Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.2 Brasília 2020 Epub 26-Mar-2020
http://dx.doi.org/10.5123/s1679-49742020000200002
RESEARCH NOTE
Dental auxiliary hepatitis B immunization: a cross-sectional study in the São Paulo state public health system, Brazil, 2018*
1Universidade Estadual Paulista, Faculdade de Odontologia de Araçatuba, Araçatuba, SP, Brazil
Objective:
to investigate dental auxiliaries (DA) hepatitis B immunization in Brazilian National Health System (SUS) services in nine cities in São Paulo State, Brazil, in 2018.
Methods:
this was a cross-sectional study based on interviews using a questionnaire as well as evaluation of immunity using the anti-HBs test, evaluation of prior testing, test result and interpretation and guidance provided about hepatitis B.
Results:
of the 70 registered DA, 35 completed the course of vaccinations, 29 had negative anti-HBs test results, 16 had tested previously, and 43 did not correctly understand their result; there was association (p=0.025) between completed course of vaccinations and receipt of guidance.
Conclusion:
most DA received guidance about hepatitis B; however, a considerable portion did not complete the course of vaccinations and had negative anti-HBs test results; few DA had tested previously nor correctly interpreted the result; evidence was found of an alarming scenario in which there are severe shortcomings in DA hepatitis B immunization.
Keywords: Cross-Sectional Studies; Occupational Health; Hepatitis B; Immunization; Dental Auxiliaries; Accidents, Occupational
Introduction
Hepatitis B virus (HBV) infection can result in liver tissue inflammation and lead to hepatocellular necrosis.1 According to the World Health Organization (WHO), viral forms of hepatitis caused 1.34 million deaths in 2015, representing a severe public health problem worldwide. It is estimated that 257 million people are living with chronic HBV infection, affecting mainly the WHO African Region and the Western Pacific Region.2
Within the realm of dentistry, HBV can spread through direct contact with blood, saliva and contaminated instruments.3 Dental auxiliaries stand out owing to their high susceptibility to HBV infection, this being inherent to their occupational exposure.4 In order for them to safely carry out the routine of waste disposal, dental instrument and equipment cleaning, disinfection and sterilization, as well as of the work environment itself, it is fundamental for these health workers to be informed about infection prevention methods.4,5
One of the most relevant prevention measures is taking the full course of vaccines: three doses of hepatitis B vaccine at zero, one and six months.6 Having an anti-HBs test is also recommended to confirm immunization based on checking antibody levels,7 given that it is possible for a person not to develop immunity even after having taken the recommended course of vaccines. A study conducted in 2015 with 340 individuals at a faculty of medicine in India found that 20% of those who had completed the course of vaccines were not protected.8 The test is safe, simple and quick; however, health professionals are still not very familiar with it.9,10
The aim of this study was to investigate hepatitis B immunization among dental auxiliaries (DAs) working in Brazilian National Health System (SUS) services in São Paulo state, Brazil, in 2018.
Methods
This was a cross-sectional study conducted in 2018, with DAs working in SUS services in nine cities in São Paulo state: Valparaíso, Bento de Abreu, Lavínia, Mirandópolis, Penápolis, Brejo Alegre, Alto Alegre, Clementina and Buritama. These cities fall within Regional Health Division II of the São Paulo State Health Department and are located in the northwest region of the state. They did not have Dental Specialty Centers at the time of the study.
DAs registered with the National Health Establishments Registry as working in primary healthcare centers in the cities were invited to take part in the study, since they were not on short-term or long-term leave or were not retired. Those who did not agree to having the anti-HBs test were excluded.
DAs were interviewed using a semi-structured questionnaire to assess for having had a complete course of hepatitis B vaccinations (yes; no; don’t know), having had an anti-HBs previously (yes; no) and interpretation of the results of previous anti-HBs tests.
The questionnaire also included questions about the following variables:
sex (male; female);
age group (in years: 20-35; 36-45; 46-55; 56 or over);
length of time working as a DA and length of time working as a civil servant (in years: 5 or less; 6-15; 16-25; 26 or over);
level of schooling (complete higher education; incomplete higher education; complete high school education);
occurrence of accident with sharps (yes; no); and
receipt of guidance about hepatitis B (yes; no).
The interviews were conducted at the primary healthcare centers in unoccupied rooms in order to avoid interruptions. Data on DAs from the same cities were collected on the same day in order to avoid them exchanging information about the study.
The anti-HBsAg® kit (Wama, Brazil) was used to check for immunity to HBV. Correct result interpretation was considered to be when a positive result was interpreted as meaning that the person was immune to hepatitis B. The anti-HBs tests were performed by a trained doctor. The interview/proposed questionnaire were tested in a pilot study conducted beforehand with a sample not included in the study, equivalent to 10% of the study sample.
Statistical analysis was performed using Epi InfoTM version 7.0. The results were presented according to distribution of absolute frequency; in the case of continuous variables, the average and the standard deviation were calculated. Pearson’s chi-square test and Fisher’s exact test were used to check for association between completed course of vaccinations, receipt of guidance, prior anti-HBs test and anti-HBs result. A 5% significance level was used.
The study project was approved by the Universidade Estadual Paulista Araçatuba Dental Faculty Permanent Human Research Ethics Committee (CEP/FOA/Unesp), as per Certification of Submission for Ethical Appraisal (CAAE) no 54227416.0.0000.5420) issued on June 29th 2018. The study was conducted in accordance with Ministry of Health National Health Council Resolution no 466, dated December 12th 2012. Participants signed a Free and Informed Consent form
Results
Of the total of 70 registered DAs, 63 agreed to take part in the study. DAs were predominantly female (n=58), in the 36-45 years age group (n=24) and their average age was 42 ± 12 years (Table 1); 27 had been working as DAs for a period of 6-15 years, or 12 ± 9 years on average, and 25 had been working as civil servants for the same period of time, or 13 ± 8 years on average.
Table 1 - Data on sociodemographic profile, length of time in the profession and accidents with sharps among Brazilian National Health System dental auxiliaries (N=63) in nine cities in São Paulo State, 2018
| Variable | N | ||
|---|---|---|---|
| Sex | |||
| Female | 58 | ||
| Male | 5 | ||
| Age group (in years) | |||
| 20-35 | 20 | ||
| 36-45 46-55 ≥56 | 24 13 6 | ||
| Length of time working as a dental auxiliary (in years) | |||
| ≤5 | 15 | ||
| 6-15 | 27 | ||
| 16-25 | 19 | ||
| ≥26 | 2 | ||
| Length of time working as a civil servant (in years) | |||
| ≤5 | 18 | ||
| 6-15 | 25 | ||
| 16-25 | 16 | ||
| ≥26 | 4 | ||
| Schooling | |||
| Complete higher education | 24 | ||
| Incomplete higher education | 12 | ||
| Complete high school education | 27 | ||
Just over half the DAs (n=35) had completed the full vaccination course (Figure 1). A large number (n=29) had a negative anti-HBs test result; the majority (n=47) had never had the test and only 20 knew the correct meaning of the test result. Moreover, the majority (n=32) had a history of accidents with sharps.
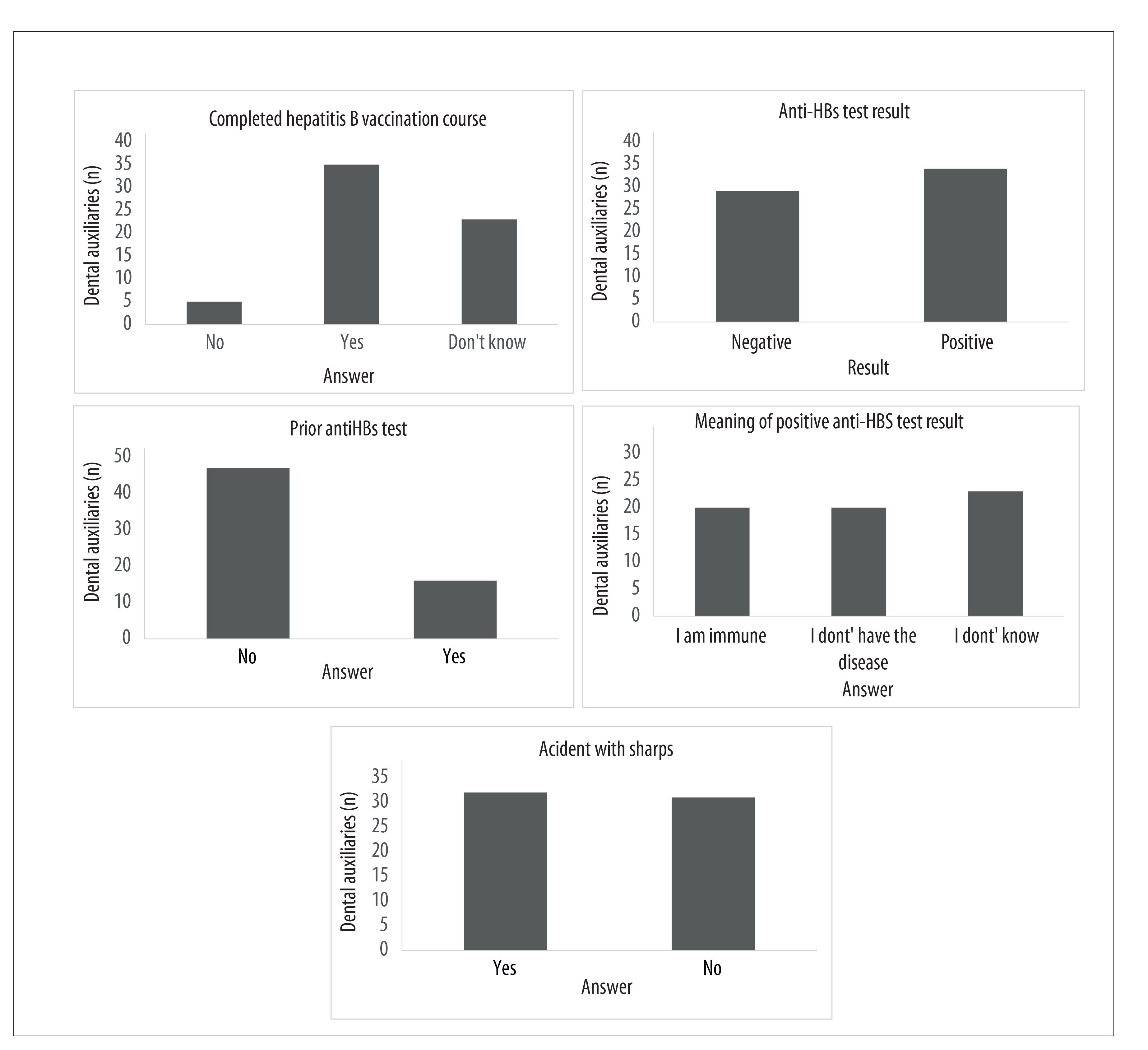
Figure 1 - Proportions of participants according to completed hepatitis B vaccination course, result, previous anti-HBs test and test result interpretation among Brazilian National Health System dental auxiliaries (N=63) in nine cities in São Paulo State, 2018
Association (p=0.025) was found between having taking the full course of vaccinations and receiving guidance about hepatitis B (Table 2). Completed course of vaccinations was found in 32/51 of DAs who had received guidance and in only 3/12 of those who had not received guidance.
Table 2 - Relation between completed hepatitis B vaccination course and the ‘anti-HBs test result’, ‘prior anti-HBs test’ and ‘receipt of guidance about hepatitis B’ variables among Brazilian National Health System dental auxiliaries (N=63) in nine cities in São Paulo State, 2018
| Variables | Completed vaccination course | ||||
|---|---|---|---|---|---|
| No | Yes | Total | P-value | ||
| n | n | n | |||
| Anti-HBs test result | |||||
| Negative | 14 | 15 | 29 | 0.756a | |
| Positive | 14 | 20 | 34 | ||
| Prior anti-HBs test | |||||
| No | 22 | 25 | 47 | 0.722a | |
| Yes | 6 | 10 | 16 | ||
| Receipt of guidance about hepatitis B | |||||
| No | 9 | 3 | 12 | 0.025b | |
| Yes | 19 | 32 | 51 | ||
a) Pearson’s chi-square test.
b) Fisher’s exact test.
Discussion
A considerable proportion of DAs had not taken a full course of vaccinations and had a negative anti-HB test result and, apart from not having tested previously, they interpreted their result incorrectly. The majority reported having had an accident with sharps at work and having received guidance about hepatitis B.
Findings indicate that prevalence of percutaneous lesions is higher among DAs than among dental surgeons.11,12 This fact may be related to disassembling, cleaning or discarding instruments, with risk of accidents event after the procedure is finished.
Almost half the DAs were not immunized against HBV. Studies conducted in high and middle-income countries have also found worrying indicators of dental professionals who were not immune to the virus.13,14 These findings reinforce the importance of developing strategies aimed at increasing vaccination prevalence and checking for immunity.15
The majority of the DAs had never had an anti-HBs test. Similar findings were identified by a study conducted by Garcia et al.16 with 289 dental surgeons and 104 dental auxiliaries in the municipality of Florianópolis, Santa Catarina State, Brazil, providing evidence that checking for immunity continues to be missing from prevention measures adopted systematically by oral health professionals. Lack of knowledge and lack of guidance result in low adherence to the procedure.5,17,18
The anti-HBs test checks for immunity to HBV. However, it can be confused with the test that identifies HBV infection. In this study, more than a quarter of DAs incorrectly interpreted the result, reporting that they did not have the disease when the test result was negative. The proportion of DAs who correctly interpreted the meaning of the test was smaller when compared to a recent study conducted by Garbin et al.19 with SUS dental surgeons (60%) in São Paulo State.
Association was found between having received guidance and taking a full course of vaccinations. Nevertheless, just over half the DAs had had all three vaccine doses. The high proportion of those who reported not knowing their vaccination coverage status is noteworthy. Absence of guidance and information about the need to take all three doses of the vaccine may compromise their being completely vaccinated, even though this vaccine is available free of change on the SUS.20-22
Lack of knowledge about the number of vaccine doses and the interval between each dose is prejudicial to vaccination completeness.21,22 These are factors capable of making someone forget to take all the dose or mistakenly believe that one or two doses are enough to ensure immunity.
No association was found between having a complete course of vaccines and the result of the anti-HBs test. Having a complete course of vaccines does not guarantee immunity and some individuals may continue to be exposed to risk of infection even after taking all three doses.8,23 This may arise from factors such as obesity, tobacco smoking, kidney failure, liver disease, immunosupression, inadequate vaccine administration and incorrect intervals between doses.23 It is also possible for the level of antibodies to decrease naturally over time and booster doses may be necessary.24
The sample being comprised only of DAs from São Paulo state is a limitation of the study, as different results may be found in public services in other places in the same state or elsewhere in the country. Moreover, excluding DAs who refused to have an anti-HBs could have influenced the results, if DAs who avoided this preventive action were the most vulnerable to the disease. Considering that not all dental auxiliaries are registered with the São Paulo Regional Dentistry Council, an important factor for the study was being able to invite all primary healthcare center DAs to take part in it, as long as they were registered with the National Health Establishments Registry.
The majority of DAs had received guidance about hepatitis B. However, a considerable part of them had not completed a full course of vaccines and had negative anti-HBs test results. Few DAs had tested previously and, of those who had tested, few of them were able to interpret the result correctly. An alarming scenario has been revealed, in which severe shortcomings in dental auxiliary hepatitis B immunization were found, making evident the need for actions and strategies that consolidate the adoption of vaccination coverage control and monitoring actions and systematic periodical checking of DAs immunity to hepatitis B.
REFERENCES
1. Chisari FV, Isogawa M, Wieland SF. Pathogenesis of hepatitis B virus infection. Pathol Biol (Paris) [Internet]. 2010 Feb [cited 2019 Nov 11];58(4):258-66. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2888709/ . doi: 10.1016/j.patbio.2009.11.001 [ Links ]
2. World Health Organization. Global hepatitis report 2017 [Internet]. Geneva: World Health Organization; 2017 [cited 2019 Nov 11]. 83 p. Available from: Available from: https://www.who.int/hepatitis/publications/global-hepatitis-report2017/en/ [ Links ]
3. Dahiya P, Kamal R, Sharma V, Kaur S. "Hepatitis" - prevention and management in dental practice. J Educ Health Promot [Internet]. 2015 May [cited 2019 Nov 11];4:33. Available from: Available from: http://www.jehp.net/article.asp?issn=2277-9531;year=2015;volume=4;issue=1;spage=33;epage=33;aulast=Dahiya . doi: 10.4103/2277-9531.157188 [ Links ]
4. Garbin CAS, Garbin AJI, Fagundes ACG, Santos RR, Gonçalves PE. Accidentes de trabajo que afectan los profesionales de la salud. Acta Odontol Venez [Internet]. 2009 [citado 2019 nov 11];47(1):92-101. Disponível em: Disponível em: http://190.169.30.98/ojs/index.php/rev_aov/article/view/179/155 [ Links ]
5. Rossato EM, Ferreira J. Acidentes com perfurocortantes e cobertura vacinal contra hepatite B entre trabalhadores da Saúde no Município de Santa Rosa, Estado do Rio Grande do Sul, Brasil, 2008. Epidemiol Serv Saúde [Internet]. 2012 jul-set [citado 2019 nov 11];21(3):487-96. Disponível em: Disponível em: http://scielo.iec.gov.br/pdf/ess/v21n3/v21n3a14.pdf . doi: 10.5123/S1679-49742012000300014 [ Links ]
6. Divisão de Imunização. Divisão de Hepatites. Centro de Vigilância Epidemiológica “Prof. Alexandre Vranjac”. Coordenadoria de Controle de Doenças. Secretaria de Estado da Saúde de São Paulo - DI/DH/CVE/CCD/SES-SP. Vacina contra hepatite B. Rev Saúde Pública [Internet]. 2006 dez [citado 2019 nov 11];40(6):1137-40. Disponível em: Disponível em: http://www.scielo.br/pdf/rsp/v40n6/26.pdf . doi: 10.1590/S0034-89102006000700026 [ Links ]
7. Resende VLS, Abreu MHG, Paiva SM, Teixeira R, Pordeus IA. Concerns regarding hepatitis B vaccination and post-vaccination test among Brazilian dentists. Virol J [Internet]. 2010 Jul [cited 2019 Nov 11];7:154. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2909964/ . doi: 10.1186/1743-422X-7-154 [ Links ]
8. Sahana HV, Sarala N, Prasad SR. Decrease in anti-hbs antibodies over time in medical students and healthcare workers after hepatitis b vaccination. Biomed Res Int [Internet]. 2017 Sep [cited 2019 Nov 11];2017:1327492. Available from: Available from: https://www.hindawi.com/journals/bmri/2017/1327492/ . doi: 10.1155/2017/1327492 [ Links ]
9. Garbin AJI, Wakayama B, Garbin CAS. Negligência no autocuidado em saúde: a imunização contra a Hepatite B na odontologia. Arch Health Invest [Internet]. 2016 [citado 2019 nov 11]; 5(2):85-9. Disponível em: Disponível em: http://www.archhealthinvestigation.com.br/ArcHI/article/view/1314/0 . doi: 10.21270/archi.v5i2.1314 [ Links ]
10. Garbin AJI, Wakayama B, Ortega MM, Garbin CAS. Imunização contra a hepatite B e os acidentes ocupacionais: Importância do conhecimento na odontologia. Rev Saúde Pesq [Internet]. 2016 maio-ago [citado 2019 nov 11];9(2):343-8. Disponível em: Disponível em: http://periodicos.unicesumar.edu.br/index.php/saudpesq/article/viewFile/4738/2847 [ Links ]
11. Garcia LP, Blank VLG. Prevalência de exposições ocupacionais de cirurgiões-dentistas e auxiliares de consultório dentário a material biológico. Cad Saúde Pública [Internet]. 2006 jan [citado 2019 nov 11];22(1):97-108. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v22n1/11.pdf . doi: 10.1590/S0102-311X2006000100011 [ Links ]
12. Kerr SP, Blank LW. Percutaneous injuries among dental health care workers. Gen Dent. 1999 Mar-Apr;47(2):146-51. [ Links ]
13. Ammon A, Reichart PA, Pauli G, Petersen LR. Hepatitis B and C among Berlin dental personnel: incidence, risk factors, and effectiveness of barrier prevention measures. Epidemiol Infect [Internet]. 2000 Oct [cited 2019 Nov 11];125(2):407-13. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2869614/ . doi: 10.1017/s0950268899004537 [ Links ]
14. Sernia S, Ortis M, Antoniozzi T, Maffongelli E, La Torre G. Levels of anti-HBs antibody in HBV-vaccinated students enrolled in the faculty of medicine, dentistry and health professions of a large Italian university. BioMed Res Int [Internet]. 2015 Jan [cited 2019 Nov 11];2015:712020. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4299313/ . doi: 10.1155/2015/712020 [ Links ]
15. Lages AS, França EB, Freitas MIF. Profissionais de saúde no processo de vacinação contra hepatite B em duas unidades básicas de Belo Horizonte: uma avaliação qualitativa. Rev Bras Epidemiol [Internet]. 2013 jun [citado 2019 nov 11]16(2):364-75. Disponível em: Disponível em: http://www.scielo.br/pdf/rbepid/v16n2/1415-790X-rbepid-16-02-00364.pdf . doi: 10.1590/S1415-790X2013000200012 [ Links ]
16. Garcia LP, Blank VLG, Blank N. Aderência a medidas de proteção individual contra a hepatite B entre cirurgiões-dentistas e auxiliares de consultório dentário. Rev Bras Epidemiol [Internet]. 2007 dez [citado 2019 nov 11];10(4):525-36. Disponível em: Disponível em: https://www.scielosp.org/pdf/rbepid/2007.v10n4/525-535 . doi: 10.1590/S1415-790X2007000400011 [ Links ]
17. Garcia LP, Facchini LA. Vacinação contra a hepatite B entre trabalhadores da atenção básica à saúde. Cad Saúde Pública [Internet]. 2008 maio [citado 2019 nov 11];24(5):1130-40. Disponível em: Disponível em: http://www.scielo.br/pdf/csp/v24n5/20.pdf . doi: 10.1590/S0102-311X2008000500020 [ Links ]
18. Batista SMF, Andreasi MAS, Borges AMT, Lindenberg ASC, Silva AL, Fernandes TD, et al. Seropositivity for hepatitis B virus, vaccination coverage, and vaccine response in dentists from Campo Grande, Mato Grosso do Sul, Brazil. Mem Inst Oswaldo Cruz [Internet]. 2006 May [cited 2019 Nov 11];101(3):263-7. Available from: Available from: http://www.scielo.br/pdf/mioc/v101n3/v101n3a06.pdf . doi: 10.1590/S0074-02762006000300006 [ Links ]
19. Garbin CAS, Vanzo KLT, Moimaz SAS, Garbin AJI, Chiba FY. Vaccination coverage and immunity against hepatitis B in public health dentists. Rev Soc Bras Med Trop [Internet]. 2019 Jun [cited 2019 Nov 11];52:e20180534. Available from: Available from: http://www.scielo.br/pdf/rsbmt/v52/1678-9849-rsbmt-52-e20180534.pdf . doi: 10.1590/0037-8682-0534-2018 [ Links ]
20. Assunção AA, Araújo TM, Ribeiro RBN, Oliveira SVS. Hepatitis B vaccination and occupation exposure in the healthcare sector in Belo Horizonte, Southeastern Brazil. Rev Saúde Pública [Internet]. 2012 Aug [cited 2019 Nov 11];46(4):665-73. Available from: Available from: http://www.scielo.br/pdf/rsp/v46n4/en_aop3554.pdf . doi: 10.1590/S0034-89102012005000042 [ Links ]
21. Francisco PMSB, Donalisio MR, Gabriel FJO, Barros MBA. Hepatitis B vaccination in adolescentes living in Campinas, São Paulo, Brazil. Rev Bras Epidemiol [Internet]. 2015 Sep [cited 2019 Nov 11];18(3):552-67. Available from: Available from: http://www.scielo.br/pdf/rbepid/v18n3/1415-790X-rbepid-18-03-00552.pdf . doi: 10.1590/1980-5497201500030003 [ Links ]
22. Ferreira RC, Guimarães ALS, Pereira RD, Andrade RM, Xavier RP, Martins AMEBL. Vacinação contra hepatite B e fatores associados entre cirurgiões-dentistas. Rev Bras Epidemiol [Internet]. 2012 jun [citado 2019 nov 11];15(2):315-23. Disponível em: Disponível em: http://www.scielo.br/pdf/rbepid/v15n2/09.pdf . doi: 10.1590/S1415-790X2012000200009 [ Links ]
23. Batra V, Goswami A, Dadhich S, Kothari D, Bhargava N. Hepatitis B immunization in healthcare workers. Ann Gastroenterol [Internet]. 2015 Apr-Jun [cited 2019 Nov 11];28(2):276-80. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367220/ [ Links ]
24. Arias-Moliz MT, Rojas L, Liébana-Cabanillas F, Bernal C, Castillo F, Rodríguez-Archilla A, et al. Serologic control against hepatitis B virus among dental students of the University of Granada, Spain. Med Oral Patol Oral Cir Bucal [Internet]. 2015 Sep [cited 2019 Nov 11];20(5):e566-71. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4598925/ . doi: 10.4317/medoral.20579 [ Links ]
*Article derived from the Master’s Degree thesis entitled ‘Public health service worker hepatitis B vaccine coverage and immunity’, defended by Ketlin Lara Tosta Vanzo at the Preventive and Social Dentistry Postgraduate Program, Araçatuba Dental Faculty/Universidade Estadual Paulista ‘Júlio de Mesquita Filho’ (Unesp), in 2018. This study received financial support from the Coordination for the Improvement of Higher Education Personnel/Ministry of Education (CAPES/MEC), by means of a Master’s Degree scholarship (Funding code: 001) granted to Ketlin Lara Tosta Vanzo.
Received: April 09, 2019; Accepted: October 22, 2019











 texto em
texto em 


