Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.4 Brasília 2020 Epub 23-Jul-2020
http://dx.doi.org/10.5123/s1679-49742020000400004
Original article
Operational failures of leprosy control in household social networks with overlapping cases in endemic areas in Brazil*
1Universidade Federal do Ceará, Faculdade de Medicina, Fortaleza, CE, Brazil
2Universidade Federal da Bahia, Instituto Multidisciplinar em Saúde, Vitória da Conquista, BA, Brazil
3Secretaria Municipal de Saúde de Cacoal, Estratégia Saúde da Família, Cacoal, RO, Brazil
4Secretaria Municipal de Saúde de Picos, Coordenação de Programa de Hanseníase e Tuberculose, Picos, PI, Brazil
5Universidade Federal do Rio de Janeiro, Hospital Universitário Clementino Fraga Filho, Rio de Janeiro, RJ, Brazil
6Hospital Giselda Trigueiro, Secretaria de Estado da Saúde Pública, Natal, RN, Brazil
Objective. To analyze institutional/programmatic vulnerability of health services in the development of health care actions for people affected by leprosy and contact surveillance. Methods. This was a cross-sectional study conducted in 2017 based on primary data from a sample of leprosy cases notified between 2001-2014 with overlapping cases in household social networks (HSN) in municipalities in the states of Bahia, Piauí and Rondônia, Brazil. Results. A total of 233 leprosy cases were analyzed, 154 (66.1%) belonged to HSN with 3 or more leprosy cases. In 53.2% of cases, 2 or more generations were affected, this being an outcome associated with absence of dermato-neurological examination (prevalence ratio 1.32; confidence interval [95%CI 1.10;1.59]; p-value=0.004). Conclusion. Operational failures in the surveillance of leprosy contacts in areas of high endemicity reinforce the character of institutional/programmatic vulnerability in HSN contexts with more than one case of leprosy in the three states analyzed.
Key words: Leprosy; Epidemiology; Contact Tracing; Surveillance; Cross-Sectional Studies
Introduction
The leprosy burden in Brazil remains at high endemic levels, especially in the country’s North, Midwest and Northeast regions.1 Between 2012 and 2016, new case (NC) detection rates considered to be hyperendemic were recorded in states such as Mato Grosso (88.9/100,000 inhabitants), Tocantins (69.13/100,000 inhab.) and Maranhão (53.91/100,000 inhab.).1The size of the burden is evidenced by NC detection in the general population and in under-15 year olds, as well as by records of NCs diagnosed late that already had visible physical disabilities (grade II). Standing out as an aggravating factor is the greater expression of cases in more vulnerable populations.1 In their control guidelines, both the Brazilian Ministry of Health and the World Health Organization (WHO) emphasize the relevance of early diagnosis and timely treatment as priority strategic measures for reducing the burden of the disease.2
Brazil faces problems in ensuring comprehensive care for people/families in the context of its National Health System (SUS), including in the primary healthcare network.4Operational failures in leprosy health care and surveillance are critical and, probably, account for the undersizing of the endemic burden.3 This latter issue includes contact coverage and quality of contact assessment.2
Leprosy contact surveillance, officially in place, includes dermatology and neurology examinations, immunoprophylaxis with BCG (Bacillus Calmette-Guérin) vaccine and contact follow-up for at least five years following diagnosis of the index case (IC).2The indicator currently used to monitor these actions is the proportion of contacts examined, among registered contacts, with monitoring of coverage at the municipal and state level.2 On average Brazil has managed to assess 77% of registered contacts and this is considered to be a regular pattern.1 However, no official indicators are available about the quality of the actions comprising examination of contacts, nor about surveillance continuity in the years following diagnosis.3
In SUS organization policy, prevention, surveillance, control and care actions should be developed primarily in primary healthcare facilities, with reference services responsible for providing matrix-based support.2 When well-developed, counter-referral is therefore an opportunity for continuing education. Priority situations for reference services should include, among others, uncertain diagnoses, child cases, complex physical disabilities, relapses, leprosy reactions and adverse effects caused by multidrug therapy (MDT).2Notwithstanding, difficulties exist with regard to operational implementation of primary healthcare actions in a continuous, systematized and quality manner.3
Vulnerability occurs in complex processes of increased biosocial fragility that are expressive of biological, existential and social values,4 demonstrating that it is essential to capture interferences between the multiple dimensions of the health-disease process. Distinct situations of vulnerability can be broken down, taking into account three interconnected components: (i) individual; (ii) social or collective; and (iii) programmatic or institutional.12 The programmatic dimension relates to health services and the way in which they act to reduce vulnerability, whereby the possibility of scaling up these services is provided for.4
However, it is possible for care centralization to create difficulties related to access and comprehensive care for people affected by the disease, including prevention and surveillance actions with contacts. The dimension of programmatic vulnerability is expressed by aspects relating to social resources intended to meet access needs and to solve problems that are felt and perceived.11 This vulnerability implies operational failures in the way actions are established to control the disease, involving policies, planning, management, monitoring and evaluation in the light of the principles of the Brazilian National Health System (SUS): universal access; comprehensive health care; equity; decentralized management and service hierarchization; and social participation/monitoring.3
Programmatic vulnerability can, therefore, contribute to leprosy remaining within a primary healthcare territory, with cases that remain as a “hidden endemic” failing to be detected in a timely manner.3As such, programmatic vulnerability can often result in different generations being affected and a substantial number of cases in the same household social network over consecutive years. In these contexts, the possibility of contacts becoming new leprosy cases (coprevalent cases) is increased.13
The scarcity of papers taking this analytical perspective justifies this study being conducted, the objective of which was to analyze the institutional/programmatic vulnerability of health services in the development of care actions for leprosy cases and surveillance actions for their contacts, with emphasis on HSN with overlapping cases of the disease.
Methods
This study was conducted in Brazilian municipalities selected according to patterns of endemicity and primary healthcare network structure. Two municipalities located in the state of Bahia (Vitória da Conquista and Tremedal), one in Piauí (Floriano) and one in Rondônia (Cacoal) (Figure 1) were included in the study.
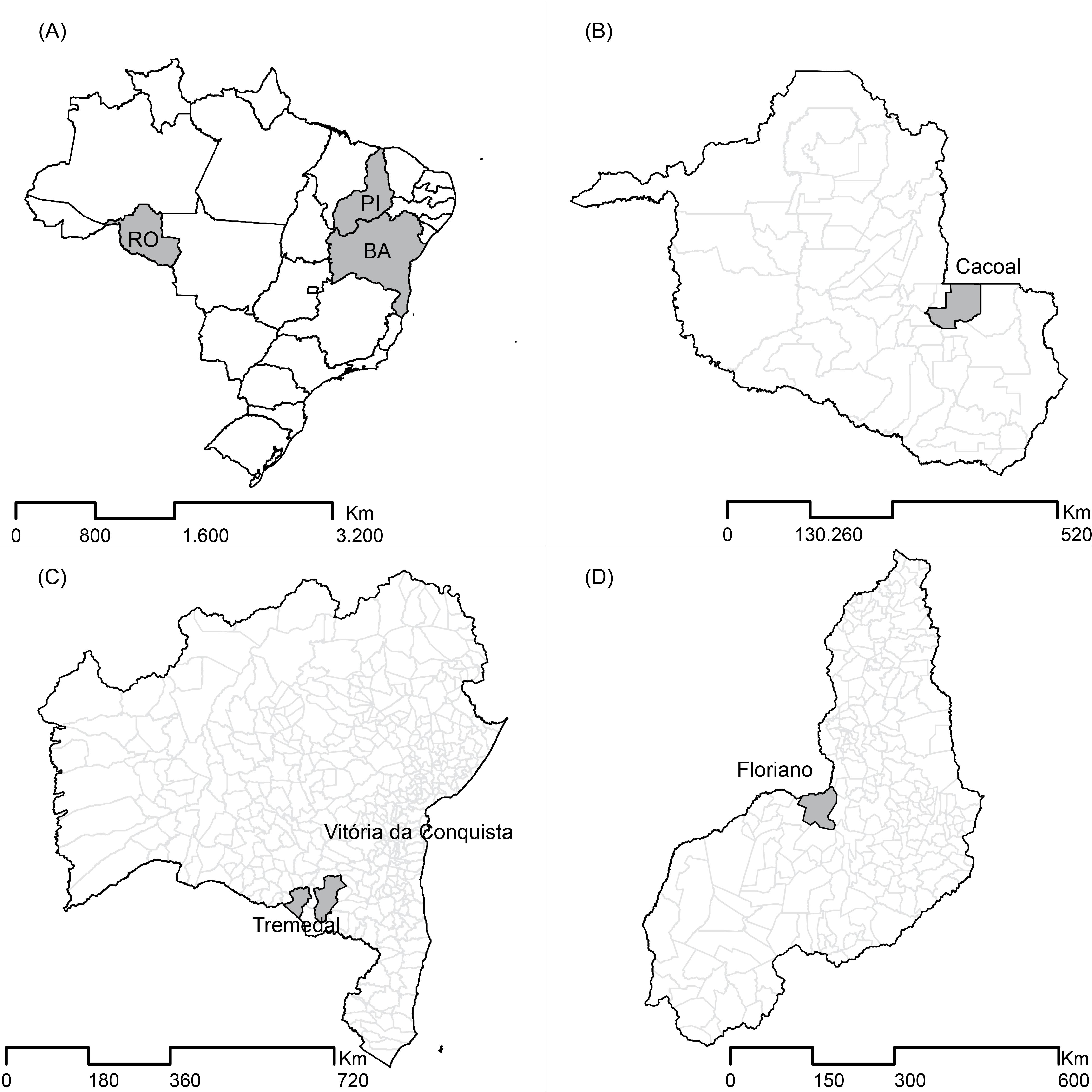
Figure 1 – Geographical location of the municipalities taking part in the study within their respective statesA: Brazil and states taking part in the study.B: State of Bahia (municipalities of Vitória da Conquista and Tremedal).C: State of Rondônia (municipality of Cacoal).D: State of Piauí (municipality of Floriano).
With regard to the municipalities in the state of Bahia, the population estimated by the Brazilian Institute of Geography and Statistics (IBGE) for 2017 was 348,718 inhab. in Vitória da Conquista and 17,700 inhab. in Tremedal. In the state of Piauí the IBGE population estimate for Floriano was 58,969 inhab. and 88,507 inhab. for Cacoal in the state of Rondônia. Family Health Strategy coverage in 2016 was 100% in Tremedal and Floriano, while in Vitória da Conquista it was 48%, and in Cacoal it was 78.2%.15In 2017, Floriano had the highest endemicity (69.7 cases/100,000 inhab.), while Vitória da Conquista had the lowest detection rate (17.2 cases/100,000 inhab.), with both rates being considered to be high.17
This was an analytical cross-sectional study conducted as part of the IntegraHans North-Northeast project (coordinated by the Federal University of Ceará [UFC]) and the IntegraHans Piauí project (coordinated by the Federal University of Piauí [UFPI] in partnership with UFC).18 These projects were developed between 2014 and 2015.
The study population involved 899 new leprosy cases notified between 2001 and 2014, resident in the four municipalities covered by the study, with no restriction as to age. The study sample was comprised of people with leprosy (index cases [IC]) who are part of an HSN with overlapping cases of the disease.
An index case (IC) was considered to be the first leprosy case diagnosed in an HSN, while a coprevalent case (CPC) was taken to be a contact in the HSN who became a new case (CN). In addition to the leprosy IC, the HSN included all household and social contacts as defined by the Ministry of Health,2 as well as other household and social contacts who became cases (coprevalent cases – CPCs). Identification of at least 2 leprosy cases in one HSN defined existence of leprosy “overlapping”, this being an indicator of increased risk.14
A structured instrument was administered for ICs located within the territory who agreed to take part in the study. The instrument was designed by the lead author of this study and by a collaborating researcher, both of whom are qualified in Nursing and Public Health. Both took part in the training conducted by the project coordinators. The data were collected using physical instruments and later consolidated using Epi Info version 7.1.5 (Centers for Disease Control and Prevention [CDC], Atlanta, USA).
The variables included in the analysis were as follows: prior registration of the household by a community health agent (ACS) (yes; no); place of initial healthcare upon suspicion of leprosy (primary healthcare center [UBS]; municipal reference unit; other); place of diagnosis (UBS; municipal reference unit; other); place of leprosy treatment, multidrug therapy (municipal reference unit; other); and knowledge of disease before diagnosis (yes; no).
For CPCs additional information was collected about surveillance activities: dermatology examination performed; neurology examination performed; BCG vaccine received; advised about BCG vaccine administration; advised about mobilizing other contacts; and guidance received on returning to the health service.2
As well as identifying the percentage of leprosy case contacts assessed among those who were registered (coverage indicator), identification of indicators of surveillance action quality was also considered to be necessary. This was done using the IntegraHans score which was built by the project for this purpose.
This score is based on six components which have different weightings: complete dermatology examination of the entire body surface performed (weight 6); complete neurology examination performed (weight 5); BCG vaccination when indicated (weight 4); guidance on returning to the health center, if symptoms appear or to attend an appointment made in advance (weight 3); advice on BCG (weight 2); and advice on tracing other contacts (weight 1). The score has three classifications: poor (0-6), regular (7-14) and excellent (15-21). Considering the importance of monitoring this form of surveillance, the score enables an indicator that is easy to interpret to be compiled, for use in the healthcare network.
When assessing differences between the groups, Pearson’s Chi-Square test (Χ2) was used for observation values equal to or greater than five, while Fisher’s exact test was used for the remainder. During the crude analysis, we sought to verify existence of association between the IntegraHans score and two or more generations being affected in the HSN, as well as 3 or more leprosy cases in the same HSN. Prevalence ratios (PR) and their respective 95% confidence intervals (95%CI) were calculated. P-values <0.05 were considered to be significant. Stata 11.2 (Stata Corporation, College Station, USA) was used to analyze the data.
Variables were included that assess operational aspects of leprosy control actions. For ICs the following variables were analyzed: ‘household registered by ACS’, ‘first service accessed upon suspicion of leprosy’, ‘place of diagnosis’ and ‘place of treatment’ (all of these had three alternative answers: UBS; reference unit; other); plus a further variable, ‘ever heard of leprosy’ (yes; no). For contacts the following variables were analyzed: ‘dermatology examination’, ‘neurology examination’, ‘advice on BCG’, ‘BCG vaccine administered’, ‘advice on mobilizing other contacts’ (for medical assessment) and ‘guidance on returning to health services’ (the answer to all these variables was: yes or no); plus the ‘Integrahans score’ (excellent; regular; poor). In the case of discreet quantitative numerical variables, the average and respective 95%CI were calculated.
The study projects were submitted to and approved by the UFC Research Ethics Committee (Opinion No. 544.962, dated February 28th 2014) and the UFPI Research Ethics Committee (Opinion No. 1.115.818, dated July 17th 2015). Due respect was paid to National Health Council Resolution No. 466, dated October 12th 2012. The study was explained to all leprosy cases invited to take part before they agreed to do so and before they signed a Free and Informed Consent form. In the case of participants under 18 years, their legal guardians signed the Free and Informed Consent form and children aged over 12 signed a Free and Informed Assent form as well.
Results
In the selected municipalities, 405 (45.1%) leprosy cases that had at least one more leprosy case in their HSN were identified. Two hundred and thirty-three (57.5%) of these cases were reached, the majority of whom were in the 41-60 age group (n=98; 42.1%) and were of brown race/skin color (n=147; 63.1%) (Table 1). There were 169 (41.7%) losses due to change of address and 3 (0.7%) refusals to take part.
Table 1 – Socioeconomic and demographic characterization of contacts and index cases (n=233) in municipalities in the states of Bahia, Piauí and Rondônia, 2001-2014
| Variables | Contacts | Index cases | Total |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Sex | |||
|
| |||
| Male | 56 (50.9) | 59 (48.0) | 115 (49.4) |
| Female | 54 (49.1) | 64 (52.0) | 118 (50.6) |
| Age range (in years) | |||
| ≤14 | 5 (4.5) | 1 (0.8) | 6 (2.6) |
| 15-40 | 35 (31.8) | 29 (23.6) | 64 (27.5) |
| 41-60 | 49 (44.5) | 49 (39.8) | 98 (42.1) |
| >60 | 21 (19.1) | 44 (35.8) | 65 (27.9) |
| Race/skin color | |||
| White | 14 (12.7) | 18 (14.6) | 32 (13.7) |
| Brown | 70 (63.6) | 77 (62.6) | 147 (63.1) |
| Black | 23 (20.9) | 24 (19.5) | 47 (20.2) |
| Yellow | 3 (2.7) | 4 (3.3) | 7 (3.0) |
|
| |||
| Marital status | |||
|
| |||
| Single | 22 (20.0) | 14 (11.4) | 36 (15.5) |
| Married | 60 (54.5) | 64 (52.0) | 124 (53.2) |
| Common-law partnership | 10 (9.1) | 8 (6.5) | 18 (7.7) |
| Separated/divorced | 10 (9.1) | 23 (18.7) | 33 (14.2) |
| Widowed | 8 (7.3) | 14 (11.4) | 22 (9.4) |
|
| |||
| Schooling | |||
|
| |||
| Illiterate | 21 (19.1) | 28 (22.8) | 49 (21) |
| Literate | 7 (6.4) | 14 (11.4) | 21 (9.0) |
| 1st to 3rd grade | 13 (11.8) | 20 (16.3) | 33 (14.2) |
| 4th to 7th grade | 31 (28.2) | 23 (18.7) | 54 (23.2) |
| Complete middle school education | 4 (3.6) | 3 (2.4) | 7 (3.0) |
| 1st or 2nd year of high school | 15 (13.6) | 4 (3.3) | 19 (8.2) |
| Complete high school education | 14 (12.7) | 21 (17.1) | 35 (15) |
| Incomplete higher education | 3 (2.7) | 4 (3.3) | 7 (3.0) |
| Complete higher education | 2 (1.8) | 6 (4.9) | 8 (3.4) |
|
| |||
| Total | 110 (47.2) | 123 (52.8) | 233 (100.0) |
Of the total 233 leprosy cases included in the study, 66.1% (n=154) were found to belong to HSN with 3 or more diagnosed leprosy cases, whereby the overall average was 4.1 cases per HSN, with standard deviation of 3.3 cases. In 53.2% of cases (n=124), the disease affected two generations, while in 20.2% of cases (n=47), it affected three generations.
A large proportion of the households had been registered by ACS (n=197; 84.5%); however, specialized health services were accessed more in the event of suspicion of having leprosy (n=167; 71.7%), confirmation of diagnosis (n=200; 85.8%) and treatment (n=178; 76.4%) (Table 2).
Table 2 – Operational aspects of leprosy control actions among contacts and index cases (n=233), by case occurrence in two or more generations of families assessed in municipalities in Bahia, Piauí and Rondônia, 2001-2014
| Variables | Total | Two or more generations | p-value | PRa | 95%CIb | p-valuec | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| No | Yes | ||||||
|
| |||||||
| n (%) | n (%) | n (%) | |||||
| Index cases and contacts | |||||||
|
| |||||||
| Household registered by ACSe | |||||||
|
| |||||||
| Yes | 197 (84.5) | 47 (23.9) | 150 (76.1) | 0.026c | 1.31 | 0.98;1.74 | 0.026 |
| No | 36 (15.5) | 15 (41.7) | 21 (58.3) | 1.00 | – | – | |
|
| |||||||
| First service accessed upon suspicion | |||||||
|
| |||||||
| UBSf | 49 (21.0) | 12 (24.5) | 37 (75.5) | 0.679c | 1.00 | – | – |
| Municipal reference service | 167 (71.7) | 44 (26.3) | 123 (73.7) | 0.97 | 0.81;1.17 | 0.794 | |
| Other | 17 (7.3) | 6 (35.3) | 11 (64.7) | 0.86 | 0.58;1.26 | 0.389 | |
|
| |||||||
| Place of diagnosis | |||||||
|
| |||||||
| UBSf | 27 (11.6) | 9 (33.3) | 18 (66.7) | 0.220d | 1.00 | – | – |
| Reference unit | 200 (85.8) | 50 (25.0) | 150 (75.0) | 1.12 | 0.85;1.49 | 0.354 | |
| Other | 6 (2.6) | 3 (50.0) | 3 (50.0) | 0.75 | 0.32;1.74 | 0.443 | |
|
| |||||||
| Place of treatment | |||||||
|
| |||||||
| UBSf | 55 (23.6) | 15 (27.3) | 40 (72.7) | 0.899c | 1.00 | – | – |
| Reference unit | 178 (76.4) | 47 (26.4) | 131 (73.6) | 1.01 | 0.84;1.21 | 0.899 | |
|
| |||||||
| Ever heard of leprosy | |||||||
|
| |||||||
| Yes | 178 (76.4) | 48 (27.0) | 130 (73.0) | 0.825c | 1.00 | – | – |
| No | 55 (23.6) | 14 (25.5) | 41 (74.5) | 1.02 | 0.85;1.22 | 0.824 | |
|
| |||||||
| Contacts (n=110) | |||||||
|
| |||||||
| Dermatology examination | |||||||
|
| |||||||
| Yes | 48 (43.6) | 4 (8.3) | 44 (91.7) | 0.005d | 1.00 | – | – |
| No | 62 (56.4) | 19 (30.6) | 43 (69.4) | 1.32 | 1.10;1.59 | 0.004 | |
|
| |||||||
| Neurology examination | |||||||
|
| |||||||
| Yes | 47 (42.7) | 4 (8.5) | 43 (91.5) | 0.008d | 1.00 | – | – |
| No | 63 (57.3) | 19 (30.2) | 44 (69.8) | 1.31 | 1.09;1.57 | 0.006 | |
|
| |||||||
| Advised about BCGg | |||||||
|
| |||||||
| Yes | 77 (70.0) | 22 (28.6) | 55 (71.4) | 0.002d | 1.36 | 1.16;1.58 | 0.003 |
| No | 33 (30.0) | 1 (3.0) | 32 (97.0) | 1.00 | – | – | |
|
| |||||||
| BCGg vaccination administered | |||||||
|
| |||||||
| Yes | 28 (25.5) | 1 (3.6) | 27 (96.4) | 0.007d | 1.00 | – | – |
| No | 82 (74.5) | 22 (26.8) | 60 (73.2) | 1.32 | 1.14;1.53 | 0.009 | |
|
| |||||||
| Advice on mobilizing other contacts | |||||||
|
| |||||||
| Yes | 68 (61.8) | 19 (27.9) | 49 (72.1) | 0.029d | 1.26 | 1.05;1.50 | 0.021 |
| No | 42 (38.2) | 4 (9.5) | 38 (90.5) | 1.00 | – | – | |
|
| |||||||
| Guidance on returning to health services | |||||||
|
| |||||||
| Yes | 53 (48.2) | 10 (18.9) | 43 (81.1) | 0.646c | 1.00 | – | – |
| No | 57 (51.8) | 13 (22.8) | 44 (77.2) | 1.05 | 0.87;1.27 | 0.612 | |
|
| |||||||
| IntegraHans Score | |||||||
|
| |||||||
| Excellent | 38 (34.5) | 3 (7.9) | 35 (92.1) | 0.017d | 1.00 | – | – |
| Regular | 10 (9.1) | 1 (10.0) | 9 (90.0) | 0.98 | 0.78;1.22 | 0.830 | |
| Poor | 62 (56.4) | 19 (30.6) | 43 (69.4) | 1.33 | 1.10;1.61 | 0.008 | |
a) PR: prevalence ratio.
b) 95%CI: 95% confidence interval.
c) Pearson’s Chi-Square test.
d) Fisher’s exact test.
e) ACS: community health agent.
f) UBS: primary healthcare center.
g) BCG: Bacillus Calmette-Guérin.
The majority of CPCs reported that at the time the IC was diagnosed they did not undergo a dermatology examination (n=62; 56.4%) or a neurology examination (n=63; 57.3%). Although advice on BCG administration (n=77; 70.0%) was frequent, the majority had not been vaccinated (n=82; 74.5%). Many CPCs were advised to mobilize other contacts for assessment (n=68; 61.8%); but did not receive guidance on returning for new assessments in the following years (n=57; 51.8%). The IntegraHans score was classified as ‘poor’ (n=62; 56.4%) for a high proportion of cases (Table 2).
Association was found between two or more generations being affected and: contacts not having undergone a dermatology examination (PR=1.32 – 95%CI 1.10;1.59); having received guidance on BCG (PR=1.36 – 95%CI 1.16;1.58), not having received a BCG vaccination (PR=1.32 – 95%CI 1.14;1.53); having been advised to mobilize other contacts to get assessment (PR=1.26 – 95%CI 1.05;1.50); and having had a ‘poor’ IntegraHans score (PR=1.33 – 95%CI 1.10;1.61) (Table 2).
When the number of cases per HSN was compared with the quality of contact control actions, association was found between the 3 or more cases per HSN outcome and: contacts not having undergone a dermatology examination (PR=1.29 – 95%CI 1.07;1.56); not having had a neurology examination (PR=1.28 – 95%CI 1.06;1.55); lack of advice on BCG vaccination (PR=1.38 – 95%CI 1.18;1,62); and not having BCG vaccination (PR=1.34 – 95%CI 1.15;1.56). Association was also found between this outcome (3 or more cases per HSN) and lack of advice on mobilizing other contacts (PR=1.22 – 95%CI 1.02;1.47) and having a ‘poor’ IntegraHans score (PR=1.33 – 95%CI 1.10;1.61) (Table 3).
Table 3 – Operational aspects of leprosy control actions among contacts and index cases (n=233) by occurrence of three or more leprosy cases in household social networks (HSN) in municipalities in Bahia, Piauí and Rondônia, 2001-2014
| Variables | Total | Three or more HSN cases | p-value | PRa | 95%CIb | p-valuec | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| No | Yes | ||||||
|
| |||||||
| n (%) | n (%) | n (%) | |||||
| Index cases and contacts | |||||||
|
| |||||||
| Household registered by ACSe | |||||||
|
| |||||||
| Yes | 197 (84.5) | 65 (33.0) | 132 (67.0) | 0.492c | 1.09 | 0.83;1.44 | 0.492 |
| No | 36 (15.5) | 14 (38.9) | 22 (61.1) | 1.00 | – | – | |
|
| |||||||
| Place of diagnosis | |||||||
|
| |||||||
| UBSf | 27 (11.6) | 7 (25.9) | 20 (74.1) | 0.465d | 1.00 | – | – |
| Reference unit | 200 (85.8) | 69 (34.5) | 131 (65.5) | 0.88 | 0.69;1.13 | 0.376 | |
| Other | 6 (2.6) | 3 (50.0) | 3 (50.0) | 0.67 | 0.29;1.55 | 0.246 | |
|
| |||||||
| Place of treatment | |||||||
|
| |||||||
| UBSf | 55 (23.6) | 17 (30.9) | 38 (69.1) | 0.591c | 1.00 | – | – |
| Reference unit | 178 (76.4) | 62 (34.8) | 116 (65.2) | 0.94 | 0.77;1.16 | 0.591 | |
|
| |||||||
| Contacts (n=110) | |||||||
|
| |||||||
| Dermatology examination | |||||||
|
| |||||||
| Yes | 48 (43.6) | 5 (10.4) | 43 (89.6) | 0.011c | 1.00 | – | – |
| No | 62 (56.4) | 19 (30.6) | 43 (69.4) | 1.29 | 1.07;1.56 | 0.011 | |
|
| |||||||
| Neurology examination | |||||||
|
| |||||||
| Yes | 47 (42.7) | 5 (10.6) | 42 (89.4) | 0.014c | 1.00 | – | – |
| No | 63 (57.3) | 19 (30.2) | 44 (69.8) | 1.28 | 1.06;1.55 | 0.014 | |
|
| |||||||
| Advised about BCGg | |||||||
|
| |||||||
| Yes | 33 (30.0) | 1 (3.0) | 32 (97.0) | 0.001d | 1.00 | – | – |
| No | 77 (70.0) | 23 (29.9) | 54 (70.1) | 1.38 | 1.18;1.62 | 0.002 | |
|
| |||||||
| BCGg vaccination administered | |||||||
|
| |||||||
| Yes | 28 (25.5) | 1 (3.6) | 27 (96.4) | 0.007d | 1.00 | – | – |
| No | 82 (74.5) | 23 (28.0) | 59 (72.0) | 1.34 | 1.15;1.56 | 0.007 | |
|
| |||||||
| Advice on mobilizing other contacts | |||||||
|
| |||||||
| Yes | 42 (38.2) | 5 (11.9) | 37 (88.1) | 0.048c | 1.00 | – | – |
| No | 68 (61.8) | 19 (27.9) | 49 (72.1) | 1.22 | 1.02;1.47 | 0.048 | |
|
| |||||||
| Guidance on returning to health services | |||||||
|
| |||||||
| Yes | 53 (48.2) | 9 (17.0) | 44 (83.0) | 0.236c | 1.00 | – | – |
| No | 57 (51.8) | 15 (26.3) | 42 (73.7) | 1.13 | 0.93;1.37 | 0.236 | |
|
| |||||||
| IntegraHans Score | |||||||
|
| |||||||
| Excellent | 38 (34.5) | 3 (7.9) | 35 (92.1) | 0.020d | 1.00 | – | – |
| Regular | 10 (9.1) | 2 (20.0) | 8 (80.0) | 1.15 | 0.83;1.59 | 0.265 | |
| Poor | 62 (56.4) | 19 (30.6) | 43 (69.4) | 1.33 | 1.10;1.61 | 0.008 | |
a) PR: prevalence ratio.
b) 95%CI: 95% confidence interval.
c) Pearson’s Chi-Square test.
d) Fisher’s exact test.
e) ACS: community health agent.
f) UBS: primary healthcare center.
g) BCG: Bacillus Calmette-Guérin.
Discussion
The contexts analyzed in the North and Northeast regions of Brazil highlight considerable programmatic vulnerability with regard to provision and quality of leprosy contact surveillance actions. It is a complex problem, especially given the HSN with overlapping NCs, denoting increased risk of the disease. Decentralization of these actions to primary healthcare is not, however, sufficiently implemented in the municipalities studied. The high percentages of CPCs that did not have timely dermatololg/neurology examinations, were not advised about and did not have BCG vaccinations, and did not receive guidance on returning to the health center, very probably, contributed to leprosy remaining in these territories. The association found between a ‘poor’ IntegraHans score for the approach to contacts and (i) 2 or more generations being affected or (ii) existence of 3 or more cases in the same HSN stresses programmatic vulnerability and the need to restructure surveillance actions.
Despite the control guidelines established by the Ministry of Health, based on the WHO global strategy for 2020,2 operationalization of contact surveillance actions has not been fully materialized in the contexts studied. The process of decentralizing healthcare to the Family Health Strategy is not yet effective, considering the high percentages of cases that seek references service for diagnosis and treatment. In endemic areas, it is possible that these services may be overburdened, including difficulty in effectively carrying out the actions for which they are responsible.2 Moreover, reflection needs to be given to the scope of actions in municipalities without access to specialized services, which generates impacts to a greater or lesser extent on affected people.
The process of integrating leprosy control actions into primary healthcare has been underway in Brazil since the 1970s, gradually and progressively, although slowly. As a consequence, decentralization is still insufficient, and care is concentrated in specialized services in medium and large-size municipalities.3
A study conducted in the municipality of São José do Rio Preto, SP, with the aim of assessing health services as to early detection of leprosy, revealed that people with the disease traveled 9.2km on average between their homes and the places where they got treatment, confirming the importance of decentralization for improving access, early diagnosis and treatment follow-up.20A study conducted with the aim of characterizing the flow of people with leprosy from their municipality of resident to the municipality where they got treatment, in the states of Maranhão, Pará, Tocantins and Piauí, identified gaps in this process of decentralization. Standing out, in particular, are difficulties and challenges in follow-up during and after multidrug therapy (MDT).22
The reality found in the contexts analyzed may be equal to that in other parts of the country. A study conducted with individuals with leprosy in Salvador, Bahia, revealed that affected people have to follow a long path before getting care, often with excessively long average time for diagnosis and, in many cases, only after having been referred to a reference center in the state capital.10 Another study conducted in a municipality in the state of São Paulo, revealed absence of active case tracing – despite it being necessary –, in order to obtain true knowledge of the epidemiological situation, as well as absence of health education actions, pointing to the need to reorganize care for leprosy in the primary healthcare network, especially with regard to diagnosis and treatment in these spaces.23
There are therefore complex challenges to be overcome by primary healthcare professionals with regard to scaling up user access to health services.20 Certain issues standout among these challenges: (i) health management quality in relation to regionalized networks; (ii) continuing education for health professionals; (iii) lack of empowerment of affected people and their families with regard to their right to health; and (iv) insufficiency of systematic analyses in relation to epidemiological and operational indicators in the territories.3
The high percentages of CPCs not approached adequately at the time the ICs were diagnosed, when they were contacts, illustrate real difficulties for timely diagnosis and contact follow-up, as well as for immunoprophylaxis, these being measures that have been made known for a very long time in Brazil.3 As a consequence, Mycobacterium leprae in the HSN continues to circulate actively, affecting individuals of more than one generation, which can favor the emergence of physical disabilities and continuance of stigma strongly associated with leprosy.23
A case study of situations related to leprosy in children concluded that active contact tracing revealed itself to be an important method for early leprosy diagnosis in childhood, principally because the clinical signs are not always easily identifiable.26 Despite dermatology and neurology examinations being the main form of case diagnosis, it is also essential to promote skills and knowledge about the disease and its diverse manifestations.3
Also worthy of note is the fact of CPCs seen by health professionals at the time ICs were diagnosed not having been given guidance on returning to the health services in the event of skin or neurological lesions. Because of this, the recommendation for longitudinal surveillance over a five-year period can get lost in the midst of the health service routine, or as a result of the weakness of health education actions for people and their HSN.26
Another study, aimed at characterizing standards of care involving household contacts of leprosy cases living in the Northern region of Brazil, revealed that 41.6% of contacts had not undergone a dermatology examination, and that 54.9% had not had a neurology examination. The same study found that 56.0% of contacts did not receive guidance on returning to the health service for new assessments/follow-up and 40.5% were not advised on mobilizing other contacts.29 These findings point to possible health institution weaknesses in fulfilling their role of preventing leprosy,30 with the possibility of increasing the susceptibility of some HSN and maintaining transmission sources.
A cause of concern with regard to the national leprosy control policy relates to the lack of indicators to enable not only monitoring of coverage, but also the quality of contact care.3 In this respect, the IntegraHans score aimed to assess the extent to which six actions considered essential for contact surveillance occurred. Overall, care provided to less than 50.0% of CPCs was classified as ‘excellent’; i.e., almost half the CPCs did not receive some form of care essential for prevention and/or early diagnosis in their HSN, as part of the actions planned nationally.3
Continuing education processes, aligned with well-established monitoring and evaluation systems, favor the accompaniment of leprosy control action decentralization in the SUS healthcare network.2 They are activities that have the potential to inform planning of comprehensive care for people with leprosy and their HSN. Incorporation of the score, associated with monitoring of HSN with 3 or more leprosy cases and/or two or more affected generations, should also be taken into account on the processes of prioritizing scenarios of integrated surveillance in health territories.
Development of health surveillance actions by primary healthcare and their integration with other care points within the network is strategic for the sustainability of these actions and their distribution with greater fairness and quality.19 Communication and education processes among the population must, therefore, be (re)signified so that there is greater inclusion and empowerment of SUS users.
Possible limitations of this study relate to the possibility of CPC memory recall bias with regard to surveillance actions performed at the time ICs were diagnosed, in addition to it not having been possible to interview all HSH CPCs, in many cases because of change of address or refusal. The fact of the study having been based on the existence of at least 2 leprosy cases per HSN may, in some way, have contributed to poorer results in comparison to more general contexts. Notwithstanding, having studied a significant number of HSN in three states with high endemicity in Brazil strengthens the findings.
The operational failures identified in the leprosy contact surveillance process reinforce the nature of programmatic vulnerability in the scenarios studied, even among contacts of HSN with overlapping cases. We stress once more the critical aspects relating to access to the SUS healthcare network, as well as the development of longitudinal surveillance actions. In addition to coverage, it is fundamental to develop new strategies aimed at improving the quality of these actions.
Contrary to the recommendations of the national leprosy control policy in Brazil, reference services continued to be the main National Health System space where leprosy contact surveillance, and leprosy diagnosis and treatment actions were undertaken. In the municipalities covered by this study, decentralization of primary healthcare was still not a daily health service practice. Use of the IntegraHans score was shown to be feasible for assessing the quality of care for leprosy contacts and should the considered as a possibility for use in health services.
In conclusion, we highlight the importance of structured processes, matrix-based support and monitoring of actions in the territory, especially in scenarios of HSN with overlapping of leprosy cases.
REFERENCES
1. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Hanseníase. Bol Epidemiol [Internet]. 2018 [citado 2019 set 29];49(4). Disponível em: http://portalarquivos2.saude.gov.br/images/pdf/2018/janeiro/31/2018-004-Hanseniase-publicacao.pdf [ Links ]
2. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância das Doenças Transmissíveis. Diretrizes para vigilância, atenção e eliminação da Hanseníase como problema de saúde pública: manual técnico-operacional [Internet]. Brasília: Ministério da Saúde; 2016 [citado 2019 set 29]. 58 p. Disponível em: https://www.saude.gov.br/images/pdf/2016/fevereiro/04/diretrizes-eliminacao-hanseniase-4fev16-web.pdf [ Links ]
3. Souza EA, Boigny RN, Ferreira AF, Alencar CH, Oliveira MLW, Ramos Júnior AN. Vulnerabilidade programática no controle da hanseníase: padrões na perspectiva de gênero no Estado da Bahia, Brasil. Cad Saúde Pública [Internet]. 2018 fev [citado 2020 jun 8];34(1):e00196216. Disponível em: https://doi.org/10.1590/0102-311x00196216 [ Links ]
4. Cecílio LCO. As necessidades de saúde como conceito. Estruturante na luta pela integralidade e equidade na atenção em saúde. In: Pinheiro R, Mattos RA (Org.). Os sentidos da integralidade na atenção e no cuidado à saúde. Rio de Janeiro: UERJ, IMS; ABRASCO; 2006. 184 p. [ Links ]
5. Romero-Montoya M, Beltran-Alzate JC, Cardona-Castro N. Evaluation and monitoring of mycobacterium leprae transmission in household contacts of patients with hansen’s disease in Colombia. PLoS Negl Trop Dis [Internet]. 2017 Jan [cited 2020 Jun 8];11(1):e0005325. Available from: https://doi.org/10.1371/journal.pntd.0005325 [ Links ]
6. Moura MLN, Dupnik KM, Sampaio GAA, Nóbrega PFC, Jeronimo AK, Nascimento Filho JM, et al. Active surveillance of hansen’s disease (leprosy): importance for case finding among extra-domiciliary contacts. PLoS Negl Trop Dis [Internet]. 2013 Mar [cited 2020 Jun 8];7(3):e2093. Available from: https://doi.org/10.1371/journal.pntd.0002093 [ Links ]
7. Sales AM, Leon AP, Duppre NC, Hacker MA, Nery JAC, Sarno EN, et al. Leprosy among patient contacts: a multilevel study of risk Factors. PLoS Negl Trop Dis [Internet]. 2011 Mar [cited 2020 Jun 8];5(3):e1013. Available from: https://doi.org/10.1371/journal.pntd.0001013 [ Links ]
8. Ministério da Saúde (BR). Secretaria de Políticas de Saúde. Departamento de Atenção Básica. Guia para o controle da hanseníase [Internet]. Brasília: Ministério da Saúde; 2002 [citado 2019 set 19]. 89 p. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/guia_controle_hanseniase_cab10.pdf [ Links ]
9. Oliveira SP. Acessibilidade ao exame de contato de hanseníase na Estratégia de Saúde da Família em Cuiabá, Mato Grosso-Brasil [dissertação]. Salvador: Instituto de Saúde Coletiva; Universidade Federal da Bahia; 2013. Disponível em: https://repositorio.ufba.br/ri/handle/ri/13132 [ Links ]
10. Martins PV, Iriart JAB. Itinerários terapêuticos de pacientes com diagnóstico de hanseníase em Salvador, Bahia. Physis [Internet]. 2014 out [citado 2020 jun 8];24(1):273-89. Disponível em: http://dx.doi.org/10.1590/S0103-73312014000100015 [ Links ]
11. Ayres JRCM, França I, Junqueira G, Saletti HC. O conceito de vulnerabilidade e as práticas em Saúde. Novas perspectivas e desafios. In: Czeresnia D, Machado C (Org.). Promoção da saúde: conceitos, reflexões, tendências. 2. ed. Rio de Janeiro: Fiocruz; 2009. p. 121-43. [ Links ]
12. Oviedo RAM, Czeresnia D. O conceito de vulnerabilidade e seu caráter biossocial. Interface [Internet]. 2015 jun [citado 2020 jun 8];19(53):237-50. Disponível em: http://dx.doi.org/10.1590/1807-57622014.0436 [ Links ]
13. Durães SMB, Guedes LS, Cunha MD, Magnanini MMF, Oliveira MLWDR. Estudo epidemiológico de 107 focos familiares de hanseníase no município de Duque de Caxias – Rio de Janeiro, Brasil. An Bras Dermatol [Internet]. 2010 out [citado 2020 jun 8];85(3):339-45. Disponível em: http://dx.doi.org/10.1590/S0365-05962010000300007 [ Links ]
14. Boigny RN, Souza EA, Romanholo HSB, Araújo OD, Araújo TME, Carneiro MAG, et al. Persistência da hanseníase em redes de convívio domiciliar: sobreposição de casos e vulnerabilidade em regiões endêmicas no Brasil. Cad Saude Publica. 2019 18;35(2):1-14. Disponível em: http://www.scielo.br/pdf/csp/v35n2/1678-4464-csp-35-02-e00105318.pdf. Doi: 10.1590/0102-311x00105318. [ Links ]
15. Instituto Brasileiro de Geografia e Estatística - IBGE. Unidades da Federação: Bahia [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2014 [citado 2019 set 09]. Disponível em: http//www.cidades.ibge.gov.br [ Links ]
16. Ministério da Saúde (BR). Secretaria de Atenção Primaria à Saúde. Cobertura da atenção básica [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2019 set 10]. Disponível em: https://egestorab.saude.gov.br/paginas/acessoPublico/relatorios/relHistoricoCoberturaAB.xhtml;jsessionid=GlB29PA-wWBYBKNO39MYdU4Y [ Links ]
17. Ministério da Saúde (BR). Situação epidemiológica - dados [Internet]. Brasília; Ministério da Saúde; 2019 [citado 2019 set 02]. Disponível em: http://portalms.saude.gov.br/saude-de-a-z/hanseniase/situacao-epidemiologica [ Links ]
18. Grupo de pesquisas clinico-epidemiológicos e operacionais em Doenças Tropicais Negligenciadas. Relatório do projeto: Atenção à saúde para hanseníase em áreas de alta endemicidade nos estados de Rondônia, Tocantins e Bahia: abordagem integrada de aspectos operacionais, epidemiológicos (espaço-temporais), clínicos e psicossociais (Integrahans-Norte e Nordeste). Fortaleza: UFC; 2017. [ Links ]
19. Grossi MAF. Vigilância da hanseníase no Estado de Minas Gerais. Rev Bras Enferm [Internet]. 2008 nov [citado 2020 jun 8];61(esp):781. Disponível em: https://doi.org/10.1590/S0034-71672008000700021 [ Links ]
20. Pereira AJ, Helene LMF, Pedrazini ES, Martins CL, Vieira CSCA. Atenção básica de saúde e a assistência em Hanseníase em serviços de saúde de um município do Estado de São Paulo. Rev Bras Enferm [Internet]. 2008 nov [citado 2020 jun 8]; 61(spe):716-25. Disponível em: https://doi.org/10.1590/S0034-71672008000700011 [ Links ]
21. Souza MF, Vanderlei LCM, Frias PG. Avaliação da implantação do Programa de Controle da Hanseníase em Camaragibe, Pernambuco. Epidemiol Serv Saúde [Internet]. 2017 out-dez [citado 2020 jun 8];26(4):817-34. Disponível em: https://doi.org/10.5123/S1679-49742017000400013 [ Links ]
22. Alencar CHM, Ramos Júnior AN, Sena Neto SA, Murto C, Alencar MJF, Barbosa JC, et al. Diagnóstico da hanseníase fora do município de residência: uma abordagem espacial, 2001 a 2009. Cad Saúde Pública [Internet]. 2012 [citado 2020 jun 8];28(9):1685-98. Disponível em: http://dx.doi.org/10.1590/S0102-311X2012000900008 [ Links ]
23. Visschedijk J, Engelhard A, Lever P, Grossi MAF, Feenstra P. Leprosy control strategies and the integration of health services: an international perspective. Cad Saúde Pública [Internet]. 2003 Dec [cited 2020 Jun 8];19(6):1567-81. Available from: http://dx.doi.org/10.1590/S0102-311X2003000600002 [ Links ]
24. Arantes CK, Garcia MLR, Filipe MS, Nardi SMT, Paschoal VDA. Avaliação dos serviços de saúde em relação ao diagnóstico precoce da hanseníase. Epidemiol Serv Saúde [Internet]. 2010 abr-jun [citado 2020 jun 8];19(2):155-64. Disponível em: http://scielo.iec.gov.br/pdf/ess/v19n2/v19n2a08.pdf [ Links ]
25. Van Brakel WH, Sihombing B, Djarir H, Beise K, Kusumawardhani L, Yulihane R, et al. Disability in people affected by leprosy: the role of impairment, activity, social participation, stigma and discrimination. Glob Health Action [Internet]. 2012 Jul [cited 2020 jun 8];5. Available from: https://doi.org/10.3402/gha.v5i0.18394 [ Links ]
26. Pires CAA, Malcher CMSR, Abreu Júnior JMC, Albuquerque TG, Corrêa IRS, Daxbacher, ELR. Hanseníase em menores de 15 anos: a importância do exame de contato. Rev Paul Pediatr [Internet]. 2012 jun [citado 2020 jun 8];30(2):292-5. Disponível em: http://dx.doi.org/10.1590/S0103-05822012000200022 [ Links ]
27. Smith CS, Noordeen SK, Richardus JH, Sansarricq H, Cole ST, Soares RC, et al. A strategy to halt leprosy transmission. Lancet Infect Dis [Internet]. 2014 Feb [cited 2020 Jun 8];14(2):96-8. Available from: https://doi.org/10.1016/s1473-3099(13)70365-7 [ Links ]
28. Silva SF. Organização de redes regionalizadas e integradas de atenção à saúde: desafios do Sistema Único de Saúde (Brasil). Ciênc Saúde Coletiva [Internet]. 2011 jun [citado 2020 jun 8];16(6):2753-62. Disponível em: http://dx.doi.org/10.1590/S1413-81232011000600014 [ Links ]
29. Romanholo HSB, Souza EA, Ramos Júnior AN, Kaiser ACGCB, Silva IO, Brito AL, et al. Surveillance of intradomiciliary contacts of leprosy cases: perspective of the client in a hyperendemic municipality. Rev Bras Enferm [Internet]. 2018 Jan-Feb [cited 2020 Jun 8];71(1):163-9. Available from: http://dx.doi.org/10.1590/0034-7167-2016-0607 [ Links ]
30. Souza EA, Ferreira AF, Boigny RN, Alencar CH, Heukelbach J, Martins-Melo FR, et al. Leprosy and gender in Brazil: trends in the endemic area of the Northeast region, 2001-2014. Rev Saúde Pública [Internet]. 2018 Feb [cited 2020 Jun 8];52:20. Available from: http://dx.doi.org/10.11606/s1518-8787.2018052000335 [ Links ]
* Article derived from the Master’s Degree dissertation entitled ‘Epidemiological, sociodemographic, clinical and operational patterns of overlapping leprosy cases in household social networks in municipalities of the North and Northeast regions of Brazil’, defended by Reagan Nzundu Boigny at the Federal University of Ceará (UFC) Public Health Postgraduate Program in 2018. The study received financial support from the National Scientific and Technological Development Council (CNPq)/Ministry of Science, Technology, Innovation and Communication (MCTIC) (Process No. 404505/2012-0, MCTI/CNPq/MS-SCTIE-Decit No. 40/2012 – Research on Neglected Diseases); and from Netherlands Hanseniasis Relief / Brazil (NHR Brazil), via a project to characterize leprosy case spatial and temporal distribution patterns focusing on vulnerability associated with leprosy recurrence in families and early detection of new cases (Opinion No. 2.365.953; Certification of Submission for Ethical Appraisal – CAAE No. 72571517.4.0000.5054). Alberto Novaes Ramos Junior is a CNPq/MCTIC Productivity grantee. Reagan Nzundu Boigny was a CNPq/MCTIC Master’s Degree grantee.
Received: January 31, 2020; Accepted: May 19, 2020











 texto en
texto en 


