Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.2 Brasília 2020 Epub 15-Abr-2020
http://dx.doi.org/10.5123/s1679-49742020000200012
ORIGINAL ARTICLE
Malaria among indigenous peoples on the Brazil-French Guiana border, 2007-2016: a descriptive study*
1Universidade Federal de Santa Catarina, Programa de Pós-Graduação em Saúde Coletiva, Florianópolis, SC, Brazil
2Universidade Federal do Amapá, Oiapoque, AP, Brazil
3Governo do Estado do Amapá, Superintendência de Vigilância em Saúde, Macapá, AP, Brazil
4Universidade Federal do Amapá, Laboratório de Estudos Morfofuncionais e Parasitários, Macapá, AP, Brazil
Objective:
to describe the profile and incidence of malaria cases among indigenous and non-indigenous people on the Brazil-French Guiana border, between 2007 and 2016.
Methods:
this is a descriptive study based on analysis of cases notified on the Malaria Epidemiological Surveillance Information System (SIVEP-Malaria), organized using Tableau 10.3.
Results:
a total of 21,729 cases were notified in the period; the highest annual number of notifications was 3,637 (16.7%) in 2009, 1,956 (53.8%) of which related to indigenous people, representing annual parasite incidence (API) of 261/1,000; higher risk of infection was found in the Kumenê base area (API between 13 and 534/1,000) and the Manga base area (API between 55 and 448/1,000); children accounted for 20.0 to 40.0% of notified cases, while pregnant women accounted for 2.0% among non-indigenous people and 1.0% among the indigenous.
Conclusion:
malaria case distribution was unequal between indigenous and non-indigenous people, with greater occurrence among the indigenous.
Keywords: Malaria; Epidemiology, Public Health Surveillance; Border Areas; Health of Indigenous Peoples
Introduction
Malaria is an age-old infectious parasitic disease which is hard to control and is widely distributed in many of the world’s countries, including Brazil. In 2017 the World Health Organization (WHO) recorded over 217,000 malaria cases in Brazil, characterizing an 84% increase compared to the previous year.1
Also in 2017, Brazil concentrated the second largest number of cases in the Americas (22%), coming only behind Venezuela which accounted for some 50% of cases. Over 90% of recorded Brazilian cases occur in the Amazon Region, where socio-economic, cultural and environmental issues tend to favor vector reproduction and, consequently, Plasmodium infection. In 2017, there were estimated to have been 189,503 malaria cases in Brazil, with 90% of infections caused by Plasmodium vivax, and 30 reported malaria deaths.1,2
In the border region between Brazil and French Guiana, factors such as the establishment of settlements, mining and mineral prospection areas, migratory and housing conditions and occupational activities are directly linked to increased malaria transmission, in addition to environmental and socio-economic issues.3 Annual parasite incidence (API) is an indicator used to estimate risk of malaria occurrence - indicating low, medium and high risk of infection - in a given population and period. The Brazil-French Guiana border region has had more than 50 malaria cases per 1000 individuals and for this reason has been classified as having high risk of infection among its population and is, therefore, a target of Ministry of Health control actions.
Indigenous peoples, in particular, have led high malaria incidence rates in the Amazon Region: in 2012 they accounted for almost 50% of autochthonous cases recorded in this border area.4-8 According to Basta et al.,7 malaria cases increased considerably between 2003 and 2007. In the border area covered by this study, for example, recorded cases increased from 151 in 2003 to 1,823 in 2007, representing a twelvefold increase. This information can be interpreted as being the result of improved malaria control actions and case recording; however it is still viewed with concern as evidence of a serious problem to be faced by the region’s indigenous peoples. Moreover, it is possible that these numbers are understated, given that unsystematic health care provided in these areas favors underreporting. This in return reflects the health service access situation experienced by indigenous peoples in Brazil.5,6,9,10
Studies conducted focusing on the health of indigenous peoples in Brazil are relatively scarce and the epidemiological and health profiles of this population are far from being established, given the huge socio-economic, geographic and cultural diversity among the different indigenous peoples. This study sought to fill part of this gap, giving visibility to the situation experienced by this population in relation to malaria.
The objective of this study was to described the profile and incidence of malaria cases among indigenous and non-indigenous people on the Brazil-French Guiana border between 2007 and 2016, based on data available on the Malaria Epidemiological Surveillance Information System (SIVEP-Malaria).11
Methods
This is a descriptive study of malaria case distribution in the municipality of Oiapoque, Amapá state, Brazil, notified on the SIVEP-Malaria Information System between 2007 and 2016, focusing on the situation of local indigenous peoples.11
The municipality of Oiapoque is located in the far north of Amapá state on the border with French Guiana. In 2015 it had a population of 24,263 inhabitants, which included approximately 7,000 indigenous people spread over more than 100 native villages: the Karipuna and Galibi Kali’ña ethnic groups, with villages in the Manga base area; the Galibi Marworno ethnic groups, mostly located in the Kumarumã base area; and the Palikur ethnic group, belonging to the Kumenê base area.5,12-14
The data retrieved from the SIVEP-Malaria Information System11 were analyzed using Tableau version 10.3, using the access password of the Amapá State Health Surveillance Superintendent’s Office (SVS/AP), duly authorized by the Ministry of Health National Malaria Control Program. These data were subsequently organized into figures and contingency tables, by relative and absolute frequencies.
The following variables were used:
race/skin color, categorized as ‘indigenous’ and ‘non-indigenous’ (non-indigenous: black, brown, yellow or white);
year of occurrence (within the period 2007-2016);
age group (in completed years: <10; 10-59; ≥60);
place of residence (base area: Kumenê; Kumarumã; Manga);
type of plasmodium or parasite species (vivax; falciparum; mixed; non-falciparum); and
number of cases among pregnant women.
The analysis of reported cases among pregnant women was only done with effect from 2011, owing to limitations of the information system which did not hold information on the ‘race/skin color’ variable for this group for the period 2007-2010.
API was calculated taking the number of positive malaria examination results recorded on the SIVEP-Malaria system as the numerator,11 and the population as the denominator, per 1,000 (one thousand) inhabitants, in a given geographic space, in the year under consideration. Population information was obtained from the Brazilian Institute of Geography and Statistics (IBGE).12,13 The results of cure verification slides were excluded because of their being related to recurrence (resurgence and relapse). The annual risk of occurrence of malaria in endemic areas was estimated according to the following parameters: low (<10.0/1,000 inhab.); medium (10.0-49.9/1,000 inhab.); and high risk (≥50.0/1,000 inhab.).11
The chi-square test was performed to verify the difference between the groups analyzed, whereby values with describable levels equal to or less than 5% (p value ≤0.05) were considered to be statistically significant, using the Bioestat 5.3 application. In this analysis, relationships of dependence between indigenous and non-indigenous people were tested with regard to the ‘number of cases’, ‘incidence’, ‘site of infection’ and ‘cases among pregnant women’ variables. The tests were performed in partitions, i.e. several comparisons for the entire period, between indigenous and non-indigenous people.
All activities were undertaken in accordance with National Health Council Resolution No. 466, dated December 12th 2012. The study project was approved by the Federal University of Amapá Research Ethics Committee, as per Opinion No. 2.430.905, issued on December 12th 2017.
Results
Between 2007 and 2016, 21,756 malaria cases were recorded in the municipality of Oiapoque. Among the indigenous population the highest number of recorded cases (1,956) occurred in 2009, representing an API of 261 per 1000 inhabitants. In the following years, the number of cases fell; but between 2015 and 2016, once again the indigenous population had the highest number of malaria cases in the municipality in relation to the other population segments, with an API of 86 cases per 1,b000 inhab. in 2015 (Figure 1). The chi-square analysis showed that the difference between the proportions of malaria cases for both populations, indigenous and non-indigenous, over the period studied, was dependent on individuals being indigenous (p<0.001).
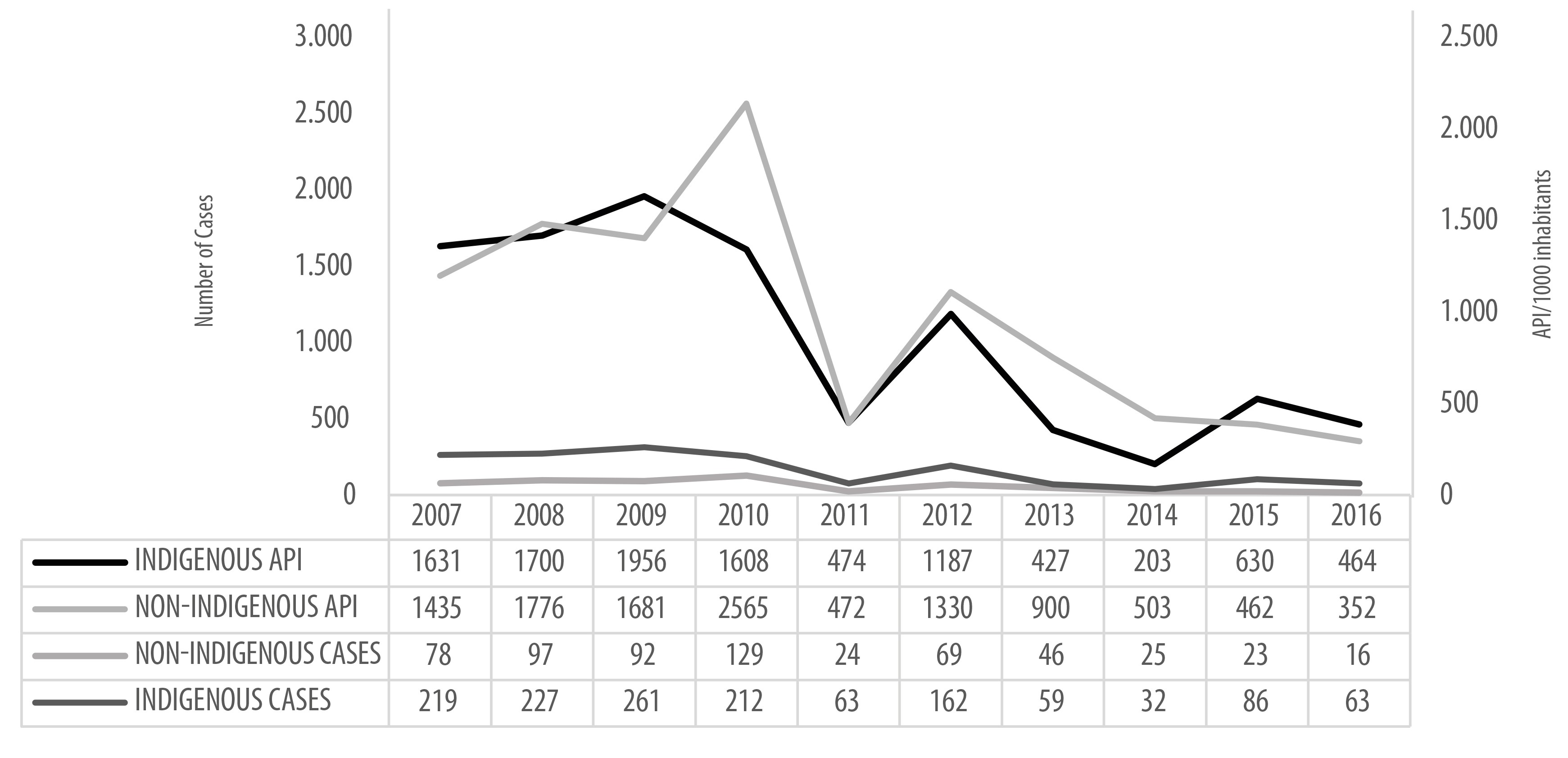
Source: Malaria Epidemiological Surveillance Information System (SIVEP-Malaria), Health Surveillance Secretariat, Ministry of Health. Updated on: 14/12/2017.
Figure 1 - Malaria case distribution and annual parasite incidence (API) among the indigenous and non-indigenous in the municipality of Oiapoque, Amapá, Brazil, according to the Malaria Epidemiological Surveillance Information System, 2007-2016
In addition, when analyzing the differences between malaria case proportions for the ‘place of residence’ (base area) variables among indigenous peoples (Kumarumã, Kumenê and Manga), greater case prevalence and incidence was found in the period 2007-2016 in the Kumenê and Manga base areas, with statistical significance in the comparison of these areas (p<0.001) (Figure 2).
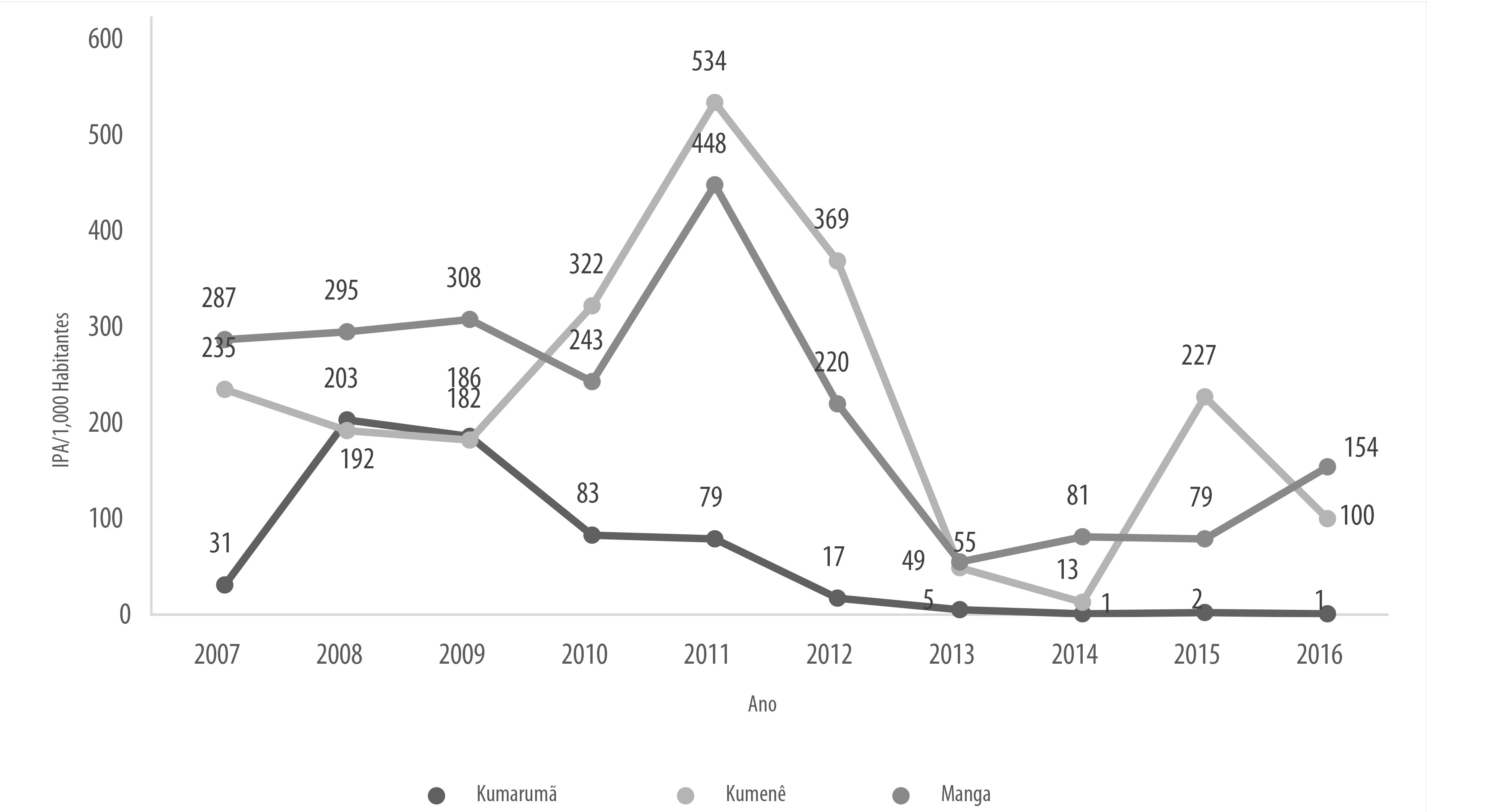
Source: Malaria Epidemiological Surveillance Information System (SIVEP-Malaria), Health Surveillance Secretariat, Ministry of Health. Updated on: 14/12/2017.
Figure 2 - Malaria annual parasite incidence (API) distribution by indigenous base area in the municipality of Oiapoque, Amapá , Brazil, according to the Malaria Epidemiological Surveillance Information System, 2007-2016
Vivax was the most incident type of plasmodium among indigenous and non-indigenous people during the entire period analyzed (2007-2016), regardless of the population segment. However, between 2011 and 2013, a lot of falciparum malaria cases were recorded. This number reduced in 2014 and cases became sporadic in the following years. Falciparum malaria cases were more frequent among the non-indigenous population. In 2012 and 2015, there was an increase in the number of ‘non’ falciparum cases among the indigenous population (Table 1).
Table 1 - Malaria case frequency by parasite species, among the indigenous and non-indigenous in the municipality of Oiapoque, AP, Brazil, according to the Malaria Epidemiological Surveillance Information System, 2007-2016
| Year | Indigenous | Non-indigenous | Total cases | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | V | M+M | Non-F | F | V | M+M | Non-F | ||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | ||
| 2007 | 188 | 6 | 1.433 | 47 | 10 | 0 | - | 0 | 260 | 8 | 1.148 | 37 | 27 | 1 | - | 0 | 3.066 |
| 2008 | 106 | 3 | 1.576 | 45 | 18 | 1 | - | 0 | 330 | 9 | 1.323 | 38 | 123 | 4 | - | 0 | 3.476 |
| 2009 | 203 | 6 | 1.743 | 48 | 10 | 0 | - | 0 | 270 | 7 | 1.366 | 38 | 42 | 1 | - | 0 | 3.634 |
| 2010 | 579 | 14 | 1.020 | 24 | 9 | 0 | - | 0 | 620 | 15 | 1.895 | 45 | 50 | 1 | - | 0 | 4.173 |
| 2011 | 474 | 11 | 1.683 | 38 | 11 | 0 | - | 0 | 472 | 11 | 1.795 | 40 | 34 | 1 | - | 0 | 4.469 |
| 2012 | 47 | 2 | 702 | 28 | 11 | 0 | 427 | 17 | 242 | 10 | 1.054 | 42 | 33 | 1 | 1 | 0 | 2.517 |
| 2013 | 30 | 2 | 380 | 29 | 1 | 0 | 16 | 1 | 128 | 10 | 756 | 57 | 15 | 1 | 1 | 0 | 1.327 |
| 2014 | 4 | 1 | 181 | 26 | - | 0 | 18 | 3 | 24 | 3 | 475 | 67 | 4 | 1 | - | 0 | 706 |
| 2015 | 1 | 0 | 406 | 37 | 1 | 0 | 222 | 20 | 4 | 0 | 448 | 41 | - | 0 | 10 | 1 | 1.092 |
| 2016 | 1 | 0 | 451 | 57 | - | 0 | 12 | 2 | 22 | 3 | 299 | 38 | 3 | 0 | 1 | 0 | 789 |
Legend
F: Plasmodium falciparum, or P. falciparum.
V: Plasmodium vivax.
M+M: P. malariae + mixed (P. falciparum and P. vivax in the same infection) .
Non-: non-P. falciparum (result of rapid test sample collections).
Source: Malaria Epidemiological Surveillance Information System (SIVEP-Malaria), Health Surveillance Secretariat, Ministry of Health. Updated on: 14/12/2017.
Note: the frequencies (%) are relative to the total number of notified cases; values under 0.5% have been rounded to ‘0’.
Among pregnant women in the period 2011-2016, greater frequency of recorded malaria cases was found in women of brown skin color and indigenous women in Oiapoque (Figure 3). There was no significant difference between malaria cases in the groups classified according to race/skin color among pregnant women (p=0.006).
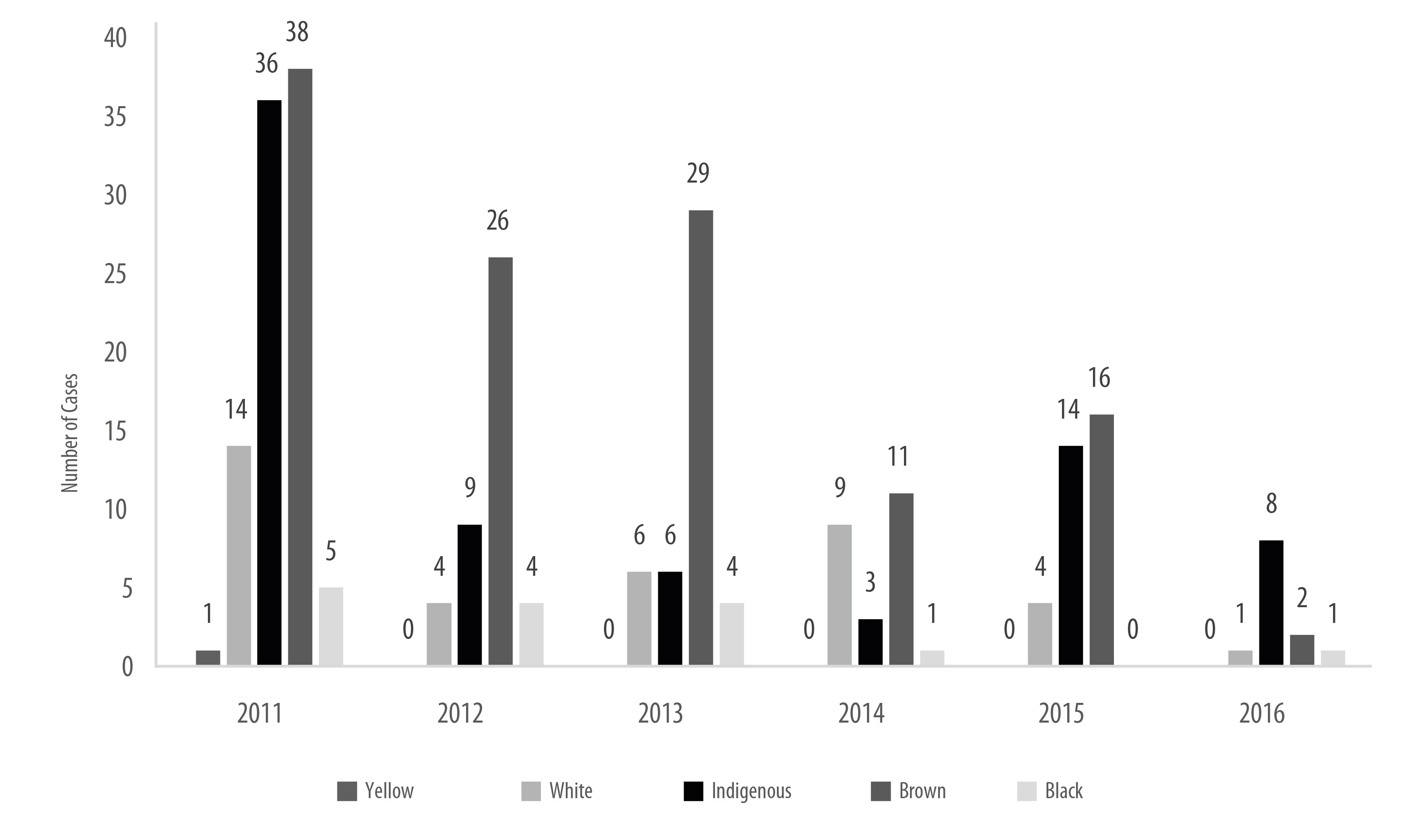
Source: Malaria Epidemiological Surveillance Information System (SIVEP-Malaria), Health Surveillance Secretariat, Ministry of Health. Updated on: 14/12/2017.
Figure 3 - Malaria cases in pregnant women, per race/skin color, in the municipality of Oiapoque, Amapá, Brazil, according to the Malaria Epidemiological Surveillance Information System, 2011-2016
When analyzing case distribution per age group among both indigenous and non-indigenous people, in the period from 2007 to 2016, the percentage was found to vary between 20% and 40% of cases in those under 10 years old, while the highest concentration was found among young adults (10 to 59 years old). This situation was very similar in both population segments throughout the entire period (Table 2). The number of malaria cases in children was substantial, with slight oscillations over the ten-year period studied.
Table 2 - Malaria case distribution by age group, among the indigenous and non-indigenous, in the municipality of Oiapoque, Amapá, Brazil, according to the Malaria Epidemiological Surveillance Information System, 2007-2016
| Age ranges (in years) | Period | Total | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | ||||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | |
| Indigenous | |||||||||||||||||||||
| <10 | 718 | 44 | 612 | 36 | 724 | 37 | 338 | 21 | 161 | 34 | 475 | 40 | 132 | 31 | 89 | 44 | 107 | 17 | 111 | 24 | 3,467 |
| 10-59 | 913 | 56 | 1,085 | 63 | 1,229 | 62 | 1,269 | 78 | 307 | 65 | 710 | 60 | 293 | 65 | 114 | 55 | 523 | 82 | 353 | 75 | 6,796 |
| ≥60 | - | 0 | 3 | 1 | 3 | 1 | 1 | 1 | 6 | 1 | 2 | 0 | 2 | 4 | - | 1 | - | 1 | - | 1 | 17 |
| Total | 1,631 | 100 | 1,700 | 100 | 1,956 | 100 | 1,608 | 100 | 474 | 100 | 1,187 | 100 | 427 | 100 | 203 | 100 | 630 | 100 | 464 | 100 | 10,280 |
| Non-indigenous | |||||||||||||||||||||
| <10 | 660 | 46 | 657 | 37 | 303 | 18 | 359 | 14 | 66 | 14 | 292 | 22 | 162 | 18 | 65 | 13 | 69 | 15 | 36 | 11 | 2,669 |
| 10-59 | 774 | 54 | 1,116 | 63 | 1,370 | 81 | 2,203 | 86 | 398 | 83 | 1,036 | 78 | 735 | 82 | 437 | 87 | 393 | 85 | 286 | 88 | 8,748 |
| ≥60 | 1 | 0 | 3 | 0 | 8 | 1 | 3 | 0 | 8 | 3 | 2 | 0 | 3 | 0 | 1 | 0 | - | 0 | 3 | 1 | 32 |
| Total | 1,435 | 100 | 1,776 | 100 | 1,681 | 100 | 2,565 | 100 | 472 | 100 | 1,330 | 100 | 900 | 100 | 503 | 10 | 462 | 100 | 325 | 100 | 11,449 |
Source: Malaria Epidemiological Surveillance Information System (SIVEP-Malaria), Health Surveillance Secretariat, Ministry of Health. Updated on: 14/12/2017.
Note: proportional values under 0.5% have been rounded to ‘0’
Discussion
During the period from 2007 to 2016, the API indicator enabled a more substantial risk of becoming ill from malaria among indigenous peoples to be identified. In practically all the years analyzed, API rates were above 50 recorded cases per 1000 inhab. and therefore with high risk of infection, with an important increase between 2007 and 2010, when the rates were above 200/1000 inhab., almost three times higher than the rates among the non-indigenous population. Although in some years the number of cases was higher among the non-indigenous segment, in all the years in the period studied incidence was higher among indigenous peoples.
According to Ministry of Health information, malaria case incidence in indigenous communities, as a general rule, increased considerably between 2012 and 2014. This resulted in prevention and control measures being directed towards the indigenous, promoting and rearranging the health network and health practices and developing administrative and managerial activities necessary for providing care, with social participation, with the aim of reducing the epidemics that are rife among their communities.9,10
The closeness of the indigenous peoples to bush and forest environments is propitious to greater exposure to pathogens present in the natural environment, especially in frontier areas.3,7 Also according to the Ministry of Health, the municipalities located along the Amazon frontier region accounted for 37.2% of all malaria cases recorded in Brazil in 2010,9,10 so that it is fundamental to pay close attention to these areas and seek out the determinants of this increase in the number of cases.
According to Braz, Duarte and Tauil,4the risk of becoming ill from malaria among indigenous peoples is two times greater than among the non-indigenous in the Amazon; this representativeness in relation to malaria incidence has also been described by Lapouble et al.15 These studies found that almost half the municipalities in the Brazilian Amazon had some type of malaria epidemic between 2003 and 2012, providing evidence that epidemic phenomena occur more in municipalities with indigenous populations, settlements and mining activities, as well as in border municipalities.4,15
This panorama contributes to malaria transmission, owing to increased exposure and, consequently, increased contact between vectors and inhabitants, thus requiring greater health service attention.4 This inequality in relation to the health situation of the indigenous compared to other populations has been found in various studies and is more substantial in the case of infectious and parasitic diseases.7,16
It can be stated that the most common parasite in circulation in the frontier area between Brazil and French Guiana is Plasmodium vivax. However, despite the municipality of Oiapoque having been part of the group with the highest percentage of falciparum cases on the Amazon Region, the falling trend in cases caused by this parasite species continues, including among the indigenous peoples of the region.4,15 There are several facts that can explain this trend, such as (i) P. vivax having broader geographic distribution, given that the vector is capable of tolerating great temperature variations and surviving at higher altitudes, (ii) presence of dormant liver stages (hypnozoites) that can be activated months after initial infection, causing relapses and early circulation of the sexual stages (gametocytes) in peripheral blood, which can make this Plasmodium less sensitive in relation to falciparum, and (iii) control strategies implemented by WHO and the Ministry of Health aimed at reducing falciparum in recent years.17,18
In the analysis by age group, there was high distribution in the under 10 year-olds among the indigenous. The proportion of cases, as well as their reduction in the final years analyzed, was similar between both population segments in the period 2007-2016. In relation to case distribution by age, corroborating various reports for the Amazon Region, we found that malaria has frequently affected both indigenous and non-indigenous children, characterizing them as a group that can be considered to be at greater risk and that therefore needs better care. This context potentializes the socio-cultural issues involved in this age group becoming ill and which do not apply only to indigenous peoples.10,14
The combination of biological determinants (herd immunity), cultural determinants (type of dwelling, relations with national society, cultural competencies), socio-political determinants (access to health services) and geographic determinants (being located in frontier and hard-to-reach areas) results in malaria in indigenous areas having a differentiated epidemiological behavior.4 Malaria transmission in indigenous frontier areas is also influenced by the diversity and complexity of the relations that establish themselves in frontier areas; it is, however, little studied, despite Brazil having many initiatives with other countries aimed at integrated malaria control.2 Moreover, health care in Brazil’s frontier areas is marked by shortage of health professionals and consequently by the population in these areas having difficulty in accessing these services.
It is important to mention that there is a specific health policy for indigenous peoples. In this sense, Brazilian National Health System (SUS) Primary Care should tailor its actions directed towards them, taking into consideration the way they organize themselves, so as to favor health promotion and the prevention of diseases such as malaria.20,21 High mobility of the indigenous in frontier areas, difficulties faced by health teams in accessing these regions and the persistent incursion of prospectors and miners hamper malaria control actions in these regions. Constant mobility in these areas also contributes to the changing epidemiological profile of malaria.22,23
Another relevant condition relates to malaria cases in pregnancy. Pregnant women in endemic areas are affected relatively frequently, causing a series of harmful effects for both mother and fetus.24 Pregnant women are particularly vulnerable to malaria because their immune status changes during pregnancy, making them more susceptible to alterations during the course of pregnancy, increasing the risk of complicated forms of the disease. For the fetus, maternal malaria is frequent cause of threatened miscarriage, premature childbirth, low weight at birth, intrauterine growth restriction and maternal anemia.25,26 Cases can be more severe in pregnant women, children and people with primary infection, especially when infected by P. falciparum, and may progress to death.
It is important to note that the fact that the placenta is a propitious place for parasite multiplication can make pregnant women more sensitive to malaria, with exacerbation of symptoms and greater risk of complications.27,28 In 2001 and 2002, a population-based epidemiological survey conducted in the municipality of Coari, in Amazonas state, found 4.3% infection prevalence among pregnant women, compared to 0.8% prevalence among women in the same age group who were not pregnant.27
Various studies on the subject reveal that shortcomings in the physiopathological approach to maternal malaria and specific difficulties with treatment are limitations or impediments to information and analysis.27,28 As such, studies are needed on the possible impacts of malaria during pregnancy, estimating the frequency of the main alterations during the course of pregnancy and identifying possible factors associated with infection, in order to inform public policies for prevention and health care.
Within this context, indigenous health care has shown itself to be a challenge, given the peculiarities of the health needs of these populations. Diseases such as malaria, diarrhea, malnutrition, tuberculosis and respiratory infections still stand out in the epidemiological profile of these peoples. Although this profile has undergone changes over the years, it continues to be characterized by great disparity between the indigenous and other population segments.5,7,21,29 Given the high incidence of malaria during the study period (2007-2016), it is important to pay special attention to the indigenous, above all because of their marked presence in the frontier area between Brazil and French Guiana, owing to the various forms of mobility existing in this region.
This condition of mobility among indigenous peoples is reflected in the non-homogenous distribution of malaria in the frontier areas; furthermore, areas with greater or lesser transmission vary over the years, due to movements of the populations there.22,29 It is important to highlight that cultural competencies and traditional knowledge have been described by authors as being important points to be taken into consideration when assessing and planning actions related to malaria control among the indigenous.21 Different perceptions related to the health-disease process and the diverse self-care processes of people with malaria directly influence the behavior of these people and the results expected with regard to the impact of the disease, depending on the community or territory.24,30 New studies are also needed to gain a better understanding of the dynamics of malaria transmission among indigenous peoples.
This study has contributed to outlining the profiles of illness caused by malaria among the indigenous peoples of a frontier area. A limitation to its development, analysis and conclusions lies in the quality of the records held on the Malaria Epidemiological Surveillance Information System - SIVAP-Malaria -, given the possibility of duplicated information, failure to record or incorrect recording of the race/skin color variable, which may lead to underreporting of cases among the indigenous. Another limitation of the study lies in the fact that SIVAP-Malaria does not specify the clinical forms of the disease, this being information that would enable further analyses. However, given the amplitude of the data, it would not be possible to obtain the information needed from sources other than SIVAP-Malaria.
Malaria control among the indigenous is a complex action. Socio-economic, cultural, environmental, ecological, biological and logistical issues involved in approaching this population affect the efficacy of control and prevention measures, implying the need for investment in research that seeks to find viable response alternatives to these challenges. It should be highlighted that the Manga and Kumenê villages deserve special attention, strengthening and greater precision in targeting malaria control and prevention actions, given that these are the places with the greatest case distribution on the frontier between Brazil and French Guiana.
REFERENCES
1. World Health Organization. World malaria report [Internet]. Geneva: World Health Organization; 2018 [cited 2020 Feb 13]. Available from: Available from: https://www.who.int/malaria/publications/world-malaria-report-2018/en/ [ Links ]
2. World Health Organization. World malaria report. Geneva: World Health Organization ; 2019 [cited 2020 Feb 13]. Available from: Available from: https://www.who.int/publications-detail/world-malaria-report-2019 [ Links ]
3. Alves MR. Dinâmica espacial da malária em aldeias indígenas da região amazônica brasileira [dissertação]. Rio de Janeiro: Fundação Instituto Oswaldo Cruz / Escola Nacional de Saúde Pública Sergio Arouca; 2010. [ Links ]
4. Braz RM, Duarte EC, Tauil PL. Characteristics of malária epidemics in the municipalities of the Brazilian Amazon. Cad Saúde Pública [Internet]. 2013 May [cited 2020 Feb 13];29(5):935-44. Available from: Available from: https://doi.org/10.1590/S0102-311X2013000500011 [ Links ]
5. Mendes AM. Situação epidemiológica da malária no município de Oiapoque-AP. Relatório anual: articulador municipal nas ações de controle e malária. Oiapoque: Ministério da Saúde; 2013. [ Links ]
6. Franco VC. Determinantes da malária em municípios da faixa de fronteira da região Amazônica: o caso do Oiapoque [dissertação]. Rio de Janeiro: Fundação Instituto Oswaldo Cruz / Escola Nacional de Saúde Pública Sergio Arouca; 2013. Disponível em: https://www.arca.fiocruz.br/handle/icict/25150 [ Links ]
7. Basta PC, Orellana JDY, Arantes R. Perfil epidemiológico dos povos indígenas no Brasil: notas sobre agravos selecionados. In: Garnelo L, Pontes AL (Org.) Saúde indígena: uma introdução ao tema [Internet]. Brasília: MEC-SECADI; 2012 [citado 2020 fev 13]. p. 60-107. (Série Via dos Saberes n° 5). [ Links ]
8. Vieira PRR. Malária na área indígena: espacialização dos casos autóctones no município do Oiapoque-Amapá [dissertação]. Macapá: Universidade Federal do Amapá; 2011. Disponível em: http://unbral.nuvem.ufrgs.br/portal/items/show/1172 [ Links ]
9. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Situação epidemiológica da malária no Brasil, 2012 e 2013. Bol Epidemiol [Internet]. 2015 [citado 2020 fev 13];44(1):1-17. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/periodicos/boletim_epidemiologico_numero_1_2013.pdf [ Links ]
10. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Malária: monitoramento dos casos no Brasil em 2014. Bol Epidemiol [Internet]. 2015 [citado 2020 fev 13];46(25):1-5. Disponível em: Disponível em: https://portalarquivos2.saude.gov.br/images/pdf/2015/agosto/18/2015-009---Mal--ria-para-publica----o.pdf [ Links ]
11. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Sistema de Informação de Vigilância Epidemiológica da Malária (SIVEP-Malária) [Internet]. Brasília: Ministério da Saúde; 2017 [citado 2017 jul 18]. Disponível em: Disponível em: http://www.saude.gov.br/sivep_malaria [ Links ]
12. Instituto Brasileiro de Geografia e Estatística. Os indígenas no censo demográfico 2010: primeiras considerações com base no quesito cor ou raça [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2012 [citado 2020 fev 13]. 31 p. Disponível em: Disponível em: https://indigenas.ibge.gov.br/images/indigenas/estudos/indigena_censo2010.pdf [ Links ]
13. Instituto Brasileiro de Geografia e Estatística. Censo demográfico: Oiapoque [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística ; 2015 [citado 2017 fev 8]. Disponível em: Disponível em: https://cidades.ibge.gov.br/brasil/ap/oiapoque/panorama [ Links ]
14. Galois DT, Grupioni DF. Povos indígenas no Amapá e norte do Pará: quem são, onde estão, quantos são, como vivem e o que pensam? [Internet]. São Paulo: Instituto de Pesquisa e Formação em Educação Indígena, Núcleo de História Indígena e do Indigenismo da Universidade de São Paulo; 2009 [citado 2020 fev 13]. 96 p. Disponível em: Disponível em: https://www.institutoiepe.org.br/media/livros/livro_povos_indigenas_no_AP_e_N_do_PA-sem_fotos.pdf [ Links ]
15. Lapouble OMM, Santelli ACFS, Muniz-Junqueira MI. Situação epidemiológica da malária na região amazônica brasileira, 2003 a 2012. Rev Panam Salud Pública [Internet]. 2015 [citado 2020 fev 13];38(4):300-6. Disponível em: Disponível em: https://www.scielosp.org/pdf/rpsp/2015.v38n4/300-306 [ Links ]
16. Mendes AM, Bastos JL, Bresan D, Leite MS. Epidemiologic situation of tuberculosis in Rio Grande do Sul: an analysis about Sinan’s data between 2003 and 2012 focusing on indigenous peoples. Rev Bras Epidemiol [Internet]. 2016 jul-sep [cited 2020 Feb 13];19(3):658-69. Available from: Available from: https://doi.org/10.1590/1980-5497201600030015 [ Links ]
17. Shanks GD. Control and elimination of Plasmodium vivax. Adv Parasitol [Internet]. 2012 [cited 2020 Feb 13];80(5):301-41. Available from: Available from: https://doi.org/10.1016/B978-0-12-397900-1.00006-2 [ Links ]
18. World Health Organization. World malaria report 2015 [Internet]. Geneva: World Health Organization ; 2015 [cited 2020 Feb 13]. Available from: Available from: https://www.who.int/malaria/publications/world-malaria-report-2015/report/en/ [ Links ]
19. Gomes MSM, Vieira JLF, Machado RLD, Nacher M, Stefani A, Musset L, et al. Efficacy in the treatment of malaria by Plasmodium vivax in Oiapoque, Brazil, on the border with French Guiana: the importance of control over external factors. Malar J [Internet]. 2015 Oct [cited 2020 Feb 13];14:402. Available from: Available from: https://malariajournal.biomedcentral.com/articles/10.1186/s12936-015-0925-7 [ Links ]
20. Rodrigues EC, Lopes Neto D. Malaria control in na Amazon municipality. Rev Latino-Am Enferm [Internet]. 2011 Nov-Dec [cited 2020 Feb 13];19(6):1297-305. Available from: Available from: https://doi.org/10.1590/S0104-11692011000600004 [ Links ]
21. Mendes AM, Leite MS, Langdon EJ, Grisotti M. O desafio da atenção primária na saúde indígena no Brasil. Rev Panam Salud Pública [Internet]. 2018 nov [citado 2020 fev 13];42:184. Disponível em: Disponível em: https://doi.org/10.26633/RPSP.2018.184 [ Links ]
22. Peiter PC. Living conditions, health status and health services availability along the Brazilian border: a geographical approach. Cad Saúde Pública [Internet]. 2007 [cited 2020 Feb 13];23 Suppl 2:S237-50. Available from: Available from: https://doi.org/10.1590/S0102-311X2007001400013 [ Links ]
23. Menezes RAO, Gomes MDSM, Mendes AM, Couto ÁARDA, Nacher M, Pimenta TS, et al. Enteroparasite and vivax malaria co-infection on the Brazil-French Guiana border: Epidemiological, haematological and immunological aspects. PloS One [Internet]. 2018 Jan [cited 2020 Feb 13];13(1):1-20. Available from: Available from: https://doi.org/10.1371/journal.pone.0189958 [ Links ]
24. Fernandez-Niño JÁ, Idrovo AJ, Giraldo-Gartner V, Molina-León HF. Los domínios culturales de la malária: uma aproximaciòn a los saberes no institucionales. Rev Biomédica [Internet]. 2014 [citado 2020 fev 13];34(2):250-9. Disponível em: Disponível em: https://doi.org/10.7705/biomedica.v34i2.1629 [ Links ]
25. Santos RCS, Araújo OCL. Malária na gestação. Est Científica [Internet]. 2011 [citado 2020 fev 13];1(2):45-53. Disponível em: Disponível em: https://periodicos.unifap.br/index.php/estacao/article/view/243/rafaelv1n2.pdf [ Links ]
26. Martins ND. Estudo epidemiológico de casos de malária em gestantes no Estado do Amapá entre 2003 e 2012. Biota Amazônia [Internet]. 2014 [citado 2020 fev 13];4(1):22-9. Disponível em: Disponível em: http://dx.doi.org/10.18561/2179-5746/biotaamazonia.v4n1p22-29 [ Links ]
27. Chagas ECS, Nascimento CT, Santana Filho FS, Bôtto-Menezes CH, Martinez-Espinosa FE. Malária durante a gravidez: efeito sobre o curso da gestação na região amazônica. Rev Panam Salud Pública [Internet]. 2009 [citado 2020 fev 13];26(3):203-08. Disponível em: Disponível em: https://www.arca.fiocruz.br/handle/icict/1909 [ Links ]
28. Fernandes FB, Lopes RGC, Mendes-Filho SPM. Malária grave em gestantes. Rev Bras Ginecol Obstet [Internet]. 2010 dez [citado 2020 fev 13];32(1):579-83. Disponível em: Disponível em: https://doi.org/10.1590/S0100-72032010001200003 [ Links ]
29. Teixeira LF. A malária no estado do Amazonas de 2003 a 2011: distribuição espaço-temporal e correlação com populações indígenas [dissertação]. Rio de Janeiro: Fundação Instituto Oswaldo Cruz; 2014. Disponível em: https://www.arca.fiocruz.br/handle/icict/13363 [ Links ]
30. Rodrigues-Ocaña E. Nuevos aires, aguas y lugares. Luchas contra la malaria y la historia social de las enfermedades. Dynamis [Internet]. 2009 [citado 2020 fev 13];29:365-75. Disponível em: Disponível em: http://scielo.isciii.es/pdf/dyn/v29/16.pdf [ Links ]
Received: April 01, 2019; Accepted: January 29, 2020











 texto em
texto em 


