Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.3 Brasília jun. 2020 Epub 03-Jun-2020
http://dx.doi.org/10.5123/s1679-49742020000300012
Original article
Activity limitation and social participation restriction of people with leprosy: a cross-sectional analysis of magnitude and associated factors in a hyperendemic municipality in the state of Piauí, Brazil, 2001-2014 *
1Universidade Federal do Ceará, Faculdade de Medicina, Fortaleza, CE, Brazil
2Universidade Federal do Piauí, Campus Ministro Petrônio Portela, Teresina, PI, Brazil
3Universidade Federal do Piauí, Campus Senador Helvídio Nunes de Barros, Picos, PI, Brazil
4Secretaria Municipal de Saúde, Coordenação do Programa de Controle da Hanseníase, Picos, PI, Brazil
Objective
to analyse the magnitude and factors associated with activity limitation and social participation restriction of people with leprosy from 2001 to 2014 in Picos, Piauí, Brazil.
Methods
this was a cross-sectional study with data collected through interviews and physical examinations; the SALSA Scale (Screening of Activity Limitation and Safety Awareness) and Social Participation Scale were used; crude prevalence ratios (PR) were calculated.
Results
263 people with leprosy participated in the study; activity limitation was associated with grade I/II disability (PR=1.66; 95%CI 1.14;2.41), age ≥60 years (PR=1.68; 95%CI 1.09;3.02) and low schooling (PR=1.76; 95%CI 1.26;2.45); correlation was found between eye-hand-foot score and activity limitation (r=0.29; p<0.001) and participation restriction (r=0.27; p<0.001).
Conclusion
activity limitation and participation restriction had high prevalence in the context studied and were associated with disease severity, advanced age and social vulnerability.
Key words: Leprosy; Social Participation; Activities of Daily Living; Cross-Sectional Studies
Introduction
Leprosy is an age-old communicable disease with a long period of clinical latency and is caused by the Mycobacterium leprae bacterium .1 It is part of a group of neglected tropical diseases, with high endemicity in countries where inequalities are pronounced, such as India, Brazil and Indonesia, which accounted for 80% of notified cases worldwide in 2017.2
Despite efforts made to integrate leprosy control into the healthcare network in Brazil, in 2017 the country registered 92% of all new cases on the American continent, totaling 26,875 notifications and an overall detection rate of 12.9/100,000 inhabitants.2 Geographic distribution of leprosy cases in Brazil is of a focalized nature and overlaps with impoverished regions, mainly the in North, Northeast and Midwest regions of the country.3
There is great concern about controlling the dynamics of transmission, especially because of the physical disabilities caused by the disease. Disability is bodily, personal or social functional difficulty experienced by an individual with a given health condition in their interaction with contextual factors.5 Nerve alterations related to M. leprae infection can result in problems, such as reduced ability to work, limited social life, reduction in community participation and psychological disorders.6
The majority of studies take into account disability and incapacity that can be caused by leprosy, but few studies address how this can affect a person’s daily routine and diverse aspects of their social life.7 Moreover, as a dermato-neurological clinical syndrome, leprosy should not only be considered with regard to its magnitude, but also with regard to its transcendence, taking into consideration the personal and social costs of this condition for the population.6
Activity limitation refers to the difficulty an individual has in performing a task, while social participation restriction refers to problems an individual may face when involved in real-life situations, in different areas, such as mobility, interpersonal relationships, marriage, employment, leisure activities and taking part in social and religious activities.5 Activity limitation and social participation restrictions are concepts devised by the World Health Organization (WHO) and lead us to consider leprosy as a disease that goes beyond bacterial load and clinical aspects.
Occurrence of activity limitation and social participation restriction in people with leprosy can lead to prejudice and discrimination. As a consequence, direct or indirect harm to health can occur as a result of social marginalization. In addition to hindering access to prevention, these can lead to late diagnosis, abandonment of treatment and reduction in health care.9
From this perspective, this study aimed to analyze the magnitude and factors associated with activity limitation and social participation restriction of people with leprosy between 2001 and 2014, in Picos, Piauí, Brazil.
Methods
This was a cross-sectional study conducted in Picos, in the state of Piauí, located in the Northeast region of Brazil. This study provides information on part of the Integrahans-Piauí project, coordinated by the Federal University of Piauí (UFPI), in partnership with the Federal University of Ceará (UFC).
The municipality of Picos was selected because it is classified as being leprosy hyperendemic, belonging to Cluster 6 on the national level, as well as being a leprosy treatment reference center for the entire Guaribas Valley.10 In 2018 the municipality’s demographic density was 137.30 inhabitants/km2and its estimated population was 78,002.11 The Family Health Strategy there had 100% percentage coverage in 2019.12 According to the 2013 Brazilian Human Development Index, Picos had a Human Development Index of 0.698.13
The study’s target population was comprised of all leprosy cases in the municipality of Picos, diagnosed between 2001 and 2014 and notified on the Notifiable Health Condition Information System (SINAN). Given the specificity of the scales used, the inclusion criteria established were being over 15 years old and resident in the municipality at the time of the study. Persons deprived of liberty and those with cognitive impairment preventing them from participating were excluded from the study. Losses were considered to be people who were not located and people who did not take part in all stages of the study and therefore did not answer all the instruments.
It was possible to identify case records duplicated on the system by checking the following variables: patient’s name, patient’s mother’s name and patient’s date of birth. These records, as well as those of people who died during the period under consideration, were not considered in the analysis.
The search for cases and data collection took place in the municipality’s primary healthcare centers, according to the person’s catchment area, as well as in community spaces such as churches and schools. Each person was identified on the SINAN system and as the addresses held on the system were those stated at the time of case notification, the National Brazilian Health System User Registry was checked to confirm and/or update addresses and telephone numbers. Cases were approached with the assistance of Family Health Team community health agents and nurses of each catchment area.
With the aim of achieving uniform data collection, the field researchers (health professionals and undergraduate students taking part in the Integrahans-Piauí project) underwent training. They were responsible for interviews involving the administration of standardized questionnaires and for performing physical examination (simplified neurological assessment), as described below.
The following sociodemographic and clinical variables were investigated: age range (15-29, 30-44, 45-59, ≥60 years); sex (male, female); years of study (<8 years, ≥8 years); race/skin color (white, brown, black, yellow, indigenous); area of residence (rural, urban); work situation (working, retired, unemployed, housewife and student); leprosy operational classification (paucibacillary [PB], multibacillary [MB]); clinical forms (indeterminate, tuberculoid, borderline, lepromatous); and self-reported (yes, no) occurrence of reaction episodes (immune responses to bacilli, which can occur before, during or after leprosy treatment).14
Simplified neurological assessment was also conducted in order to classify physical disability, using a standardized Ministry of Health instrument.14 Grade of physical disability (GPD) and eye-hand-foot (EHF) impairment score were established based on inspection, nerve palpation, strength test and hand and feet sensitivity test with Semmes-Weinstein monofilaments. Physical disability was classified according to the highest grade found in the examination: grade 0 (no leprosy-related disability); grade 1 (reduction or loss of sensitivity); and grade 2 (presence of disabilities and visible deformities).14 In turn, the EHF score assesses presence and magnitude of physical disabilities and the sum of all individual GPDs in relation to the eyes, both hands and both feet, thus determining the maximum grade of disability for each affected segment, with a final score varying between 0 and 12.14
The SALSA scale (Screening of Activity Limitation and Safety Awareness) was used to measure activity limitation. The scale’s score varies between 1 and 80; the lower the score, the lesser the difficulty in doing everyday activities, while higher scores indicate growing levels of activity limitation. The scores are categorized as follows: 10-24 (no limitation); 25-39 (mild limitation); 40-49 (moderate limitation); 50-59 (severe limitation); 60-80 (very severe limitation).15
The Social Participation Scale version 4.6 was used to measure social participation restriction. The scale is comprised of 18 items, measured by means of an interview, with total points ranging from 0 to 90. People who scored up to 12 points were classified as not having any significant participation restriction. From 12 upwards different grades of restriction were identified: mild restriction (13-22), moderate restriction (23-32), high restriction (33-52) and extreme restriction (53-90).16
For both scales, the final scores were calculated manually as soon as they had been administered in order to measure and inform participants about the existence of activity limitation or social participation restriction, as well as to assist them with any care needs shown by the outcomes.
In the case of the quantitative variables, the descriptive data were presented showing averages, standard deviations, minimum and maximum values, while categorical variables were presented showing absolute frequencies and percentages.
Crude analysis was performed using Pearson’s chi-square statistical test, while Poisson regression was used to calculate the prevalence ratio (PR), with 95% confidence intervals (95%CI), in order to investigate associations with the dependent variable (occurrence of absence of activity limitation or participation restriction) and its association with the explanatory variables.
In order to verify association of social participation restriction and activity limitation with demographic and clinical variables, the variables were reclassified. In the case of activity limitation, people were considered either as having no limitation or having limitation (if they fell into the mild, moderate, severe and very severe classifications). Similarly with regard to participation restriction, people were considered as having no restriction or as having restriction (if they fell into the mild, moderate, high and extreme classifications).
With regard to the scores calculated (EHF score, Salsa score and Social Participation score), after checking for normality using the Shapiro Wilk test, scatter plots were built to test for the existence of linear correlation between the variables. The Pearson or Spearman correlation coefficient (r) was considered: r=0.10 to 0.30 (weak correlation), r=0.40 to 0.60 (moderate correlation) and r=0.70 to 1 (strong correlation). A 5% significance level was adopted with 80% statistical power.
The data were analyzed with the aid of Stata version 11.0 (Stata Corporation, College Station, USA).
The study was approved by the Federal University of Piauí Research Ethics Committee, report no. 1.115.818, on 17/05/2015. Data collection was done after a Free and Informed Consent form had been signed following explanation of the study’s objectives. Each person’s privacy and confidentiality was respected, as was their relationship with the health team responsible for their health service catchment area.
Results
A total of 703 people with leprosy were identified as having been notified between 2001 and 2014 in the municipality of Picos. The inclusion criteria were not met by 36 deaths, 32 people whose address had changed, four people under 15 years old and one person deprived of liberty. There were 363 losses, due to people not being located (n=289) or not taking part in one or more stages of the study (n=74), as well as four refusals to take part. The study sample was comprised of 263 people.
Almost half the sample was found to have some degree of activity limitation (45.3%), and approximately one quarter of them (24.0%) had some degree of participation restriction ( Figure 1 ). The average SALSA score was 27.6, with a minimum score of 13.0 and a maximum score of 76.0. The average participation score was 9.0 (minimum 0.0, maximum 59.0).
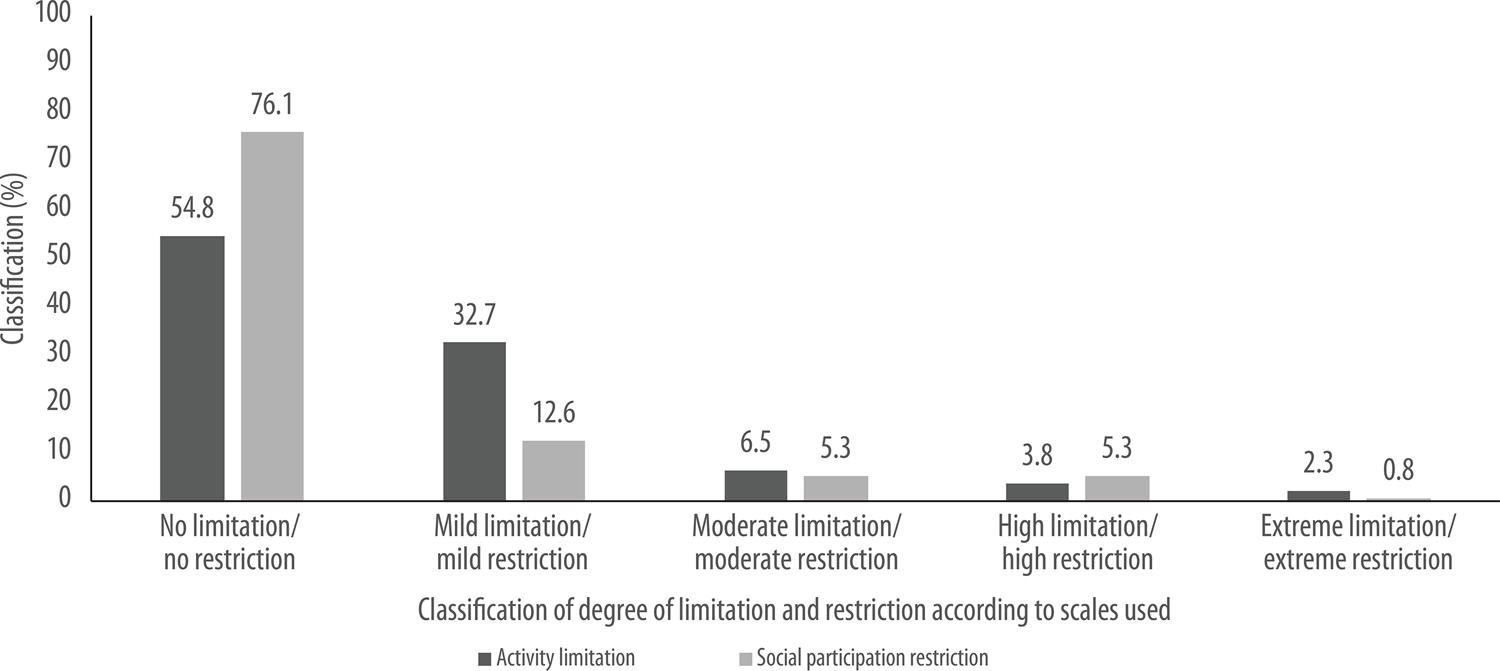
Figure 1 – Percentage distribution of frequencies of activity limitation and participation restriction of people with leprosy, Picos, Piauí, Brazil 2001-2014 (n=263)
The male sex was predominant (50.2%). Average age was 52 years (varying between 15 and 87 years, standard deviation 1) and 36.9% were over 60 years old; 43.0% had less than 8 years of study; 50.2% were of brown race/skin color; 94.3% lived in the urban area; and 44.1% were working.
The operational classification of 52.5% of the participants was multibacillary, and the most frequent clinical forms were borderline and indeterminate (34.6% and 32.3%, respectively). As for nerve damage, 61.2% had GPD 1 and an EHF score varying between 0 and 12, with 33.1% having score 2. The majority reported not having had a reaction episode (82.1%).
Greatest limitation was found to be statistically associated with the 60 and over age range (PR=1.68, 95%CI 1.09;3.02), when compared to the 30-44 age range, currently with GPD 1 or 2 (PR=1.66, 95%CI 1.14;2.41) and with low schooling or less than 8 years of study (PR=1.76, 95%CI 1.26;2.45) ( Table 1 ).
Table 1 – Absolute and percentage distribution and association between activity limitation and demographic and clinical variables of people with leprosy, Picos, Piauí, Brazil 2001-2014 (n=263)
| Variables | Activity limitation | PRa | 95%CIa | p-valueb | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Total | Yes | No | ||||
|
| ||||||
| n (%) | n (%) | n (%) | ||||
| Age range (years) | ||||||
| 15-29 | 33 (12.5) | 11 (33.3) | 22 (66.7) | 1.11 | 0.56;2.18 | 0.028 |
| 30-44 | 40 (15.2) | 12 (30.0) | 28 (70.0) | 1.00 | - | |
| 45-59 | 93 (35.4) | 43 (46.2) | 50 (53.8) | 1.54 | 0.91;2.59 | |
| ≥ 60 | 97 (36.9) | 53 (54.6) | 44 (45.4) | 1.68 | 1.09;3.02 | |
| Sex | ||||||
| Female | 131 (49.8) | 65 (49.6) | 66 (50.4) | 1.00 | - | 0.156 |
| Male | 132 (50.2) | 54 (40.9) | 78 (59.1) | 0.82 | 0.63;1.07 | |
| Years of study | ||||||
| < 8 | 165 (62.7) | 89 (53.9) | 76 (46.1) | 1.76 | 1.26;2.45 | <0.001 |
| ≥ 8 | 98 (37.3) | 30 (30.6) | 68 (69.4) | 1.00 | - | |
| Operational classification | ||||||
| Paucibacillary | 125 (47.5) | 53 (42.4) | 72 (57.6) | 1.00 | - | 0.377 |
| Multibacillary | 138 (52.5) | 66 (47.8) | 72 (52.2) | 1.12 | 0.86 ;1.45 | |
| GPD | ||||||
| Yes (1 and 2) | 191 (72.6) | 97 (50.8) | 94 (49.2) | 1.66 | 1.14;2.41 | <0.001 |
| No | 72 (27.4) | 22 (30.6) | 50 (69.4) | 1.00 | - | |
PR = prevalence ratio.
GPD = grade of physical disability.
95%CI = 95% confidence interval.
a) Calculated using Poisson regression.
b) Calculated using Pearson’s Chi-Square statistical test.
No statistically significant associations were found for social participation restriction, although indications were found in relation to association between the operational classification and GPD 1 or 2 variables ( Table 2 ). The p-value demonstrates possible significance between these variables, but this is not corroborated by the confidence interval identified for association. As such, in this study, people with a higher degree of disability or more severe clinical forms did not necessarily have a higher level of social participation restriction.
Table 2 – Absolute and percentage distribution and association between social participation restriction and demographic and clinical variables of people with leprosy, Picos, Piauí, Brazil 2001-2014 (n=263)
| Variables | Social participation restriction | PRa | 95%CIa | p-valueb | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Total | Yes | No | ||||
|
| ||||||
| n (%) | n (%) | n (%) | ||||
| Age range (years) | ||||||
| 15-29 | 33 (12.5) | 8 (24.2) | 25 (75.8) | 2.42 | 0.80;7.34 | 0.153 |
| 30-44 | 40 (15.2) | 4 (10.0) | 36 (90.0) | 1.00 | - | |
| 45-59 | 93 (35.4) | 26 (28.0) | 67 (72.0) | 2.79 | 1.04;7.48 | |
| ≥ 60 | 97 (36.9) | 25 (25.8) | 72 (74.2) | 2.57 | 0.95;6.93 | |
| Sex | ||||||
| Female | 131 (49.8) | 36 (27.5) | 95 (72.5) | 1.00 | - | 0.182 |
| Male | 132 (50.2) | 27 (20.5) | 105 (79.5) | 0.74 | 0.48;1.15 | |
| Years of study | ||||||
| < 8 | 165 (62.7) | 46 (27.9) | 119 (72.1) | 1.76 | 1.26;2.45 | 0.053 |
| ≥ 8 | 98 (37.3) | 17 (17.3) | 81 (82.7) | 1.00 | - | |
| Operational classification | ||||||
| Paucibacillary | 125 (47.5) | 23 (18.4) | 102 (81.6) | 1.00 | - | 0.046 |
| Multibacillary | 138 (52.5) | 40 (29.0) | 98 (71.0) | 1.39 | 0.98;1.98 | |
| GPD | ||||||
| Yes (1 and 2) | 191 (72.6) | 52 (27.2) | 139 (72.8) | 1.78 | 0.98;3.21 | 0.043 |
| No | 72 (27.4) | 11 (15.3) | 61(84.7) | 1.00 | - | |
PR = prevalence ratio.
GPD = grade of physical disability.
95%CI = 95% confidence interval.
a) Calculated using Poisson regression.
b) Calculated using Pearson’s Chi-Square statistical test.
Significant correlation was found between EHF score and activity limitation (r=0.29; p<0.001) and participation restriction (r=0.27; p<0.001). Analysis of correlation between SALSA score (informs as to absence or presence of activity limitation and to what degree: mild, moderate, high and extreme limitation) and EHF score (provides the sum of all individual grades of disability for both eyes, both hands and both feet, determining the maximum grade of disability in relation to loss of sensitivity or presence of visible deformity), according to operational classification, was positive, weak and significant in paucibacillary cases (r=0.32; p<0.001) and multibacillary cases (r=0.24; p=0.003) ( Figure 2 ). It was found that varying degrees of segment impairment (score >5) do not necessarily generate an increased activity limitation score.
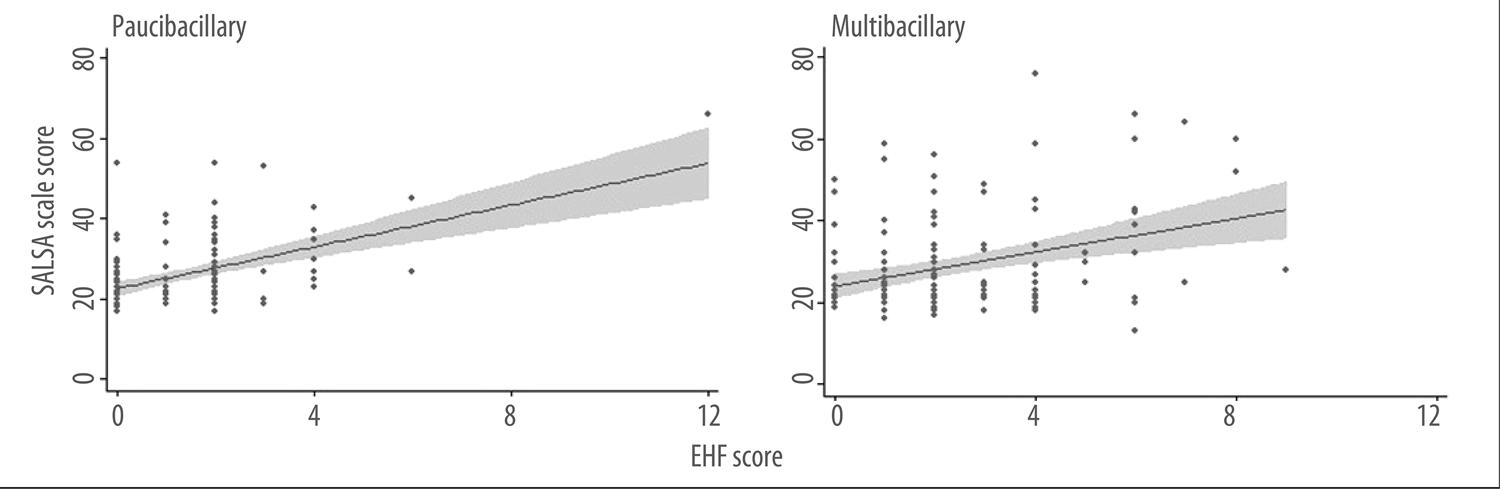
Figure 2 – Correlation between SALSA score (Screening of Activity Limitation and Safety Awareness) and eye-hand-foot score (EHF), according to operational classification, in people with leprosy, Picos, Piauí, Brazil 2001-2014 (n=263)
Correlation between participation score (informs as to absence or presence of social participation restriction and to what degree: mild, moderate, high and extreme restriction) and EHF score also revealed positive, weak and significant correlation in paucibacillary cases (r=0.23; p=0.009) and multibacillary cases (r=0.22; p=0.010) ( Figure 3 ). A greater degree of impairment of the segment assessed does not produce an increase in social participation restriction in all cases.
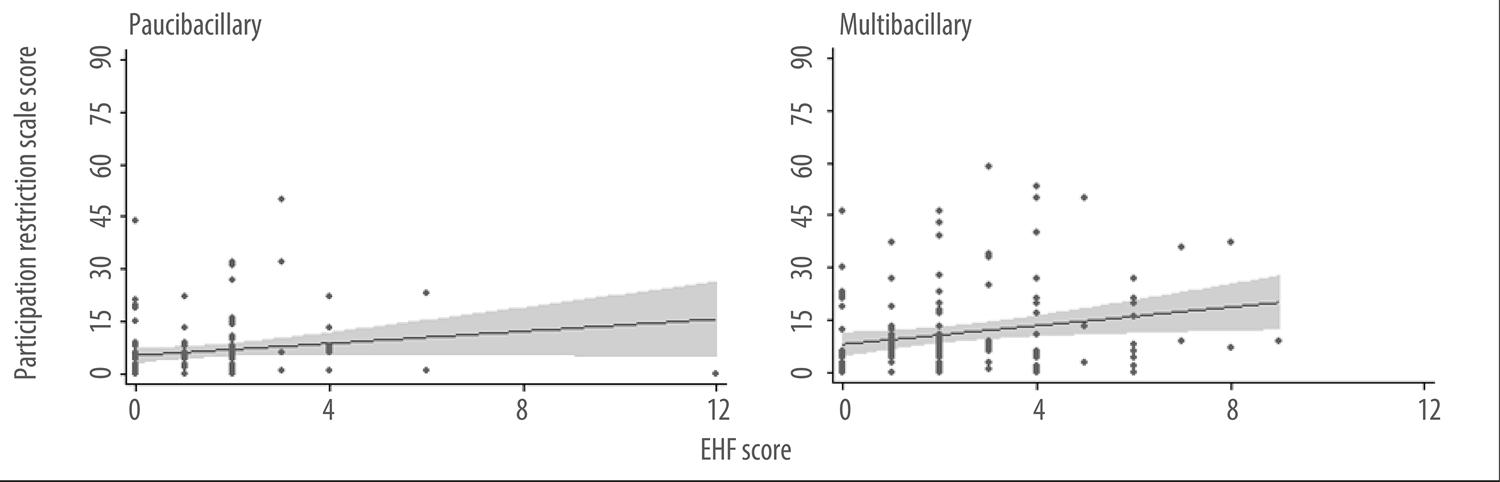
Figure 3 – Correlation between social participation restriction score and eye-hand-foot score (EHF), according to operational classification, in people with leprosy, Picos, Piauí, Brazil 2001-2014 (n= 263)
Analysis of the correlation between the two study outcomes demonstrated that social participation restriction was significantly associated with activity limitation in both operational classifications, showing moderate and significant correlation in multibacillary cases (r=0.54; p<0.001) and weak and significant correlation in paucibacillary cases (r=0.23; p=0.012).
This study identified 16 (6.1%) people with high and extreme social participation restriction, whereby 13 (81.3%) were multibacillary cases and 14 (87.5%) were cases with GPD 1 or 2 and activity limitation.
Discussion
This study reinforces the importance of analyzing the dimensions of social participation restriction and activity limitation when assessing people with leprosy. High prevalence of these two analytical dimensions was found in the hyperendemic context of the municipality, as well as association of activity limitation and social participation restriction with disease severity (multibacillary operational classification), more advanced age group (>60 years) and elements of social vulnerability (low schooling). Moreover, the psychosocial aspects continue to be leprosy control-related challenges for the Brazilian National Health System (SUS), in addition to the physical aspects.
Classification of activity limitation varies depending on the scenario.17 Segundo Bezerra et al., people affected by leprosy do not perceive themselves as being limited and continue to be involved in society, despite the stigma surrounding the disease. Studies conducted in Fortaleza and Sobral/CE in 2006, in Araguaína/TO in 2010, and in Uberaba/MG in 2014, reported similar results,17 with individuals showing more activity limitation than social participation restriction. In turn, in studies conducted in Vitória da Conquista/BA in 2014 and in Cajazeiras/PB in 2011, approximately 25% and 57% of people with leprosy, respectively, had some degree of restriction.21
Greater occurrence of activity limitation in people over 60 years old was an expected association, given that the SALSA scale manual itself indicates that scores tend to increase with age, there being no difference between men and women of the same age and with the same physical disabilities.15
Physical disability is a characteristic of leprosy due to underlying nerve damage arising from the action of the bacillus.16 The importance of assessing GPD at the time of diagnosis, treatment and following discharge from health services must be emphasized. As it identifies disability and incapacity risk factors, this assessment needs to be integrated into specific ESF specific analysis analysis in order to achieve a more comprehensive approach.23
People with reduced sensitivity end up avoiding everyday activities capable of causing injury, as well as changing the way they do them.22 The study conducted by Sousa et al. in Aracaju/SE in 2014 also found that GPD is significantly associated with activity limitations in this population.24
Low schooling was identified as a factor related to the existence of some degree of activity limitation. This fact may be related to precarious social conditions, which tend to increase vulnerability and decrease the search for knowledge about actions to prevent the disease and its consequences.25 Adequate follow-up of treatment is therefore compromised, as are self-care measures, and this can lead to or worsen physical disabilities.18 Health professionals need to pay attention to social determinants of the disease, carrying out promotion and prevention activities, as well as inclusive development and social rehabilitation activities.27
Association was found between social participation restriction and operational classification of leprosy and GPD in India in 2014, demonstrating that there was greater restriction among people with multibacillary classification and with visible disabilities (GPD 2).28 Operational classification is an important measure for establishing treatment duration. The multibacillary category indicates later and more severe forms, known to be related to physical disabilities and deformities and the possibility of leading to social participation restriction.14
The EHF score provides evidence, during assessment, of the existence of overlapping impairment in segments of the body. It is more appropriate than disability grading, which is more commonly used, for simplifying follow-up records and systems, as well as for describing the extent of physical disabilities.14 Studies conducted in Araguaína/TO in 2010, and in Nova Iguaçu/RJ between 2010 and 2011, also found correlation between activity limitation, social participation restriction and EHF score. On the other hand, Barbosa et al. were not able to demonstrate definite correlation between activity limitation and EHF score in Fortaleza and Sobral/CE in 2006.17
Most of those who had some degree of disability also had activity limitation, while the same did not apply to social participation restriction, despite association found in both cases. Occurrence of a physical or functional alteration can change the routine for carrying out an everyday activity, but not necessarily lead to a person’s exclusion from social actions. On the other hand, stigma and prejudice arising from the cultural history of leprosy can lead to exclusion, even when lesions are not visible.16
Despite the relevance of the analyses performed using previously administered and validated instruments, this study does have some weaknesses that need to be discussed. The need to find participants over a long time series led to a considerable loss of the sample. This may have led to underestimation of the prevalence rates found and this needs to be taken into consideration when interpreting the findings. There may also have been selection and sampling bias, in that those individuals who did not take part in the study and who were considered to be losses (not located and refusals), could have differences in relation to the variables studied among the study participants. Another issue is the statistical approach used, which does not include adjusted analyses, so that the confounding potential of variables studied in the associations found was not assessed; as such the magnitude of these associations may be overestimated.
Activity limitation and social participation restriction were highly prevalent dimensions in the context analyzed, and aspects such as disease severity, advanced age and social vulnerability were associated with these outcomes. The findings therefore suggest the influence of these dimensions on the disease’s transcendence and chronicity, reinforcing the need for continuous and multiprofessional follow-up when preparing treatment plans adequate for people with leprosy. In this context, early diagnosis can ensure prevention of disabilities.
REFERENCES
1. Lockwood DNJ. Chronic aspects of leprosy-neglected but important. Trans R Soc Trop Med Hyg [Internet]. 2019 Dec [cited 2020 May 7];113(12):813-7. Available from: https://doi.org/10.1093/trstmh/try131 [ Links ]
2. World Health Organization. Global leprosy update, 2017: reducing the disease burden due to leprosy. Wkly Epidemiol Rec [Internet]. 2018 Oct [cited 2020 May 7];35:445-56. Available from: https://apps.who.int/iris/bitstream/handle/10665/274290/WER9335-445-456.pdf?sequence=1&isAllowed=y [ Links ]
3. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância de Doenças e Agravos não Transmissíveis e Promoção da Saúde. Taxa de Detecção geral de hanseníase por 100.000 habitantes. Estados e regiões, Brasil, 1990 a 2017 [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2020 maio 7]. Disponível em: https://www.saude.gov.br/images/pdf/2018/julho/13/Taxa-de-deteccao-geral-de-hanseniase-1990a2017.pdf [ Links ]
4. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância de Doenças e Agravos não Transmissíveis e Promoção da Saúde. Saúde Brasil 2017: uma análise da situação de saúde e os desafios para o alcance dos objetivos de desenvolvimento sustentável [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2020 maio 7]. 426 p. Disponível em: https://bvsms.saude.gov.br/bvs/publicacoes/saude_brasil_2017_analise_situacao_saude_desafios_objetivos_desenvolvimento_sustetantavel.pdf [ Links ]
5. Organização Mundial de Saúde. CIF: classificação internacional de funcionalidade, incapacidade e saúde. São Paulo: EDUSP; 2008. [ Links ]
6. Organização Mundial da Saúde. Organização Pan-Americana da Saúde. Estratégia global para hanseníase 2016-2020: acelerando rumo a um mundo sem hanseníase [Internet]. Nova Deli: Organização Mundial da Saúde; 2016 [citado 2020 maio 7]. 21 p. Disponível em: https://apps.who.int/iris/bitstream/handle/10665/208824/9789290225201-pt.pdf [ Links ]
7. van Brakel WH, Anderson AM, Mutatkar RK, Barkirtzief Z, Nicholis PG, Raju MS, et al. The participation scale: measuring a key concept in public health. Disabil Rehabil. 2006 Feb [cited 2020 May 7];28(4):193-203. Available from: https://doi.org/10.1080/09638280500192785 [ Links ]
8. van Brakel WH, Anderson AM, Wörpel FC, Saiju R, Bk HB, Sherpa S, et al. A scale to assess activities of daily living in persons affected by leprosy. Lepr Rev [Internet]. 1999 Sep [cited 2020 May 7];70(3):314-23. Available from: https://doi.org/10.5935/0305-7518.19990035 [ Links ]
9. Garbin CAS, Garbin AJI, Carloni MEOG, Rovida TAS, Martins RJ. The stigma and prejudice of leprosy: influence on the human condition. Rev Soc Bras Med Trop [Internet]. 2015 Mar-Apr [cited 2020 May 7];48(2):194-201. Available from: https://doi.org/0037-8682-0004-2015 [ Links ]
10. Secretaria de Estado da Saúde do Piauí - SESAPI. Supervisão da Hanseníase, Coordenação de doenças transmissíveis. Situação atual da hanseníase no estado do Piauí no período de 2013 a 2014. Teresina: Secretaria de Estado da Saúde do Piauí; 2014. [ Links ]
11. Instituto Brasileiro de Geografia e Estatística - IBGE. Censo demográfico – cidades: Picos [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2017 [citado 2019 abr 15]. Disponível em: https://cidades.ibge.gov.br/brasil/pi/picos. [ Links ]
12. Ministério da Saúde (BR). E-Gestor atenção básica: informação e gestão da atenção básica [Internet]. Brasília: Ministério da Saúde; 2017 [citado 2019 abr 15]. Disponível em: https://egestorab.saude.gov.br/paginas/acessoPublico/relatorios/relHistoricoCoberturaAB.xhtml [ Links ]
13. Atlas do Desenvolvimento Humano no Brasil. Picos, PI [Internet]. [S.l.]: Atlas do Desenvolvimento Humano no Brasil; 201- [citado 2019 abr 15]. Disponível em: http://atlasbrasil.org.br/2013/pt/perfil_m/picos_pi [ Links ]
14. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância de Doenças Transmissíveis. Guia prático sobre a hanseníase [Internet]. Brasília: Ministério da Saúde; 2017 [citado 2020 maio 7]. 68 p. Disponível em: https://portalarquivos2.saude.gov.br/images/pdf/2017/novembro/22/Guia-Pratico-de-Hanseniase-WEB.pdf [ Links ]
15. SALSA Collaborative Study Group. Salsa Scale: manual do usuário – versão 1.1 [Internet]. Apeldoorn: SALSA Collaborative Study Group; 2010 [cited 2020 may 7]. 33 p. Available from: https://www.infontd.org/toolkits/salsa-scale [ Links ]
16. Participation Scale Development Team. Participation scale: users manual v.4.6. [Internet]. Amsterdam: Participation Scale Development Team; 2005 [cited 2020 May 7]. Available from: https://www.infontd.org/toolkits/nmd-toolkit/participation-scale [ Links ]
17. Barbosa JC, Ramos Junior AN, Alencar, MJF, Castro CGJ. Pós-alta em hanseníase no Ceará: limitação da atividade funcional, consciência de risco e participação social. Rev Bras Enferm [Internet]. 2008 [citado 2020 maio 7];61(n.spe):727-33. Disponível em: https://doi.org/10.1590/S0034-71672008000700012 [ Links ]
18. Monteiro LD, Alencar CH, Barbosa JC, Novaes CCBS, Silva RCP, Heukelbach J. Pós-alta de hanseníase: limitação de atividade e participação social em área hiperendêmica do Norte do Brasil. Rev Bras Epidemiol [Internet]. 2014 jan-mar [citado 2020 maio 7];17(1):91-104. Disponível em: https://doi.org/10.1590/1415-790X201400010008ENG [ Links ]
19. Bezerra PB, Silva MCL, Andrade MCF, Silva LVC. Avaliação física e funcional de pacientes com hanseníase. Revenferm UFPE [Internet]. 2015 set [citado 2020 maio 7];9(suppl 8);9336-42. Disponível em: https://doi.org/10.5205/reuol.6812-75590-1-ED.0908sup201501 [ Links ]
20. Reis BM, Castro SS, Fernandes LFRM. Limitação da atividade e restrição da participação social em relação à faixa etária, ao sexo e à escolaridade de pessoas com hanseníase. An Bras Dermatol [Internet]. 2017 [citado 2020 maio 7];92(3):339-43. Disponível em: http://www.anaisdedermatologia.org.br/detalhe-artigo/102740/Limitacao-da-atividade-e-restricao-da-participacao-social-em-relacao-a-faixa-etaria--ao-sexo-e-a-escolaridade-de-pessoas-com-hanseniase- [ Links ]
21. Castilhano AA. Sentidos e motivações da restrição à participação social em pessoas afetadas pela hanseníase no município de Vitória da Conquista – BA, no período de 2001 a 2014 [dissertação]. Fortaleza (CE): Universidade Federal do Ceará; 2017. 106 p. Disponível em: http://www.repositorio.ufc.br/handle/riufc/25751 [ Links ]
22. Oliveira LR, Nascimento AR, Nascimento MMP, Pereira AP, Lemos ICS, Kerntopf MR. Limitação de atividades e participação social entre usuários de um grupo de autocuidado em hanseníase. Rev Interdisc [Internet]. 2016 jan-mar [citado 2020 maio 7];9(1):171-81. Disponível em: https://revistainterdisciplinar.uninovafapi.edu.br/index.php/revinter/article/view/791 [ Links ]
23. Ministério da Saúde (BR).Departamento da Vigilância das Doenças Transmissíveis. Secretaria de Vigilância em Saúde. Diretrizes para vigilância, atenção e eliminação da Hanseníase como problema de saúde pública: manual técnico-operacional [Internet]. Brasília: Ministério da Saúde; 2016 [citado 2020 maio 7]. 58 p. Disponível em: https://www.saude.gov.br/images/pdf/2016/fevereiro/04/diretrizes-eliminacao-hanseniase-4fev16-web.pdf [ Links ]
24. Souza VTC, Silva Júnior WM, Jesus AMR, Oliveira DT, Raptis HA, Freitas PHL, et al. Is the WHO disability grading system for leprosy related to the level of functional activity and social participation? Lepr Rev [Internet]. 2016 Jun [cited 2020 May 7];87(2):191-200. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30212053 [ Links ]
25. Queirós MI, Ramos Júnior AN, Alencar CHM, Monteiro LD, Sena AL, Barbosa JC. Perfil clínico epidemiológico de pacientes com hanseníase atendidos em hospital universitário no Ceará entre 2007 e 2011. An Bras Dermatol [Internet]. 2016 [citado 2020 maio 7];91(3):311-7. Disponível em: http://www.anaisdedermatologia.org.br/detalhe-artigo/102471/Perfil-clinico-epidemiologico-de-pacientes-com-hanseniase-atendidos-em-hospital-universitario-no-Ceara-entre-2007-e-2011- [ Links ]
26. Souza EA, Ferreira AF, Heukelbach J, Boigny RN, Alencar CH, Ramos Júnior AN. Epidemiology and spatiotemporal patterns of leprosy detection in the State of Bahia, Brazilian Northeast Region, 2001-2014. Trop Med Infect Dis [Internet]. 2018 Jul [cited 2020 May 7];3(3):E79. Available from: https://doi.org/10.3390/tropicalmed3030079 [ Links ]
27. Lana FCF, Amaral, EP. Análise espacial da Hanseníase na microrregião de Almenara, MG, Brasil. Rev Bras Enferm [Internet]. 2008 nov [citado 2020 maio 7];61(n.spe.):701-7. Disponível em: https://doi.org/10.1590/S0034-71672008000700008 [ Links ]
28. Ramasamy S, Govindharaj P, Kumar A, Govindasamy K, John A. Changes in social participation of persons affected by leprosy, before and after multidrug therapy, in an endemic State in Eastern India. DCID [Internet]. 2019 [cited 2020 May 7];30(2):54-64. Available from: https://pdfs.semanticscholar.org/c687/72c50bb689c43fae768fc8ec2f8e8da3cc99.pdf?_ga=2.258683661.641582606.1589824107-783148302.1544653156 [ Links ]
29. Castro LE, Cunha AJ, Fontana AP, Halfoun VLC, Gomes MK. Physical disability and social participation in patients affected by leprosy after discontinuation of multidrug therapy. Lepr Rev [Internet]. 2014 Sep [cited 2020 May 7];85(3):208-17. Available from: https://europepmc.org/article/med/25509722 [ Links ]
Associate Editor: Bárbara Reis Santos - orcid.org/0000-0001-6952-0352
*Article derived from the Master’s Degree dissertation entitled ‘Patterns and factors associated with activity limitation and participation restriction of people with leprosy from 2001-2014 in Picos/PI’, defended by Danelle da Silva Nascimento at the Federal University of Ceará Public Health Postgraduate Program in 2019. This research received funding from the National Council for Scientific and Technological Development (CNPq), process No. 404505/2012-0, Call for Proposals MCTI/CNPq/MS-SCTIE-Decit No. 40/2012 – Neglected Diseases Research.
Received: January 02, 2020; Accepted: May 05, 2020











 texto en
texto en 


