Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.2 Brasília 2020 Epub 16-Abr-2020
http://dx.doi.org/10.5123/s1679-49742020000200006
ORIGINAL ARTICLE
Adolescent intentional self-harm notifications and hospitalizations in Brazil, 2007-2016
1Fundação Oswaldo Cruz, Escola Nacional de Saúde Pública Sergio Arouca, Rio de Janeiro, RJ, Brazil
Objective:
to describe the profile of case notifications and hospitalizations of intentional self-harm involving adolescents in Brazil.
Methods:
this was a descriptive study with data from the Notifiable Health Conditions Information System (SINAN) (2011-2014) and the Brazilian National Health System Hospital Information System (SIH/SUS) (2007-2016) about intentional self-harm.
Results:
there were 15,702 notifications, with predominance of the 15-19 years age group (76.4%), females (71.6%) and White race/skin color (58.3%); the home was the most frequent place of occurrence (88.5% among those 10-14 years old and 89.9% among those 15-19 years old); poisoning/intoxication was the most used method (76.6% and 78% in the 10-14 and 15-19 age groups, respectively); there were 12,060 hospitalizations, with a predominance of females (58.1%) and greater occurrence in Southeast Region (2.7 and 7.0 notifications/100,000 inhabitants in the 10-14 and 15-19 age groups, respectively).
Conclusion:
the results reinforce the need for health services to be sensitive to recording cases and providing care to these adolescents.
Keywords: Suicide, Attempted; Adolescent; Information Systems; Hospitalization; Epidemiology, Descriptive
Introduction
Intentional self-harm is defined as violence that a person inflicts on him or herself and can be classified as suicidal behavior or self-injury. Suicidal behavior is characterized by the fact of a person causing injury to him or herself, regardless of the degree of lethal intention or the real motive for the act. It includes thoughts, planning, attempts to kill oneself and suicide itself.1 In turn, self-injury encompasses self-mutilation, ranging from less severe forms such as scratches, cuts and bites, to more severe forms, such as limb amputation.2),(3 Sex, age, culture and ethnic group have important implications for the epidemiology of suicide, and several risk factors are known to be associated with distinct causes which interact between each other, such as medical, biological, environmental, psychiatric, psychological, philosophical/existential problems, as well as social motivations and problems.4
Transition from childhood to adolescence represents a critical period for vulnerability to suicidal behavior.5 In adolescence, certain particularities proper to this age increase risk of intentional self-harm, such as (i) profound biopsychosocial transformations, (ii) behavior that is naturally more impulsive and depressive, (iii) increased mental disorders, (iv) greater susceptibility to alcohol and drug consumption, (v) loneliness, (vi) questioning about social problems, meaning of life and belonging to the world, (vii) increased family conflicts, mostly arising from the quest for autonomy, (viii) crises or break-ups with boy/girlfriends or friends and (ix) temerity in social and sexual contacts.3),(6)-(9
All of this context of vulnerability places intentional self-harm as a serious Public Health problem, and adolescence as a period of life when this problem is a leading cause of death.3),(10 In 2012, suicide was in third place among causes of adolescent deaths worldwide, after traffic accidents and respiratory infections.11 Notwithstanding, difficulties exist in obtaining statistics about suicide attempts, due to several factors: sociocultural, moral, religious and economic issues; unclear diagnosis; and difficulty in obtaining knowledge about the circumstances of these occurrences, given that many of these attempts are of low severity and are dealt with at home.12
In Brazil, two health information systems have been used to obtain knowledge about the dimension of suicide attempts. One is the Brazilian National Health System Hospital Information System (SIH/SUS), responsible for recording hospital morbidity data and supplying data on procedures performed during hospitalizations in public hospitals and SUS outsourced hospitals;13 the other is the continuous component of the Violence and Accidents Surveillance System (VIVA), the database of which is fed by the Individual Notification Form for interpersonal/self-inflicted violence held on the Notifiable Health Conditions Information System (SINAN). This form is filled out in all cases of suspected or confirmed violence receiving care in health services.14),(15
Suicide attempts are an important element of the study of intentional self-harm committed by adolescents, given that they are an important predictor of self-inflicted death. The number of suicide attempts surpasses the number of successful suicides: it is estimated that for each successful suicide in the general population, there are at least 20 suicide attempts among young people.16)-(19 However, it is estimated that between 67% and 75% of such attempts are of low lethality, as mentioned above: only one third of adolescents who suffer this type of harm receive care in emergency health services for injuries resulting from their acts.20)-(21
In Brazil, hospitalization rates due to suicide attempts are higher among female adolescents (three female hospitalizations per one male hospitalization), as well as among older adolescents and adolescents in municipalities with more than one million inhabitants. The preferred means used in suicide attempts among female adolescents is substance intoxication, especially analgesics. Among males, the use of sharp objects and fire arms is more prevalent.22 Between 2000 and 2009, 15.1% of suicide attempt hospitalizations involved adolescents and, in 2014, 22.8% of suicide attempts notified on the SINAN system corresponded to individuals in this stage of life.23
Epidemiological studies are important. Having knowledge of the profile of suicide attempts enables not only which adolescents are at greater risk to be identified, but also informs decisions aimed at suicide prevention and actions for healthcare in this area.12
Within this context, the objective of this article was to describe suicide involving adolescents in Brazil in relation to two of its aspects: (i) notifications made between 2011 and 2014 and (ii) hospitalizations due to intentional self-harm from 2007 to 2016.
Methods
This was a descriptive study about case notifications and hospitalizations arising from intentional self-harm occurring in adolescence (10-19 years) in Brazil.
The following health information systems were used as the sources of information:
Violence and Accidents Surveillance System/Notifiable Health Conditions Information System - VIVA/SINAN. Notifications selected for analysis were taken from those SINAN Individual Notification Forms which had ‘yes’ as the answer to the ‘intentional self-harm’ item, and when the answer to the ‘perpetrator’ item was ‘the person themself’. The period 2011-2014 was selected because notification of interpersonal/self-inflicted violence was only included on the list of compulsorily notifiable events in 2011, and also because the data for the year 2014 were the most recent available on the website of the Brazilian National Health System Information Technology Department (DATASUS) at the time of analysis.
Brazilian National Health System Hospital Information System - SIH/SUS. Hospitalizations were selected for the years 2007-2016 having ‘intentional self-harm’ as the main diagnosis, as per codes X60 to X84 of the International Statistical Classification of Diseases and Related Health Problems - 10th Revision (ICD-10). All the data were aggregated and analyzed according to sex and two age ranges - 10-14 and 15-19 years.
Frequency measurements for the following variables were measured in order to analyze notifications recorded on VIVA/SINAN:
race/skin color (white; black/brown; indigenous; yellow);
disability (yes; no);
zone of residence (rural/peri-urban; urban);
place of occurrence (residence; collective dwelling; school; public thoroughfare; and other [sports facility, bar or similar; commerce or service facility; industry; building site]);
means used (hanging; blunt object; sharp object; hot substance; poisoning/intoxication; firearm);
previous occurrence (yes; no);
alcohol (yes; no); and
action taken and service used (health services; social services; education services; Child and Adolescent Protection Council; Special Child and Adolescent Protection Police Station; Child and Youth Justice Service; other [Women’s Care Service; Public Prosecution Service; Human Rights Reference Center]).
With the purpose of verifying associations between the variables mentioned above and the outcome - notifications of intentional self-harm -, Pearson’s chi square test with a 5% significance level was used. The means used to inflict harm were also described, according to Federative Unit (UF).
Notification and hospitalization rates were calculated (per 100,000 inhabitants) by national macro-region and UF, for the periods studied. For this calculation, the numerator was the number of intentional self-harm notifications or hospitalizations, while the denominator was comprised of the adolescent population estimates provided by the
Brazilian Institute of Geography and Statistics, for each year under consideration. Excel and Stata 14.0 were used to build the database and to calculate the rates.
The study project did not require assessment by a Research Ethics Committee because it used secondary data with no patient identification, available for public consultation on the DATASUS website (www.datasus.gov.br)
Results
Between 2011 and 2014, health services notified 67.388 cases of intentional self-harm, accounting for 14% of all recorded violence. A total of 15,702 (23.3%) of these notifications referred to adolescents, 3,699 (23.6%) of whom were 10-14 years old, while 12,003 (76.4%) were 15-19 years old. Females were predominant in both these age groups: 2,952 (79.8%) in the 10-14 age group and 8,594 (71.6%) in the 15-19 age group.
Table 1 shows that the adolescents’ race/skin color was significantly associated with intentional self-harm in both age groups and also according to sex (p=0.004 and p<0.001, respectively). Adolescents of White race/skin color aged 10-14 years accounted for 59.2% of the total. The differences repeated themselves in the 15-19 age group (58.7% females versus 57.3% males). In turn, among indigenous adolescents and those of yellow race/skin color in both age groups, males stood out in suicide attempt occurrences. Significant association was also found between disability and suicide attempts, with greater frequency among males, in both age groups (p<0.001). Living in an urban area was also found to be associated with suicide attempts among 15-19 year-old adolescents (p=0.001).
Table 1 - Distribution of notifications of intentional self-harm involving adolescents, by age and sex, according to sociodemographic characteristics, circumstances of the act and action taken, Brazil, 2011-2014
| Characteristics | Age (in years) and sex | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10-14 | 15-19 | |||||||||||||
| Male (N=747) | Female (N=2,952) | Total (N=3,699) | p- valuea | Male (N=3,409) | Female (N=8,594) | Total (N=12,003) | p- valuea | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |||
| Race/skin color | 0.004 | <0.001 | ||||||||||||
| White | 355 | 56.7 | 1,483 | 59.2 | 1,838 | 58.7 | 1,683 | 57.3 | 4,238 | 58.7 | 5,921 | 58.3 | ||
| Black/brown | 251 | 40.1 | 991 | 39.6 | 1,242 | 39.7 | 1,181 | 40.2 | 2,873 | 39.8 | 4,054 | 39.9 | ||
| Indigenous | 11 | 1.8 | 15 | 0.6 | 26 | 0.8 | 54 | 1.8 | 56 | 0.8 | 110 | 1.1 | ||
| Yellow | 9 | 1.4 | 15 | 0.6 | 24 | 0.8 | 19 | 0.7 | 50 | 0.7 | 69 | 0.7 | ||
| Disability | 118 | 20.5 | 350 | 15.5 | 468 | 16.5 | 0.004 | 527 | 20.8 | 958 | 15.1 | 1,485 | 16.7 | <0.001 |
| Zone of residence | 0.217 | 0.001 | ||||||||||||
| Rural/peri-urban | 73 | 0.1 | 249 | 8.7 | 322 | 9.0 | 359 | 10.8 | 744 | 8.8 | 1,103 | 9.4 | ||
| Urban | 648 | 89.9 | 2,627 | 91.3 | 3,275 | 91.1 | 2,957 | 89.2 | 7,674 | 91.2 | 10,631 | 90.6 | ||
| Place of occurrence | <0.001 | <0.001 | ||||||||||||
| Residence | 554 | 78.9 | 2,525 | 91.0 | 3,079 | 88.5 | 2,542 | 82.0 | 7,397 | 93.0 | 9,939 | 89.9 | ||
| Collective dwelling | 8 | 1.1 | 26 | 0.9 | 34 | 1.0 | 29 | 0.9 | 30 | 0.4 | 59 | 0.5 | ||
| School | 25 | 3.6 | 82 | 3.0 | 107 | 3.1 | 30 | 1.0 | 70 | 0.9 | 100 | 0.9 | ||
| Public thoroughfare | 70 | 10.0 | 57 | 2.1 | 127 | 3.7 | 278 | 9.0 | 230 | 2.9 | 508 | 4.6 | ||
| Other | 45 | 6.4 | 86 | 3.1 | 131 | 3.8 | 221 | 7.1 | 224 | 2.8 | 445 | 4.0 | ||
| Means used | <0.001 | <0.001 | ||||||||||||
| Hanging | 73 | 15.6 | 65 | 3.2 | 138 | 5.6 | 358 | 14.6 | 201 | 3.4 | 559 | 6.7 | ||
| Blunt object | 7 | 1.5 | 23 | 1.1 | 30 | 1.2 | 30 | 1.2 | 41 | 0.7 | 71 | 0.8 | ||
| Sharp object | 56 | 12.0 | 268 | 13.3 | 324 | 13.1 | 339 | 13.8 | 622 | 10.4 | 961 | 11.4 | ||
| Hot substance | 15 | 3.2 | 39 | 1.9 | 54 | 2.2 | 46 | 1.9 | 95 | 1.6 | 141 | 1.7 | ||
| Poisoning/intoxication | 288 | 61.5 | 1,610 | 80.1 | 1,898 | 76.6 | 1,574 | 64.2 | 4,986 | 83.6 | 6,560 | 78.0 | ||
| Firearm | 29 | 6.2 | 6 | 0.3 | 35 | 1.4 | 103 | 4.2 | 17 | 0.3 | 120 | 1.4 | ||
| Previous occurrence | 132 | 24.6 | 656 | 29.1 | 788 | 28.2 | 0.041 | 695 | 28.1 | 1,906 | 30.1 | 2,601 | 29.6 | 0.057 |
| Alcohol | 88 | 16.5 | 163 | 7.9 | 251 | 9.7 | <0.001 | 562 | 24.7 | 637 | 11.1 | 1,199 | 15.0 | <0.001 |
| Referral service | 0.230 | 0.038 | ||||||||||||
| Health service | 331 | 65.9 | 1,490 | 71.4 | 1,821 | 70.4 | 1,499 | 80.5 | 4,437 | 83.5 | 5,936 | 82.7 | ||
| Social services | 24 | 4.8 | 76 | 3.6 | 100 | 3.9 | 101 | 5.4 | 225 | 4.2 | 326 | 4.5 | ||
| Education services | - | - | 1 | 0.1 | 1 | - | - | - | - | - | - | - | ||
| Child and Adolescent Protection Council | 145 | 28.9 | 513 | 24.6 | 658 | 25.4 | 258 | 13.9 | 636 | 12.0 | 894 | 12.5 | ||
| Special Child and Adolescent Protection Police Station | 2 | 0.4 | 5 | 0.2 | 7 | 0.3 | 3 | 0.2 | 6 | 0.1 | 9 | 0.1 | ||
| Child and Youth Justice Service | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Other | - | - | 1 | 0.1 | 1 | 0.0 | 2 | 0.1 | 8 | 0.2 | 10 | 0.1 | ||
a) Pearson’s chi-square test
Notes: The values of the ‘unknown’ and ‘missing’ categories were excluded from the analysis. For the 10-14 years age group, these accounted for the following values, by variable: race/skin color (n=569), disability (n=868), zone of residence (n=102), place of occurrence (n=221), previous occurrence (n=905) and alcohol (n=1104). While for the 15-19 years age group they accounted for the following values: race/skin color (n=1849), disability (n=3117), zone of residence (n=269), place of occurrence (n=952), previous occurrence (n=3201) and alcohol (n=3981).
The ‘Means used’ and ‘Action taken’ do not add up to the total value, given that more than one option can be ticked for each of them on the Individual Notification Form for interpersonal/self-inflicted violence on the Notifiable Health Conditions Information System (SINAN), which was the data source used in the study.
Residence (home) was the main place where adolescents attempted suicide, principally females, whereby among the 10-14 age group the suicide attempt rate at home was 91.0%, while among males in the same age range it was 78.9%. In the 15-19 age range this proportion was 93.0% for females and 82.0% for males (p<0.001) (Table 1).
Poisoning/intoxication stood out as the means most used in suicide attempts, regardless of age or sex. Sharp objects were the second most frequent means used in suicide attempts among females aged 10-14 (13.3%), while for males in both age groups the second most frequent means used was hanging, following by sharp objects, firearms and hot substances (p<0.001) (Table 1). Regardless of age range, poisoning and intoxicating were the main means used in suicide attempts in almost all the Brazilian states: as the exceptions were adolescents aged 10-14 in Acre state and both age groups in Amazonas state where hanging was the main means used.
Table 1 also shows a considerable number of repeated suicide attempts (approximately 30% in each age range), more so among females. Association with use of alcohol in suicide attempts was more evident among males (p<0.001). Health services were the main destination of adolescents who attempted suicide, followed by Child and Adolescent Protection Councils (Table 1).
The Southern region stands out with regard to notification numbers and rates, regardless of age or sex: in the 10-14 age group, the rate varied between 17.6 cases (females) and 4.4 cases (males) per 100,000 inhab., increasing to 44.1 cases (females) and 18.4 cases (males) per 100,000 inhab. in the 15-19 age range. The Southern region was followed by the Southeast, Midwest, Northeast and Northern region with regard to the notification rate (Table 2).
Table 2 - Distribution of notification rates (per 100,000 inhab.) of intentional self-harm involving adolescents, by age and sex, by region and Federative Unit (UF) of occurrence, Brazil, 2011-2014
| Region and UF | Age (in years) and sex | |||||
|---|---|---|---|---|---|---|
| 10-14 | 15-19 | |||||
| Male (N=747) | Female (N=2,952) | Total (N=3,699) | Male (N=3,409) | Female (N=8,594) | Total (N=12,003) | |
| Rate | Rate | Rate | Rate | Rate | Rate | |
| North | 0.9 | 2.5 | 1.7 | 4.4 | 10.8 | 7.5 |
| Rondônia | 0.9 | 1.3 | 1.1 | 1.2 | 2.5 | 1.8 |
| Acre | 1.1 | 5.9 | 3.5 | 0.6 | 8.8 | 4.7 |
| Amazonas | 1.1 | 0.2 | 0.7 | 4.3 | 3.5 | 3.9 |
| Roraima | 0.9 | 13.1 | 6.9 | 30.5 | 65.4 | 47.6 |
| Pará | 0.3 | 0.3 | 0.3 | 0.1 | 1.4 | 0.8 |
| Amapá | 2.4 | 6.5 | 4.4 | 5.8 | 27.5 | 16.5 |
| Tocantins | 3.4 | 14.1 | 8.7 | 24.6 | 66.3 | 45.1 |
| Northeast | 0.9 | 3.9 | 2.4 | 4.7 | 12.8 | 8.7 |
| Maranhão | 0.4 | 0.4 | 0.4 | 1.8 | 2.4 | 2.1 |
| Piauí | 1.9 | 7.0 | 4.4 | 11.7 | 25.8 | 18.7 |
| Ceará | 0.4 | 1.3 | 0.8 | 1.3 | 4.0 | 2.6 |
| Rio Grande do Norte | 0.5 | 1.7 | 1.1 | 3.8 | 6.4 | 5.1 |
| Paraíba | 0.6 | 3.5 | 2.0 | 5.4 | 8.3 | 6.8 |
| Pernambuco | 1.2 | 6.4 | 3.8 | 7.1 | 18.5 | 12.7 |
| Alagoas | 5.4 | 26.6 | 15.9 | 24.2 | 90.7 | 57.4 |
| Sergipe | 0.2 | 0.5 | 0.4 | 1.2 | 1.5 | 1.4 |
| Bahia | 0.1 | 0.6 | 0.4 | 1.4 | 2.8 | 2.1 |
| Southeast | 2.6 | 11.2 | 6.8 | 11.5 | 32.2 | 21.7 |
| Minas Gerais | 3.4 | 17.2 | 10.2 | 17.6 | 55.4 | 36.1 |
| Espírito Santo | 2.5 | 11.3 | 6.8 | 6.0 | 22.8 | 14.2 |
| Rio de Janeiro | 1.4 | 4.2 | 2.8 | 4.7 | 10.0 | 7.3 |
| São Paulo | 1.2 | 10.8 | 6.6 | 11.7 | 30.2 | 20.8 |
| South | 4.4 | 17.6 | 10.9 | 18.4 | 44.1 | 31.0 |
| Paraná | 4.5 | 15.8 | 10.1 | 15.5 | 37.0 | 26.1 |
| Santa Catarina | 4.1 | 18.3 | 11.1 | 21.2 | 50.9 | 35.7 |
| Rio Grande do Sul | 4.6 | 19.2 | 11.7 | 19.7 | 47.3 | 33.2 |
| Midwest | 2.5 | 9.4 | 5.9 | 11.5 | 24.9 | 18.1 |
| Mato Grosso do Sul | 6.9 | 35.7 | 20.9 | 34.8 | 95.8 | 64.6 |
| Mato Grosso | 0.5 | 3.5 | 2.0 | 3.6 | 8.9 | 6.2 |
| Goiás | 2.1 | 4.1 | 3.1 | 9.1 | 12.1 | 10.6 |
| Distrito Federal | 1.4 | 4.1 | 2.7 | 4.5 | 8.1 | 6.4 |
Table 2 shows that Mato Grosso do Sul was the state with the highest suicide attempt rate among adolescents taken to health services (20.9 and 64.6 notified cases/100,000 inhab., respectively in the 10-14 and 15-19 age group), followed by Alagoas, Roraima, Tocantins, Minas Gerais and Santa Catarina. In all the Brazilian states, with the exception of Amazonas, the highest rates of suicide attempts among adolescents notified by health services were found among females. While in Amazonas state, in both age groups, suicide attempt rates were higher among males, in the states of Pará and Maranhão, suicide attempt rates were the same in both sexes in the 10-14 age group.
There were 12,060 hospitalizations due to intentional self-harm between 2007 and 2016, 3,350 (27.8%) of which were among those 10-14 years old and 8,710 (72.2%) among 15-19 year-olds. In both age groups, the majority were female adolescents, accounting for 1,947 (58.1%) hospitalizations in the younger age group and 4,435 (50.9%) in the older age group (data not presented).
Figure 1 shows the time series of suicide attempt hospitalization rates by sex, for each age group studied. In the 10-14 age group, a slight increase in the rates was found up to 2008. After 2008 a falling trend was found in males until 2010, followed by stability in both sexes. Between 2014 and 2015, the rates increased again, especially among males (2.5 and 2.4 hospitalizations/100,000 inhab.), falling once more until 2016. Among female adolescents, the rates were found to be more stable throughout the period, with a slight increase in 2013 and 2015.
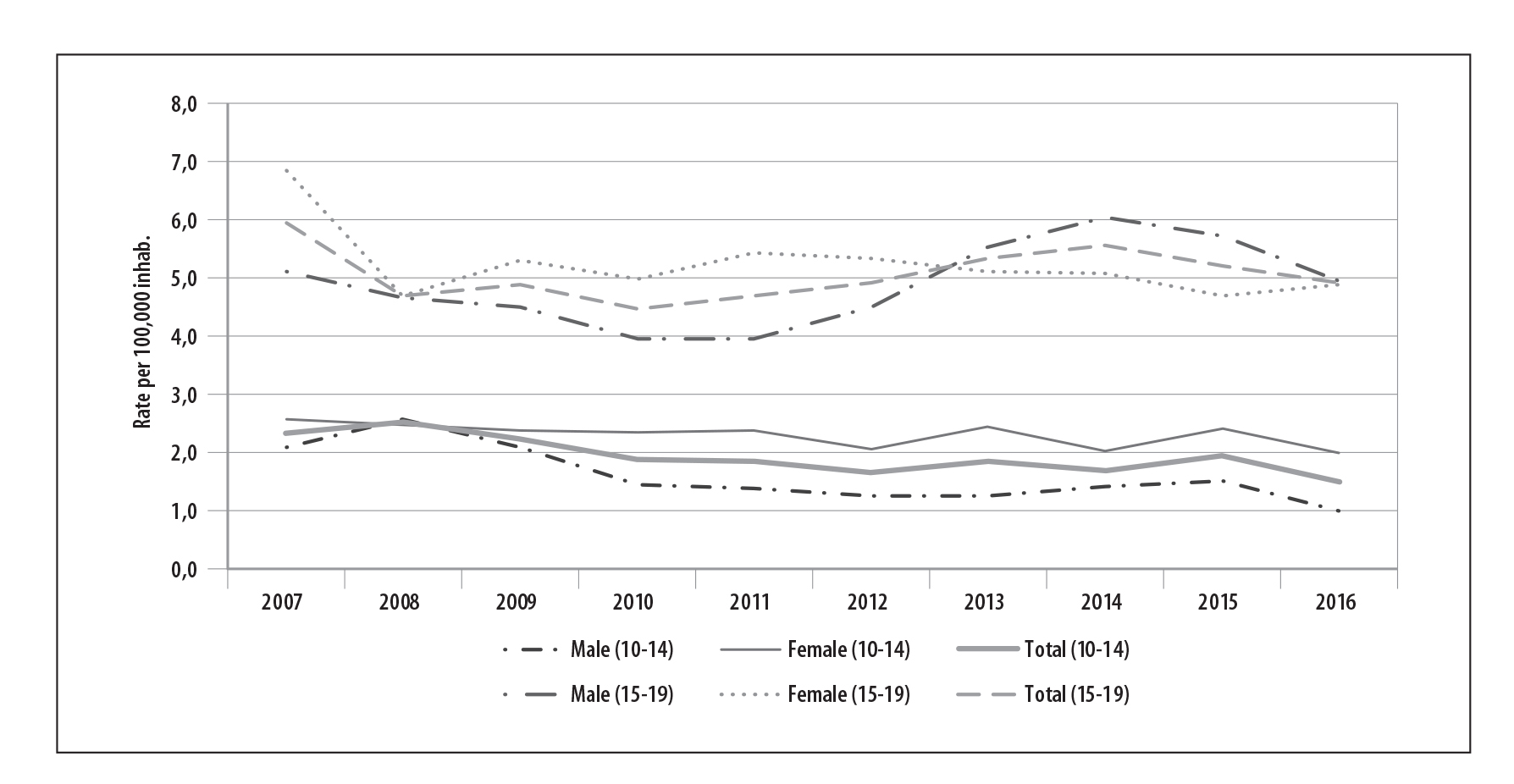
Figure 1 - Temporal distribution of hospitalization rates due to intentional self-harm involving adolescents, by age and sex, Brazil, 2007-2016
Distinct behavior was found in adolescents in the 15-19 age group. Rates were higher in this age range than in the 10-14 age group. With effect from 2007, rates were higher among females than among males. With effect from 2012, this relationship became the opposite, with males having a rate of 5.0 hospitalizations/100,000 inhab. in 2012, increasing 6.0/100,000 inhab. in 2014, while the rate reduced among females, above all with effect from 2011.
Table 3 shows that the Southeast region led the suicide attempt hospitalization rates in both sexes, followed by the North, South and Midwest regions, while rates were lowest in the Northeast region. Taking the analysis on an overall basis, it can be seen that there were more male hospitalizations than female hospitalizations in the majority of the states in the 15-19 age group. The states of Pará and Paraíba stood out in relation to hospitalization rates among 10-14 year-old adolescents who attempted suicide, while young people aged 15-19 stood out in the states of Acre and Ceará. The states of Alagoas and Sergipe had the lowest suicide attempt hospitalization rates in Brazil in the 10-14 age group, while the country’s lowest rate in the 15-19 age group was found in the state of Rio Grande do Norte.
Table 3 - Distribution of hospitalization rates (per 100,000 inhab.) due to intentional self-harm involving adolescents, by age and sex, by region and Federative Unit (UF), Brazil, 2017-2016
| Region and UF | Age (in years) and sex | |||||
|---|---|---|---|---|---|---|
| 10-14 | 15-19 | |||||
| Male (N=1,403) | Female (N=1,947) | Total (N=3,350) | Male (N=4,275) | Female (N=4,435) | Total (N=8,710) | |
| North | 3.1 | 1.9 | 2.5 | 5.0 | 3.3 | 4.2 |
| Rondônia | 1.2 | 1.9 | 1.5 | 5.0 | 4.7 | 4.8 |
| Acre | 3.0 | 2.4 | 2.7 | 20.7 | 6.5 | 13.6 |
| Amazonas | 0.5 | 0.4 | 0.4 | 1.3 | 0.8 | 1.0 |
| Roraima | 0.4 | 0.8 | 0.6 | 1.6 | 0.4 | 1.0 |
| Pará | 5.4 | 2.9 | 4.2 | 6.4 | 4.6 | 5.5 |
| Amapá | 0.5 | 1.2 | 0.9 | 0.8 | 3.0 | 1.9 |
| Tocantins | 2.2 | 1.4 | 1.8 | 1.8 | 1.2 | 1.5 |
| Northeast | 1.2 | 1.1 | 1.2 | 4.4 | 2.9 | 3.7 |
| Maranhão | 0.6 | 0.7 | 0.6 | 3.2 | 1.5 | 2.4 |
| Piauí | 0.8 | 0.9 | 0.9 | 1.3 | 3.2 | 2.2 |
| Ceará | 2.1 | 2.2 | 2.1 | 14.7 | 7.1 | 11.0 |
| Rio Grande do Norte | 0.5 | 0.2 | 0.4 | 1.1 | 0.6 | 0.9 |
| Paraíba | 6.4 | 1.3 | 3.9 | 6.6 | 2.0 | 4.3 |
| Pernambuco | 0.4 | 0.4 | 0.4 | 1.2 | 1.1 | 1.1 |
| Alagoas | 0.3 | 0.4 | 0.3 | 1.2 | 0.8 | 1.0 |
| Sergipe | 0.2 | 0.5 | 0.3 | 4.9 | 1.1 | 3.0 |
| Bahia | 1.0 | 1.5 | 1.2 | 2.2 | 3.5 | 2.8 |
| Southeast | 1.7 | 3.7 | 2.7 | 5.8 | 8.3 | 7.0 |
| Minas Gerais | 2.0 | 3.7 | 2.8 | 6.2 | 9.7 | 7.9 |
| Espírito Santo | 2.2 | 3.4 | 2.8 | 4.8 | 6.1 | 5.4 |
| Rio de Janeiro | 0.4 | 0.7 | 0.6 | 2.0 | 2.0 | 2.0 |
| São Paulo | 1.9 | 4.9 | 3.4 | 7.1 | 10.2 | 8.6 |
| South | 1.4 | 1.9 | 1.6 | 3.8 | 3.8 | 3.8 |
| Paraná | 1.6 | 2.3 | 2.0 | 4.4 | 5.2 | 4.8 |
| Santa Catarina | 1.6 | 2.5 | 2.0 | 4.2 | 3.9 | 4.1 |
| Rio Grande do Sul | 1.0 | 1.1 | 1.0 | 3.0 | 2.4 | 2.7 |
| Midwest | 1.3 | 1.5 | 1.4 | 3.9 | 3.8 | 3.8 |
| Mato Grosso do Sul | 1.1 | 0.8 | 1.0 | 4.2 | 3.3 | 3.7 |
| Mato Grosso | 1.3 | 1.8 | 1.6 | 4.0 | 2.0 | 3.1 |
| Goiás | 1.0 | 1.5 | 1.3 | 3.1 | 3.7 | 3.4 |
| Distrito Federal | 1.9 | 2.0 | 2.0 | 5.4 | 6.5 | 6.0 |
Discussion
This study provides a panorama of suicide attempts among adolescents receiving care for this reason in health services in Brazil in recent years. Even though underreporting is known to exist, there is a considerably high number of notifications and hospitalizations due to intentional self-harm. Notwithstanding the limitations of the data, the findings reinforce a profile already known in the literature: more cases among females; greater occurrence among older adolescents (15-19 years); the home as the main place where the act occurs; and vulnerability of health conditions as a risk factor, such as the presence of disabilities for instance.1),(3),(24
Standing out among the differences between the sexes is the choice of the less lethal method by females, this being a group in which reoccurrence tends to appear. Whereas among males abusive use of psychoactive substances and alcohol, as well as choice of methods that involve greater risk of self-inflicted death, are predominant.1),(24
With regard to age, Brent et al.25 explain that older adolescents are, from the point of view of cognition, more capable of planning and carrying out suicidal acts, demonstrating more elaborate intentions than younger adolescents, as well as having a higher level of autonomy and, therefore, receiving less parental supervision and support. This situation can increase the opportunity for their family and social disconnection, making recognition of imminent risk of putting an end to their own lives less likely.24
With regard to race/skin color, the discussions in the specialized literature are not very conclusive. Studies show that White individuals have, traditionally, higher rates of self-destructive behavior than non-White individuals.5),(18),(25
In relation to suicide attempt distribution and notification in Brazil, a combination of sociocultural, economic and psychobiological conditioning factors can be seen which may possibly explain the high rates found in the Southern region, affecting in particular farming families exposed to pesticides and to living in a more isolated manner. The predominantly German culture and consequent “immigration” of the suicide rate from the country of origin, low schooling, patriarchal tradition, greater incidence of mental disorders and generational history of suicide, which can be found in many families, are relevant questions for reflection on the subject.1 However, it is curious to note that the Southeast region is the leader regarding hospitalizations due to the cause studied here, which may be explained by greater use and effectiveness of emergency medical services provided in urban centers, in addition to questions related to the regional/local context, possible better described in specific analyses by region/location.12),(22
In the analysis of trends over time, attention is drawn to the slight decrease in hospitalizations due to suicide attempts between 2009 and 2013, as well as the higher number of older male adolescents in relation to their female peers between 2013 and 2016. Despite the national rate having increased up until 2012,3 a hypothesis regarding the decrease mentioned above is the increase in prevention actions, considerably levered by growing alerts made by the World Health Organization3 and greater awareness of the subject on the part of Education and Health teams. It is important to pay attention to the increase in male adolescent hospitalizations up until 2016, possibly indicating greater fragility of this group in a social and economic context which stimulates greater competition for opportunities, given the low perspective of work and future and, consequently, the tendency of their mental suffering and loss of meaning of life to increase. In this adverse scenario, in general adolescents may be more vulnerable in the face of this perspective. Some react to this situation with social isolation, stress and personal insecurity, which may contribute to increased pressure for social success, brought to bear by their families and by the competitive environment outside the home.18 Future studies, especially studies including analysis of these factors in current times, may advance with understanding on this matter.
Reflection about intentional self-harm that does not lead to death is strategic, in view of characteristics typical of adolescence: impulsiveness, identification problems, relationship conflicts and break-ups, as well as frequent angry frustration without the availability of assistance from an understanding adult. Having better knowledge about the group that attempts suicide is crucial when planning prevention; multidisciplinary care is also recommendable, for both adolescents and their families, in order to avoid the high reoccurrence (30%) that makes adolescents more vulnerable to successful suicide attempts.26
Approaching these attempts seriously, providing attention and care to adolescents and their families and considering the act of a suicide attempt as a warning sign of problems that may be coming to the surface are some of the main strategies for avoiding future suicide. Health services need to be prepared in this sense: both for providing emergency care and for ensuring continuity of adolescent support strategies, helping them to find meaning in life and to overcome their anguish.
Brent27 also makes certain recommendations for health professionals: (1) gain better understanding of suicidal behavior in younger age groups, in order to intervene earlier; (2) pay attention to use of social media and their impact on young people,28 recognizing not only their harmful potential but also the prevention potential of information and communication networks;29 (3) focus on the most recent attempts and their short-term effects, in cases in which toxic substance abuse stands out; and (4) combine biological knowledge about human beings and young people in particular, using theoretical, psychological and contextual models.
It is important to point out some limitations of this study, such as weaknesses of the notification and hospitalization statistics provided by the health information systems that were used. Firstly because cases cared for in health services are the most serious. In the general population it is estimated that only one in every three suicide attempts is attended to by emergency medical services. Social stigma surrounding suicidal behavior and fear of criminalization of the act are some of the reasons for not recording these episodes with health services. Secondly, data underreporting and case classification errors occur. In addition to all the weaknesses of the public health system, it must be recalled that available information on hospital records as used in this study, only relate to Brazilian National Health System services. Data about private emergency and hospital cases does not exist, even more so with regard to intentional self-harm.
The results presented by this study reinforce the need for health services to be sensitive to recording and providing care to adolescents who reach them because of this cause. The number of suicide attempts is high and reveals the dimension of the phenomenon. It is essential to fulfill the obligation to formulate and implement public policies targeting adolescence. Meeting the needs of these young people skillfully and with understanding when they reach health services, supporting them psychologically and providing follow-up is essential for improving their quality of life, especially those who undergo intense mental suffering and social isolation.
Referências
1. Botega NJ. Crise suicida: Avaliação e manejo. Porto Alegre: Artmed; 2015. [ Links ]
2. Organização Mundial da Saúde. Centro Colaborador da OMS para a Classificação de Doenças em Português. Classificação estatística internacional de doenças e problemas relacionados à saúde. 10. ed. Rev. Volume I. São Paulo: Editora da Universidade de São Paulo; 2009. [ Links ]
3. World Health Organization. Preventing suicide: a global imperative [Internet]. Geneva: World Health Organization; 2014 [cited 2020 Feb 13]. Available from: Available from: https://www.who.int/mental_health/suicide-prevention/world_report_2014/en/ [ Links ]
4. Minayo MC, Avanci JQ, Figueiredo AEB. Violência Autoinfligida: ideações, tentativas e suicídio consumado. In: Minayo MC, Assis SG (Org.). Novas e velhas faces da violência no século XXI: visão da literatura brasileira do campo da saúde. Rio de Janeiro: Editora Fiocruz; 2017. [ Links ]
5. Centers for Disease Control and Prevention, Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, et al. Youth risk behavior surveillance: United States, 2005. MMWR [Internet]. 2006 Jun [cited 2020 Feb 13];55(SS-5):1-108. Available from: Available from: https://www.cdc.gov/mmwr/PDF/SS/SS5505.pdf [ Links ]
6. Hedeland RL, Teilmann G, Jorgensen MH, Thiesen LR, Andersen J. Risk factors and characteristics of suicide attempts among 381 suicidal adolescents. Acta Paediatr [Internet]. 2016 May [cited 2020 Feb 13];105(10):1231-8. Available from: Available from: https://doi.org/10.1111/apa.13458 [ Links ]
7. Daniel SS, Goldston DB. Interventions for suicidal youth: a review of the literature and developmental considerations. Suicide Life Threat Behav [Internet]. 2009 Feb [cited 2020 Feb 13];39(3):252. Available from: Available from: http://10.1521/suli.2009.39.3.252 [ Links ]
8. Joffe RT, Offord DR, Boyle MH. Ontario child health study: suicidal behavior in youth age 12-16 years. Am J Psychiatry [Internet]. 1988 Nov [cited 2020 Feb 13];145(11):1420-3. Available from: Available from: https://doi.org/10.1176/ajp.145.11.1420 [ Links ]
9. World Health Organization. Preventing suicide: a resource for media professional [Internet]. Geneva: World Health Organization; 2017 [cited 2020 Feb 13]. 18 p. Available from: Available from: https://www.who.int/mental_health/prevention/suicide/resource_media.pdf [ Links ]
10. Evans E, Hawton K, Rodham K. Factors associated with suicidal phenomena in adolescents: a systematic review of population-based studies. Clin Psychol Rev [Internet]. 2004 Dec [cited 2020 Feb 13];24(8);957-79. Available from: Available from: https://doi.org/10.1016/j.cpr.2004.04.005 [ Links ]
11. World Health Organization. Global accelerated action for the health of adolescents (AA-HA!): guidance to support country implementation [Internet]. Geneva: World Health Organization; 2016 [cited 2020 Feb 13]. Available from: Available from: https://www.who.int/maternal_child_adolescent/topics/adolescence/framework-accelerated-action/en/ [ Links ]
12. Santos SA, Legay LF, Aguiar FP, Lovisi GM, Abelha L, Oliveira SP. Tentativas e suicídios por intoxicação exógena no Rio de Janeiro, Brasil: análise das informações através do linkage probabilístico. Cad Saúde Pública [Internet]. 2014 maio [citado 2020 fev 13];30(5):1057-66. Disponível em: Disponível em: https://doi.org/10.1590/0102-311X00054213 [ Links ]
13. Souza ER. Processos, sistemas e métodos de informa-ção em acidentes e violências no âmbito da Saúde Pú-blica. In: Minayo MCS, Deslandes SF (Org.). Caminhos do pensamento: epistemologia e método. Rio de Janeiro: Fiocruz; 2002. p. 255-73. [ Links ]
14. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise de Situação de Saúde. Viva: instrutivo de notificação de violência doméstica, sexual e outras violências [Internet]. Brasília: Ministério da Saúde; 2011 [citado 2020 Fev 13]. 72 p. Disponível em: Disponível em: http://www.crianca.mppr.mp.br/arquivos/File/sinan/viva_instrutivo_not_viol_domestica_sexual_e_out.pdf [ Links ]
15. Pinto LW, Assis SG. Estudo descritivo das tentativas de suicídio na população idosa brasileira, 2000-2014. Ciênc Saúde Coletiva [Internet]. 2015 jun [citado 2020 fev 13];20(6):1681-92. Disponível em: Disponível em: https://doi.org/10.1590/1413-81232015206.03532015 [ Links ]
16. World Health Organization. Mental health: suicide data [Internet]. Geneva: World Health Organization; 2016 [cited 2018 Sep 29]. Available from: Available from: http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/ [ Links ]
17. Miranda R, Scott M, Hicks R, Wilcox HC, Harris MJ, Shaffer D. Suicide attempt characteristics, diagnoses, and future attempts: comparing multiple attempters to single attempters and ideators. J Am Acad Child Adolesc Psychiatry [Internet]. 2008 Jan [cited 2020 Feb 13];47(1):32-40. Available from: Available from: https://doi.org/10.1097/chi.0b013e31815a56cb [ Links ]
18. Doshi A, Boudreaux ED, Wang N, Pelletier AJ, Camargo Jr CA. National study of US Emergency department visits for attempted suicide and self-inflicted injury, 1997-2001. Ann Emerg Med [Internet]. 2005 Oct [cited 2020 Feb 13];46(4):963-75. Available from: Available from: https://doi.org/10.1016/j.annemergmed.2005.04.018 [ Links ]
19. Ribeiro JD, Franklin JC, Fox KR, Bentley K, Kleiman EM, Chang B, Nock MK. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med [Internet]. 2016 Jan [cited 2020 Feb 13];46(2):225-36. Available from: Available from: https://doi.org/10.1017/S0033291715001804 [ Links ]
20. Kann L, Kinchen S, Shanklin SL, Flint KH, Kawkins J, Harris WA, et al. Youth risk behavior surveillance-United States, 2013. MMWR [Internet]. 2014 Jun [cited 2020 Feb 13];63(4):1-168. Available from: Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/ss6304a1.htm [ Links ]
21. Carlson GA, Abbott SF. Mood disorders and suicide. In: Caplan HI, Sadock BJ. Comprehensive textbook of psychiatry, vol 2, 6th ed. Baltimore: Williams & Wilkins; 1995. p. 2367-91. [ Links ]
22. Minayo MCS, Assis SG, Souza ER. Suicídios no Brasil por faixas etárias (2000-2008). Rio de Janeiro: Claves/Fiocruz; 2013. [ Links ]
23. Minayo MCS, Bahia CA, Avanci JQ. Suicídios consumados e tentativas notificadas no Brasil. In: Ministério da Saúde (Org.). Saúde Brasil 2014: uma análise da situação de saúde e das causas externas [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2020 fev 13]. v. 1, p. 325-41. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/saude_brasil_2014_analise_situacao.pdf [ Links ]
24. Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry [Internet]. 2006 Mar-Apr [cited 2020 Feb 13];47(3-4):372-94. Available from: Available from: https://doi.org/10.1111/j.1469-7610.2006.01615.x [ Links ]
25. Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry [Internet]. 1999 Dec [cited 2020 Feb 13];38(12):1497-505. Available from: Available from: https://doi.org/10.1097/00004583-199912000-00010 [ Links ]
26. Anderson LM, Lowry LS, Wuensch KL. Racial differences in adolescents’ answering questions about suicide. Death Stud [Internet]. 2015 Jun [cited 2020 Feb 13];39(10);600-4. Available from: Available from: https://doi.org/10.1080/07481187.2015.1047058 [ Links ]
27. Brent D. A time to reap and a time to sow: reducing the adolescent suicide rate now and in the future: commentary on Cha et al. J Child Psychol Psychiatry [Internet]. 2018 Apr [cited 2020 Feb 13];59(4);483-5. Available from: Available from: https://doi.org/10.1111/jcpp.12903 [ Links ]
28. Sgobin SMT, Travali ALM, Coelho OR, Botega NJ. Direct and indirect cost of suicide attempts in a general hospital: a cost of illness study. São Paulo Med J [Internet]. 2015 May-Jun [cited 2020 Feb 13];133(3):218-26. Available from: Available from: https://doi.org/10.1590/1516-3180.2014.8491808 [ Links ]
29. Hokby S, Hadlaczky G, Westerlund J, Wasserman D, Balazs J, Germanavicius A, Carli V. Are mental health effects of internet use attributable to the webbased content or perceived consequences of usage? A longitudinal study of European adolescents. JMIR Menl Health [Internet]. 2016 Jul [cited 2020 Feb 13];3(3):e31. Available from: Available from: https://mental.jmir.org/2016/3/e31/ [ Links ]
Received: March 08, 2019; Accepted: December 16, 2019











 texto en
texto en 
 Curriculum ScienTI
Curriculum ScienTI

