 2003 and 2012, found greater probability of late diagnosis among drug users, among males and among heterosexuals.29
The most common conditions diagnosed at the time of AIDS notification were CD4+ T count <350cells/mm3, candidiasis, pneumonia, cerebral toxoplasmosis and herpes as per the Adapted CDC criterion, and cachexia, asthenia, anemia/lymphopenia/thrombocytopenia, candidiasis, fever, diarrhea and persistent dermatitis as per the Rio de Janeiro/Caracas criterion. Their proportions were lower than those found in a study conducted in city in Goiás state, in which 58.9% had an opportunistic infection, whereby candidiasis (20.4%), syphilis (15.1%) and herpes zoster (14.1%) were the most frequent.23 A study conducted in Nigeria for the period 2005-2010, found higher prevalence of diseases and conditions in advanced stages of AIDS, especially among males.30
The limitations of this study include: use of a secondary database with information limited to the notification form; the short period analyzed to obtain the temporal trend owing to Sinan not being available for tabulation in the period prior to 2007; and the period of just three years following the state of obligatory HIV notification.
In conclusion, there was an increase in the AIDS incidence rate and the HIV detection rate in all age ranges. This indicates that prevention strategies need to be rethought, given that the number of infected people continues to increase. Despite increased detection of people with HIV, there is still a large number of people who are not aware of their serological status and could be benefited by ART and consequent very low viral loads, thus contributing to reducing HIV transmission among the population. As such, educational campaigns on HIV transmission routes and prevention methods need to be reviewed and need to include aspects related to treatment and antiretroviral therapy, as well as emphasizing condom use.
On the other hand, the stationary trend of AIDS mortality suggests that availability of ART can favor the reduction of AIDS deaths. Notwithstanding, medicalization of prevention needs to be better evaluated in the long term as to cost-benefit and effectiveness. The average profile with regard to age, sex, transmission route and exposure category is within the national average, thus facilitating focus on health care and prevention.
Acknowledgements
We thank the Riberao Preto Medical School, University of Sao Paulo - Community Health Postgraduate Program, for providing a postdoctoral position and for the opportunity to conduct this study.
REFERENCES
1. Lazzarotto AR, Deresz LF, Sprinz E. HIV/Aids e treinamento concorrente: a revisão sistemática. Rev Bras Med Esporte [Internet]. 2010 mar-abr [citado 2020 jan 8];16(2):149-54. Disponível em: Disponível em: http://www.scielo.br/pdf/rbme/v16n2/15.pdf . doi: 10.1590/S1517-86922010000200015 [ Links ]
2. Dourado I, Veras MASM, Barreira D, Brito AM. Tendências da epidemia de Aids no Brasil após a terapia anti-retroviral. Rev Saúde Pública [Internet]. 2006 abr [citado 2020 jan 8];40 Supl 1:9-17. Disponível em: Disponível em: http://www.scielo.br/pdf/rsp/v40s0/03.pdf . doi: 10.1590/S0034-89102006000800003 [ Links ]
3. Hallal R, Ravasi G, Kuchenbecker R, Greco D, Simão M. O acesso universal ao tratamento antirretroviral no Brasil. Actas de Saúde Colet [Internet]. 2010 [citado 2020 jan 8];4(2):53-65. Disponível em: Disponível em: http://tempus.unb.br/index.php/tempus/article/viewFile/791/778 [ Links ]
4. Polejack L, Seidl EMF. Monitoring and evaluation of adherence to ARV treatment for HIV/aids: challenges and possibilities. Ciênc Saude Coletiva [Internet]. 2010 Jun [cited 2020 Jan 8];15(Supl 1):1201-08. Available from: Available from: http://www.scielo.br/pdf/csc/v15s1/029.pdf . doi: 10.1590/S1413-81232010000700029 [ Links ]
5. Kundro MA, Terwel SR, Toibaro JJ, Viloria GA, Losso MH. Late diagnosis of HIV infection in asymptomatic patients. Medicina (B Aires) [Internet]. 2016 [cited 2020 Jan 8];76(5):273-8. Available from: Available from: http://www.medicinabuenosaires.com/PMID/27723614.pdf [ Links ]
6. Sidibé M. Charting a path to end the AIDS epidemic. Bull World Health Organ [Internet]. 2016 Jun [cited 2020 Jan 8];94(6):408. Available from: Available from: https://www.who.int/bulletin/volumes/94/6/16-176875/en/ . doi: 10.2471/BLT.16.176875 [ Links ]
7. Brasil. Ministério da Saúde. Portaria MS/GM nº 1.271, de 06 de junho de 2014. Define a Lista Nacional de Notificação Compulsória de doenças, agravos e eventos de saúde pública nos serviços de saúde públicos e privados em todo o território nacional, nos termos do anexo, e dá outras providências [Internet]. Diário Oficial da União, Brasília (DF), 9 junho 2014 [citado 2020 jan 8];Seção I:67. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2014/prt1271_06_06_2014.html [ Links ]
8. Secretaria de Estado de Saúde (MG). Subsecretaria de Vigilância e Proteção à Saúde. Boletim epidemiológico mineiro: sífilis - análise epidemiológica de HIV/AIDS panorama do ano de 2015 [Internet]. Belo Horizonte: Secretaria do Estado da Saúde; 2016 [citado 2020 jan 8]. 41 p. Disponível em: Disponível em: https://ammg.org.br/wp-content/uploads/BEM-SÍFILIS-PDF.pdf [ Links ]
9. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de DST, Aids e hepatites virais. Aids e IST. Bol Epidemiol [Internet]. 2017 [citado 2020 jan 8]; 5(1):3-60. Disponível em: Disponível em: http://www.aids.gov.br/pt-br/pub/2017/boletim-epidemiologico-hivaids-2017 [ Links ]
10. Pereira BM, Silva NM, Moura LRP, Brito CMS, Câmara JT. Estudo epidemiológico de pacientes com infecção pelo Vírus da imunodeficiência humana/Síndrome da imunodeficiência adquirida (HIV/Aids), Caxias-MA. R Interd [Internet]. 2016 out-dez [citado 2020 jan 8];9(4):132-41. Disponível em: Disponível em: https://dialnet.unirioja.es/servlet/articulo?codigo=6771942 [ Links ]
11. Silva AP, Ferreira MAM, Braga MJ, Abrantes LA. Eficiência na alocação de recursos públicos destinados à educação, saúde e habitação em municípios mineiros. Contabilidade, Gestão e Governança [Internet]. 2012 abr [citado 2020 jan 8];15(1):96-114. Disponível em: Disponível em: http://cgg-amg.unb.br/index.php/contabil/article/viewFile/389/pdf [ Links ]
12. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Coordenação-Geral de Desenvolvimento da Epidemiologia em Serviços. Guia de vigilância em saúde [Internet]. 3. ed. Brasília: Ministério da Saúde; 2019 [citado 2020 jan 8]. 740 p. Disponível em: Disponível em: http://portalarquivos2.saude.gov.br/images/pdf/2019/junho/25/guia-vigilancia-saude-volume-unico-3ed.pdf [ Links ]
13. Antunes JLF, Cardoso MRA. Uso da análise de séries temporais em estudos epidemiológicos. Epidemiol Serv Saúde [Internet]. 2015 jul-set [citado 2020 jan 8];24(3):565-76. Disponível em: Disponível em: http://www.scielo.br/pdf/ress/v24n3/2237-9622-ress-24-03-00565.pdf . doi: 10.5123/S1679-49742015000300024 [ Links ]
14. Maksud I, Fernandes NM, Filgueiras SL. Tecnologias de prevenção do HIV e desafios para os serviços de saúde. Rev Bras Epidemiol [Internet]. 2015 set [citado 2020 jan 8];18 supl 1:104-19. Disponível em: Disponível em: http://www.scielo.br/pdf/rbepid/v18s1/pt_1415-790X-rbepid-18-s1-00104.pdf . doi: 10.1590/1809-4503201500050008 [ Links ]
15. Grangeiro A, Castanheira ER, Nemes MIB. A re-emergência da epidemia de aids no Brasil: desafios e perspectivas para o seu enfrentamento. Interface (Botucatu) [Internet]. 2015 jan-mar [citado 2020 jan 8];19(52):5-6. Disponível em: Disponível em: http://www.scielo.br/pdf/icse/v19n52/1807-5762-icse-19-52-0005.pdf . doi: 10.1590/1807-57622015.0038 [ Links ]
16. Greco DB. Trinta anos de enfrentamento à epidemia da Aids no Brasil,1985-2015. Ciên Saúde Coletiva [Internet]. 2016 maio [citado 2020 jan 8];21(5):1553-64. Disponível em: Disponível em: http://www.scielo.br/pdf/csc/v21n5/1413-8123-csc-21-05-1553.pdf . doi: 10.1590/1413-81232015215.04402016 [ Links ]
17. Nunes AA, Caliani LS, Nunes MS, Silva AS, Mello LM. Análise do perfil de pacientes com HIV/Aids hospitalizados após introdução da terapia antirretroviral (HAART). Ciên Saúde Coletiva [Internet]. 2015 out [citado 2020 jan 8];20(10):3191-8. Disponível em: Disponível em: http://www.scielo.br/pdf/csc/v20n10/1413-8123-csc-20-10-3191.pdf . doi: 10.1590/1413-812320152010.03062015 [ Links ]
18. Melo MC, Pimenta AM. Característica epidemiológica da AIDS na população com mais de 50 anos em Betim e Microrregião. R Enferm Cent O Min [Internet]. 2012 set-dez [citado 2020 jan 8];2(3):419-42. Disponível em: Disponível em: http://seer.ufsj.edu.br/index.php/recom/article/view/269 . doi: 10.19175/recom.v0i0.269 [ Links ]
19. Martins TA, Kerr LRFS, Kendall C, Mota RMS. Cenário epidemiológico da infecção pelo HIV e AIDS no mundo. Rev Fisioter S Fun [Internet]. 2014 jan-jun [citado 2020 jan 8];3(1):4-7. Disponível em: Disponível em: https://pdfs.semanticscholar.org/3e26/c1e4937b0fcae0ac2e650103b28a21e48ae6.pdf [ Links ]
20. Silva RAR, Torres GV, Dantas SC, Nelson ARC, Duarte FHS, Costa DARS. Health care for people with HIV: evaluation of users. J Res.: Fundam Care [Internet]. 2017 jan-mar [citado 2020 jan 8];9(1):21-7. Disponível em: Disponível em: https://www.redalyc.org/pdf/5057/505754108004_5.pdf . doi: 10.9789/2175-5361.2017.v9i1.21-27 [ Links ]
21. Santos NJ, Barbosa MR, Pinho RM, Villela WV, Aidar T, Filipe EMV. Contextos de vulnerabilidade para o HIV entre mulheres brasileiras. Cad Saúde Pública [Internet]. 2009 [citado 2020 jan 8]; 25 Sup2:S321-33. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v25s2/14.pdf . doi: 10.1590/S0102-311X2009001400014 [ Links ]
22. Silva LTS, Silva D, Salvetti MG, Torres GV, Silva RA, Souza NL. Perfil dos casos de síndrome da imunodeficiência adquirida em um Estado do nordeste do Brasil. Rev Enferm UFSM [Internet]. 2014 out-dez [citado 2020 jan 8];4(4):727-38. Disponível em: Disponível em: https://periodicos.ufsm.br/reufsm/article/view/15207 . doi: 10.5902/2179769215207 [ Links ]
23. Silva CTX, Arruda JT, Silva DLB, Souza GP. Perfil clínico epidemiológico dos pacientes com AIDS atendidos no serviço de assistência especializada em Anápolis-GO nos anos de 2009 a 2013. Rev Educ Saúde [Internet]. 2016 jun [citado 2020 jan 8];4(1):16-25. Disponível em: Disponível em: http://periodicos.unievangelica.edu.br/index.php/educacaoemsaude/article/view/1691 [ Links ]
24. Melo MC, Pimenta AM, Donalísio MR. Perfil epidemiológico de idosos com Aids na macrorregião de saúde de Belo Horizonte. R Enferm Cent O Min [Internet]. 2016 jan-abr [citado 2020 jan 8];1(6):2020-33. Disponível em: Disponível em: http://www.seer.ufsj.edu.br/index.php/recom/article/view/330 . doi: 10.19175/recom.v6i2.330 [ Links ]
25. Galvão JMV, Costa ACM, Galvão JV. Demographic and socio-demographic profile of people living with HIV/AIDS. Rev Enferm UFPI [Internet]. 2017 Jan-Apr [cited 2020 Jan 8];6(1):4-8. Available from: Available from: https://revistas.ufpi.br/index.php/reufpi/article/view/5533/0 . doi: 10.26694/reufpi.v6i1.5533 [ Links ]
26. Instituto Brasileiro de Geografia e Estatística, Coordenação de População e Indicadores Sociais. Síntese de indicadores sociais: uma análise das condições de vida da população brasileira: 2016 [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2016. 146 p. Disponível em: https://biblioteca.ibge.gov.br/visualizacao/livros/liv98965.pdf [ Links ]
27. Villela WV, Monteiro S. Gênero, estigma e saúde: reflexões a partir da prostituição, do aborto e do HIV/aids entre mulheres. Epidemiol Serv Saúde [Internet]. 2015 jul-set [citado 2020 jan 8];24(3):531-40. Disponível em: Disponível em: http://www.scielo.br/pdf/ress/v24n3/2237-9622-ress-24-03-00531.pdf . doi: 10.5123/S1679-49742015000300019 [ Links ]
28. Pascom ARP, Szwarcwald CL. Sex inequalities in HIV-related practices in the Brazilian population aged 15 to 64 years old, 2008. Cad Saúde Pública [Internet]. 2011 [cited 2020 Jan 8];27 Suppl 1:27-35. Available from: Available from: http://www.scielo.br/pdf/csp/v27s1/04.pdf . doi: 10.1590/S0102-311X2011001300004 [ Links ]
29. Jeong SJ, Italiano C, Chaiwarith R, Ng O, Vanar S, Jiamsakul A, et al. Late presentation into Care of HIV disease and its associated factors in Asia: results of TAHOD. AIDS Res Hum Retroviruses [Internet]. 2016 Mar [cited 2020 Jan 8];32(3): 255-61. Available from: Available from: https://www.liebertpub.com/doi/full/10.1089/AID.2015.0058?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . doi: 10.1089/AID.2015.0058 [ Links ]
30. Agaba PA, Meloni ST, Sule HM, Agbaji OO, Ekeh PN, Job GC, et al. Patients who presente late to HIV care and associated risk factors in Nigeria. HIV Med [Internet]. 2014 Aug [cited 2020 Jan 8];15(7):396-405. Available from: Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/hiv.12125 . doi: 10.1111/hiv.12125 [ Links ]
Received: November 21, 2018; Accepted: November 12, 2019











 texto en
texto en 


