Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.3 Brasília jun. 2020 Epub 03-Jun-2020
http://dx.doi.org/10.5123/s1679-49742020000300014
Original article
Completeness of yellow fever notification forms in the state of Espírito Santo, Brazil, 2017 *
1Universidade Federal do Espírito Santo, Programa de Pós-Graduação em Saúde Coletiva, Vitória, ES, Brazil
2Universidade Federal do Espírito Santo, Departamento de Geografia, Vitória, ES, Brazil
3Secretaria de Estado da Saúde do Espírito Santo, Vitória, ES, Brazil
Objective
to describe the completeness of data on yellow fever notification forms in the municipalities of the state of Espírito Santo, Brazil, in 2017.
Methods
this is a descriptive ecological study with data from the Notifiable Health Conditions Information System (SINAN); form completeness was categorized as poor (<70.0%), regular (70-89.9%) or excellent (≥90.0%); thematic maps were prepared.
Results
53.1% of the municipalities had poor or regular classification for many notification form variables, especially case Final Classification (57.1%), Confirmation/Dismissal Criterion (63.2%) and Closure Date (26.5%), which are required fields.
Conclusion
completeness was poor or regular for several variables, pointing to the need for a systematic assessment of information on yellow fever held on SINAN.
Key words: Yellow Fever; Epidemiology; Health Information Systems; Disease Notification; Ecological Studies
Introduction
Yellow fever is a vaccine-preventable acute febrile communicable disease, characterized by two distinct epidemiological transmission cycles: sylvatic and urban.1 Sylvatic yellow fever is considered to be an endemic disease in Brazil (Amazon Region) and Africa. Epidemic periods are occasionally recorded in the region outside of the Amazon, characterizing the disease’s reemergence in Brazil.2
In the sylvatic cycle, the disease is transmitted by mosquitoes which are active during the day and have strictly sylvatic habits. The Haemagogus and Sabethes genera are the most significant in Latin America.3 Non-human primates spread mosquito infection and disseminate the virus as they roam through the jungle.4 In the urban cycle, the disease is anthroponotic, the virus is transmitted between human beings and mosquitoes, predominantly of the Aedes aegypti genus, in urban areas.3
The current outbreak of the disease in humans in Brazil has occurred mainly in metropolitan regions where the Aedes aegypti vector is widespread to such an extent that there is risk of urban yellow fever being reintroduced.2
Besides Brazil, substantial yellow fever outbreaks have occurred in recent years in Angola and the Democratic Republic of the Congo. Alongside global distribution of the main urban vector, Aedes aegypti , infection has the potential to spread internationally, increasing the impact not just of yellow fever on the health of populations, but also the impact on the financial burden of national Public Health systems.
The yellow fever virus reemerged in December 2016 in the Southeast region of Brazil,5 causing the biggest outbreak of sylvatic yellow fever in Brazil since the period between 1934 and 1940, affecting mainly the states of the Southeast region, where population concentration is higher and there is a considerable rate of Aedes aegypti infestation.6 Above all the 2016/2017 epidemic involved the states of Minas Gerais, Espírito Santo, São Paulo and Rio de Janeiro. In 2017, the highest yellow fever incidence rates were recorded in Espírito Santo (6.3/100,000 inhabitants) and in Minas Gerais (2.2 cases/100,000 inhab.). Nationwide, 261 deaths were notified, with 33.6% lethality; in Espírito Santo there were 83 deaths and 32.9% lethality.8
In order to analyze and understand the true magnitude of that yellow fever epidemic, it is important to be able to count on a reliable and quality information system, with notification form fields filled in correctly with complete and up to date data. A low quality surveillance system restricts epidemiological analysis of the disease as well as the monitoring of its dynamics, compromising the adequate adoption of intervention measures to minimize the effects of an outbreak and its spreading to other regions.5
As such, the objective of this study was to describe the completeness of data on yellow fever notification forms in the municipalities of the state of Espírito Santo, Brazil, in 2017.
Methods
This study included all notification forms of suspected or confirmed yellow fever cases recorded by the municipal Health Departments in Espírito Santo in 2017. Duplicate notification forms were excluded.
The yellow fever investigation form has 70 fields to be filled in. In order to analyze data completeness, we selected required variables and key variables, in accordance with their epidemiological importance in relation to the disease. The required variables analyzed in this study were: final case classification, probable location of infection and case closure date. The key variables were: occupation, entomological and epizootic disease investigation data (occurrence of epizootic diseases, virus isolation in mosquitoes and presence of the Aedes aegypti mosquito in urban areas), signs and symptoms, non-specific tests and case confirmation/dismissal criterion. Completeness of the variables was defined according to the extent to which the respective information fields were filled in, with the exception of the ‘Unknown’ field.
For our analysis we used the ‘Data quality’ item of the document entitled Updated Guidelines for Evaluating Public Health Surveillance Systems, published by the United States Centers for Disease Control and Prevention (CDC), which reflects the completeness and validity of data recorded on Public Health surveillance systems.5 , 10 A direct and easy measurement for evaluating data quality consists of examining the percentage of epidemiological surveillance form items answered as ‘unknown’ or left blank.5
For better exemplification of the analysis and better visualization of the results, the completeness rates of the selected variables were stratified according to their completeness: poor, when less than 70% of the data was filled in for all cases; regular, with 70% to 89.9% filled in; and excellent when data was filled in for 90% or more of cases.13
First of all, the database was reorganized using Microsoft Excel, version 10. It was later included in Arcgis 10.3 software along with a digital grid containing geographical information about the state of Espírito Santo. The grid is available on the Brazilian Institute of Geography and Statistics (IBGE) website.14
Thematic maps were prepared of completeness of the filling in of the variable categories represented by the following notification form items: [32] Occupation; [33] Inform entomological and epizootic disease investigation data; [39] Signs and Symptoms; [45] Non-specific Tests; [57] Final Classification; [58] Confirmation/Dismissal criterion; and [70] Closure Date.
The notification form item used to inform entomological (mosquitoes) and epizootic disease investigation is comprised of three fields: Occurrence of Epizootic Diseases; Virus isolation in mosquitoes; Presence of the Aedes aegypti mosquito in urban areas. The completeness of this item was calculated by taking the average rates of these three fields.
The completeness rate of the Signs and Symptoms category was obtained by calculating the average of the rates for the following variables: Abdominal pain, Faget Sign, Signs of Hemorrhage and Renal Excretion Disorders.
The completeness of the Non-specific Tests category corresponded to the average rate of the fields used to record the following tests: total bilirubin, direct bilirubin and AST (TGO) and ALT (TGP) aminotransferase.
Finally we calculated the completeness of the variables relating to averages of the following rates: Final Classification, Confirmation/Dismissal Criterion and Closure Date. The results were shown in the form of a map of the state.
The study project was approved by the Human Research Ethics Committee of the Federal University of Espírito Santo Health Sciences Center (CEP/CCS/UFES) on June 26th2017: Certification of Submission for Ethical Appraisal (CAAE) No. 68580617.3.0000.5060; Opinion No. 2.137.234.
Results
In 2017, 858 suspected cases of yellow fever were notified in the state of Espírito Santo. Sixty-three notifications were duplicated and therefore removed. As such, 795 forms were studied. Confirmed yellow fever cases accounted for 26.9% of the investigation forms (N=214); while inclusive cases accounted for 36.4% (N=290).
With regard to suspected case distribution in 2017, these were notified in 49 of the state’s 78 municipalities. In particular, the state capital, Vitória, had 157 notifications (19.7%) ( Table 1 ).
Table 1 – Distribution of suspected sylvatic yellow fever cases by notifying municipality, Espírito Santo, Brazil, 2017
| Notifying municipality | N | % |
|---|---|---|
| Vitória | 157 | 19.7 |
| Serra | 99 | 12.4 |
| Colatina | 63 | 7.9 |
| Santa Leopoldina | 48 | 6.0 |
| Domingos Martins | 43 | 5.4 |
| Vila Velha | 42 | 5.3 |
| Ibatiba | 37 | 4.6 |
| Santa Maria de Jetibá | 30 | 3.7 |
| Cariacica | 24 | 3.0 |
| Laranja da Terra | 19 | 2.3 |
| Cachoeiro de Itapemirim | 17 | 2.1 |
| Itarana | 17 | 2.1 |
| Muniz Freire | 17 | 2.1 |
| Alfredo Chaves | 15 | 1.8 |
| Castelo | 14 | 1.7 |
| Baixo Guandu | 11 | 1.3 |
| Conceição do Castelo | 11 | 1.3 |
| Viana | 10 | 1.2 |
|
| ||
| Total for unlisted municipalities | 121 | 15.2 |
|
| ||
| Total for the state of Espírito Santo | 795 | 100.0 |
With regard to probable location of infection, confirmed cases were distributed over 34 municipalities, mainly concentrated in the state’s sierra region, especially in the municipalities of Domingos Martins and Marechal Floriano. The five municipalities that comprise the Greater Vitória metropolitan region recorded cases of yellow fever; but no autochthonous case was reported within the boundaries of the capital.
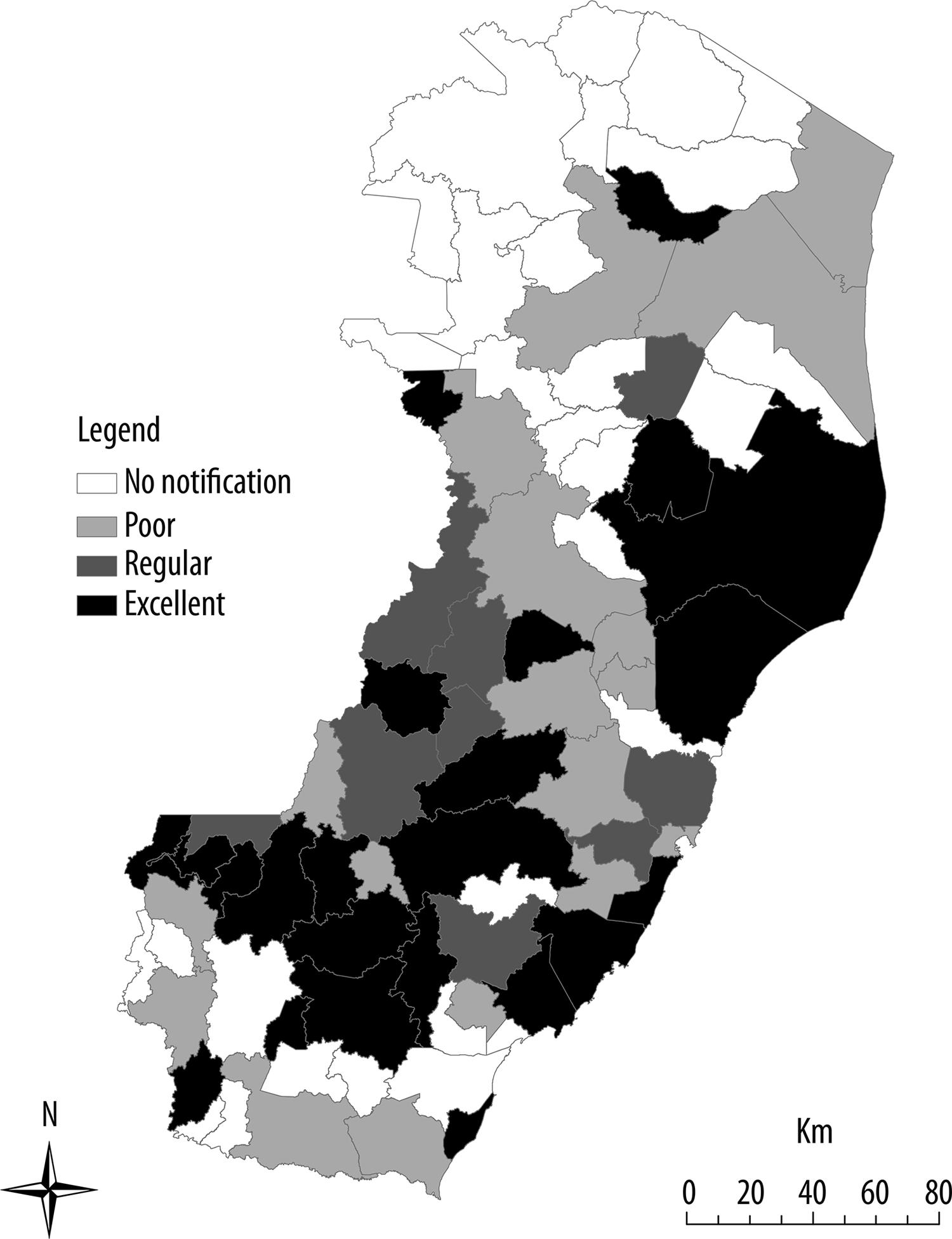
Figure 1 shows the map of yellow fever notification form completeness for the occupation, epidemiological precedents, signs and symptoms and non-specific test variables.
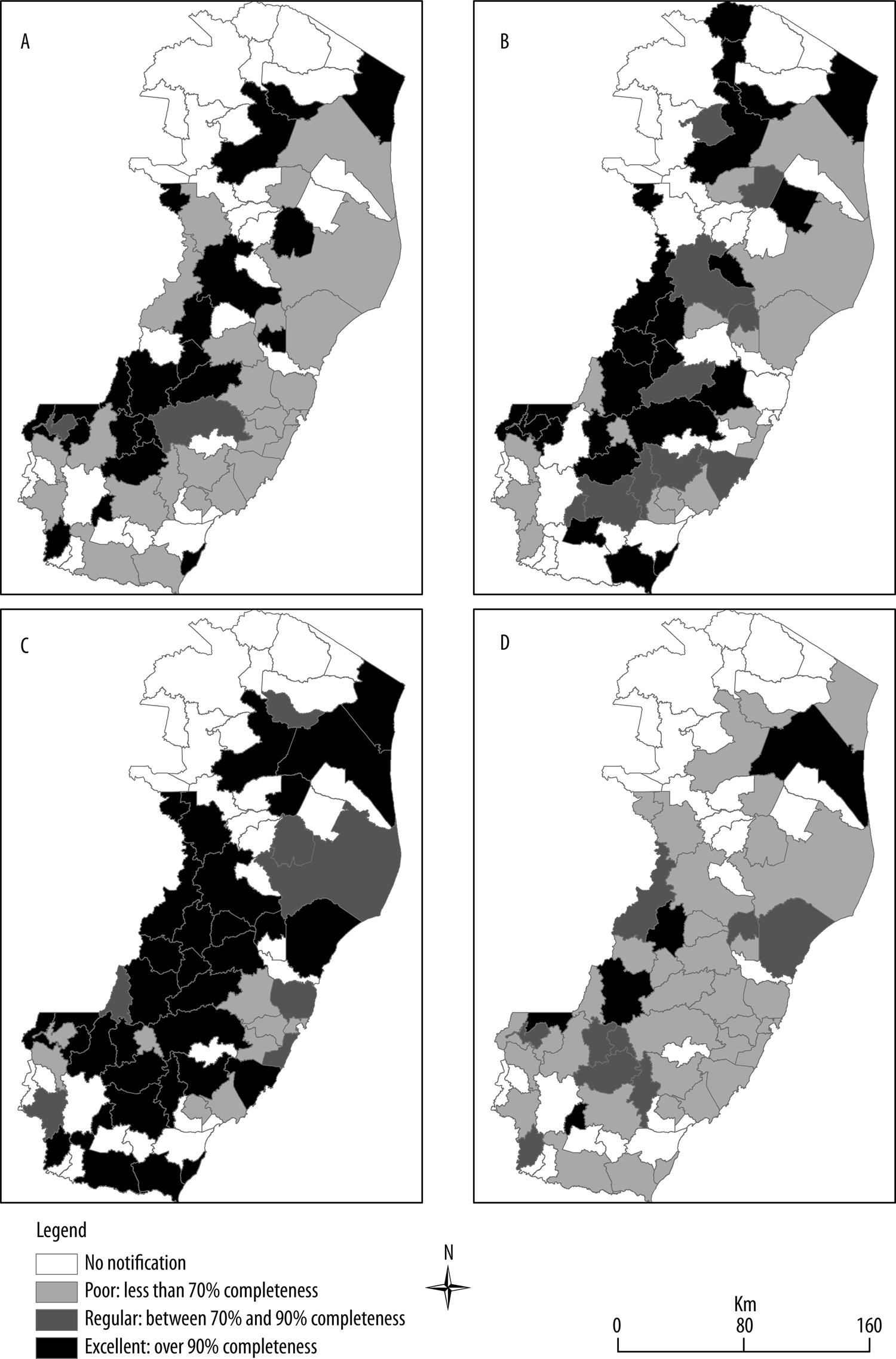
Figure 1 – Evaluation of completeness of the ‘A – occupation’, ‘B – epidemiological precedents’, ‘C – signs and symptoms’ and ‘D – non-specific test’ variables on yellow fever notification forms held on the Notifiable Health Conditions Information System, Espírito Santo, Brazil, 2017
Percentage completeness of the Occupation variable ( Figure 1A ) varied between poor and excellent. The average rating for the state as a whole was poor. The municipalities comprising the Greater Vitória metropolitan region and coastal municipalities were classified as having poor completeness; this variable was complete for 24 of the state’s 78 municipalities.
With regard to epidemiological precedents ( Figure 1B ), the municipalities that comprise the Greater Vitória metropolitan region were classified as having poor completeness of these data, except for Guarapari and Vila Velha which were classified as having regular completeness.
Thirty-three municipalities had excellent classification for the Signs and Symptoms category ( Figure 1C ), while completeness of this indicator was classified as poor for the state capital Vitória.
Thirty-seven of the state’s 78 municipalities had not filled in the variables relating to the completeness of the Non-specific Tests category ( Figure 1D ), which was therefore classified as poor. Only five municipalities were classified as having excellent completeness in this category: São Mateus (northern region of the state), Itaguaçu and Afonso Cláudio (metropolitan region of the capital Vitória), Ibatiba and Jerônimo Monteiro (southern region of the state).
Figure 2 shows how each municipality was classified (poor, regular or excellent) with regard to average completeness of case Final Classification, Confirmation/Dismissal Criterion and Closure Data variables. Twenty-six municipalities had either poor or regular completeness of the variables. The capital Vitória had poor completeness. Twenty-three of the state’s cities were classified as having excellent completeness, in particular in the southern region of the state where eleven municipalities were classified as excellent.
Discussion
The study found that classification of the municipalities of the state of Espírito Santo ranged between poor and regular for many of the notification form variables, in particular the state capital Vitória. With regard to the occupation, epidemiological precedents, signs and symptoms and non-specific test variables, completeness was poor in the municipalities comprising the metropolitan region of Vitória – except for Vila Velha and Guarapari with regard to epidemiological precedents.
The results also show duplication of suspected yellow fever case notification in the state. Inconclusive cases, for which it was not possible to confirm or dismiss yellow fever infection because of insufficient data, blank form fields, improperly filled in fields or because samples were not taken for diagnosis tests to be performed.
Completeness classified as ranging between poor and excellent was found for the occupation, signs and symptoms and non-specific tests variables. These are considered to be key variables although data input on the system is not mandatory for them.13 They are important variables for epidemiological analyses, identification of specific yellow fever characteristics and locating where the virus is circulating, as well as serving for calculating indicators.18 75.5% of the notifying municipalities did not fill in the data on non-specific tests. These are total and indirect bilirubin and AST (TGO) e ALT (TGP) aminotransferase tests. They are performed to check liver function, with the aim of detecting liver disease, performing differential diagnosis with other diseases, assessing the extent of liver tissue damage and guiding as to treatment.20
The Final Classification, Probable Location of Infection and Closure Date variables are necessary for closing cases and are fields that are required to be filled in, since when they are missing notification cannot be included on SINAN.12 The proportion of unknown and blank information was found to be high, so that completeness classification was between poor and regular. Given that these data are not collected at the beginning of case investigation, they need to be monitored in order for the fields to be filled in later. This passive data collection method can result in underreporting, late notification and late data input, problems with processing and transferring updated information and adequate feedback to the notifying source, consequently leading to discouragement and discontinuity in the surveillance process,20 whereas timely case closure provides knowledge as to confirmed and dismissed cases and enables control measures to be adopted.
A study published in the United Kingdom in 2018 about existing and potential yellow fever infection risk zones, found case underreporting and lack of knowledge of exact distribution of the disease. Infection control strategies require a quality database in order to identify populations most vulnerable to becoming ill.22
Poor and regular variable classification can arise from lack of motivation, lack of personnel or lack of time to fill in the notification form completely, because of priority being given to other demands in the notifying units. Another factor than can also be considered regarding incomplete filling in of notification forms is the fact of health workers seeing this activity as being merely bureaucratic and of secondary importance16 A further possible motive for justifying yellow fever notification form field incompleteness in Espírito Santo could be the fact of the state having been considered to be free from yellow fever virus circulation,9 and therefore having health personnel who, because of lack of knowledge about notification, diagnosis methods, signs and symptoms of the disease, were not prepared to cope with an epidemic of the magnitude seen between 2016 and 2017.
Duplicated cases tend to occur on health information systems because of the same event being notified by different units and lack of notification monitoring. The existence of these cases on the SINAN system can lead to overestimation and apparent increased incidence of the disease.12
On the other hand, case underreporting is attributed to a variety of factors, such as delayed notification and data input, problems with information processing and transfer, delays in tests results being made available, failure to update data or lack of adequate feedback to the notifying source, which can also result in discouragement and discontinuity of the process.17
Although this study reveals important findings for health surveillance and evaluation of health information quality, as well as for replication of the methods used to evaluate SINAN form completeness in other Brazilian states – and also for other health conditions –, it has a limitation which lies precisely in its regional characteristics which are peculiar to Espírito Santo and do not extend to other Brazilian states.
Geospatial analysis and mapping are known to be useful tools for detecting spatial patterns of diseases and associated factors, offering innovative possibilities for linking Public Health epidemiological data; and situating them and overlapping them geographically, thus facilitating visualization of statistical data over the territory.28
The results found on the Notifiable Health Conditions Information System about the spatial distribution of yellow fever demonstrate poor and regular completeness for several of the variables studied, pointing to the need for a systematic evaluation of the quality of the information generated by health information systems.
Analyses performed using poor quality data may not represent the true epidemiological profile of health conditions, to the detriment of the adoption of more adequate control measures and mapping of risk regions.10
Health professionals need to be trained and have their awareness raised as to (i) correctly filling in disease and health condition notification forms, not leaving fields blank or filling them in as ‘Unknown’, and to promote between each other (ii) understanding of the importance of this activity as not just being bureaucratic, given that it is through the epidemiological profile provided by health information systems that measures are adopted for prevention, resource distribution and implementing public policies in this area.
REFERENCES
1. Monath TP, Vasconcelos PFC. Yellow fever. J Clin Virol [Internet]. 2015 Mar [cited 2020 May 8];64:160-73. Available from: https://doi.org/10.1016/j.jcv.2014.08.030 [ Links ]
2. Klitling R, Gould EA, Paupy C, Lamballerie X. What does the future hold for yellow fever virus? Genes (Basel) [Internet]. 2018 Jun [cited 2020 May 8];9(6):291-318. Available from: https://doi.org/10.3390/genes9060291 [ Links ]
3. Jentes ES, Poumerol E, Gershman MD, Lemarchand J, Lewis RF, Wilder- Smith A, et al. The revised global yellow fever risk map and recommendations for vaccination, 2010: consensus of the Informal WHO working Group on Geographic Risk for yellow fever. Lancet Infect Dis [Internet]. 2011 Aug [cited 2020 May 8];11(8):622-32. https://doi.org/10.1016/S1473-3099(11)70147-5 [ Links ]
4. Veronesi R, Focaccia R. Tratado de infectologia. 4. Ed. Rio de Janeiro: Atheneu; 2010. [ Links ]
5. Klaucke DN, Buehler JW, Thacker SB, Parrish G, Trowbridge FL, Berkelman RL, Center for Diseases Control and Prevention. Guidelines for evaluating surveillance systems: recommendations from the guidelines working group. Morb Mortal Wkly Rep [Internet]. 1988 May [cited 2020 May 8];37(S-5):1-18. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/00001769.htm [ Links ]
6. World Health Organization - WHO. Yellow fever – Brazil [Internet]. Geneva: World Health Organization; 2017[cited 2017 Apr 3]. Available from: http://www.who.int/csr/don/06-march-2017-yellow-fever-brazil/en/ [ Links ]
7. Possas C, Lourenço-de-Oliveira R, Tauil PL, Pinheiro FP, Pissinatti A, Cunha RV, et al. Yellow fever outbreak in Brazil: the puzzle of rapid viral spread and challenges for immunisation. Mem Inst Oswaldo Cruz [Internet]. 2018 Sep [cited 2020 May 8];113(10):1-12. Available from: https://doi.org/10.1590/0074-02760180278 [ Links ]
8. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Monitoramento do período sazonal da febre amarela no Brasil 2017/2018: informe 10 [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2018 jan 25]. 13 p. Disponível em: https://portalarquivos2.saude.gov.br/images/pdf/2018/janeiro/25/af-informe-febre-amarela-10-25jan18.pdf [ Links ]
9. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Emergência epidemiológica de febre amarela no Brasil, no período de dezembro de 2016 a julho de 2017. Bol Epidemiol [Internet]. 2017 [citado 2019 fev 7];48(28):1-22. Disponível em: http://portalarquivos2.saude.gov.br/images/pdf/2017/setembro/06/2017_027.pdf [ Links ]
10. German RR, Westmoreland D, Armstrong G, Birkhead GS, Horan JM, Center for Diseases Control and Prevention, et al. Updated guidelines for evaluating public health surveillance systems: recommendations from the guidelines working group. Morb Mortal Wkly Rep [Internet]. 2001 Jul [cited 2020 May 8];50(RR13):1-35. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5013a1.htm [ Links ]
11. Barreto PA, Braga ALDS, Andrade M. Avaliação da completude dos registros de dengue: estudo exploratório das notificações compulsórias. Onl Braz J Nurs [Internet]. 2012 dez [citado 2020 maio 8];11(3):829-47. Disponível em: http://www.objnursing.uff.br/index.php/nursing/article/view/3920 [ Links ]
12. Cavalvante KRLJ, Tauil PL. Risco de reintrodução da febre amarela urbana no Brasil. Epidemiol Serv Saúde [Internet]. 2017 jul-set [citado 2020 maio 8];26(3):617-20. Disponível em: https://doi.org/10.5123/S1679-49742017000300018 [ Links ]
13. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Sistema de agravos de notificação – Sinan: normas e rotinas [Internet]. 2. ed. Brasília: Ministério da Saúde; 2007 [citado 2020 maio 8]. 68 p. Disponível em: https://bvsms.saude.gov.br/bvs/publicacoes/07_0098_M.pdf [ Links ]
14. Instituto Brasileiro de Geografia e Estatística. Malhas digitais: Espírito Santo [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2018 [citado 2018 jul 20]. Disponível em: https://downloads.ibge.gov.br/downloads_geociencias.htm [ Links ]
15. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância. Roteiro para uso do Sinan NET, análise da qualidade da base de dados e cálculo de indicadores epidemiológicos e operacionais [Internet]. Brasília: Ministério da Saúde; 2008 [citado 2019 fev 7]. 51 p. Disponível em: http://www.saude.ba.gov.br/wp-content/uploads/2017/12/Caderno-de-analise-EXANT.pdf [ Links ]
16. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Sinan relatórios: manual de operação [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2020 maio 8]. 124 p. Disponível em: https://portalsinan.saude.gov.br/images/documentos/Aplicativos/relatorios/Manual%20de%20Operacao%20SINAN%20Relatorios%20-%20versao_4.8.pdf [ Links ]
17. Duarte HHP, França EB. Qualidade dos dados da vigilância epidemiológica da dengue em Belo Horizonte, MG. Rev Saúde Pública [Internet]. 2006 fev [citado 2020 maio 8];40(1):134-42. Disponível em: https://doi.org/10.1590/S0034-89102006000100021 [ Links ]
18. Hamrick PN, Aldighieris S, Machado G, Leonel DG, Vilca LM, Uriona S, et al. Geographic patterns and environmental factors associated with human yellow fever presence in the Americas. PLoS Negl Trop Dis [Internet]. 2017 Sep [cited 2020 May 8];11(9):1-27. Available from: https://doi.org/10.1371/journal.pntd.0005897 [ Links ]
19. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Instrucional de preenchimento da ficha de notificação/investigação: febre amarela instruções para preenchimento ficha de investigação – Sinan NET [Internet]. Brasília: Ministério da Saúde; 2006 [citado 2019 jan 20]. Disponível em: http://portalsinan.saude.gov.br/images/documentos/Agravos/Febre%20Amarela/Febre_Amarela_v5_instr.pdf [ Links ]
20. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Guia de vigilância em saúde: volume 2 [Internet]. Brasília: Ministério da Saúde; 2017 [citado 2020 maio 8]. 3 v. Disponível em: https://bvsms.saude.gov.br/bvs/publicacoes/guia_vigilancia_saude_volume_2.pdf [ Links ]
21. Barbosa JR, Barrado JCS, Zara ALSA, Siqueira Júnior JB. Avaliação da qualidade dos dados, valor preditivo positivo, oportunidade e representatividade do sistema de vigilância epidemiológica da dengue no Brasil, 2005 a 2009. Epidemiol Serv Saúde [Internet]. 2015 jan-mar [citado 2020 maio 8];24(1):49-58. Disponível em: https://doi.org/10.5123/S1679-49742015000100006 [ Links ]
22. Schearer FM, Longbottom J, Browne AJ, Pigott DM, Brady OJ, Kraemer MUG, et al. Existing and potential infection risk zones of yellow fever worldwide: a modelling analysis. Lancet [Internet]. 2018 Mar [cited 2020 May 8];6(3):E270-78. Available from: https://doi.org/10.1016/S2214-109X(18)30024-X [ Links ]
23. Marques CA, Siqueira MM, Portugal FB. Avaliação da não completude das notificações compulsórias de dengue registradas por município de pequeno porte no Brasil. Ciênc Saúde Coletiva [Internet]. 2020 mar [citado 2020 jan 6];25(3):891-900. Disponível em: https://doi.org/10.1590/1413-81232020253.16162018 [ Links ]
24. Goldani LZ. Yellow fever outbreak in Brazil, 2017. Braz J Infect Dis [Internet]. 2017 Mar-Apr [cited 2020 May 8];21(2):123-6. Available from: https://doi.org/10.1016/j.bjid.2017.02.004 [ Links ]
25. Rezende IMD, Sacchetto L, Mello EMD, Alves PA, Iani FCDM, Adelino TER, et al. Persistence of yellow fever virus outside the Amazon basin, causing epidemics in Southeast Brazil, form 2016 to 2018. PLoS Negl Trop Dis [Internet]. 2018 Jun [cited 2020 May 8];12(6):e0006538. Available from: https://doi.org/10.1371/journal.pntd.0006538 [ Links ]
26. Silva GDM, Bartholomay P, Cruz OG, Garcia LP. Avaliação da qualidade dos dados, oportunidade e aceitabilidade da vigilância da tuberculose nas microregiões do Brasil. Ciênc Saúde Coletiva [Internet]. 2017 out [citado 2020 maio 8];22(10):3307-19. Disponível em: http://dx.doi.org/10.1590/1413-812320172210.18032017 [ Links ]
27. Meirelles MQB, Lopes AKB, Lima KC. Vigilância epidemiológica de HIV/Aids em gestantes: uma avaliação acerca da qualidade da informação disponível. Rev Panam Salud Pública [Internet]. 2016 dez [citado 2020 maio 8];40(6):427-34. Disponível em: https://www.scielosp.org/article/rpsp/2016.v40n6/427-434/ [ Links ]
28. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. sistema de informação de agravos de notificação: dicionário de dados – Sinan NET – Versão 5.0 [Internet]. Brasília: Ministério da saúde; 2010 [citado 2019 jan 20]. Disponível em: http://portalsinan.saude.gov.br/images/documentos/Agravos/Febre%20Amarela/DIC_DADOS_Febre_Amarela_v5.pdf [ Links ]
*Manuscript based on the Master’s Degree dissertation by Priscila Carminati Siqueira, entitled ‘Spatial analysis of notified yellow fever cases in the state of Espírito Santo’, defended at the Federal University of Espírito Santo (UFES) Public Health Postgraduate Program in 2019.
Associate Editor: Bruno Pereira Nunes - orcid.org/0000-0002-4496-4122
Received: October 21, 2019; Accepted: April 14, 2020











 texto en
texto en