Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.4 Brasília 2020 Epub 23-Jul-2020
http://dx.doi.org/10.5123/s1679-49742020000400006
Original article
Common mental disorders and associated factors among people with leprosy: cross-sectional analysis in Cuiabá, Brazil, 2018 *
1 Universidade Federal de Mato Grosso, Programa de Pós-graduação em Saúde Coletiva, Cuiabá, MT, Brazil
2 Universidade Federal de Mato Grosso, Instituto de Saúde Coletiva, Cuiabá, MT, Brazil
Objective. To analyze the occurrence of common mental disorders (CMDs) and associated factors in people with leprosy with complications in the state of Mato Grosso, Brazil, in 2018. Methods. This was a cross-sectional study with people attending Júlio Müller University Hospital. The Self-Report-Questionnaire (SRQ-20) was used. Poisson regression analysis was performed to estimate prevalence ratios (PR) and 95% confidence intervals (95%CI). Results. Among 206 people with leprosy, CMDs were found in 70.4% (95%CI 61.10;76.67) and were associated with the female sex (PR=1.29 – 95%CI 1.09;1.53), the 26-45 age range (PR=1.52 – 95%CI 1.09;2.11) and the 46-60 age range (PR=1.40 – 95%CI 1.01;1.95), low family income (PR=1.25 – 95%CI 1.05;1.49), and unsatisfactory quality of life in the physical domain (PR=3.03 – 95%CI 1.12;8.19) and the psychological domain (PR=1.91; 95%CI 1.40;2.61). Conclusion. CMDs were frequent and associated with female sex, productive age group, low income and unsatisfactory quality of life. Actions aimed at mental health in this population group are necessary.
Key words: Mental Disorders; Leprosy; Cross-Sectional Studies, Epidemiology
Introduction
Leprosy is still a Public Health problem in several countries worldwide, including Brazil. 1 It is caused by the Mycobacterium leprae bacillus and manifests itself in the form of skin, mucous membrane and nerve lesions and, at an advanced state, can affect other organs. 1 Leprosy can affect people of any sex or age, ranging from children to the elderly, with a high potential for causing physical disabilities and deformities, as well as complications during treatment. 2
Between 2014 and 2018, 140,578 new leprosy cases were notified in Brazil, 55.2% of which were male. 2 In the same period, the World Health Organization (WHO) informed that new cases had been detected in 23 countries, with Brazil in second place – with 28,660 new cases –, after India, with 120,334 new cases, despite the control policies adopted. 3
Occurrence of leprosy in the state of Mato Grosso is historic and has become worse since the 1970s, 4 as a result of social changes arising from disorderly land occupation. Currently, Mato Grosso has the highest number of new cases and is in second place among the Brazilian states, with an overall detection rate of 62 cases per 100,000 inhabitants. Its capital city, Cuiabá, recorded a rate of 46.28 cases per 100,000 inhab. in 2019. 2
According to WHO, in the definition provided in the Global Leprosy Strategy 2016-2020, 5 effective control of the disease will be achieved through action strategies that are not just limited to detection of new cases, but rather also have a more solid medical care component and policies giving greater visibility and weight to human and social aspects related to reducing stigma and promoting the inclusion of people with leprosy. 1
Standing out among WHO 1 and Brazilian Health Ministry 5 recommendations for leprosy control is the appearance of clinical complications, including adverse reactions to treatment, leprosy reactions, relapses, need for surgical rehabilitation, and doubts as to diagnosis, these being situations when the individual needs to be referred to reference services.
Both diagnosis and complications due to leprosy can cause feelings of weakness, fear of social exclusion and mental problems. 1 In Bangladesh, 6 between 2002 and 2003, high prevalence of mental problems was found among people with leprosy when compared to the general population, with greater frequency of depression and stigma associated with the state of depression. The proportion of moderate and severe symptoms of depression was 43.1% among people with leprosy receiving care at a reference center in Bauru, a municipality in the state of São Paulo. 7
In the Brazilian context there is considerable scientific production about leprosy, including with regard to the state of Mato Grosso. 8 Notwithstanding, little is known about the mental health of people in Mato Grosso with complications 5 attributed to leprosy.
The objective of this study was to analyze occurrence of common mental disorders and associated factors in people with leprosy and complications in the state of Mato Grosso, Brazil, in 2018.
Methods
This cross-sectional study is part of a larger study on the quality of life of people with leprosy conducted between January and May 2018, 10 based on previous study. 11
In 2010, Mato Grosso had a population of 3,035,122 inhabitants distributed over 141 municipalities and a human development index of 0.725. 12 In 2016, 2,550 people were diagnosed with leprosy in Mato Grosso, 10 30.0% of whom (765) had complications during treatment, according to Brazilian National Health System (SUS) criteria for Planning and Programming Health Actions and Services. 13
With regard to this study, the participants came from 16 health regions of the state of Mato Grosso, 12 with confirmed diagnosis and referral to the Federal University of Mato Grosso Júlio Müller University Hospital (HUJM/UFMT), a state reference unit for leprosy treatment and care for complications 2 caused by the disease.
Confirmatory leprosy diagnosis was performed according to WHO recommendations, 3 and was based on the presence of at least one of the three signs characteristic of the disease: (i) definitive loss of sensation in an area of pale skin (hypo-pigmented) or reddish skin; (ii) thickened or increased peripheral nerve, with loss of sensation and/or weakness of the muscles related to this nerve; or (iii) presence of acid-fast bacilli in blanched skin folds. Complications may occur during the treatment period and these cases are referred to reference units duly equipped to provide this care. 2
Convenience sampling was used in view of lack of prediction about cases referred for care at the HUJM/UFMT infectious diseases outpatient department. As such, cases present at the department for medical consultations were invited to take part in the study until the sample size was reached. Data collection took place between January and May 2018.
People included in the study were those aged 18 or over, diagnosed as having leprosy, with an appointment for medical care at the HUJM/UFMT infectious diseases outpatient department; those who had cognitive-behavioral incapacity or a clinical complication that prevented them from answering the instrument used during the interview were excluded from the study.
The study outcome was the presence of common mental disorders (CMDs), presented as a dichotomous variable (yes; no) and assessed using the self-report-questionnaire (SRQ-20). The SQR-20, developed by WHO and adapted and validated for the Brazilian population by Mari & Williams in 1986, 14 is used to identify the best cut-off points among males and females, with the aim of detecting mental disorders. It is comprised of 20 questions, of which 4 are about physical symptoms and 16 are about psycho-emotional disorders. In this study, the SQR-20 cut-off points were 7 or more affirmative answers for females and 6 or more affirmative answers for males.
The other variables studied included sociodemographic characteristics: sex (male; female); age (in years: 18-25, 26-45, 46-60, 61 or over); race/skin color (white; black; brown; yellow/indigenous); schooling (in years of study: ≤9; >9); marital status (single; married/separated/widowed/other); family income (in minimum wages [MW], in the sum of BRL 954: ≤1 MW; >1 MW); whether they worked before leprosy diagnosis (yes; no); and work situation following leprosy diagnosis (unemployed; employed; self-employed; housewife; retired; on social security leave from work (National Institute of Social Security [INSS]).
Among the characteristics related to health history, quality of life was assessed using the short version of the quality of life assessment instrument developed by WHO, i.e. World Health Organization Quality of Life-bref (WHOQOL-bref), 15 in relation to the physical, psychological, social relationships and environment domains. The WHOQOL-bref is comprised of 26 question, with likert scale answer options varying from 1 to 5, depending on degree of satisfaction in relation to perception of quality of life: perceived as ‘unsatisfactory’ for scores from 1 to 3.9; and ‘satisfactory’ for scores from 4 to 4.9.
Use of psychoactive substances was assessed by the instrument referred to as the ‘Alcohol, Smoking and Substance Involvement Screening Test’ (ASSIST), 16 comprised of eight questions: the first seven questions refer to use of tobacco, alcohol, cannabis, cocaine, amphetamine type stimulants, inhalants, hypnotics/sedatives, hallucinogens and opioids; while the eighth and final question refers to injecting drug use resulting in dependency. As such, the following question was asked: During the last three months, how frequently have you had a strong desire or urgent need to consume any of the drugs mentioned above? , with the following answer alternatives: never; monthly; weekly; daily. A score of zero was given to negative answers as to desire to consume any substance (no); while a score above zero was given to desire to consume a substance (yes).
Presence of other morbidities was measured by asking the question Do you have any other illness? with ‘yes’ or ‘no’ as answer options; if yes, what illness do you have?
A pilot test was carried out with five people who were waiting to be seen at the outpatient department, to check whether they understood the questions, train the interviewers, prevent biases and ensure that the approach was in keeping with the ethical principles for research with human beings.
As the sample size for the original study 10 was not determined for the CMDs outcome, the power of the sample to investigate factors associated with CMDs was calculated a posteriori . As such, the sample size was defined as being 206 people, the ratio between exposed and non-exposed as 0.4, with prevalence of 0.8 and 0.60 for exposed and non-exposed, respectively, and alpha as 0.05, resulting in power of 79%.
The descriptive analysis was performed using SPSS version 20.0; this process started with descriptive analyses, by calculating absolute and relative frequencies for the categorical variables and mean and standard deviation (DP) for the continuous variables. Following this the crude prevalence ratios ( crude PR) and adjusted prevalence ratios ( adjusted PR) were calculated and their respective 95% confidence intervals (95%CI) were estimated, using the Poisson regression model with robust estimate of variance. All variables with a p-value <0.20 in the bivariate analysis were included in the multiple regression analysis; a model was built with all the variables and then one variable was removed at a time, starting with the least significant. Variables with p<0.05 were kept in the final model.
The study project was approved by the Júlio Müller University Hospital / Federal University of Mato Grosso Human Research Ethics Committee: Opinion No. 2.038.402/CEP/HUJM, dated April 28 th 2017. All participants were informed about the objectives of the study and signed a Free and Informed Consent form before being interviewed.
Results
The sample was comprised of 206 people with complications during treatment of leprosy. Care was provided initially in their health regions in the state of Mato Grosso, before being referred to the Federal University of Mato Grosso Júlio Müller University Hospital, which is accredited by the Ministry of Health for specialized care provision ( Figure 1 ). All those invited agreed to take part in the study and no one was excluded. CMDs prevalence of 70.4% (95%CI 61.10;76.67) was found in the sample ( Figure 2 ).
Figure 1 – Sample selection process for the study on common mental disorders in people with leprosy receiving care at the Júlio Müller University Hospital Infectious Diseases Outpatient Department, Cuiabá, Mato Grosso, 2018
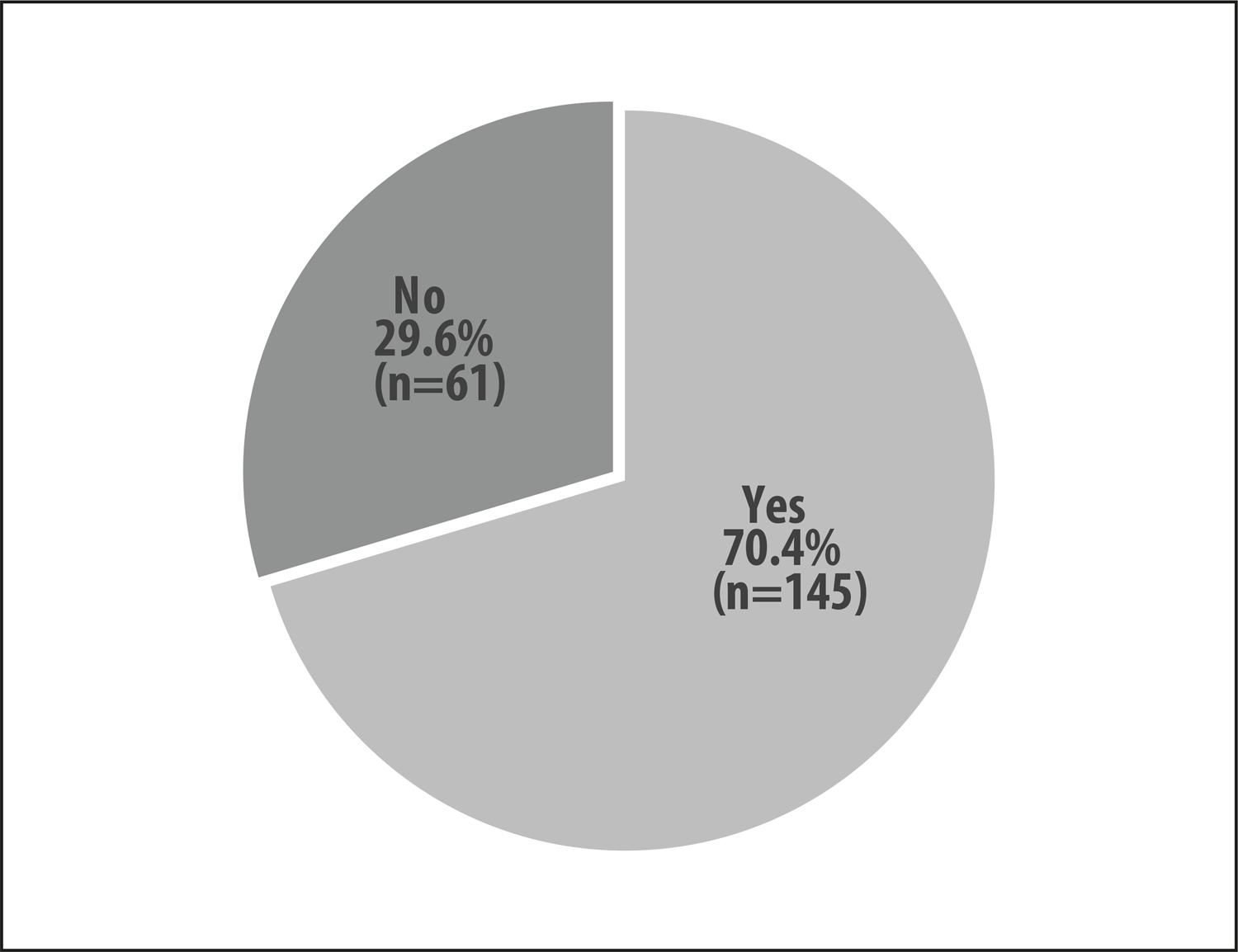
Figure 2 – Prevalence (%) of common mental disorders among people with leprosy with complications, receiving care at the Júlio Müller University Hospital Infectious Diseases Outpatient Department, Cuiabá, Mato Grosso, 2018
Mean age of the interviewed cases was 49 years (SD±14). The largest proportions of participants came from the Center-North Mato Grosso health region (59.7%), were male (52.4%), in the 46-60 year age range (43.2%), of brown race/skin color (53.4%), with up to 9 years of study (56.3%), were married or living in other marital arrangements (68.0%) and with family income of up to one minimum wage (55.3%); 75.7% had worked before being diagnosed as having leprosy and following this 28.6% (of the participants) became unemployed, 15.5% retired and 14.1% requested leave from work from the INSS ( Table 1 ).
Table 1 – Distribution, prevalence ratio and 95% confidence interval (95%CI) of common mental disorders, according to sociodemographic variables among people with leprosy receiving care at the Júlio Müller University Hospital Infectious Diseases Outpatient Department, Cuiabá, Mato Grosso, 2018
| Variables | n (%) | crude PR b | p-value c | adjusted PR b | p-value c | |
|---|---|---|---|---|---|---|
|
|
|
|||||
| n (%) | (95%CI) | (95%CI) | ||||
| Health region | ||||||
|
| ||||||
| Center-north | 123 (59.7) | 84 (68.3) | 1.02 (0.93;1.13) | 0.661 | – | – |
| North | 30 (14.6) | 21 (70.0) | 1.12 (0.77;1.61) | |||
| West | 22 (10.7) | 17 (77.3) | 1.29 (0.72;2.30) | |||
| South | 24 (11.7) | 19 (79.2) | 1.32 (0.74;2.33) | |||
| East | 7 (3.3) | 4 (57.1) | 1.00 | |||
|
| ||||||
| Sex | ||||||
|
| ||||||
| Female | 98 (47.6) | 80 (81.6) | 1.86 (1.23;2.88) | <0.001 | 1.29 (1.09; 1.53) | 0.003 |
| Male | 108 (52.4) | 65 (60.2) | 1.00 | 1.00 | ||
|
| ||||||
| Age range (years) | ||||||
|
| ||||||
| 18-25 | 14 (6.8) | 5 (35.7) | 0.62 (0.24;1.61) | <0.001 | 0.67 (0.32;1.40) | 0.016 |
| 26-45 | 64 (31.1) | 51 (79.7) | 1.76 (1.13;2.75) | 1.52 (1.09;2.11) | ||
| 46-60 | 89 (43.2) | 69 (77.5) | 1.51 (1.09;2.09) | 1.40 (1.01;1.95) | ||
| ≥61 | 39 (18.9) | 20 (51.3) | 1.00 | 1.00 | ||
|
| ||||||
| Race/skin color | ||||||
|
| ||||||
| Black | 41 (19.9) | 31 (75.5) | 1.03 (0.60;1.77) | 0.389 | – | – |
| Brown | 110 (53.4) | 73 (50.3) | 0.88 (0.70;1.09) | |||
| White | 55 (26.7) | 41 (74.5) | 1.00 | |||
|
| ||||||
| Schooling (years of study) | ||||||
|
| ||||||
| ≤9 | 116 (56.3) | 83 (71.6) | 1.05 (0.80;1.36) | 0.678 | – | – |
| >9 | 90 (43.7) | 62 (68.9) | 1.00 | |||
|
| ||||||
| Marital status | ||||||
|
| ||||||
| Married/separated/widowed/other | 140 (68.0) | 101 (72.1) | 1.08 (0.87;1.35) | 0.421 | – | – |
| Single | 66 (32.0) | 44 (66.7) | 1.00 | |||
|
| ||||||
| Family income (in minimum wages) | ||||||
|
| ||||||
| ≤1 Minimum wages | 114 (55.3) | 88 (77.2) | 1.42 (1.03;1.95) | 0.017 | 1.25 (1.05;1.49) | 0.011 |
| >1 Minimum wages | 92 (44.7) | 57 (62.0) | 1.00 | 1.00 | ||
|
| ||||||
| Worked before leprosy diagnosis | ||||||
|
| ||||||
| Yes | 156 (75.7) | 114 (73.1) | 0.83 (0.51;1.35) | 0.135 | – | – |
| No | 50 (24.3) | 31 (62.0) | 1.00 | |||
|
| ||||||
| Work situation following leprosy diagnosis | ||||||
|
| ||||||
| Unemployed | 59 (28.6) | 46 (78.0) | 1.17 (0.93;1.47) | 0.414 | – | – |
| Self-employed | 16 (7.8) | 10 (62.5) | 0.94 (0.61;1.43) | |||
| Housewife | 16 (7.8) | 12 (75.0) | 1.12 (0.80;1.58) | |||
| Retired | 32 (15.5) | 19 (59.4) | 0.89 (0.63;1.25) | |||
| Social security (INSS) leave | 29 (14.1) | 22 (75.9) | 1.14 (0.86;1.50) | |||
| Employed | 54 (26.2) | 36 (66.7) | 1.00 | |||
a) CMDs: common mental disorder.
b) PR: prevalence ratio.
c) Wald Test - Poisson regression with robust variance.
Association between CMDs and sociodemographic variables was found ( Table 1 ), being significantly greater in females (PR=1,86 – 95%CI 1.23;2.88), in those in the 26-45 age range (PR=1.76 – 95%CI 1.13;2.75) and the 46-60 age range (PR=1,51 – 95%CI 1.09;2.09), and those with family income less than or equal to one minimum wage (PR=1.42 – 95%CI 1.03;1.95).
In Table 2 , it can be seen that 20.4% stated using some form of psychoactive substance and 33.0% reported having another morbidity. With regard to quality of life in the all domains studied, the majority of these people with leprosy rated it as being unsatisfactory. Association between quality of life and CMDs was found for all domains, although the prevalence ratio was greater for the psychological domain (PR=2.03 – 95%CI 1.49;1.77). Among the respondents, 73.8% of those with CMDs stated using some form of psychoactive substance and 77.9% self-reported other morbidities, although these factors were not associated with CMDs.
Table 2 – Distribution, prevalence ratio and 95% confidence interval (95%CI) of common mental disorders, according to health conditions among people with leprosy receiving care at the Júlio Müller University Hospital Infectious Diseases Outpatient Department, Cuiabá, Mato Grosso, 2018
| Variables | n (%) | CMDsª | crude PR b | p-value c | adjusted PR b | p-value c |
|---|---|---|---|---|---|---|
|
|
|
|||||
| n (%) | (95%CI) | (95%CI) | ||||
| Quality of life - physical domain | ||||||
|
| ||||||
| Unsatisfactory | 191 (92.7) | 142 (74.3) | 1.21 (1.07;1.38) | <0.001 | 3.03 (1.12;8.19) | 0.028 |
| Satisfactory | 15 (7.3) | 3 (20.0) | 1.00 | 1.00 | ||
|
| ||||||
| Quality of life – psychological domain | ||||||
|
| ||||||
| Unsatisfactory | 146 (70.9) | 121 (82.9) | 2.03 (1.49;1.77) | <0.001 | 1.91 (1.40;2.61) | <0.001 |
| Satisfactory | 60 (29.1) | 24 (40.0) | 1.00 | 1.00 | ||
|
| ||||||
| Quality of life – social relationships domain | ||||||
|
| ||||||
| Unsatisfactory | 122 (59.2) | 96 (78.7) | 1.55 (1.13;2.12) | 0.001 | – | – |
| Satisfactory | 84 (40.8) | 49 (58.3) | 1.00 | |||
|
| ||||||
| Quality of life – environment domain | ||||||
|
| ||||||
| Unsatisfactory | 187 (90.8) | 38 (73.8) | 1.18 (1.04;1.34) | <0.001 | – | – |
| Satisfactory | 19 (9.2) | 7(36.8) | 1.00 | |||
|
| ||||||
| Use of psychoactive substances | ||||||
|
| ||||||
| Yes | 42 (20.4) | 31 (73.8) | 1.18 (0.63;2.20) | 0.570 | – | – |
| No | 164 (79.6) | 114 (69.5) | 1.00 | |||
|
| ||||||
| Other morbidity | ||||||
|
| ||||||
| Yes | 68 (33.0) | 53 (77.9) | 1.48 (0.91;2.92) | 0.095 | – | – |
| No | 138 (67.0) | 92 (66.7) | 1.00 | |||
a) CMDs: common mental disorder.
b) PR: prevalence ratio.
c) Wald Test - Poisson regression with robust variance.
In the adjusted regression model ( Table 1 ), the highest PR values were found for the 26-45 age group (PR=1.52 – 95%CI 1.09;2.11) and the 46-60 age group (PR=1.40 – 95%CI 1.01;1.95), females (PR=1.29 – 95%CI 1.09;1.53), low family income (PR=1.25 – 95%CI 1.05;1.49) and unsatisfactory quality of life for the physical domain (PR=3.03 – 95%CI 1.12;8.19) and for the psychological domain (PR=1.91 – 95%CI 1.40;2.61), as shown in Table 2 .
Discussion
Among people with leprosy having treatment for complications at a reference outpatient department in the state of Mato Grosso, high frequency of CMDss was associated with the female sex, age range, low family income and unsatisfactory quality of life with regard to the physical and psychological domains.
CMDs etiology is complex and involves biological and psychological factors, 17 as well as characteristics of the socioeconomic context. Prevalence of people with CMDs in this study was higher than that found among health workers 18 also assessed using SRQ-20. Although they used a different instrument in a Latin American leprosy reference service, Correa et al. 7 found that 43.1% of individuals had symptoms of depression, suggesting that mental health problem prevalence is greater among people with leprosy than among other groups. Prejudice, stigma and the pain and disabilities caused by the disease help to explain high CMDs prevalence among this group.
A study conducted in an infectious diseases outpatient department concluded that especially among females, leprosy was related to alterations in family and work relationships, as well as affecting body image. 19 Its authors also added that feelings such as fear, anxiety and depression can affect the evolution of the disease, intensifying leprosy reactions. 19
The majority of the study participants were of productive age. In 2010, Lima et al. 20 considered leprosy to be an adult disease, owing to its long incubation period, although the underaged are also susceptible. This conclusion was also reached by other studies with the Brazilian population. 8 The association between being elderly and CMDs may, possibly, be due to the process of aging and consequent decline in the person’s physical condition, 22 favoring the occurrence of other morbidities and complicating even more the clinical picture of a disease like leprosy.
Little attention has been paid to psychosocial characteristics related to leprosy, which can be worsened by sequelae, discrimination and low self-esteem, compromising treatment and reoccurrence of the disease. 6 It is noteworthy, for example, that around 20% of the people assessed in this study stated having felt a strong desire or urgent need to consume some form of psychoactive drugs in the last three months. Chagas & Assis 23 suggest that tobacco consumption reduces hemoglobin, results in lung problems, risk of necrosis (skin lesions, lesions to the hands and/or the feet and/or the eyes) and the appearance of peripheral ulcers caused by the disease. Moreover, it is necessary to carry out studies on the use of psychoactive drugs to avoid abandoning leprosy treatment, for this reason.
In the final model, unsatisfactory quality of life was found to be associated with CMDs with regard to the physical and psychological domains. In 2012, Simões et al., 24 observed 29 people with leprosy in the city of Uberaba, Minas Gerais state, and found that the physical domain was the domain that least contributed to quality of life. The literature shows that leprosy, generally, causes a series of neurological manifestations, whereby pain is a symptom that appears when larger nerves are impaired. Its presence as a limiting factor for quality of life has also been reported in other studies. 25
The relationship between environmental conditions and quality of life was also found in a comparative study between individuals with leprosy from different environments: riverside dwellers along the River Purus, in the state of Amazonas; and people living in Santo André, an industrial municipality in the metropolitan region of São Paulo city. 11 In 2010, 76.9% of those assessed on the Amazon had impaired quality of life, compared to 19% of those assessed in Santo André. 11 Such distinct distributions may, possibly, be attributed to the conditions – of greater or lesser precariousness – of the populations studied.
The psychological domain reveals its most explicit facet through negative feelings. In 2008, among 120 people in treatment for leprosy in Belo Horizonte, the state capital of Minas Gerais,apart from pain and the discomfort of physical impairment, survival was marked by the presence of psychological suffering. 27 Today, people in treatment for leprosy can have psychotherapy sessions with qualified professionals on the SUS, which contributes to reduction of CMDs. 2
The lower association found with CMDs and unsatisfactory quality of life in the social relationships domain is not corroborated by other studies. However, both in Uberaba, in 2012, 24 and in Belo Horizonte, in 2008, 27 quality of life was found to be impaired due to isolation and social and economic difficulties, among other factors, in view of the changes caused by leprosy.
The results of this study should be analyzed with caution. Its cross-sectional design makes it impossible to establish temporality for the associations studied, and reverse causality must be considered. Another limitation of the study relates to the target population, represented by a convenience sample from an infectious diseases outpatient department of just one hospital, thus limiting the external validity of the results. Notwithstanding, the sample had sufficient power for the analyses of association. It is also possible that there may be information biases due to imprecise answers, related to stigma and prejudice which may have been experienced, as well as to the anxiety of those who are waiting for their medical appointment at the time they are interviewed.
In conclusion, occurrence of CMDs in people with leprosy was found to be associated with females, the economically active age range, low socioeconomic level and unsatisfactory quality of life for the physical and psychological domains. As such, the need is highlighted for health professionals to pay greater attention to social and psychological care provided to people with leprosy, supporting them and helping to improve their quality of life, so as to minimize the adversities imposed by the disease. We hope that this study will contribute both to public policies and to comprehensive care practices for people with leprosy.
REFERENCES
1. World Health Organization - WHO. Global leprosy strategy 2016–2020: accelerating towards a leprosy-free world – monitoring and evaluation guide [Internet]. Geneva: World Health Organization; 2017 [cited 2020 Feb 14]. 90 p. Available from: https://apps.who.int/iris/bitstream/handle/10665/254907/9789290225492-eng.pdf?sequence=1&isAllowed=y [ Links ]
2. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Hanseníase. Bol Epidemiol [Internet]. 2020 jan [citado 2020 fev 14];número especial:1-51. Disponível em: https://www.saude.gov.br/images/pdf/2020/janeiro/31/Boletim-hanseniase-2020-web.pdf [ Links ]
3. World Health Organization - WHO. Global leprosy update, 2018: moving towards a leprosy-free world. WER [Internet]. 2019 Aug [cited 2019 Oct 31];(35/36):389-411. Available from: https://apps.who.int/iris/bitstream/handle/10665/326776/WER9435-36-389-411-en-fr.pdf?sequence=1&isAllowed=y [ Links ]
4. Magalhães MCC , Santos ES , Queiroz ML , Lima ML , Borges RCM , Souza MS , et al . Migração e hanseníase em Mato Grosso . Rev Bras Epidemiol [Internet]. 2011 set [citado 2020 jun 16]; 14 ( 3 ): 386 - 97 . Disponível em: http://dx.doi.org/10.1590/S1415-790X2011000300004 [ Links ]
5. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Guia de vigilância em saúde: volume único [Internet]. 2. ed. Brasília: Ministério da Saúde; 2019 [citado 2019 dez 31]. 740 p. Disponível em: https://portalarquivos2.saude.gov.br/images/pdf/2019/junho/25/guia-vigilancia-saude-volume-unico-3ed.pdf [ Links ]
6. Tsutsumi A, Izutsu T, Islam MDA, Amed JU, Nakahara S, Takagi F, et al. Depressive status of leprosy patients in Bangladesh: association with self-perception of stigma. Lep Rev [Internet]. 2004 Mar [cited 2020 Feb 15];75(1):57-66. Available from:: https://pubmed.ncbi.nlm.nih.gov/15072127/ [ Links ]
7. Corrêa BJ, Marciano LHSC, Nardi ST, Marques T, Assis TF, Prado RBR. Associação entre sintomas depressivos, trabalho e grau de incapacidade na hanseníase. Acta Fisiatr [Internet]. 2014 [citado 2020 fev 14];21(1):1-5. Disponível em: https://www.actafisiatrica.org.br/detalhe_artigo.asp?id=528 [ Links ]
8. Freitas BHBM, Xavier DR, Cortela DCB, Ferreira SMB . Hanseníase em menores de quinze anos em municípios prioritários, Mato Grosso, Brasil . Rev Bras Epidemiol [Internet]. 2018 ago [cited 2020 jun 15]; 21 :e180016. Disponível em: https://doi.org/10.1590/1980-549720180016 [ Links ]
9. Ferreira SMB , Ignotti E , Gamba MA . Fatores associados à recidiva em hanseníase em Mato Grosso . Rev Saúde Pública [Internet]. 2011 ago [citado 2020 jun 15]; 45 ( 4 ): 756 - 64 . Disponível em: https://doi.org/10.1590/S0034-89102011005000043 [ Links ]
10. Finotti RFC. Qualidade de vida e fatores associados entre pessoas acometidas pela hanseníase do ambulatório de infectologia do Hospital Universitário Júlio Müller [dissertação]. Cuiabá (MT): Instituto de Saúde Coletiva da UFMT; 2018 . Disponível em: https://www.ufmt.br/ufmt/site/noticia/visualizar/42039/Cuiaba [ Links ]
11. Proto RS , Machado Filho CDS , Rehder JRC , Paixão MP , Angelucci RI . Qualidade de vida em hanseníase: análise comparativo entre pacientes da região Amazônica com pacientes da região do ABC, São Paulo, Brasil . An Bras Dermatol [Internet]. 2010 nov-dez [citado 2020 jan 31]: 85 ( 6 ): 939 - 41 . Disponível em: http://dx.doi.org/10.1590/S0365-05962010000600030 [ Links ]
12. Instituto Brasileiro de Geografia e Estatística - IBGE. Sinopse do censo demográfico de 2010 [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2011 [citado 2019 mar 12]. 261 p. Disponível em: https://biblioteca.ibge.gov.br/visualizacao/livros/liv49230.pdf [ Links ]
13. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Regulação, Avaliação e Controle de Sistemas. Critérios e parâmetros para o planejamento e programação de ações e serviços de saúde no âmbito do Sistema Único de Saúde [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2017 mar 24]. v. 1. (Série Parâmetros SUS). Disponível em: http://portalarquivos.saude.gov.br/images/pdf/2015/outubro/02/Crit--rios-e-Par--metros-SUS---Portaria-GM-MS-1631-2015.pdf [ Links ]
14. Mari JJ , Willians PA . A validity study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of São Paulo . Br J Psychiatry [Internet]. 1986 Jan [cited 2020 Jun 16]; 148 : 23 - 6 . Available from: https://doi.org/10.1192/bjp.148.1.23 [ Links ]
15. Fleck MPA, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. Aplicação da versão em português do instrumento abreviado de avaliação da qualidade de vida "WHOQOL-bref. Rev Saúde Pública [Internet]. 2000 abr [citado 2019 dez 19];34(2):178-183. Disponível em: http://dx.doi.org/10.1590/S0034-89102000000200012 [ Links ]
16. Henrique IFS, Micheli D, Lacerda RB, Lacerda LA, Formigoni MLOS . Validação da versão brasileira do teste de triagem do envolvimento com álcool, cigarro e outras substâncias (ASSIST) . Rev Assoc Med Bras [Internet]. 2004 jan-abr [citado 2020 fev 14]; 50 ( 2 ): 199 - 206 . Disponível em: http://dx.doi.org/10.1590/S0104-42302004000200039 [ Links ]
17. World Health Organization. The world health report 2001: mental health: new understanding, new hope [Internet]. Geneva: World Health Organization; 2001 [cited 2019 Oct 31]. 171 p. Available from: https://www.who.int/whr/2001/en/whr01_en.pdf?ua=1 [ Links ]
18. Carlotto MS. Transtornos mentais comuns em trabalhadores de unidades básicas de saúde: prevalência e fatores associados. Psicol Argum [Internet]. 2016 abr-jun [citado 2020 fev 14];34(85):133-46. Disponível em: http://dx.doi.org/10.7213/psicol.argum.34.085.AO04 [ Links ]
19. Santana, LD, Silva, SPC, Lira MOSC, Vieira MCA, Santos NTN, Silva TIM, et al . Significado da doença para mulheres com hanseníase . Rev Enferm UFSM [Internet]. 2017 jan-fev [citado 2019 mar]; 7 ( 1 ): 111 -22. Disponível em: https://doi.org/10.5902/2179769224824 [ Links ]
20. Lima HMN, Sauaia N, Costa VRL, Coelho Neto GT, Figueiredo PMS. Perfil epidemiológico dos pacientes com hanseníase atendidos em Centro de Saúde em São Luís, MA. Rev Bras Clin Med [Internet]. 2010 jul [citado 2019 dez 14];8(4):323-7. Disponível em: http://files.bvs.br/upload/S/1679-1010/2010/v8n4/a007.pdf [ Links ]
21. Araujo RMS, Tavares CM, Silva JMO, Alves RS, Santos WB, Rodrigues PLS. Análise do perfil epidemiológico da hanseníase. Rev Enferm UFPE [Internet]. 2017 set [citado 2019 dez 14];11(Supl. 9):3632-41. Disponível em: https://doi.org/10.5205/1981-8963-v11i9a234513p3632-3641-2017 [ Links ]
22. Souza CDF, Fernandes TRMO, Matos TS, Ribeiro Filho JM, Almeida GKA, Lima JCB, et al. Grau de incapacidade física na população idosa afetada pela hanseníase no estado da Bahia, Brasil. Acta Fisiatr [Internet]. 2017 set [citado 2019 out 14];24(1):27-32. Disponível em: https://doi.org/10.5935/0104-7795.20170006 [ Links ]
23. Chagas ICS, Assis BPN. Ulceras em hanseníase. In: Lyon S, Grossi MAF. Hanseníase. Rio de Janeiro: Medbook; 2013 . p. 229-50. [ Links ]
24. Simões S, Castro SS, Scatena LM, Castro RO, Lau FA. Qualidade de vida dos portadores de hanseníase num município de médio porte. Medicina (Ribeirão Preto) [Internet]. 2016 jan [citado 2020 jan 03];49(1):60-7. Disponível em: https://doi.org/10.11606/issn.2176-7262.v49i1p60-67 [ Links ]
25. Hietaharju A , Croft R , Alam R , Birch P , Mong A , Haanpää M . Chronic neuropathic pain in treated leprosy . Lancet [Internet]. 2000 Sep [cited 2019 Dec 14]; 356 ( 9235 ): 1080 - 1 . Available from: https://doi.org/10.1016/S0140-6736 (00)02736-7 [ Links ]
26. Lustosa AA , Nogueira LT , Pedrosa JIS , Teles JBM , Campelo V . The impact of leprosy on health-related quality of life . Rev Soc Bras Med Trop [Internet]. 2011 Oct [cited 2019 Sep 27]; 44 ( 5 ): 621 - 6 . Available from: http://dx.doi.org/10.1590/S0037-86822011000500019 [ Links ]
27. Costa MD, Terra FS, Costa RD, Lyon S, Costa AMDD, Antunes CMF. Avaliação da qualidade de vida de pacientes em surto reacional de hanseníase tratados em centro de referência. An Bras Dermatol [Internet]. 2012 jan-fev [citado 2019 out 14];87(1):26-35. Disponível em: http://dx.doi.org/10.1590/S0365-05962012000100003 [ Links ]
*Article derived from the Master’s Degree dissertation entitled ‘Quality of life and associated factors among people with leprosy at Outpatient Department III of the Júlio Müller University Hospital (HUJM)’, defended by Rejane de Fátima Conde Finotti at the Federal University of Mato Grosso (UFMT) Public Health Postgraduate Program in 2018.
Received: December 16, 2019; Accepted: May 15, 2020











 texto en
texto en 


