Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.2 Brasília 2020 Epub 24-Abr-2020
http://dx.doi.org/10.5123/s1679-49742020000200014
ORIGINAL ARTICLE
Suicide mortality in Rio Grande do Sul, Brazil: a cross-sectional analysis of cases, 2017-2018
1Instituto-Geral de Perícias do Rio Grande do Sul, Departamento de Perícias Laboratoriais, Porto Alegre, RS, Brazil
2Pan American Health Organization/World Health Organization, Washington, DC, USA
3Universidade Federal do Rio Grande do Sul, Programa de Pós-Graduação em Ciências Farmacêuticas, Porto Alegre, RS, Brazil
Objective:
to analyze the epidemiological and toxicological profile of suicide cases in Rio Grande do Sul, Brazil, in 2017 and 2018.
Methods:
this was a cross-sectional study with data from police incident reports and state General Forensic Institute records; multiple correspondence analyses were performed and logistic regression models were built.
Results:
there were 2,564 suicides (11.3/100,000 inhabitants/year), mostly involving males (79.4%), and the 50-54 years age group (10.3%); the main method was hanging (72.5%); positive results for ethanol were found in 29.1% of cases and for other psychotropic drugs in 36.1% of cases; young people were 4.5 times (95%CI 2.7;7.7) and 2.4 times (95%CI 1.5;3.6) more likely to be the victims when there were positive results for an illegal substance or parental absence, respectively.
Conclusion:
male and adult victims predominated, hanging was the most common means, and, in one third of the cases, psychotropic drugs were present.
Keywords: Suicide; Cross-Sectional Studies; Demography; Public Health; Forensic Toxicology; Multivariate Analysis
Introduction
Suicide, or death caused by intentional self-inflected injury, is among the ten leading causes of death worldwide, with more than 800,000 victims every year (2012),1)-(3 affecting around 65,000 people in the region of the Americas alone (2005-2009).3),(4
The World Health Organization (WHO) has set a target for reducing the mortality rate for this public health problem by 10% by 2020, starting as at 2013. To this end, it intends to develop preventive actions, including the implementation of strategies focused on populations at greater risk.5 In January 2018, only 28 of the 194 WHO Member States reported having a suicide prevention measure in force on the national level.6
Suicide is multifactorial and involves family, community, social, public health and mental illness aspects, as well as varying by region.2),(4),(7 In Brazil the mean suicide mortality rate between 2010 and 2014 was 5.2 cases per 100,000 inhabitants/year.8 In 2015 this rate increased to 6.62 while in 2016 it was 6.1.9
The state of Rio Grande do Sul (RS) has historically had the highest suicide rate among the Brazilian Federative Units.10 In 2015, the rate was 10.5 cases per 100,000 inhab.,2 and in 2016 it was 11.0/100,000 inhab.,9),(11 whereby the rate was higher among males (17.8) than among females (4.5).9
Knowledge about current incidence, characteristics of the victims, common aspects and the most affected regions enables local preventive actions to be developed, by health services and also by society, which assist in identifying the population at risk and in reducing stigma related to the phenomenon.
The objective of this study was to analyze the epidemiological and toxicological profile of suicide victims in the state of Rio Grande do Sul, Brazil, in 2017 and 2018.
Methods
A cross-sectional study was conducted involving all deaths recorded as suicide in the state of Rio Grande do Sul (RS), between January 1st 2017 and December 31st 2018.
Located in the far south of Brazil, RS is the country’s fifth most populous state, having 11,377,239 inhab. (2019), most of whom live in urban areas. In 2009, the state had approximately 4,000 beds in public health establishments, coming in thirteenth place nationally. Moreover, in 2013, the state recorded the highest percentage in Brazil of cases of depression per mental health professional: 13.2%.12
All autopsy records held at the Rio Grande do Sul General Forensic Institute (IGP-RS) related to suicide were examined, as were the respective toxicology reports issued by the IGP-RS Laboratory Examinations Department. Police incident reports were also consulted via the state Public Security Department computerized systems.
All victims of suicide in RS in the period under assessment were classified according to the following variables:
sex (male; female);
age (in years: child [0-12]; adolescent [13-18]; adult [19-59]; elderly [60 or over]);
youth, aged 15-29 years (youth; not youth);
parental absence on birth record (absence; presence);
cause of death (hanging; use of firearm; intoxication; jumping; use of cold weapon; other);
city where death occurred;
region13 where death occurred (Alto-Jacuí; Campanha; Central; Centro Sul; Fronteira Noroeste; Fronteira Oeste; Hortênsias; Litoral; Médio Alto Uruguai; Metropolitano Delta do Jacuí; Missões; Nordeste; Noroeste Colonial; Norte; Paranhana-Encosta Serra; Produção; Serra; Sul; Vale do Caí; Vale do Rio dos Sinos; Vale do Rio Pardo; Vale do Taquari);
macro-region14 in which death occurred (Porto Alegre; Caxias do Sul; Santa Maria; Pelotas; Passo Fundo);
year of death (2017; 2018);
toxicology (toxicology available; no information);
ethanol (positive; negative; no information);
psychotropic drugs (positive; negative; no information);
anxiolytic drugs (positive; negative; no information);
antidepressants (positive; negative; no information);
illicit compounds (positive; negative; no information); and
poisons (positive; negative; no information).
Quantitative analyses for ethanol (dg/L) were performed using whole blood samples, while qualitative analyses, both for psychotropic drugs and poisons, were performed using urine, vitreous humor and/or entrails.
Suicide rates per 100,000 inhab. were calculated taking the number of cases in each municipality of RS and its population size in 2017 and 2018, as estimated by the Brazilian Institute of Geography and Statistics (IBGE).12 Rate ratios between the sexes (male/female) were estimated.
Descriptive statistics were calculated and multiple corresponding analysis was performed, the interpretation of which is based on the proximity between categories situated in the same area of the diagram. In this form of analysis, however, there is not a direct relationship between the distances between the points,15 so that other complementary statistical tests need to be used.
Logistic regression models were used to estimate associations, taking a 5% significance level. Six independent models were built:
Model A (dependent variable ‘youth’ and independent variable ‘region’; model adjusted by sex);
Model B (dependent variable ‘poisons’ and independent variable ‘region’; model adjusted by sex and age);
Model C (dependent variable ‘toxicology’ and independent variable ‘region’; model adjusted by year);
Model D (dependent variable ‘ethanol’ and independent variables, ‘sex’, ‘age, ‘parental absence’, ‘cause of death’, ‘psychotropics’, ‘anxiolytics’, ‘antidepressants’ and ‘illicit compounds’);
Model E (dependent variable ‘psychotropics’ and independent variables, ‘sex’, ‘age, ‘parental absence’, ‘cause of death’ and ‘ethanol’); and
Model F (dependent variable ‘youth’ and independent variables, ‘sex’, ‘parental absence’, ‘cause of death’, ‘ethanol’, ‘psychotropics’, ‘anxiolytics’, ‘antidepressants’ and ‘illicit compounds’).
The Hosmer-Lemeshow test was used to check the fit of the logistic models. The free software R® version 3.5.1 was used in all the analyses.
The study project was approved by the Rio Grande do Sul Federal University Research Ethics Committee (CEP/UFRGS): Opinion No. 2.532.550, dated March 8th 2018.
Results
There were 2,546 records of suicide deaths in RS: namely 1,284 in 2017 and 1,280 in 2018, corresponding to a rate of 11.3 cases/100,000 inhab./year. The Caxias do Sul and Passo Fundo macro-regions had the highest rates in 2017, both having 13.9 cases/100,000 inhab. In 2018, the highest rate (15.1) was found in the Passo Fundo marco-region. The Vale do Rio Pardo and Médio Alto Uruguai regions had the highest rates in 2017 and 2018, respectively (Table 1). The Paranhana-Encosta Serra and Hortênsias regions recorded an increase in the total number of suicides; while the Metropolitano Delta do Jacuí region, where the state capital is located, recorded a reduction.
Table 1 - Suicide case distribution by regions and odds ratios of associations estimated using logistic models, Rio Grande do Sul, 2017-2018
| Independent variable | Year | Dependent variables | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | Youth (Model A) | Poison (Model B) | Toxicology (no information) (Model C) | ||||||||
| n | Rate | Sex Ratio | n | Sex Ratio | Sex Ratio | ORa | n | ORa | n | ORa | n | |
| Region | p=0.003 | p<0.001 | p<0.001 | |||||||||
| Alto-Jacuíb | 28 | 14.8 | 2.1 | 15 | 8.1 | 14.0 | 1.7 (0.7;4.6) | 8 | - | - | 8.3 (3.5;22.8) | 6 |
| Campanhab | 21 | 9.3 | 4.3 | 22 | 9.9 | 4.5 | 3.0 (1.1;9.7) | 5 | 2.0 (0.1;49.7) | 1 | 0.8 (0.4;1.5) | 27 |
| Centrab | 86 | 12.6 | 3.5 | 88 | 13.1 | 3.6 | 1.8 (0.9;3.5) | 31 | 4.2 (1.0;19.6) | 4 | reference | 98 |
| Centro Sulc | 36 | 13.7 | 8.0 | 35 | 13.3 | 1.5 | 1.1 (0.5;2.5) | 18 | 3.7 (0.6;29.7) | 2 | 14.1 (6.2;38.0) | 6 |
| Fronteira Noroested | 41 | 18.2 | 3.6 | 39 | 17.8 | 5.5 | 2.5 (1.1;5.8)* | 11 | - | - | - | - |
| Fronteira Oesteb | 60 | 11.1 | 9.0 | 60 | 11.5 | 5.7 | 2.3 (1.1;4.7) | 18 | - | - | 2.6 (1.6;4.2) | 40 |
| Hortênsiase | 11 | 7.5 | 1.8 | 21 | 14.2 | 4.3 | 2.1 (0.7;6.9) | 5 | 3.4 (0.3;78.8) | 1 | 8.8 (3.2;30.6) | 4 |
| Litorale | 35 | 9.4 | 7.8 | 44 | 11.4 | 7.8 | 2.0 (0.9;4.6) | 13 | - | - | 19.0 (8.0;56.1) | 5 |
| Médio Alto Uruguaid | 28 | 15.9 | 2.1 | 36 | 21.2 | 2.6 | 1.5 (0.7;3.5) | 13 | 11.7 (2;24.1) | 1 | 15.1 (6.3;44.9) | 5 |
| Metropolitano Delta do Jacuíe | 217 | 8.6 | 4.0 | 188 | 7.4 | 2.5 | 1.3 (0.7;2.2) | 96 | 17.4 (5.0;65.5) | 6 | 17.0 (10.6;27.9) | 29 |
| Missõesd | 34 | 14.5 | 2.8 | 36 | 15.9 | 2.6 | 1.9 (0.8;4.3) | 12 | 4.5 (0.8;36.3) | 2 | 21.4 (8.4;72.6) | 4 |
| Nordestef | 36 | 17 | 5.0 | 31 | 14.7 | 5.2 | reference | 19 | reference | 8 | 2.7 (1.5;4.9) | 22 |
| Noroeste Coloniald | 37 | 11.6 | 6.4 | 42 | 13.4 | 3.2 | 2.7 (1.2;6.6) | 10 | 17.0 (2.5;345) | 1 | 5.5 (3.0;10.7) | 15 |
| Norted | 34 | 15.3 | 4.7 | 29 | 13.3 | 13.5 | 2.7 (1.1;7.2) | 8 | 3.7 (0.7;29.7) | 2 | 1.7 (1.0;3.1) | 27 |
| Paranhana-Encosta Serrae | 14 | 6.2 | 13.0 | 22 | 9.5 | 4.5 | 1.6 (0.6;4.6) | 7 | - | - | 44.3 (9.2;797) | 1 |
| Produçãod | 72 | 13.9 | 5.5 | 70 | 13.5 | 3.4 | 1.8 (0.9;3.6) | 25 | 22.4 (3.4;448) | 1 | 5.8 (3.5;9.9) | 26 |
| Serraf | 97 | 10.1 | 4.1 | 80 | 8.1 | 2.8 | 1.6 (0.8;3.0) | 35 | 2.1 (0.7;7.0) | 13 | 16.6 (9.0;32.7) | 13 |
| Sulc | 111 | 12.5 | 3.4 | 114 | 12.9 | 3.8 | 2.1 (1.1;3.9) | 36 | 12.9 (3.0;70.0) | 3 | 3.1 (2.0;4.6) | 67 |
| Vale do Caíf | 22 | 12 | 4.5 | 28 | 14.9 | 6.0 | 9.5 (2.6;61.8) | 2 | - | - | 20.1 (7.0;84.9) | 3 |
| Vale do Rio dos Sinose | 113 | 8.2 | 3.5 | 128 | 9.2 | 4.3 | 1.7 (0.9;3.1) | 46 | 62.8 (10;1249) | 1 | 27.0 (14.3;55.8) | 11 |
| Vale do Rio Pardof | 96 | 20.8 | 5.0 | 90 | 19.5 | 4.0 | 2.7 (1.3;5.3) | 24 | 5.0 (1.3;21.1) | 5 | 1.3 (0.9;2.0) | 93 |
| Vale do Taquarif | 55 | 14.8 | 4.0 | 62 | 16.5 | 3.4 | 3.8 (1.7;8.8) | 11 | 1.8 (0.3;11.2) | 3 | 1.0 (0.6;1.6) | 66 |
| Total | 1.284 | 11.3 | 4.2 | 1.280 | 11.3 | 3.6 | - | 453 | - | 54 | - | 568 |
a) OR: odds ratio, with 95% confidence interval (95%CI).
b) Santa Maria macro-region.
c) Pelotas macro-region.
d) Passo Fundo macro-region.
e) Porto Alegre macro-region.
f) Caxias do Sul macro-region.
Notes:
Model A (dependent variable ‘youth’ and independent variable ‘region’, adjusted by sex).
Model B (dependent variable ‘poisons’ and independent variable ‘region’, adjusted by sex and age).
Model C (dependent variable ‘toxicology’ and independent variable ‘region’, adjusted by year).
The sex ratio was approximately 4:1, with rates of 20.9 cases/100,000 inhab. among males and 5.1/100,000 inhab. among females. There was an increase in the mortality rate among male victims in the Norte, Hortênsias and Alto Jacuí regions; and an increase among female victims in the Centro Sul and Paranhana-Encosta Serra regions (Table 1). When assessing the results by municipality (Table 2), in 2017 and 2018, the state capital and most populous city, Porto Alegre, had the highest number of victims. Mortality increased in the cities of Passo Fundo and Canoas, while it decreased in Rio Grande.
Table 2 - Absolute number, mortality rate (per 100,000 inhabitants) and rate ratio between sexes (male/female) in the eight municipalities with the highest number of suicide cases and highest suicide mortality rates, Rio Grande do Sul, 2017-2018
| Municipalities | 2017 | 2018 | ||||
|---|---|---|---|---|---|---|
| n | Sex Ratio | Sex Ratio | n | Sex Ratio | Sex Ratio | |
| Eight highest numbers of suicide cases | ||||||
| Porto Alegrea | 120 | 8.1 | 3.6 | 110 | 7.4 | 2.1 |
| Caxias do Sulb | 45 | 9.3 | 4.0 | 38 | 7.5 | 2.5 |
| Pelotasc | 43 | 12.5 | 2.9 | 34 | 9,9 | 3.6 |
| Santa Mariad | 34 | 12.2 | 4.7 | 26 | 9.3 | 2.3 |
| Rio Grandec | 30 | 14.3 | 4.0 | 16 | 7.6 | 4.3 |
| Canoasa | 28 | 8.1 | 2.1 | 36 | 10.4 | 2.0 |
| Passo Fundoe | 23 | 11.6 | 6.7 | 30 | 14.9 | 3.3 |
| Santa Cruz do Sulb | 23 | 18.0 | 6.7 | 21 | 16.2 | 3.2 |
| Eight highest suicide rates (per 100,000 inhab.) | ||||||
| André da Rochab | 2 | 153.1 | * | 1 | 75.5 | * |
| Santa Terezab | - | - | - | 2 | 115.3 | 1.0 |
| Carlos Gomese | 2 | 129.3 | * | - | - | - |
| Floriano Peixotoe | - | - | - | 2 | 111.4 | * |
| Esperança do Sule | 2 | 62.4 | * | 3 | 101.0 | 2.0 |
| São Domingos do Sule | 1 | 32.5 | * | 3 | 97.9 | * |
| Vale Verdeb | 4 | 115.6 | 3.0 | 1 | 28.7 | * |
| Almirante Tamandaré do Sule | 2 | 96,2 | * | - | - | - |
a) Porto Alegre macro-region.
b) Caxias do Sul macro-region.
c) Pelotas macro-region.
d) Santa Maria macro-region.
e) Passo Fundo macro-region.
* All cases of the male sex.
The most prevalent age range among male victims was the 50-54 years group, while the 50-59 years group was most prevalent among females (Figure 1).
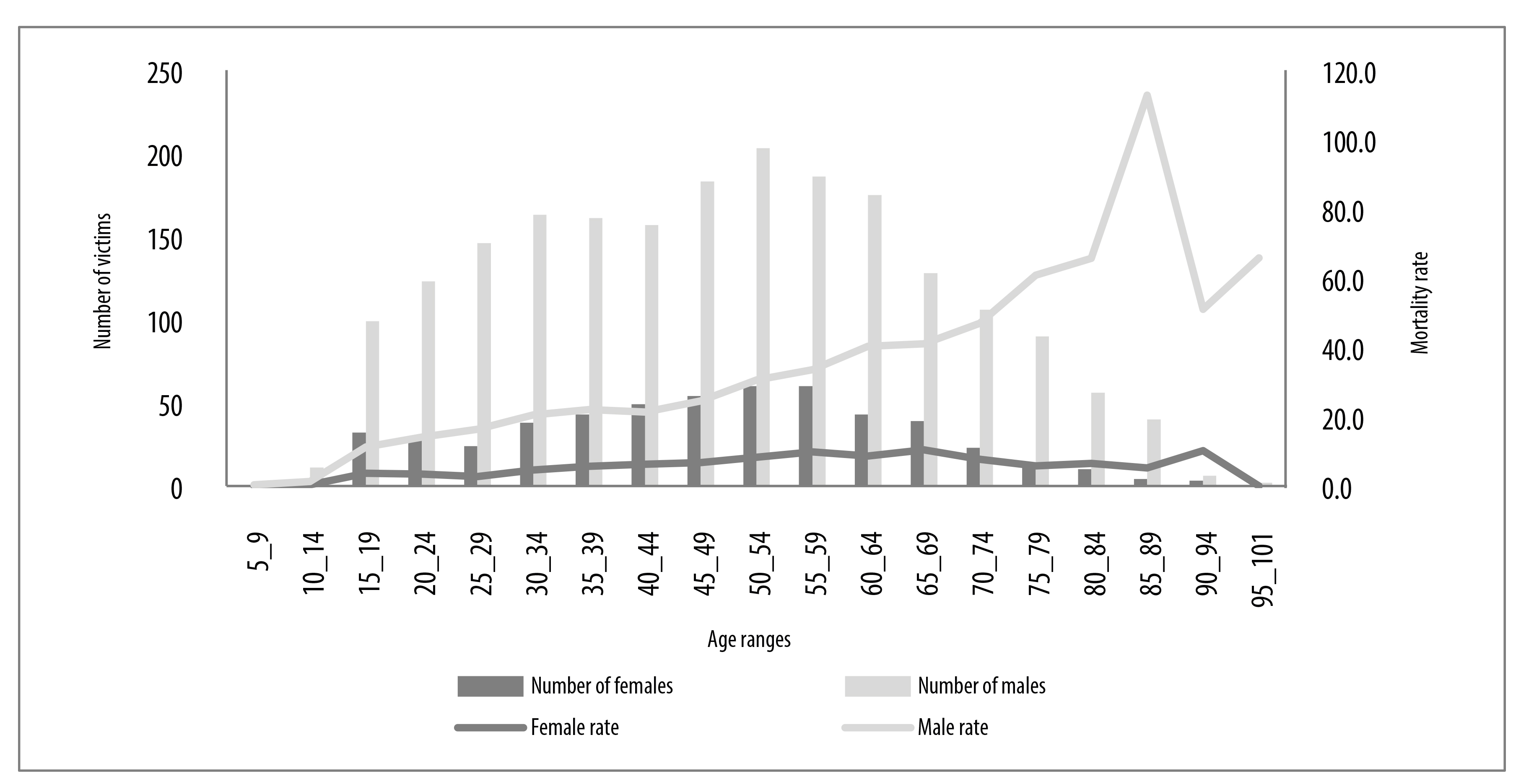
Figure 1 - Age distribution of suicide victims and suicide mortality rate (per 100,000 inhabitants) by sex, Rio Grande do Sul, 2017-2018
Nevertheless, the highest rates were found in the 85-89 group among males (112.8 cases/100,000 inhab.), and the 65-69 group among females (10.4 cases/100,000 inhab.). Between 2017 and 2018, there was an increase of 11.6% in the total number of female victims, 13.9% in the elderly age group and 21.1% in the frequency of cases involving parental absence. An increase - of 38.5% - was also found in the share of intoxication as a means of committing suicide (Table 3).
Table 3 - Suicide case distribution according to epidemiological and toxicological characteristics and odds ratios of associations estimated using logistic models, Rio Grande do Sul, 2017-2018
| Independent variables | Year | Dependent variables | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | Total | Ethanol (Model D) | Psychotropics (Model E) | Youth (Model F) | ||||||
| N | % | N | % | N | ORa (95%CIb) | N | ORa (95%CIb) | N | ORa (95%CIb) | N | |
| Sex | p<0.001 | p<0.001 | p=0.446 | ||||||||
| Male | 1,035 | 80.6 | 1,002 | 78.3 | 2.037 | Reference | 479 | 1.9 (1.4;2.4) | 443 | reference | 368 |
| Female | 249 | 19.4 | 278 | 21.7 | 527 | 2.0 (1.5;2.8) | 60 | Reference | 194 | 0.9 (0.6;1.2) | 85 |
| Age (in years) | p<0.001 | p=0.010 | |||||||||
| Child (0-12) | 3 | 0.2 | 3 | 0.2 | 6 | - | - | - | - | - | - |
| Adolescent (13-18) | 58 | 4.5 | 48 | 3.8 | 106 | 3.3 (1.8;6.7) | 12 | 1.9 (1.2;3.4) | 23 | - | - |
| Adult (19-59) | 878 | 68.4 | 836 | 65.3 | 1,714 | Reference | 437 | Reference | 471 | - | - |
| Elderly (60 or more) | 345 | 26.9 | 393 | 30.7 | 738 | 2.3 (1.7;3.1) | 90 | 1.3 (1.0;1.6) | 143 | - | - |
| Parental absence | p=0.630 | p=0.444 | p<0.001 | ||||||||
| Absence | 76 | 5.9 | 92 | 7.2 | 168 | Reference | 34 | Reference | 37 | Reference | 43 |
| Presence | 1,208 | 94.1 | 1,188 | 92.8 | 2,396 | 0.9 (0.5;1.4) | 505 | 0.8 (0.5;1.3) | 600 | 2.4 (1.5;3.6) | 410 |
| Cause of death | p=0.194 | p<0.001 | p=0.370 | ||||||||
| Hanging | 941 | 73.3 | 916 | 71.6 | 1,857 | Reference | 406 | 5.7 (3.8;8.8) | 403 | Reference | 331 |
| Use of fire arm | 189 | 14.7 | 168 | 13.1 | 357 | 0.8 (0.6;1.1) | 80 | 7.6 (4.7;12.7) | 59 | 1.0 (0.7;1.5) | 55 |
| Intoxication | 78 | 6.1 | 108 | 8.5 | 186 | 1.0 (0.7;1.7) | 31 | reference | 126 | 0.8 (0.5;1.3) | 35 |
| Jumping | 37 | 2.9 | 22 | 1.7 | 59 | 2.1 (0.9;5.4) | 8 | 3.9 (1.9;8.2) | 20 | 0.6 (0.3;1.1) | 15 |
| Use of cold weapon | 21 | 1.6 | 22 | 1.7 | 43 | 1.8 (0.7;5.5) | 6 | 3.6 (1.6;8.4) | 14 | 1.9 (0.6;8.2) | 4 |
| Otherc | 18 | 1.4 | 43 | 3.4 | 61 | 1.1 (0.5;2.8) | 8 | 4.6 (2.0;10.8) | 15 | 0.7 (0.3;1.9) | 13 |
| Toxicology resultsd | |||||||||||
| Ethanol | p=0.743 | p=0.009 | |||||||||
| Positive | 283 | 30.9 | 256 | 27.3 | 539 | - | - | reference | 166 | 1.5 (1.1;2.0) | 100 |
| Negative | 632 | 69.1 | 682 | 72.7 | 1314 | - | - | 1.0 (0.7;1.2) | 434 | reference | 258 |
| No information | 369 | - | 342 | - | 711 | - | - | - | 37 | - | 95 |
| Ethanol + psychotropics | 75 | 29.4e | 91 | 38.6e | 166 | - | - | - | - | - | 39 |
| 29.3f | 26.4f | ||||||||||
| Psychotropics | p=0.009 | p=0.135 | |||||||||
| Positive | 268 | 31.2 | 369 | 40.7 | 637 | 1.8 (1.2;2.9) | 166 | - | - | reference | 126 |
| Negative | 590 | 68.8 | 537 | 59.3 | 1127 | reference | 325 | - | - | 0.7 (0.4;1.1) | 218 |
| No information | 426 | - | 374 | - | 800 | - | 48 | - | - | - | 109 |
| Anxiolytics | p=0.817 | p=0.012 | |||||||||
| Positive | 108 | 40.3 | 145 | 39.3 | 253 | reference | 52 | - | - | 1.9 (1.2;3.3) | 31 |
| Negative | 750 | - | 761 | - | 1511 | 1.0 (0.7;1.7) | 439 | - | - | reference | 313 |
| Antidepressants | p=0.501 | p=0.637 | |||||||||
| Positive | 63 | 23.5 | 126 | 34.1 | 189 | 1.2 (0.7;2.0) | 29 | - | - | 1.1 (0.6;2.0) | 27 |
| Negative | 795 | - | 780 | - | 1575 | reference | 463 | - | - | reference | 317 |
| Illicit compounds | p<0.001 | p<0.001 | |||||||||
| Positive | 92 | 34.3 | 99 | 26.8 | 191 | reference | 98 | - | - | reference | 72 |
| Negative | 766 | - | 807 | - | 1573 | 3.7 (2.3;6.0) | 393 | - | - | 4.5 (2.7;7.7) | 272 |
a) OR: odds ratio.
b) 95%CI; 95% confidence interval.
c) Drowning, burning, traffic accident, cerebral trauma, electrocution and blunt instrument.
d) Main toxicology findings.
e) In relation to total positive results for ethanol.
f) In relation to total positive results for other psychotropics.
Notes:
Model D:
Dependent variable: ethanol.
Independent variables: sex; age; parental absence; cause of death; psychotropics; anxiolytics; antidepressants; illicit compounds.
Modelo E:
Dependent variable: psychotropics.
Independent variables: sex; age; parental absence; cause of death; ethanol.
Modelo F:
Dependent variable: youth (15-29 years).
Independent variables: sex; parental absence; cause of death; ethanol; psychotropics; anxiolytics; antidepressants; illicit compounds.
Hanging corresponded to 72.5% of cases, followed by use of firearms (13.9%), intoxication (7.3%), jumping (2.3%), use of cold weapons (1.7%) and other means, including drowning, burning, traffic accident, cerebral trauma, electrocution and use of blunt instruments. No association was found between cause of death and presence of ethanol (p=0.194) nor with the fact of being youths (p=0.370). The odds ratio of the presence of a psychoactive compound was 7.6 (95%CI 4.7;12.7) among victims who committed suicide via intoxication, compared to those who used firearms (Table 3).
In the diagram shown in Figure 2, it can be seen that the categories ‘intoxication’, ‘female sex’, presence of ‘psychotropics’, ‘jumping’, negative results for ‘ethanol’ and belonging to the Pelotas macro-region fell into the same quadrant. Similarly, being of the ‘male sex’ was close to ‘firearm’; just as being in the Santa Maria macro-region was close to missing data on ‘ethanol’ and ‘psychotropics’. These results indicate possible associations between these parameters.

Note:
Categories located in the same quadrant and/or very close to each other indicate association, except when they are found in the central region of the diagram, where there is little influence of the respective parameter over the theme studied.
Figure 2 - Graphic representation of multiple correspondence analysis between the categories of the ‘psychotropics’, ‘ethanol’, ‘sex’, ‘parental absence’, ‘youth’, ‘macro-region’13 and ‘cause of death’ variables among suicide cases, Rio Grande do Sul, 2017-2018
Victims from the Nordeste region, compared to those from the Vale do Caí region, had 9.5 times more odds (95%CI 2.6;61.8) of being youths, i.e. in the 15-29 age group (Table 1); youths also had 4.5 times (95%CI 2.7;7.7) and 1.9 times (95%CI 1.2;3.3) more likelihood of being victims when results were positive for an illicit substance or negative for anxiolytics, respectively. No association was found between youth and sex (p=0.446), psychotropics (p=0.135) or antidepressants (p=0.637) (Table 3).
Absence of one of the parents on the birth certificate was found in the case of 168 victims, corresponding to 6.4% among females and 6.6% among males. There was association between parental absence and youth (p<0.001), with 2.4 times more likelihood (95%CI 1.5;3.6) of victims being 15-29 years old when only one of the parents was present (Table 3). On the other hand, there was no association between parental absence and ethanol (p=0.630) or other psychotropic drugs (p=0.444).
With regard to toxicological examinations, deaths from suicide in RS between 2017 and 2018 required a total of 4,288 specialized analyses of biological samples collected from 1,996 victims. The number of examined cases that were not submitted to laboratory assessments reduced from one year to the other, although they continued corresponding to a high percentage (n=568; 22.2%) of cases. Association was found (p<0.001) between lack of biological sample collection and region (Table 1). There was a 17.0 times increase (95%CI 10.6;27.9) in the likelihood of absence of requested toxicology examinations in the Central region, when compared to the Metropolitana Delta do Jacuí region. Presence of ethanol was detected in 29.1% (n=539) of samples sent for analysis (n=915 in 2017; 938 in 2018). As can be seen in Figure 2 and in Table 3, there was association between alcohol consumption and sex (p<0001). Ethanol was found to be more present among male victims, compared to female victims (OR=2.0 - 95%CI 1.5;2.8).
Despite the number of positive ethanol results having reduced between 2017 and 2018, there was an increase in its mean concentration in both sexes. Among male victims, mean ethanol concentration increased from 14.6dg/L (2017) to 15.0 (2018), while among female victims, it increased from 10.4dg/L (2017) to 11.6 (2018). Moreover, the odds ratio of presence of alcohol among adolescents and the elderly, when compared to adults, was de 3.3 (95%CI 1.8;6.7) and 2.3 (95%CI 1.7;3.1) respectively (Table 3).
Furthermore, there was significant association between illicit compounds (p<0.001) and absence of psychotropics (p=0.009). Other psychotropic substances were detected in 36.1% (n=637) of samples analyzed with this purpose (n=858 in 2017 and n=906 in 2018), whereby association with sex was found (p<0.001). There was a 1.9 times increase (95%CI 1.4;2.4) in the odds of presence of psychotropics among female victims in relation to male victims. Age was also found to be associated with intake of illicit compounds (p=0.010), with a 1.9 times increase (95%CI 1.2;3.4) in the odds of positive results for psychotropics among adult victims, compared to adolescents, and 1.3 times (95%CI 1.0;1.6) in relation to the elderly (Figure 2 and Table 3).
When considering detection of illicit compounds, positive results were nine times more frequent among male victims, with cocaine being identified in 173 cases, and tetrahydrocannabinol in 34 cases.
Simultaneous intake of ethanol and another psychoactive substance was found in 166 victims, whereby the proportion between males and females was 6:1, while 23.5% (n=39) of these cases involved youth (15-29 years old).
Poisons were detected in 10.6% (n=54) of samples sent for analysis with this purpose (n=115 in 2017; n=395 in 2018), and were associated (p<0.001) with the region. An increase of 17.4 times (95%CI 5.0;65.5) was found in the odds of presence of poison in victims from the Nordeste region, compared to those from the Metropolitano Delta do Jacuí region (Table 1).
Discussion
The profile of suicide victims in Rio Grande do Sul revealed predominance of the male sex, hanging as the main form of suicide and, in approximately one third of cases, presence of psychotropic compounds.
According to WHO, suicide mortality is classified as being low when there are fewer than 5 cases/100,000 inhab.; medium when there are 5 to 14 cases; high when there are 15 to 29 cases; and very high when there are 30 or more deaths per 100,000 inhab.4 As such, the rates found in RS are considered high. However, use of these rates needs to take into consideration that the existence of few cases gives rise to high rates in the case of municipalities with small populations.
The data obtained through this study suggest the need to target state health care actions to the Vale do Rio Pardo and Médio Alto Uruguai regions, as well as to the Fronteira Noroeste, Missões, Nordeste and Vale do Taquari regions, where rates are classified as high. The Nordeste region stood out with regard to frequency of young victims and use of poison and should therefore be an important target for preventive actions.
According to Malta et al.,2 risk of suicide is highest in the Southern region of Brazil, whereby RS is the state with the highest mortality rates and disability-adjusted life years (DALY). This indicator simultaneously measures the effect of mortality and the effect of health problems that affect people’s quality of life.16
In most of the world’s countries, including Brazil,1),(2),(4),(7),(8),(11),(16)-(19 suicide deaths affect males more, as seen in RS, although in Southern India, China, Cambodia and Vietnam, as well as in some Pacific Ocean islands, such as the Philippines, this proportion falls.2),(4),(7),(9),(10),(19),(20 Lower suicide frequency among women may be attributed to lower prevalence of alcoholism, religiousness, the condition of motherhood, condescending attitudes regarding roles socially expected of the female gender, early recognition of signs of risk of depression and mental illness, greater tendency to seek help at times of crisis and greater participation in social support networks.10
In this sense, with regard to committing suicide, anthropological studies have found evidence of the role of hanging in gaucho patriarchal culture. In rural communities, especially those of German origin, such problems have become worse as the capitalist process of production has advanced, with leasing and loss of small farming properties, indebtedness, rural exodus, dissolution of culture and moral values and, ultimately, anomy.10 Incidence of hanging as a means of committing suicide was similar to that described in other periods, other Brazilian states and also in other countries.4),(10),(11),(18),(19),(21
Among females, the highest suicide mortality rate in RS was found in the 65-69 years age group. In Brazil as a whole, the highest mortality rate from this cause among females occurred in the 40-59 years age group.11 The high rates found among elderly victims corroborate data published in several other studies.4),(11),(17 In China, for example, according to the National Mortality Surveillance System, between 2013 and 2014 the elderly accounted for 38.2% of all suicide cases, even though they only corresponded to 8.9% of the population.22
According to WHO, suicide is the second leading cause of death among youth (15-29 years).1),(4) Suicide mortality in this age range has increased in Australia, Canada, Kuwait, New Zealand, Sri Lanka and the United Kingdom (1997-1999).23 In Brazil, between 1979 and 1998, an increase in cases among young people in 11 state capitals was found, among which Porto Alegre and Curitiba accounted for the highest rates.23
Further studies are needed in order to understand the influence of other factors related to suicides among youth in RS, such as for example, absence of parents throughout the lives of victims, which was a parameter not assessed by this study.
Mental disorders and use of psychotropic substances have been responsible for two thirds of suicides worldwide,2),(10),(16),(19)-(21),(24),(25 corresponding, in 2010, to 22 million DALYs.16 The percentage found of samples containing ethanol echoes the data found by Gonçalves, Ponce & Leyton in the city of São Paulo, where not only one third of suicide cases was linked to alcohol intake; but also higher concentrations of alcoholic beverages were found in male victims in that city.18
Regulation of alcoholic beverage availability (taxation and control of prices, marketing and sales outlets) could have a positive impact on suicide rates if they were implanted in Brazil, as recommended by WHO.26
Higher prevalence of medication intake among female victims reaffirms conclusions of previous studies about suicide attempts in Fraiburgo, a municipality located in the midwest of Santa Catarina, a state neighboring RS, between 2014 and 2017, in Mato Grosso state between 2008 and 2013, and in Minas Gerais state between 1997 and 2012.27
With regard to the study’s limitations, underreporting needs to be highlighted. Incidence of these occurrences in RS may be even greater, as it is not uncommon for death from suicide to be concealed due to family embarrassment in the face of the impact of the fact.10 In addition these is also the social impact of a problem that involves, on average, 5 to 6 people close to the victim, with regard to possible emotional and economic consequences.6),(24
Despite the importance of toxicological assessments in suicide cases, the results obtained revealed shortcomings as to standardization of forensic medicine procedures involving collection of biological samples, especially in the Central region which is part of the Santa Maria macro-region. This difficulty has also been reported in another study conducted in the city of São Paulo, where only 38.8% of suicide deaths were submitted to laboratory analyses.28 Whether or not obtaining significant associations through laboratory tests necessarily implies a causal relationship between the variables involved and the outcome of suicide, nevertheless we suggest that this association should be investigated.
With effect from April 2018, the DPL/IGP-RS Toxicology Division increased its whole blood analyses to include poisons and psychotropics (in addition to ethanol). As such, the higher number of positive results found between 2017 and 2018 (Table 3) may not have resulted from higher intake on the part of victims but rather from the amount of examinations performed.
As suicide results from a complex psychological, genetic, cultural and socio-environmental interaction,2),(10),(19),(24 multidisciplinary approaches need to be used, while respecting regional circumstances.7),(29 Data needs to be gathered continually, especially in low- and middle-income countries,4),(7 in order to strengthen effective strategies and redirect ineffective strategies.
Existing programs can serve as guidance, such as ‘Preventing Suicides’, in England, the National Suicide Prevention Plan 2015-2020, in Guiana, the National Mental Health and Suicide Prevention Policy, in Fiji, and the ‘Life Project’ in the Brazilian state of Santa Catarina. Notwithstanding, care must be taken not to apply procedures that work in other contexts without first testing them in the local reality.7),(27
Some initiatives have already been implemented in RS. In 2019, an intersectoral guide was prepared about suicidal behavior among children and adolescents, aimed at Education, Social Work, Health and Public Security professionals.30
Talking about the subject without alarmism and addressing social stigmas, raising awareness and encouraging suicide prevention through efficient interventions, based on secure data, can contribute to reversing the critical situation currently faced.11
The results of this study document not only the high rate of suicides in Rio Grande do Sul but also the profile of suicide victims, most of whom were male, chose hanging as the method and one third of whom were found to have used psychotropic drugs. Important relationships with parental absence and ethanol intake, as well as different affected age groups according to sex, have also been presented. While the reasons for the regional differences found require further research, they also indicate actions for monitoring more vulnerable groups and can inform health services regarding the formulation of preventive public policies.
Referências
1. World Health Organization. National suicide prevention strategies: progress, examples and indicators [Internet]. Geneva: World Health Organization; 2018 [cited 2019 Nov 04]. 74 p. Available from: Available from: https://apps.who.int/iris/bitstream/handle/10665/279765/9789241515016-eng.pdf?ua=1 [ Links ]
2. Malta DC, Minayo MCS, Soares Filho AM, Silva MMA, Montenegro MMS, Ladeira RM, et al. Mortalidade e anos de vida perdidos por violências interpessoais e autoprovocadas no Brasil e Estados: análise das estimativas do Estudo Carga Global de Doença, 1990 e 2015. Rev Bras Epidemiol [Internet]. 2017 maio [citado 2020 mar 4];20 Suppl 1:142-56. Disponível em: Disponível em: https://doi.org/10.1590/1980-5497201700050012 [ Links ]
3. Organización Panamericana de la Salud. Organización Mundial de la Salud. Prevención de la conducta suicida [Internet]. Washington: Organización Panamericana de la Salud; 2016 [citado 2019 nov 04]. 98 p. Disponível em: Disponível em: http://iris.paho.org/xmlui/bitstream/handle/123456789/31167/9789275319192-spa.pdf?sequence=1&isAllowed=y [ Links ]
4. Botti NCL, Veríssimo DS, Souza ED, Souza GN, Diniz IA, Campos LG, et al. Suicídio em infográficos: coletânea de infografia temática. Divinópolis: UFSJ; 2019. 120 p. [ Links ]
5. World Health Organization. Mental health action plan 2013-2020 [Internet]. Geneva: World Health Organization; 2013 [cited 2019 Nov 04]. 50 p. Available from: Available from: https://apps.who.int/iris/bitstream/handle/10665/89966/9789241506021_eng.pdf?sequence=1 [ Links ]
6. World Health Organization. Suicide prevention [Internet]. Geneva: World Health Organization; 2018 [cited 2019 Nov 04]. Available from: Available from: http:// https://www.who.int/health-topics/suicide#tab=tab_1 [ Links ]
7. Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ [Internet]. 2019 Feb [cited 2020 Mar 4];364:l94. Available from: Available from: https://doi.org/10.1136/bmj.l94 [ Links ]
8. Dantas AP, Azevedo UM, Nunes AD, Amador AE, Marques MV, Barbosa IR. Analysis of suicide mortality in Brazil: spatial distribution and socioeconomic context. Rev Bras Psiquiatr [Internet]. 2018 Jan-Mar [cited 2020 Mar 4];40(1):12-18. Available from: Available from: https://doi.org/10.1590/1516-4446-2017-2241 [ Links ]
9. Governo do Estado do Rio Grande do Sul. Secretaria de Saúde. Centro Estadual de Vigilância em Saúde. Suicídio e tentativa de suicídio. Bol Vig Epidemiol [Internet]. 2018 set [citado 2020 mar 4];1(1):1-8. Disponível em: Disponível em: https://www.cevs.rs.gov.br/suicidio [ Links ]
10. Meneghel SN, Victora CG, Faria NMX, Carvalho LA, Falk JW. Características epidemiológicas do suicídio no Rio Grande do Sul. Rev Saúde Pública [Internet]. 2004 dez [citado 2020 mar 4];38(6):804-10. Disponível em: Disponível em: https://doi.org/10.1590/S0034-89102004000600008 [ Links ]
11. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Perfil epidemiológico das tentativas e óbitos por suicídio no Brasil e a rede de atenção à saúde. Bol Epidemiol [Internet]. 2017 [citado 2020 mar 4];48(30):1-14. Disponível em: Disponível em: http://portalarquivos.saude.gov.br/images/pdf/2017/setembro/21/2017-025-Perfil-epidemiologico-das-tentativas-e-obitos-por-suicidio-no-Brasil-e-a-rede-de-atencao-a-saude.pdf [ Links ]
12. Instituto Brasileiro de Geografia e Estatística. Rio Grande do Sul [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 201- [cited 2019 dez 15]. Disponível em: Disponível em: https://cidades.ibge.gov.br/brasil/rs/pesquisa [ Links ]
13. Assembleia Legislativa do Estado do Rio Grande do Sul. Decreto nº 40 349, de 11 de outubro de 2000. Estabelece uma divisão territorial como referência para as estruturas administrativas regionais dos órgãos do Poder Executivo [Internet]. Porto Alegre (RS), 2000. Disponível em: http://www.al.rs.gov.br/legis/M010/M0100099.ASP?Hid_Tipo=TEXTO&Hid_TodasNormas=3517&hTexto=&Hid_IDNorma=3517 [ Links ]
14. Assembleia Legislativa do Estado do Rio Grande do Sul. Decreto nº 40 623, de 12 de fevereiro de 2001. Estabelece nova divisão territorial para o Instituto-Geral de Perícias [Internet]. Porto Alegre (RS), 2001. Disponível em: http://www.al.rs.gov.br/legis/M010/M0100099.ASP?Hid_Tipo=TEXTO&Hid_TodasNormas=2107&hTexto=&Hid_IDNorma=2107 [ Links ]
15. Souza AC, Bastos RR, Vieira MT. Análise de correspondência simples e múltipla para dados amostrais complexos. In: 19º Simpósio Nacional de Probabilidade e Estatística - Sinape [Internet]; 2010 jul 26-30; São Pedro (SP). São Pedro (SP): Sinape; 2010 [citado 2019 nov 4]. 6 p. Disponível em: Disponível em: http://www.ime.unicamp.br/sinape/sites/default/files/Artigo%20Sinape%20v2.pdf [ Links ]
16. Ferrari AJ, Norman RE, Freedman G, Baxter AJ, Pirkis JE, Harris MG, et al. The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the global burden of disease study. PLoS One [Internet]. 2014 Apr [cited 2020 Mar 4];9(4):e91936. Available from: Available from: https://doi.org/10.1371/journal.pone.0091936 [ Links ]
17. Martini M, Fonseca RC, Sousa MH, Farias IA, Cardoso TA, Kunz M, et al. Age and sex trends for suicide in Brazil between 2000 and 2016. Soc Psychiatry Psychiatr Epidemiol [Internet]. 2019 Jul [cited 2020 Mar 4];54(7):857-60. Available from: Available from: https://link.springer.com/article/10.1007%2Fs00127-019-01689-8 [ Links ]
18. Gonçalves REM, Ponce JC, Leyton V. Alcohol use by suicide victims in the city of Sao Paulo, Brazil, 2011-2015. J Forensic Leg Med [Internet]. 2018 Jan [cited 2020 Mar 4];53:68-72. Available from: Available from: https://doi.org/10.1016/j.jflm.2017.11.006 [ Links ]
19. Faria NMX, Victora CG, Meneghel SN, Carvalho LA, Falk JW. Suicide rates in the State of Rio Grande do Sul, Brazil: association with socioeconomic, cultural, and agricultural factors. Cad Saúde Pública [Internet]. 2006 Dec [cited 2020 Mar 4];22(12):2611-21. Available from: Available from: https://doi.org/10.1590/S0102-311X2006001200011 [ Links ]
20. World Health Organization. Preventing suicide: a global imperative [Internet]. Geneva: World Health Organization; 2014 [cited 2019 Nov 4]. 92 p. Available from: Available from: https://apps.who.int/iris/bitstream/handle/10665/131056/9789241564779_eng.pdf?sequence=1 [ Links ]
21. Zerbini T, Ponce JC, Sinagawa DM, Cintra RB, Munoz DR, Leyton V. Blood alcohol levels in suicide by hanging cases in the state of São Paulo, Brazil. J Forensic Leg Med [Internet]. 2012 Jul [cited 2020 Mar 4];19(5):294-6. Available from: Available from: https://doi.org/10.1016/j.jflm.2012.02.022 [ Links ]
22. Zhong BL, Chiu HF, Conwell Y. Rates and characteristics of elderly suicide in China, 2013-14. J Affect Disord [Internet]. 2016 Dec [cited 2020 Mar 4];206:273-9. Available from: Available from: https://doi.org/10.1016/j.jad.2016.09.003 [ Links ]
23. Werlang BSG, Borges VR, Fensterseifer L. Fatores de risco ou proteção para a presença de ideação suicida na adolescência. Interam J Psychol. 2005;39(2):259-66. [ Links ]
24. Associação Brasileira de Psiquiatria. Comissão de Estudos e Prevenção de Suicídio. Suicídio: informando para prevenir [Internet]. Brasília: CFM/ABP; 2014 [citado 2020 mar 4]. 52 p. Disponível em: Disponível em: https://www.cvv.org.br/wp-content/uploads/2017/05/suicidio_informado_para_prevenir_abp_2014.pdf [ Links ]
25. Zupanc T, Agius M, Paska A, Pregelj P. Blood alcohol concentration of suicide victims by partial hanging. J Forensic Leg Med [Internet]. 2013 Nov [cited 2020 Mar 4];20(8):976-9. Available from: Available from: https://doi.org/10.1016/j.jflm.2013.09.011 [ Links ]
26. World Health Organization. Global status report on alcohol and health 2018 [Internet]. Geneva: World Health Organization; 2018 [cited 2019 Nov 11]. 472 p. Available from: Available from: https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf?ua=1 [ Links ]
27. Rohling BSV, Ciesca D, Liebl G. Projeto Vida: integração da vigilância epidemiológica e setor da saúde mental frente às tentativas de suicídio em Fraiburgo, Santa Catarina, 2014-2017. Epidemiol Serv Saúde [Internet]. 2018 [citado 2020 mar 4];27(3):1-8. Disponível em: Disponível em: https://doi.org/10.5123/s1679-49742018000300014 [ Links ]
28. Cotrim BC, Chasin AAM. Blood alcohol content and death from fatal injury: a study in the metropolitan area of São Paulo, Brazil. J Psychoactive Drugs. 2000 Jul-Sep;32(3):269-75. [ Links ]
29. Centro de Valorização da Vida. Falando abertamente sobre suicídio [Internet]. São Paulo: Centro de Valorização da Vida; 2017 [citado 2019 nov 04]. 3 p. Disponível em: Disponível em: https://www.cvv.org.br/wp-content/uploads/2017/05/Falando-Abertamente-CVV-2017.pdf [ Links ]
30. Comitê Estadual de Promoção da Vida e Prevenção do Suicídio do Estado do Rio Grande do Sul. Guia intersetorial de prevenção do comportamento suicida em crianças e adolescentes [Internet]. Porto Alegre: Comitê Estadual de Promoção da Vida e Prevenção do Suicídio; 2019 [citado 2019 nov 04]. 36 p. Disponível em: Disponível em: https://saude.rs.gov.br/upload/arquivos/carga20190837/26173730-guia-intersetorial-de-prevencao-do-comportamento-suicida-em-criancas-e-adolescentes-2019.pdf [ Links ]
Received: December 17, 2019; Accepted: February 20, 2020











 texto em
texto em 


