Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.3 Brasília jun. 2020 Epub 18-Jun-2020
http://dx.doi.org/10.5123/s1679-49742020000300018
Review article
Suspected COVID-19 case definition: a narrative review of the most frequent signs and symptoms among confirmed cases
1 Universidade do Sul de Santa Catarina , Programa de Pós-Graduação em Ciências da Saúde , Tubarão SC , Brazil
2 Universidade do Sul de Santa Catarina , Faculdade de Medicina , Tubarão , SC , Brazil
Objective
to describe the most frequent signs and symptoms of infection by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Methods
this is a narrative literature review carried out in April 2020; the search was performed on electronic databases and complemented with a manual review of the references of the selected papers and Brazilian Ministry of Health publications.
Results
the spectrum of clinical disease was wide; fever, coughing and dyspnea were the most frequent signs/symptoms, however, they may not be present, thus hindering case definition; gastrointestinal symptoms and loss of taste or smell have been reported among mild cases; dyspnea was frequent among severe and fatal cases.
Conclusion
considering the scarcity of diagnostic tests and the diversity of symptoms, health services should use a sensitive case definition, in order to adopt appropriate surveillance, prevention and treatment actions.
Key words: Coronavirus Infections; Signs and Symptoms; Epidemics; Review
Introduction
The coronavirus 2 pandemic related to severe acute respiratory syndrome (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19), emerged at the end of 2019 in Wuhan, Hubei Province, China, and has spread rapidly across all continents, exponentially increasing the number of infected people and causing thousands of deaths worldwide. 1 It is estimated that as at April 26 th 2020, more than 2.8 million people had been infected and over 193,000 had died from causes related to the disease caused by the novel coronavirus (COVID-19). 2
Given its vast magnitude and the diverse supplies needed to control it, such as availability of diagnostic tests for affected people, combating COVID-19 has become a challenge, especially for low and middle-income countries such as Brazil which depend on technologies produced in other countries. 3
How can SARS-CoV-2 infection be diagnosed or defined, if health centers do not have sufficient laboratory tests available? Moreover, diagnostic tests are intended to be used at specific times of infection and, depending on the stage of the disease, may not be very accurate. 4 As such, assessing clinical signs and symptoms shown by infected people can help establish the healthcare flow and indicate the need to perform confirmatory tests. 6
The objective of this study was to describe the most frequent signs and symptoms of SARS-CoV-2 infection, in order to guide case suspicion based on clinical manifestations and to characterize case severity.
Methods
A qualitative narrative review was undertaken. The purpose of narrative reviews is to describe the state of the art of a given subject and enable more in-depth discussion. This review comprises critical and personal analysis of the authors, and is not intended for generalization. The review was carried out in April 2020 and included studies that presented a description of the clinical picture of the first COVID-19 cases.
The searches were based on the following research question: What are the most frequent signs and symptoms of SARS-CoV-2 infection? The bibliographic search was performed on the Scopus, medRXiv, MEDLINE, SciELO and Google Scholar databases, and it was complemented with a manual search on the lists of references of the papers selected and also on the Brazilian Health Ministry website. No limitations were set for date, study country or area of knowledge. The following terms were use for the search: “Signs”, “symptoms” “clinical”, “laboratory”, combined with “Novel coronavirus” “Novel coronavirus 2019”, “2019 nCoV”, “COVID-19”, “Wuhan coronavirus”, “Wuhan pneumonia” and “SARS-CoV-2”.
The study included original articles, literature reviews, opinion articles and technical documents in English and Portuguese. In situations in which more than one article described the same case cohort, or in which more than one review was identified with the same theme of interest, those with smaller sample sizes and/or which were older were excluded.
Results
Most frequent signs and symptoms among confirmed COVID-19 cases
Ten studies were selected which describe the first confirmed COVID-19 cases and the most common signs and symptoms found. The studies are summarized in Table 1 .
Table 1 – Summary of the studies indicating the main signs and symptoms found in people confirmed as having COVID-19, April 2020
| Authors and years | Place of study | Type of study and sample | Diagnosis criterion | Laboratory test | Common symptoms | Notes |
|---|---|---|---|---|---|---|
| Huang et al., 2020 14 | Wuhan, China | Series a comprised of 41 cases hospitalized as at January 2 nd 2020 | RT-PCR + for COVID-19 | Leukopenia (25%) and lymphopenia (63%) | Fever (98%) + coughing (76%) + myalgia/fatigue (44%), dyspnea (55%), sputum production (28%), headache (8%), (5%) and diarrhea (3%) | Symptoms such as diarrhea, nausea, vomiting and headache were present; 32% of total cases and 38% of cases admitted to ITU had comorbidities, of which diabetes was the most common (20%). All cases had pneumonia, 98% bilateral. |
| Guan WJ et al., 2020 12 | China | Cohort a of 1,099 cases from 552 hospitals in 30 provinces | RT-PCR + for COVID-19 | Lymphopenia (83.2%) | Coughing (67.8%) + fever (43.8% at admission and 88.7% during hospitalization) | 15% had the severe form of the disease; 23.7% had at least one comorbidity (38% of severe cases). |
| Chen T et al., 2020 30 | China | Retrospective case series, that (i) died (n=113) and (ii) that recovered (n=161) | RT-PCR + for COVID-19 | Lymphopenia in 39% of deaths and 5% of recovered and leukocytosis in 50% of deaths and 4% of recovered | Fever (~90%) + coughing (~66-70%) + milder symptoms; dyspnea and tight chest more common among deaths, as well as loss of consciousness | 63% of cases that died and 39% of those that recovered had at least one chronic disease: hypertension (48%), cardiovascular diseases (14%) and cerebrovascular diseases (4%). Deaths presented tachycardia (50%) and tachypnea (27%), and saturation ≤ 93% (64%); 8% of cases that died and 10% of those that recovered did not have fever, but did have fatigue (~50%), coughing (68%), dyspnea (44%), myalgia (22%) or diarrhea (28%) as initial symptoms. |
| Bhatraju PK et al., 2020 13 | Seattle, United States | Series with 24 cases ≥18 years old hospitalized in ITU | RT-PCR + for COVID-19 | 75% lymphopenia and search for other pathogens | Dyspnea and coughing (88%) + fever (50%); sputum production (42%), rhinorrhea (17%), sore throat (8%) and headache (8%) | 58% had diabetes and 14% had asthma and the disease was exacerbated with use of glucocorticoids; 22% were smokers; 33% had more than one chronic condition. |
| Wang Z et al., 2020 15 | China | Retrospective series with 69 cases hospitalized at the Union Hospital, in Wuhan, between January 16 and 29, 2020 | RT-PCR + for COVID-19 | Reduction in neutrophils (39%), eosinophils (72%) and lymphocytes; lymphopenia (42%), higher among deaths (79% vs 32%) | Fever (87%), coughing (55%), fatigue (42%), myalgia (33%) | All 14 deaths (20%) had saturation ≤90%, were older (70.5 years vs 37 years), had more comorbidities (hypertension 36% vs 7%), cardiovascular disease (36% vs 5%) and diabetes (43% vs 2%), and increased inflammatory cytokines. |
| Mao L et al., 2020 29 | Wuhan, China | Retrospective series of 214 hospitalized cases; data retrieved from medical records | RT-PCR + for COVID-19 | Inflammatory response pattern, principally in severe cases: more leukocytes and neutrophils, fewer lymphocytes and higher CRP levels | Fever (132 [61.7%]), dry cough (107 [50.0%]) and anorexia (68 [31.8%]). CNS: dizziness (16.8%) and headache (13.1%). PNS: anosmia (5.1%) and ageusia (5.6%) | Severe cases were older (58.7 ± 15.0 years vs 48.9 ± 14.7 years), had more comorbidities (42 [47.7%] vs 41 [32.5%]), hypertension (32 [36.4%] vs 19 [15.1%]), and had fewer symptoms considered typical such as fever (40 [45.5%] vs 92 [73%]) and coughing (30 [34.1%] vs 77 [61.1%]). Severe cases presented damage to liver, kidneys and muscles. NS symptoms were more common in severe cases, but with no laboratory differences between those who did or did not have PNS symptoms. |
| Giacomelli A et al., 2020 19 | Milan, Italy | ( Letter to the editor ) Cross-sectional study with 88 hospitalized cases; 59 interviewed | Not reported | Not reported | Fever (72.8%), coughing (37.3%), dyspnea (25.4%), arthralgia (5.1%), at least one smell or taste sense disorder (33.9%) or both (18.6%) | Symptoms appeared more in women (52.6% vs 25%) and younger people (median 56 years, IQR 47-60 years vs 66 years, IQR 52-77). 72.8% had pneumonia at hospital admission. |
| Vaira LA et al., 2020 20 | Italia | Brief communication: 320 cases | Not reported | Not reported | Anosmia and ageusia associated with fever. Some kind of dysfunction: 19.4% (not accompanied by nasal obstruction or rhinitis symptoms) | |
| Pan L et al., 2020 21 | Hubei, China | Cross-sectional study: 204 hospitalized cases | RT-PCR + for COVID-19 | Increased AST and ALT in the group of patients with ALT (20.4%) and AST (16.5%) digestive symptoms, compared to the group with no ALT (5.9%) and AST (5.0%) digestive symptoms | 50.5% of hospitalized patients had digestive symptoms: loss of appetite (78.64%), diarrhea (34%) and vomiting (3.9%). Concomitantly, 94% had respiratory symptoms: fever (92.23%) and weakness (52.42%) | Descriptive, cross-section and multicenter study. Cases with digestive symptoms had longer hospitalization time in relation to patients without digestive symptoms (9 days vs 7.3 days). However, there was no significant difference in the time of hospital discharge, days in ITU or mortality between the groups . |
| Jin X et al., 2020 22 | Zhejiang, China | Retrospective study with 651 hospitalized cases and clinical/ epidemiological analysis of 74 cases with digestive symptoms | RT-PCR + for COVID-19 | Increase in AST isolated in patients with GI symptoms greater than in those with no GI symptoms (29.35 vs 24.4). No significant different in makers related to CRP infection and procalcitonin | Digestive symptoms (diarrhea, vomiting, nausea) in 11.4% of total cases. Fever (85.54%), coughing (71.62%), sputum (39.19%), fatigue (31.08%) and headache (21.62%) | Retrospective study. Chronic liver disease rate was higher in cases with GI symptoms in relation to those with no GI symptoms (10.81% vs 2.95%). Severe/critical type rate was greater in cases with GI symptoms than in those without symptoms (22.97% vs 8.14%). |
Legend:
RT-PCR: reverse transcription polymerase chain reaction.
COVID-19: disease caused by SARS-CoV-2.
ITU: intensive therapy unit.
CRP: C-reactive protein.
CNS: central nervous system.
PNS: peripheral nervous system.
NS: nervous system.
IQR: interquartile range.
AST: aspartate aminotransferase enzyme.
ALT: alanine aminotransferase enzyme.
GI: gastrointestinal.
vs: versus.
a) Study type determined by the authors, not specified in the article.
According to the Brazilian Ministry of Health, information is still limited for characterizing the spectrum of the clinical disease. The Ministry therefore establishes flu-like syndrome (FS) as being the most common manifestation, this being defined as an acute respiratory clinical picture, characterized by sensation of fever or fever, even if reported, accompanied by coughing, sore throat or runny nose or difficulty in breathing. 7 If breathing difficulties are present, severe acute respiratory syndrome (SARS) may be considered, 8 defined by FS showing dyspnea/breathing discomfort or persistent pressure in the thorax or O 2 saturation below 95% in ambient air or lips or face with a bluish color. 9
According to the World Health Organization (WHO), 2 the initial signs/symptoms of the disease appear like those of influenza, but vary from person to person, and can be mild, in the form of pneumonia, severe pneumonia and SARS. The majority of infected people have the mild form of the disease, with symptoms such as malaise, fever, tiredness, coughing, mild dyspnea, anorexia, sore throat, aching body, headache or blocked nose, some may also have diarrhea, nausea and vomiting. Signs and symptoms in elderly and immunocompromised people may be atypical and worsen rapidly, which can cause death, especially in the case of the elderly and people with pre-existing comorbidities.
The case definitions adopted by the Brazilian Health Ministry were established in February 10 and March 2020, 7 as detailed in Figure 1 . Suspect case definitions were initially based on the occurrence of fever and at least one respiratory sign or symptom, with a history of the person having traveled to places with local transmission or contact with a confirmed case. 11 However, fever is not necessarily present in all affected individuals, 7 considering that elderly people or even people with no comorbidities have not presented this specific sign. Moreover, the criterion for defining fever is not standardized, whereby it can be measured as temperature ≥37.5ºC, 12 temperature ≥37.8ºC, 7 recorded on medical records for hospitalized cases 13 or even reported by the individual without confirmation by measuring their temperature. 7
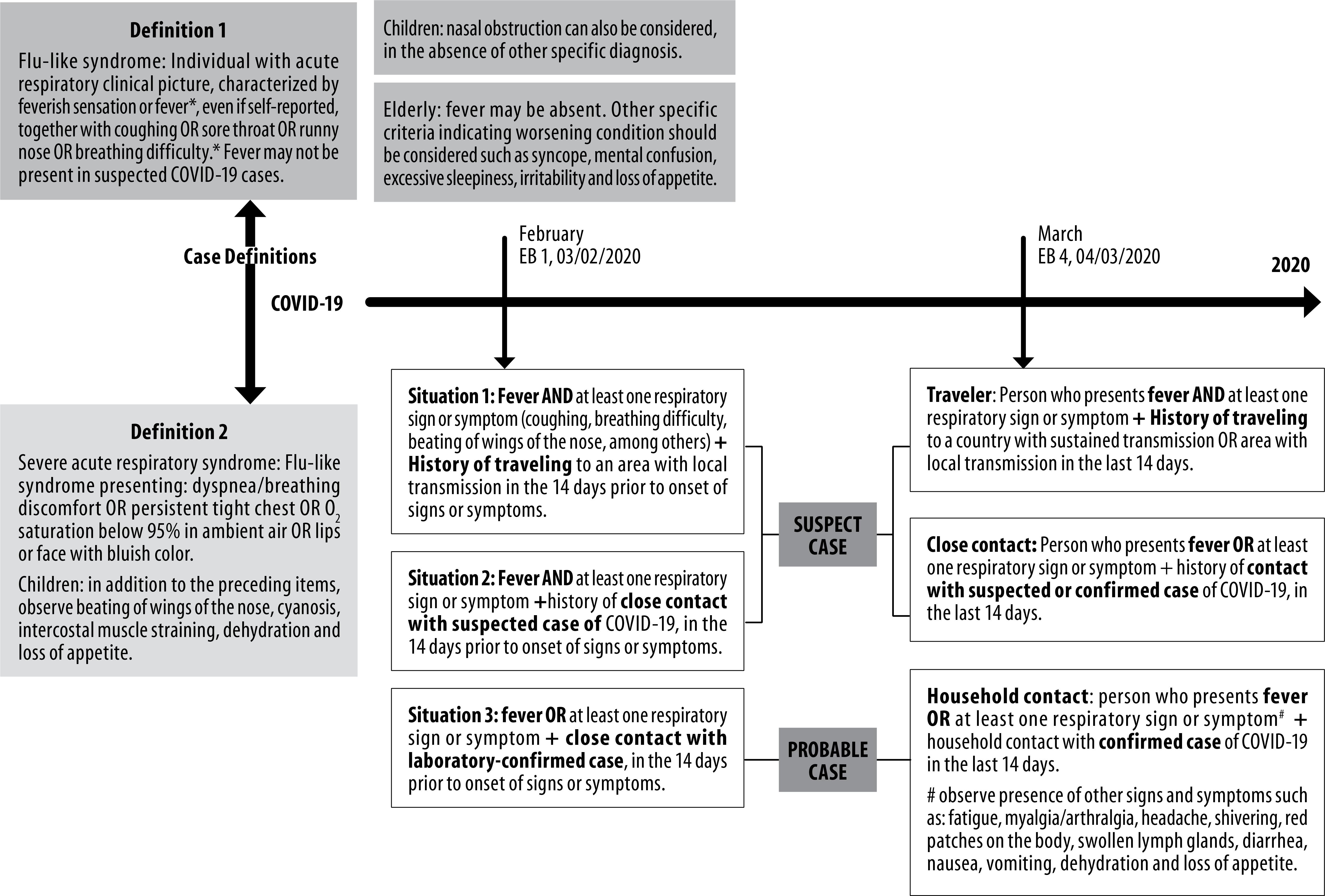
Legend: COVID-19, diseases caused by Sars-CoV-2; EB, Brazilian Health Ministry Epidemiological Bulletin.
Figure 1 – COVID-19 case definitions adopted in Brazil, 2020
Be that as it may, the most common signs and symptoms are considered to be fever (temperature ≥37.8ºC), coughing, dyspnea (breathing difficulty), myalgia and fatigue. 11 A study of 41 confirmed cases in China identified that 98% of them had fever, followed by coughing (76%), dyspnea (55%) and myalgia/fatigue (44%). 14 Wang et al. 15 described 69 cases in China and identified that some 15% of individuals analyzed had fever, coughing and dyspnea. A case report in Seattle, United States, 13 showed that 50% of cases did not have fever and that coughing and dyspnea were the most reported symptoms, accounting for 88% of cases. In a systematic review of clinical, laboratory and image findings for confirmed COVID-19 cases, 16 the most common clinical manifestations were fever (88.7% [95%CI 84.5; 92.9%]), coughing (57.6% [95%CI 40.8; 74.4%]) and dyspnea (45.6% [95%CI 10.9; 80.4%]), although they may not be present. Prevalence of fever was greater in adults than in children. 16
There are also reports of less common symptoms that are hard to measure objectively, such as anosmia (loss of sense of smell), hyposmia (reduction in sense of smell) and ageusia (loss of sense of taste). Specialist organizations propose that anosmia, hyposmia and ageusia should be included as part of screening for SARS-CoV-2 infection, principally in the absence of other respiratory diseases, such as allergic rhinitis and acute or chronic rhinosinusitis. 17 There is evidence of a significant number of people who developed these symptoms and later had positive COVID-19 test results. 18 A study with hospitalized individuals who tested positive for COVID-19 in Italy 19 found that 33.9% of them had either changes to sense of smell or taste while 18.6% had changes to both. Loss of sense of taste occurred in 91% before they were hospitalized. These symptoms were more frequently reported by women (52.6% versus 25%) and by less elderly people (median of 56 years, IQR 47-60 years versus 66 years, IQR 52-77). In Germany, anosmia was found in more than two thirds of individuals studied, while Italian and Swiss doctors are reporting similar symptoms, with many also having ageusia. In South Korea, anosmia was the main symptom in 30% of respondents with COVID-19. 18
In a cross-sectional study with 204 laboratory-confirmed cases in China, 21 gastrointestinal symptoms were reported by 50.5% at the time they were admitted to hospital, in addition to fever and respiratory symptoms. Their symptoms included ageusia, reported by 78.6% of cases, diarrhea in 34% of cases, as well as vomiting (3.9%) and abdominal pain (1.9%). In a retrospective study conducted in the Chinese Province of Zhejiang, 22 with 651 people hospitalized with diagnosis of COVID-19, 11.4% had gastrointestinal symptoms when they were admitted to hospital. The most prevalent digestive symptoms were diarrhea (71.62%), vomiting (14.86%) and nausea (13.51%).
Diagnosis criteria
In the document entitled Guidelines for COVID-19 Diagnosis and Treatment , given the inespecificity and heterogeneity of clinical presentation, the Ministry of Health considers a confirmed case to be a case with conclusive laboratory confirmation of SARS-CoV-2, regardless of signs or symptoms. 11 However, in the absence of confirmatory diagnostic tests for all suspect cases, health services have had to adopt a very sensitive suspect case definition, especially for cases with mild symptoms, considering the symptoms reported by individuals, in view of the recommendation for people not to go to hospitals or health centers for clinical evaluation, in the absence of breathing discomfort as a sign of the disease becoming worse. 8
As such, using the clinical/epidemiological criterion, a suspect FS or SARS case is considered to be when there is a history of close or household contact with a laboratory confirmed COVID-19 case during the seven days prior to onset of symptoms and when it was not possible to perform specific laboratory investigation. As such, any flu-like symptom has been considered to indicate a suspect case, above all with the aim of individual isolation so as to avoid virus transmission. Notwithstanding, it is known that the majority of these cases considered to be suspect will not be confirmed, unless they get worse and need to be hospitalized, or voluntarily have rapid tests available in some places.
According to the Ministry of Health, stratification of the severity of suspect FS cases should take place during a medical consultation, indicating that mild cases (without dyspnea or signs and symptoms of severity) can be accompanied completely by Primary Health Care and Family Health Strategy (PHC/FHS) services in view of these cases being less severe. 8 Those who have FS with dyspnea or signs and symptoms of severity, or together with comorbidities that contraindicate home isolation, need stabilization at in PHC/FHS services and referral to Reference/Urgency/Hospital centers for 24-hour observation or interventions involving greater technological density. For these people who seek care at a health service facility, suspect findings in laboratory tests and in images can be used as indications of the disease, assisting with suspect case diagnosis. 16
Molecular tests, such as reverse transcription polymerase chain reaction (RT-PCR), which identify SARS-CoV-2 virus RNA, should be used between the 3 rd and 7 th day of symptoms using nasopharyngeal secretion samples, in order to ensure greater precision of the method and to reduce false-negative results. 24 Due to the high cost and scarcity of laboratories authorized to perform them, RT-PCR tests are used for hospitalized symptomatic individuals and health workers. Immunochromatographic serological tests, known as rapid tests, have become an option for people with light to moderate symptoms who do not require hospitalization; for the general population, when screening asymptomatic cases; 6 and for observing immunity/recovery of confirmed cases. In this case, rapid tests should be used after seven days following onset of symptoms. 25
Development of a serological response to virus infection depends on the host and takes time. In the case of SARS-CoV-2, initial studies suggest that the majority of cases seroconvert between 7 and 11 days following exposure to the virus. As a result of this natural delay, an antibody test may not be useful in the case of acute disease or for early assessment of infection. Moreover, the sensitivity and specificity of serological tests varies according to the manufacturer. In general, the sensitivity of the tests approved in Brazil by the National Health Surveillance Agency (ANVISA) was greater than 85%, and specificity was greater than 94%. 4 It is important to highlight that diagnostic tests with low sensitivity can result in a higher proportion of false-negative results, and this could interfere in the social isolation measures adopted, principally for asymptomatic individuals, thus having a direct influence on virus transmissibility.
As such, SARS-CoV-2 antibody tests can facilitate contact screening; serological surveillance at the local, regional, state and national level; and identification of those who have already been exposed and may possibly be immune, considering the existence of protective immunity.
Characteristics of case severity
Some COVID-19 cases have serious complications, leading to the need for care in intensive therapy units (ITU) or even leading to death. According to the Ministry of Health, besides the percentage of asymptomatic cases, among those who have COVID-19, around 80% are mild cases, 14% are severe cases and 5% are critical cases. 7 As for more complex cases, they either progress from the initial symptoms mentioned above, or they already manifest SARS-CoV-2 infection through SARS, by having dyspnea or clinical signs such as reduction in saturation or cyanosis. 8 In addition to the higher mortality rate due to SARS, there is also a group considered to be at risk because of greater lethality. Those belonging to this group are: elderly people aged 60 and over, high-risk pregnant women and people with a variety of comorbidities. 9 As such, individuals of all ages who have chronic diseases related to the lungs, asthma, those who currently have tuberculosis or sequelae of previous tuberculosis, diabetes, hypertension, severe obesity, chronic kidney disease, liver disease, immunodeficiency and heart problems also belong to the risk group. Recent studies 12 report diabetes mellitus , systemic arterial hypertension, cerebrovascular disease and age as more decisive risk factors in relation to hospitalization in ITUs and death.
A retrospective study that assessed neurological aspects of confirmed COVID-19 cases 29 indicated that 41.1% were considered severe. Compared to the milder cases, the severe cases were older individuals (58.7 ± 15.0 years versus 48.9 ± 14.7 years), had more comorbidities (42 [47.7%] versus 41 [32.5%]), especially hypertension (32 [36.4%] versus 19 [15.1%]), and had fewer symptoms considered to be typical, such as fever (40 [45.5%] versus 92 [73%]) and coughing (30 [34.1%] versus 77 [61.1%]).
Another study that described the characteristics of cases that died compared to cases that recovered 30 found at least one chronic disease with greater frequency among cases that died (63% of those who died and 39% of those who recovered), whereby the main diseases were: systemic arterial hypertension (48%), cardiovascular diseases (14%) and cerebrovascular diseases (4%), versus 24%, 4% and 0%, respectively, in recovered cases. The following were also found to be more frequent among those who died: dyspnea (62% versus 31%), tight chest (49% versus 30%) and loss of consciousness (22% versus 1%); lymphopenia (39%) and leukocytosis (50%) ( versus 5% and 4% of those who recovered, respectively), saturation ≤93% (64% versus 12%), tachycardia (50% versus 30%) and tachypnea (27% versus 3%), as well as complications that can arise from the length of time spent in ITUs and the need for invasive procedures.
The study conducted by Wang et al. 15 assessed 69 people with COVID-19 in Wuhan, China, and indicated that all those who had saturation ≤90% (n= 14.20%) died, and that those who died were older (median of 70.5 years versus 37 years), with comorbidities such as systemic arterial hypertension (36% versus 7%), cardiovascular disease (36% versus 5%) and diabetes mellitus (43% versus 2%), and had a substantial increase in inflammatory cytokines. Fever was evident at the onset of symptoms (93% versus 85%) and on the 10 th day of illness (64% versus 38%). Dyspnea (50% versus 24%) and lymphopenia (79% versus 32%) were also more frequent in this group.
A study that investigated the characteristics and the prognosis factors of COVID-19 infection in a sample comprised of 339 elderly people (≥60 years old) with positive SARS-CoV-2 test results, 30 found that the number of critical and severe cases was greater in the group analyzed compared to cases under 60 years old. The study indicated that 23.6% were classified as being in a critical state , while a further 46.9% were in a severe state. 30
The Chinese Center for Disease Control and Prevention carried out a study with 1,023 positive COVID-19 cases. 23 Among those who became severely ill, the most common clinical signs were dyspnea, respiratory rate greater than 30 bpm and oxygen saturation under 93%. Among the more critical cases, the signs most found were respiratory insufficiency, septic shock and dysfunction or failure of multiple organs. Lethality was 2.3% in that sample. However, if only the lethality of the critical cases were assessed, the proportion would be much higher, i.e. 49%.
In this review we found that few studies describe the most common signs and symptoms by sex and age, although age is more related to the disease’s severity criteria. It is important to consider that signs and symptoms can vary between the stages of the disease, oscillating between absence of signs and symptoms and septic shock, when the clinical picture becomes worse. It should also be noted that in addition to the diversity of clinical manifestations, some 80% of infected people can remain asymptomatic. It is therefore suggested that suspect cases should be monitored constantly, in view of the manifestations of diverse symptoms, so as not to rule out cases by only considering clinical presentation which, in many cases, is subjective.
Given the imminence of Brazil becoming the world’s new epicenter of the COVID-19 pandemic, it is suggested that health services opt for over-reporting, considering the high sensitivity of the surveillance system, so that whenever signs and symptoms appear that may be related to SARS-CoV-2 infection, isolation measures can be indicated for cases and their contacts, in addition to constant real-time monitoring, based on case investigation and local epidemiological reality. In addition, health services can establish, based on the cases they care for, a set of signs and symptoms that best defines their cases and which guides screening in accordance with the specific situation. Use of telemedicine is a fundamental tool in providing care to suspect and confirmed cases that can stay at home, so as to accompany the progression of their clinical presentation and identify early any worsening of the case, so that appropriate measures can be taken. Whenever possible, it is essential to use molecular or serological diagnostic tests, depending on the day the symptoms started, in addition to laboratory tests and image examinations, to confirm diagnosis of COVID-19.
Final considerations
COVID-19 is a global reality and it is essential to fight against it using the best available evidence. Due to its multiple presentations in all age ranges, the concept of diagnosis continues to be very broad and sensitive, so that it is not possible to define so much as a single obligatory sign/symptom for determining presence of infection. Nevertheless, it appears to be consensus that people with existing comorbidities and people who are older are susceptible to being more intensely affected and having worse disease progression, so that they need to be targeted with preventive actions.
Considering the high percentage of asymptomatic people and people with mild symptoms, who will not be completely captured by the surveillance system, by means of investigation and laboratory confirmation, health services need to take great care with regard to symptom heterogeneity and clinical presentation of the disease. In this situation, nonpharmaceutical prevention measures need to be adopted for the entire population, including wearing facemasks, constant sanitization of hands and environments, in addition to social distancing. It also continues to be essential to increase access to diagnostic tests, in order to have knowledge of the epidemiological situation in each place and achieve better guidance of measures to control virus dissemination.
Brazil continues to be in a state of alert, with the aim of slowing down the new case infection curve so as not to overburden the health system. Further studies need to be conducted so that the case definition becomes more precise in relation to signs and symptoms, assisting classification of the population and guiding the gradual return to routine activities, while complying with indicated protection measures, with the aim of minimizing the consequences of the pandemic.
Referências
1. Zhu N , Zhang D , Wang W , Li X , Yang B , Song J , et al . A novel coronavirus from patients with pneumonia in China, 2019 . N Engl J Med [ Internet ]. 2020 Feb [ cited 2020 Jun 1 ]; 382 ( 8 ): 727 - 33 . Available from: https://doi.org/10.1056/nejmoa2001017 [ Links ]
2. World Health Organization - WHO . Coronavirus disease (COVID-19) pandemic [ Internet ]. Geneva : World Health Organization ; 2019 [ cited 2020 Apr 26 ]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [ Links ]
3. Croda J , Oliveira WK , Frutuoso RL , Mandetta LH , Baia-da-Silva DC , Brito-Sousa JD , et al . COVID-19 in Brazil: advantages of a socialized unified health system and preparation to contain cases . Rev Soc Bras Med Trop [ Internet ]. 2020 Apr [ cited 2020 Jun 1 ]; 53 : e20200167 . Available from: https://doi.org/10.1590/0037-8682-0167-2020 [ Links ]
4. Ministério da Saúde (BR) . Secreataria de Vigilância em Saúde e Ambiente . Acurácia dos testes diagnósticos registrados para a COVID-19: versão 1 [ Internet ]. Brasília : Ministério da Saúde ; 2020 [ citado 2020 jun 1 ]. 19 p. Disponível em: https://www.sbmfc.org.br/wp-content/uploads/2020/04/Acur_cia_dos_testes_para_COVID_19_1586558625.pdf.pdf [ Links ]
5. Zitek T . The appropriate use of testing for COVID-19 . West J Emerg Med [ Internet ]. 2020 Apr [ cited 2020 Jun 1 ]; 21 ( 3 ): 470 – 2 . Available from: https://doi.org/10.5811/westjem.2020.4.47370 [ Links ]
6. Tolia VM , Chan TC , Castillo EM . Preliminary results of initial testing for coronavirus (COVID-19) in the emergency department . West J Emerg Med [ Internet ]. 2020 Mar [ cited 2020 Jun 1 ]; 21 ( 3 ): 503 - 6 . Available from: https://doi.org/10.5811/westjem.2020.3.47348 [ Links ]
7. Ministério da Saúde (BR) . Secretaria de Vigilância em Saúde . Centro de Operações de Emergências em Saúde Pública . Doença pelo coronavírus 2019: ampliação da vigilância, medidas não farmacológicas e descentralização do diagnóstico laboratorial . Bol Epidemiol [ Internet ]. 2020 mar [ citado 2020 jun 1 ]; 5 . Disponível em: http://maismedicos.gov.br/images/PDF/2020_03_13_Boletim-Epidemiologico-05.pdf [ Links ]
8. Ministério da Saúde (BR) . Secretaria de Vigilância em Saúde . Guia de vigilância epidemiológica emergência de saúde pública de importância nacional pela doença pelo coronavírus 2019 [ Internet ]. Brasília : Ministério da Saúde ; 2020 [ citado 2020 jun 1 ]. 34 p. Disponível em: https://www.saude.gov.br/images/pdf/2020/April/06/GuiaDeVigiEp-final.pdf [ Links ]
9. Ministério da Saúde . Secretaria de Vigilância em Saúde . Centro de Operações de Emergências em Saúde Pública . Especial: doença pelo coronavírus 2019 . Bol Epidemiol [ Internet ]. 2020 abr [ citado 2020 jun 1 ]; 7 . Disponível em: https://www.saude.gov.br/images/pdf/2020/April/06/2020-04-06---BE7---Boletim-Especial-do-COE---Atualizacao-da-Avaliacao-de-Risco.pdf [ Links ]
10. Ministério da Saúde (BR) . Secretaria de Vigilância em Saúde . Centro de Operações de Emergências em Saúde Pública . Infecção humana pelo novo coronavírus (2019-nCoV) . Bol Epidemiol [ Internet ]. 2020 jan [ citado 2020 jun 1 ]; 1 . Disponível em: https://www.saude.gov.br/images/pdf/2020/janeiro/28/Boletim-epidemiologico-SVS-28jan20.pdf [ Links ]
11. Ministério da Saúde (BR) . Secreataria de Vigilância em Saúde e Ambiente . Diretrizes para diagnóstico e tratamento da COVID-19 [ Internet ]. Brasília : Ministério da Saúde ; 2020 [ citado 2020 jun 1 ]. 87 p. Disponível em: https://portalarquivos.saude.gov.br/images/pdf/2020/May/08/Diretriz-Covid19-v4-07-05.20h05m.pdf [ Links ]
12. Guan W , Ni Z , Hu Y , Liang W , Ou C , He J , et al . Clinical characteristics of coronavirus disease 2019 in China . N Engl J Med [ Internet ]. 2020 Apr [ cited 2020 Jun 1 ]; 382 ( 18 ): 1708 - 20 . Available from: https://doi.org/10.1056/NEJMoa2002032 [ Links ]
13. Bhatraju PK , Ghassemieh BJ , Nichols M , Kim R , Jerome KR , Nalla AK , et al . Covid-19 in critically Ill patients in the Seattle Region — case series . N Engl J Med [ Internet ]. 2020 Mar [ cited 2020 Jun 1 ]; 382 : 2012 - 22 . Available from: https://doi.org/10.1056/NEJMoa2004500 [ Links ]
14. Huang C , Wang Y , Li X , Ren L , Zhao J , Hu Y , et al . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China . Lancet [ Internet ]. 2020 Feb [ cited 2020 Jun 1 ]; 395 ( 10223 ): 497 - 506 . Available from: https://doi.org/10.1016/s0140-6736(20)30183-5 [ Links ]
15. Wang Z , Yang B , Li Q , Wen L , Zhang R . Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China . Clin Infect Dis [ Internet ]. Fothcoming . 2020 Mar [ cited 2020 Jun 1 ]. Available from: https://doi.org/10.1093/cid/ciaa272 [ Links ]
16. Rodriguez-Morales AJ , Cardona-Ospina JA , Gutiérrez-Ocampo E , Villamizar-Peña R , Holguin-Rivera Y , Escalera-Antezana JP , et al . Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis . Travel Med Infect Dis [ Internet ]. 2020 Mar-Abr [ cited 2020 Jun 1 ]; 34 : 101623 . Available from: https://doi.org/10.1016/j.tmaid.2020.101623 [ Links ]
17. Sociedade Brasileira de Cirurgia de Cabeça e Pescoço - SBCCP . Anosmia, hiposmia e ageusia - sintomas na infecção por COVID-19? São Paulo : Sociedade Brasileira de Cirurgia de Cabeça e Pescoço ; 2020 [ citado 2020 abr 8 ]. Disponível em: http://sbccp.org.br/anosmia-hiposmia-e-ageusia-sintomas-na-infeccao-por-covid-19/ [ Links ]
18. Gautier JF , Ravussin Y . A new symptom of COVID-19: loss of taste and smell . Obesity [ Internet ]. 2020 Apr [ cited 2020 Apr 8 ]; 28 ( 5 ): 848 . Available from: https://doi.org/10.1002/oby.22809 [ Links ]
19. Giacomelli A , Pezzati L , Conti F , Bernacchia D , Siano M , Oreni L , et al . Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study . Clin Infect Dis [ Internet ]. Fothcoming 2020 [ cited 2020 Jun 1 ]. Available from: https://doi.org/10.1093/cid/ciaa330 [ Links ]
20. Vaira LA , Salzano G , Deiana G , De Riu G . Anosmia and ageusia: common findings in COVID-19 patients . Laryngoscope [ Internet ]. Forthcoming 2020 Apr [ cited 2020 Jun 1 ]. Available from: https://doi.org/10.1002/lary.28692 [ Links ]
21. Pan L , Mu M , Yang P , Sun Y , Yan J , Li P , et al . Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study . Am J Gastroenterol [ Internet ]. 2020 May [ cited 2020 Jun 1 ]; 115 ( 5 ): 766 - 73 . Available from: https://doi.org/10.14309/ajg.0000000000000620 [ Links ]
22. Jin X , Lian J-S , Hu J-H , Gao J , Zheng L , Zhang Y-M , et al . Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms . Gut [ Internet ]. 2020 Jun [ cited 2020 Jun 1 ]; 69 ( 6 ): 1002 - 9 . Available from: https://doi.org/10.1136/gutjnl-2020-320926 [ Links ]
23. Wu Z , McGoogan JM . Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in china: summary of a report of 72 314 cases from the chinese center for disease control and prevention . JAMA [ Internet ]. 2020 Fev [ cited 2020 Jun 1 ]; 323 ( 13 ): 1239 - 42 . Available from: https://doi.org/10.1001/jama.2020.2648 [ Links ]
24. Woelfel R , Corman VM , Guggemos W , Seilmaier M , Zange S , Mueller MA , et al . Clinical presentation and virological assessment of hospitalized cases of coronavirus disease 2019 in a travel-associated transmission cluster . medRxiv [ Internet ]. Forthcoming 2020 Mar [ cited 2020 Jun 1 ]. Available from: https://doi.org/10.1101/2020.03.05.20030502 [ Links ]
25. Hadaya J , Schumm M , Livingston EH . Testing individuals for coronavirus disease 2019 (COVID-19) . JAMA [ Internet ]. 2020 Apr [ cited 2020 Jun 1 ]; 323 ( 19 ): 1981 . Available from: https://doi.org/10.1001/jama.2020.5388 [ Links ]
26. Yang J , Zheng Y , Gou X , Pu K , Chen Z , Guo Q , et al . Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis . Int J Infect Dis [ Internet]. 2020 May [ cited 2020 Jun 1 ]; 94 : 91 - 5 . Available from: https://doi.org/10.1016/j.ijid.2020.03.017 [ Links ]
27. Yang X , Yu Y , Xu J , Shu H , Xia J , Liu H , et al . Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study . Lancet Respir Med [ Internet ]. 2020 May [ cited 2020 Jun 1 ]; 8 ( 5 ): 475 - 81 . Available from: https://doi.org/10.1016/S2213-2600(20)30079-5 [ Links ]
28. Zhang J-J , Dong X , Cao Y-Y , Yuan Y-D , Yang Y-B , Yan Y-Q , et al . Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China . Allergy [ Internet ]. Forthcoming 2020 Feb [ cited 2020 Jun 1 ]. Available from: https://doi.org/10.1111/all.14238 [ Links ]
29. Mao L , Wang M , Chen S , He Q , Chang J , Hong C , et al . Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study . JAMA Neurol [ Internet ]. Forthcoming 2020 Apr [ cited 2020 Jun 1 ]. Available from: https://www.medrxiv.org/content/10.1101/2020.02.22.20026500v1.article-metrics [ Links ]
30. Chen T , Wu D , Chen H , Yan W , Yang D , Chen G , et al . Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study . BMJ [ Internet ]. 2020 Mar [ cited 2020 Jun 1 ]; 368 : m1091 . Available from: https://doi.org/10.1136/bmj.m1091 [ Links ]
Received: April 29, 2020; Accepted: May 26, 2020











 texto en
texto en 


