Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.4 Brasília 2020 Epub 25-Ago-2020
http://dx.doi.org/10.5123/s1679-49742020000400016
ORIGINAL ARTICLE
Snakebite in Tocantins: ecological analysis of determinants and risk areas, 2007- 2015 *
1Secretaria de Saúde do Estado do Tocantins, Vigilância Epidemiológica de Zoonoses e Acidentes por Animais Peçonhentos, Palmas, TO, Brazil
2Universidade Federal da Bahia, Instituto de Saúde Coletiva, Salvador, BA, Brazil
Objective
To investigate the epidemiological profile of snakebite accident cases, their determinants and risk areas in the state of Tocantins.
Methods
This was an ecological study using data from the Notifiable Health Conditions Information System, from 2007 to 2015. Multiple linear regression and the Mann-Whitney and Kruskal-Wallis tests were used.
Results
A total of 7,764 snakebite accidents were reported (incidence: 62.1/100,000 inhab.; lethality: 0.5%). The variables associated with snakebite were population density (Coeff.=1.36, 95%CI 0.72;1.99), farming work (Coeff.=0.02, 95%CI 0.01;0.03), municipal human development index (Coeff.=2.99 – 95%CI 0.60;5.38), area planted with cassava (Coeff.=8.49 – 95%CI 1.66;15.32), indigenous population (Coeff.=0,02 – 95%CI 0.00; 0.04), proportion of illiterate people (Coeff.=4.70 – 95%CI 0.61;8.79) and employed people (Coeff.=3.00 – 95%CI 0.93;5,06), which together accounted for 64.48% of the variation. The high-risk areas were Amor Perfect, Cantão, Cerrado Tocantins Araguaia and Mid-North Araguaia health regions.
Key words: Snake Bites; Ecological Studies; Health Profile; Risk Zone
Introduction
Snakebite accidents persist as a Public Health problem, owing to the assiduity with which they occur and the morbidity and mortality they cause, principally in tropical countries where the world’s most diverse snakes of medical importance are found.( 1 )This health condition frequently affects young male rural workers of economically active age.( 1 )
In 2009, the World Health Organization (WHO) included snakebites on its list of neglected tropical diseases. In 2019 it was estimated that globally every year there are 2,700,000 cases of snakebite envenoming and between 81,000 and 138,000 deaths, as well as 400,000 victims who survive with physical disability and psychological harm.2Despite these estimates, global data are relatively incipient, and the total number of affected people is underestimated.( 1 )
In the period selected for the study, there were approximately 28,500 snakebite accidents a year in Brazil, with an incidence rate of 14.5/100,000 inhab. and 0.41% lethality,( 6 )this being nine times higher than the global estimate. Brazil’s Northern region stands out due to its high incidence rate: 56.0 cases/100,000 inhab.( 4 )
Knowledge about snakebites has advanced a great deal in recent decades,( 8 )although there have been few investigations from a perspective of the spatial context considering the occurrence of this health condition as a complex societal event, given that socioeconomic and environmental conditions can be risk factors.( 4 )
The objective of this study was to investigate the profile of snakebite accident cases, their determinants and risk areas in the state of Tocantins, Brazil.
Methods
This was a multiple-group ecological study, in which municipalities were the units of analysis for the occurrence of snakebite accidents between 2007 and 2015 in the state of Tocantins.
Tocantins is part of Brazil’s Northern region and its main economic activities are agriculture and livestock rearing.( 10 )The state has 139 municipalities, a territorial area of 277,720.567km2and an estimated population of 1,515,126 inhabitants.( 11 )Indigenous people account for approximately 5% of this population, distributed between nine ethnic groups: Apinayé; Xerente; Karajá; Krahô; Xambioá; Krahô-Kanela; Javaé; Pankararu; and Avá-Canoeiro.( 10 )Tocantins has a human development index (HDI) of 0.699 and a Gini index of 0.60: 32.36% of its population are in a situation of poverty.( 11 )The state is comprised of eight health regions: Mid-North Araguaia; Bico do Papagaio; Southeast; Cerrado Tocantins Araguaia; Ilha do Bananal; Capim Dourado; Cantão; and Amor Perfeito.( 13 )
All of the state’s municipalities were included in the study, since all of them notified snakebite cases in the selected period.
Data relating to snakebite characterization were retrieved from the Tocantins State Health Department (SESAU/TO) Notifiable Health Conditions Information System (SINAN), by municipality of occurrence. The socioeconomic and demographic variables were obtained from the Brazilian Institute of Geography and Statistics (IBGE) and from the Brazilian Human Development Atlas. Data from the 2010 census was used, as were statistical projections for the intercensal periods.
The variables relating to affected people were:
sex (male; female);
age (in years: <15; 15-34; 35-54; 55 or over);
schooling (no schooling; up to complete elementary education; complete high school education; complete higher education; no information);
race/skin color (white; black; yellow; brown; indigenous; no information); and
occupation (farming; worker in general; no information).
With regard to snakebite accidents, the variables investigated were:
municipality of occurrence;
zone (urban; rural; peri-urban; no information);
month of occurrence;
anatomic site of snakebite (torso; lower limbs; upper limbs; no information);
snake genus ( Bothrops , Crotalus , Micrurus , Lachesis ; not venomous; no information);
time elapsed between accident and health care (up to six hours; over six hours; no information);
stage (mild; moderate; severe; no information);
clinical evolution (cure; death; no information); and
work-related accident (yes; no; no information).
The following variables were investigated per municipality:
municipal human development index (MHDI);
Gini index;
gross domestic product (GDP) per capita (U$);
population employed (%);
area used for agriculture (%);
population employed in farming (%);
population with access to water and refuse collection (%);
proportion of illiteracy among people aged 15 years or over (%);
proportion of indigenous people in the municipality in relation to the overall municipal population (%);
population density (inhab./km2); and
climatic aspect (dry period; rainy period).
The variables related to farming were selected based on the main activities developed in Tocantins, per municipality, taking 2015 as the reference year. The variables specifically relating to agriculture were the planted areas (in km2) of rice, pineapple, banana, sugar cane, beans, cassava, water melon, corn, soya and sorghum. With regard to livestock rearing, we considered the effective total herd, per head of cattle, goat, horse, chicken and pig. All the socioeconomic data were retrieved from the IBGE database.
We calculated the snakebite incidence rate (number of cases divided by the population, per 100,000 inhab.), the snakebite mortality rate (number of deaths divided by the population, per 100,000 inhab.) and snakebite lethality (proportion of the number of deaths in relation to the number of cases), by year and by municipality. The epidemiological profile was described according to the absolute and relative frequencies of the variables relating to those who suffered snakebite accidents and to the accidents themselves.
In the multiple linear regression analysis, the municipal demographic and socioeconomic variables were considered to be exposure. Municipal snakebite cases recorded in the period were the response variable. Association between snakebite and the municipal demographic and socioeconomic variables was analyzed through multiple linear regression. Variables that reached a 5% significance level in the unadjusted model were selected and submitted to analysis. The results were presented as coefficients (Coeff.) and 95% confidence intervals (95%CI). The Akaike information criterion (AIC) was used to assess quality of model fit. In order to investigate seasonality, analysis was performed on association between monthly accident frequency per seasonal period (dry period, from May to September; and rainy period, from October to April), using the Mann-Whitney test. In order to identify risk areas, the Kruskal-Wallis non-parametric (adjusted p-value) test was used. The resulting clusters were classified as being low risk or high risk, based on the snakebite incidence coefficients. Maps were later produced for the purposes of spatial distribution analysis.
Stata®version 12.0 was used for linear regression, Mann-Whitney and Kruskal-Wallis test processing; and Tabwin version 3.6, available from the Brazilian National Health System Information Technology Department (DATASUS)/Health Ministry), was used to produce the maps.
The study project was approved by the Federal University of Bahia Public Health Institute Research Ethics Committee (CEP/ISC/UFBA): Opinion No. 2.091.150, dated May 30th2017.
Results
In Tocantins, 7,764 snakebite accidents were notified between 2007 and 2015. Average incidence for the state as a whole was 62.1/100,000 inhab., varying between 52.2 and 78.4/100,000 inhab. ( Figure 1 ). The municipal incidence rate varied between 2.8 and 288.8/100,000 inhab. The municipalities with the highest incidence were Recursolândia (288.8/100,000 inhab.), Centenário (260.4/100,000 inhab.), Tocantínia (252.8/100,000 inhab.), Santa Maria (240.0/100,000 inhab.) and Conceição do Tocantins (235.3/100,000 inhab.) ( Figure 2 ).

Sources: Notifiable Health Conditions Information System (SINAN)/Tocantins State Health Department (SESAU/TO) and Brazilian Institute of Geography and Statistics (IBGE).
Figure 1 – Incidence rate (per 100,000 inhab.), lethality (%) and mortality rate (per 100,000 inhab.) of snakebite accidents in the state of Tocantins, Brazil, 2007-2015
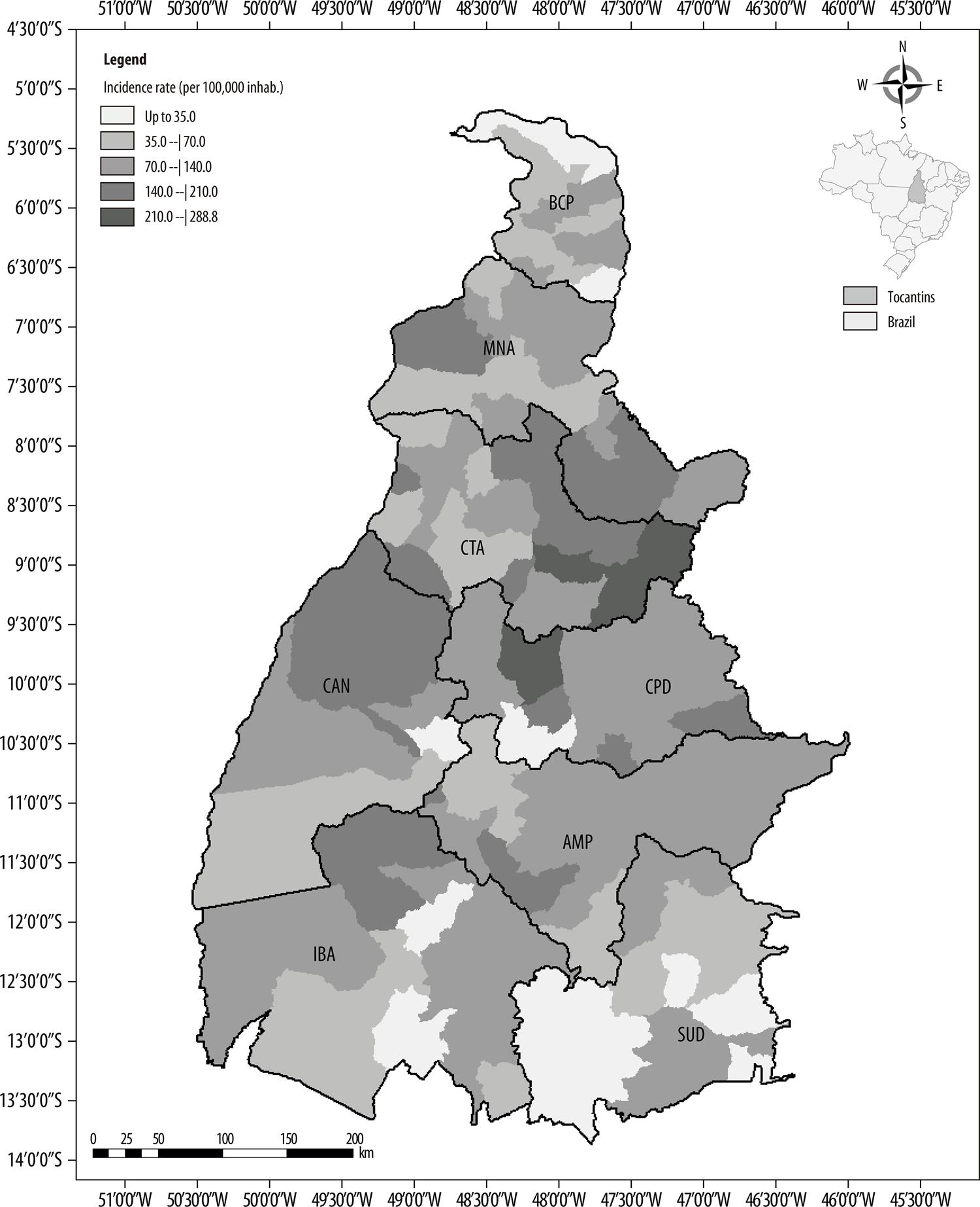
Source: Notifiable Health Conditions Information System (SINAN)/Tocantins State Health Department (SESAU/TO).
Figure 2 – Spatial distribution of snakebite accidents according to cumulative incidence rate (per 100,000 inhab.) in the municipalities comprising the health regions of the state of Tocantins, 2007-2015Legend:APE: Amor PerfeitoBCP: Bico do PapagaioCAN: CantãoCPD: Capim DouradoCTA: Cerrado Tocantins-AraguaiaIBA: Ilha do BananalMNA: Mid-North AraguaiaSUD: Southeast
The Mid-North Araguaia and Cerrado Tocantins Araguaia health regions notified the largest number of cases, accounting for 22.7% and 16.8% of the records, respectively. The Mid-North Araguaia and Cerrado Tocantins Araguaia health regions also had the highest incidence coefficients, 97.3/100,000 inhab. and 89.1/100,000 inhab., respectively ( Table 1 and Figure 3 ).
Table 1 – Classification of snakebite accident risk areas among the health regions of the state of Tocantins, Brazil, 2007-2015
| Health regions | APE | BCP | CAN | CPD | CTA | IBA | MNA | SUD | Risk classification | Incidence coefficient (per 100,000 inhab.) |
|---|---|---|---|---|---|---|---|---|---|---|
| APE | – | Different | Same | Different | Same | Different | Same | Different | High | 80.9 |
| BCP | Different | – | Different | Same | Different | Same | Different | Same | Low | 43.9 |
| CAN | Same | Same | – | Different | Same | Different | Same | Different | High | 75.3 |
| CPD | Different | Different | Different | – | Different | Same | Different | Same | Low | 40.8 |
| CTA | Same | Different | Same | Different | – | Different | Same | Different | High | 89.1 |
| IBA | Different | Same | Different | Different | Different | – | Different | Same | Low | 48.4 |
| MNA | Different | Different | Same | Different | Same | Different | – | Different | High | 97.3 |
| SUD | Different | Same | Different | Same | Different | Same | Different | – | Low | 45.7 |
a) According to the Kruskal-Wallis test, with White robust correction.
Legend:
APE: Amor Perfeito
BCP: Bico do Papagaio
CAN: Cantão
CPD: Capim Dourado
CTA: Cerrado Tocantins-Araguaia
IBA: Ilha do Bananal
MNA: Mid-North Araguaia
SUD: Southeast
Note:
In this comparison between median municipal incidence for each health region, (i) ‘different’ means that the medians are statistically distinct, and (ii) ‘same’ means that there is no statistically significant difference between the regions.
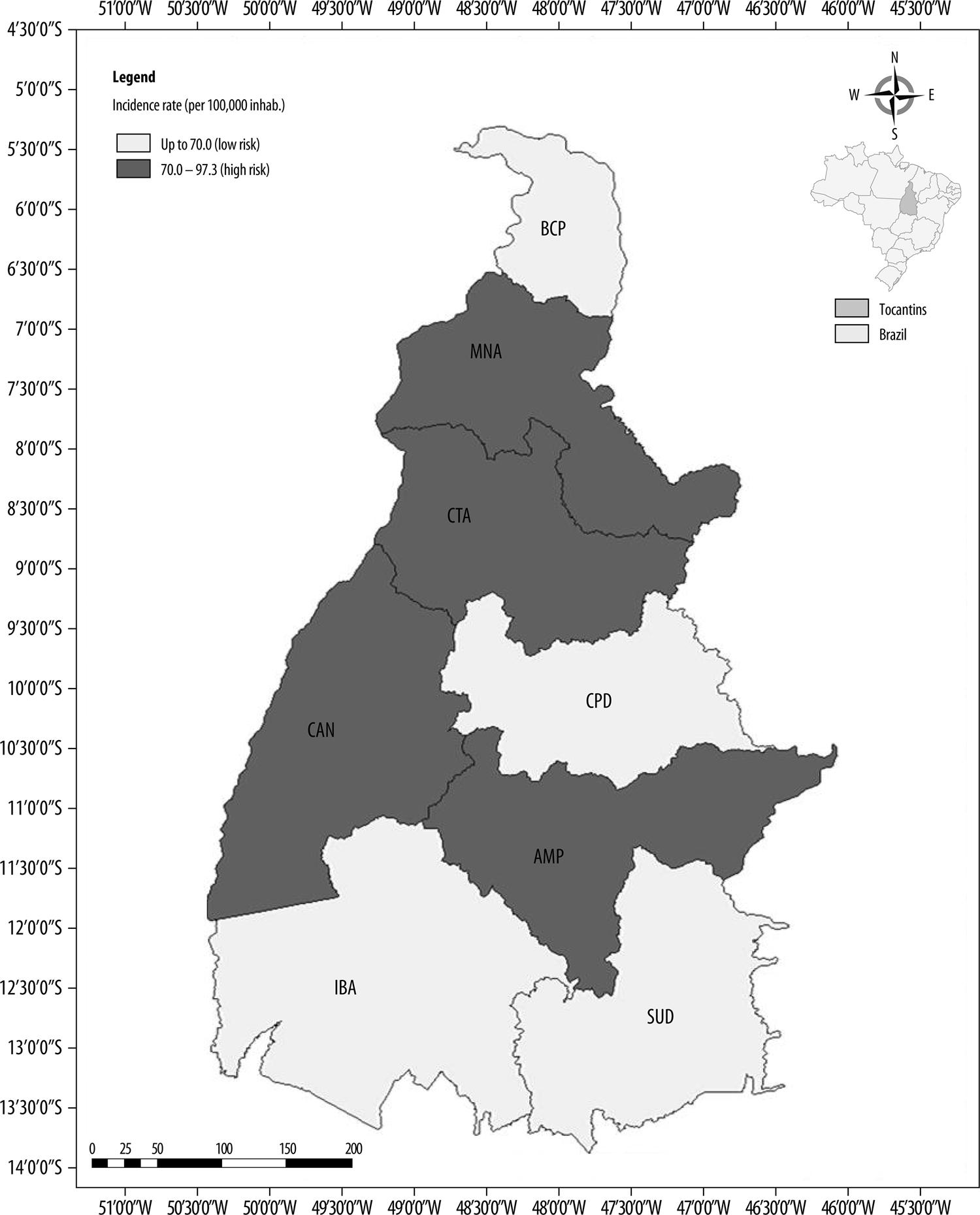
Figure 3 – Map of snakebite accident risk areas in the health regions of the state of Tocantins, 2007-2015Legend:APE: Amor PerfeitoBCP: Bico do PapagaioCAN: CantãoCPD: Capim DouradoIBA: Ilha do BananalCTA: Cerrado Tocantins-AraguaiaSUD: SudesteMNA: Médio Norte Araguaia
In the period there were 36 deaths, so that average lethality for the state was 0.5%, varying between 0.3% and 0.9%, while for the municipalities it varied between 0.0 and 8.7%. Crotalus accidents were the most lethal (1.4%), followed by Bothrops accidents (0.4%). No deaths due to Micrurus or Lachesis bites were recorded. Snake genus was not informed for three deaths. Mortality varied between 0.0 and 0.5/100,000 inhab. among the municipalities ( Figure 1 ).
Accidents occurred mainly during the rainy period (65.3%) (p<0.001). The majority of the people who were bitten were male (76.9%) and aged between 15 and 34 years (36.3%). Information was missing on schooling in 21% of cases, while among case notifications that did have information on this variable, schooling no further than elementary education was predominant (61.7%). Occupation, when reported, identified farm workers (31.1%) as the most affected. With regard to race/skin color, 76.6% were of brown skin color and 4.1% were indigenous ( Table 2 ).
Table 2 – Distribution of snakebite cases according to associated characteristics, by triennium, in the municipalities (139) of the state of Tocantins, 2007-2015
| Variables | 2007-2009 | 2010-2012 | 2013-2015 | 2007-2015 | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N (2,356) | (%) | N (2,991) | (%) | N (2,417) | (%) | N (7,764) | (%) | |
| Sex | ||||||||
| Male | 1,839 | 78.1 | 2,275 | 76.1 | 1,856 | 76.8 | 5,970 | 76.9 |
| Female | 517 | 21.9 | 716 | 23.9 | 561 | 23.2 | 1,794 | 23.1 |
| Age (years) | ||||||||
| <15 | 404 | 17.1 | 566 | 18.9 | 436 | 18.0 | 1,406 | 18.1 |
| 15-34 | 926 | 39.4 | 1,078 | 36.0 | 815 | 33.8 | 2,819 | 36.3 |
| 35-54 | 691 | 29.3 | 893 | 29.9 | 743 | 30.7 | 2,327 | 30.0 |
| ≥55 | 335 | 14.2 | 454 | 15.2 | 423 | 17.5 | 1,212 | 15.6 |
| Schooling | ||||||||
| No schooling | 139 | 5.9 | 145 | 4.8 | 111 | 4.6 | 395 | 5.1 |
| Complete elementary education | 1,639 | 69.6 | 1,812 | 60.6 | 1,330 | 55.0 | 4,781 | 61.7 |
| Complete high school education | 97 | 4.1 | 197 | 6.6 | 212 | 8.8 | 506 | 6.5 |
| Complete higher education | 13 | 0.6 | 23 | 0.8 | 29 | 1.1 | 65 | 0.8 |
| Not applicable | 114 | 4.8 | 142 | 4.7 | 127 | 5.3 | 383 | 4.9 |
| No information | 354 | 15.0 | 672 | 22.5 | 608 | 25.2 | 1,634 | 21.0 |
| Occupation | ||||||||
| Farming | 750 | 31.8 | 969 | 32.4 | 693 | 28.7 | 2,412 | 31.1 |
| Work in general | 159 | 6.7 | 202 | 6.8 | 223 | 9.2 | 584 | 7.4 |
| Other | 556 | 23.6 | 674 | 22.5 | 576 | 23.8 | 1,806 | 23.3 |
| No information | 891 | 37.9 | 1,146 | 38.3 | 925 | 38.3 | 2,962 | 38.2 |
| Race/skin color | ||||||||
| White | 278 | 11.8 | 245 | 8.2 | 178 | 7.4 | 701 | 9.0 |
| Black | 204 | 8.7 | 232 | 7.8 | 174 | 7.2 | 610 | 7.9 |
| Yellow | 40 | 1.6 | 30 | 1.0 | 34 | 1.4 | 104 | 1.3 |
| Brown | 1,724 | 73.2 | 2,330 | 77.9 | 1,895 | 78.4 | 5,949 | 76.6 |
| Indigenous | 87 | 3.7 | 123 | 4.1 | 107 | 4.4 | 317 | 4.1 |
| No information | 23 | 1.0 | 31 | 1.0 | 29 | 1.2 | 5,970 | 1.1 |
| Snake genus | ||||||||
| Bothrops | 1,761 | 74.8 | 2,390 | 79.9 | 1,840 | 76.1 | 5,991 | 77.2 |
| Crotalus | 262 | 11.1 | 260 | 8.7 | 243 | 10.1 | 765 | 9.9 |
| Micrurus | 19 | 0.8 | 17 | 0.6 | 12 | 0.5 | 48 | 0.6 |
| Lachesis | 18 | 0.8 | 13 | 0.4 | 7 | 0.3 | 38 | 0.5 |
| Not venomous | 133 | 5.6 | 128 | 4.3 | 151 | 6.2 | 412 | 5.2 |
| No information | 163 | 6.9 | 183 | 6.1 | 164 | 6.8 | 510 | 6.6 |
| Zone of occurrence | ||||||||
| Urban | 308 | 13.1 | 365 | 12.2 | 366 | 15.1 | 1,039 | 13.4 |
| Rural | 1,970 | 83.6 | 2,514 | 84.1 | 1,963 | 81.2 | 6,447 | 83.0 |
| Peri-urban | 42 | 1.8 | 54 | 1.8 | 38 | 1.6 | 134 | 1.7 |
| No information | 36 | 1.5 | 58 | 1.9 | 50 | 2.1 | 144 | 1.9 |
| Climatic aspect – rainfall | ||||||||
| More rain | 1,480 | 62.8 | 2,009 | 67.2 | 1,582 | 65.5 | 5,071 | 65.3 |
| Less rain | 876 | 37.2 | 982 | 32.8 | 835 | 34.5 | 2,693 | 34.7 |
| No information | – | 0.0 | – | 0.0 | – | 0.0 | – | 0.0 |
| Time elapsed between accident and care | ||||||||
| Up to six hours | 1,912 | 81.1 | 2,500 | 83.6 | 2,018 | 83.4 | 6,430 | 82.8 |
| Over six hours | 324 | 13.8 | 362 | 12.1 | 301 | 12.5 | 987 | 12.7 |
| No information | 120 | 5.1 | 129 | 4.3 | 98 | 4.1 | 347 | 4.5 |
| Anatomic site of snakebite | ||||||||
| Torso | 22 | 0.9 | 33 | 1.1 | 29 | 1.2 | 84 | 1.1 |
| Lower limbs | 1,951 | 82.8 | 2,434 | 81.4 | 1,996 | 82.6 | 6,381 | 82.2 |
| Upper limbs | 358 | 15.2 | 480 | 16.0 | 361 | 14.9 | 1,199 | 15.4 |
| No information | 25 | 1.1 | 44 | 1.5 | 31 | 1.3 | 100 | 1.3 |
| Stage | ||||||||
| Mild | 1,140 | 48.4 | 1,311 | 43.9 | 1,123 | 46.5 | 3,574 | 46.0 |
| Moderate | 947 | 40.2 | 1,361 | 45.5 | 1,012 | 41.9 | 3,320 | 42.8 |
| Severe | 169 | 7.2 | 160 | 5.3 | 166 | 6.9 | 495 | 6.4 |
| No information | 100 | 4.2 | 159 | 5.3 | 116 | 4.8 | 375 | 4.8 |
| Clinical evolution | ||||||||
| Cure | 2,314 | 98.2 | 2,896 | 96.8 | 2,212 | 91.5 | 7,422 | 95.7 |
| Death | 17 | 0.7 | 11 | 0.4 | 14 | 0.6 | 36 | 0.5 |
| No information | 25 | 1.1 | 84 | 2.8 | 191 | 7.9 | 300 | 3.8 |
| Work-related accident | ||||||||
| Yes | 687 | 29.2 | 906 | 30.3 | 542 | 22.4 | 2,135 | 27.5 |
| No | 1,574 | 66.8 | 1,926 | 64.4 | 1,644 | 68.0 | 5,144 | 66.3 |
| No information | 95 | 4.0 | 159 | 5.3 | 231 | 9.6 | 485 | 6.2 |
The majority of accidents involved the Bothrops genus (77.2%). In 6.6% of cases the snake was not identified and in 5.2% the snake was not venomous. Most of the accidents occurred in the rural zone (83.0%), with medical care being provided in the first hours following snakebite (82.8%). The lower limbs were the most affected (82.2%). Cases were predominantly classified as being of mild severity (46.0%) and most cases were cured (95.7%). Accidents were work-related in 27.5% of cases ( Table 2 ).
Following unadjusted analysis, the following variables achieved statistical significance (5%): MHDI (Coeff.=4.29 – 95%CI 2.04;6.55), Gini index (Coeff.=1.48 – 95%CI 0.63;4.32), population density (Coeff.=1.78 – 95%CI 0.99;2.58), proportion of illiteracy (Coeff.=4.78 – 95%CI 2.60;6.96), unemployment among over eighteen-year-olds (Coeff.=2.48 – 95%CI 0.63;4.32) and areas planted with soya (Coeff.=0.12 – 95%CI 0.02;0.21), cassava (Coeff.=20.60 – 95%CI 13.65;27.65), corn (Coeff.=0.31 – 95%CI 0.07;0.55), sorghum (Coeff.=5.56 – 95%CI 2.08;9.05), beans (Coeff.=4.67 – 95%CI 0.15;9.19) and bananas (Coeff.=58.58 – 95%CI 33.55;83.63).
Multiple linear regression revealed strong snakebite association (p<0.001) with 7 of the 16 variables investigated: population density; farm work; MHDI; area planted with cassava; indigenous people; illiteracy rate; and employment ( Table 3 ). The proposed model explained 64.48% (R2adjusted = 0.6448) of snakebites in Tocantins.
Table 3 – Final model of snakebite accident multiple linear regression analysis according to farming, geographical and socioeconomic variables in the municipalities (139) of the state of Tocantins, 2007-2015
| Variables | Coefficient | T-test | p-value >| t |a | 95%CIb |
|---|---|---|---|---|
| Population density (inhab./km2) | 1.36 | 4.23 | 0.001 | 0.72;1.99 |
| Farming work | 0.02 | 3.54 | 0.001 | 0.01;0.03 |
| MHDIc | 2.99 | 2.47 | 0.015 | 0.60;5.38 |
| Area planted with cassava (km2) | 8.49 | 2.46 | 0.015 | 1.66;15.32 |
| Indigenous population | 0.02 | 2.32 | 0.022 | 0.00; 0.04 |
| Illiteracy | 4.70 | 2.28 | 0.024 | 0.61; 8.79 |
| Employment | 3.00 | 2.87 | 0.005 | 0.93;5.06 |
| Constant (cases/100,000 inhab.) | -540.38 | -4.39 | 0.001 | -784.15;-296.60 |
a) P-value derived from T-test.
b) 95%CI: 95% confidence interval.
c) MHDI: municipal human development index.
Note:
R2adjusted = 0.6448.
Akaike information criterion (AIC) = 460.45..
Table 1 shows the results of the Kruskal-Wallis test. With regard to risk of snakebite accident, comparison between health regions identified two distinct areas (p<0.005): (i) a high-risk area with cumulative incidence of 85.7/100,000 inhab., comprised of the Amor Perfeito, Cantão, Cerrado Tocantins Araguaia and Mid-North Araguaia health regions; and a (ii) “low-risk” area with cumulative incidence of 44.7/100,000 inhab., comprised of the Bico do Papagaio, Capim Dourado, Ilha do Bananal and Southeast health regions.
Discussion
The analyses of notified snakebite cases in Tocantins between 2007 and 2015 provided evidence that this type of accident affects above all young male adult rural workers involving Bothrops envenoming of lower limbs. The cases were distributed unequally, delimitating high-risk areas (the Amor Perfeito, Cantão, Cerrado Tocantins Araguaia and Mid-North Araguaia health regions) and “low risk” areas (the Bico do Papagaio, Capim Dourado, Ilha do Bananal and Southeast regions). Snakebite accidents were related to population density, farm work, MHDI, areas planted with cassava, indigenous people, illiteracy rate and employment.
The epidemiological profile we found is in keeping with the global, national and regional patterns.( 1 )Early medical care found by us diverged from the tardiness commonly reported in the North Brazilian region,( 7 )probably because Tocantins differs within the region with regard to the main issues of geographic accessibility characteristic of the Amazon.( 4 )
In the period studied, Tocantins had the third highest snakebite incidence coefficient in Brazil as a whole and in the country’s Northern region, after the states of Roraima and Pará.( 6 )In majority of the municipalities, incidence was higher than the national average.( 6 )This emphasizes the need for municipal health plans to address snakebite, circumstantially increasing effective health surveillance and health education focused on improving case notification quality and prevention. Agreements need to be reached between municipalities or health regions with the aim of building networks to provide timely health care.
In all the health regions, including those that comprise the region at “low risk” of snakebites, risk was three times higher in relation to national parameters when taking the same period studied as a reference.( 6 )When compared to the national pattern, all of the Tocantins health regions are high risk.
Situation analysis of this health condition in the state, including “low-risk” and high-risk snakebite areas, seasonality and geographical barriers, needs to be taken into account to guide strategies for antiophidic sera distribution and surveillance action strengthening. This dedication to continuous and timely analysis is imperative in view of possible problems regarding access to certain areas, low sera stock levels and lack of availability of these immunobiologics in the municipalities, either because they are not considered risk areas or because health centers there are not adequately prepared to provide serotherapy.( 16 )
Average lethality for the state was comparable to the national average for the same period. However, the estimate found for the municipality of Tupirama is problematic, given that antiophidic sera are available through Brazil’s public health network.( 17 )Lethality is known to be a complex outcome influenced by diverse factors, such as snake genus, use of tourniquets and snakebites on the extremities of the body (fingers and toes), as well as by the time elapsed between the accident and health care (above all in cases coming from the rural zone), type of serum and number of phials used, whereby these three latter factors are health service-related.( 18 )These factors must be considered when analyzing the occurrence of severe cases and, consequently, deaths due to snake envenoming.
In Tocantins, farm work was associated with snakebites. Social weaknesses such as low schooling and illiteracy, typical among people affected by snakebites, are recurrent in this occupational group.( 19 )This situation appears to reflect the invisibility of these workers when formulating occupational health policies and protection programs. The scenario is particularly serious when snakebite is a condition that is easy to prevent by making personal protective equipment (PPE) available, but which is constantly not used during farming activities.( 18 )Areas planted with cassava ( Manihot esculenta Crantz) (in planted km2), were particularly associated with snakebite in the state. Growing this crop involves intense use of the ground and preparation of the soil for planting can cause deforestation impacts.( 20 )
Association between MHDI and snakebite may be related to the farming economy predominant in the state. Population density was strongly associated with snakebite in Tocantins. This pattern is consistent with findings for the American continent in 2017, although different to findings for Rio de Janeiro in 2004.( 21 )As Tocantins is Brazil’s most recent state, it is undergoing demographic expansion, with greater population dynamics in municipalities where farming activities are intense and encouraged through tax incentives for large corporations.( 22 )This scenario is propitious to people being recruited for rural work. In keeping with this association, the ‘employment’ variable was related to snakebite, probably due to the economic profile of the municipalities being predominantly farming-related.( 11 )These findings suggest that job activities related to agriculture (planting, harvesting, packing, transport etc.) and livestock rearing are carried out without adequate protection, this being a classic snakebite scenario.( 23 )
Absence of schooling as a determining factor provides evidence of a social vulnerability problem. This pattern has been pointed to since the work of Vital Brazil with snake-bitten individuals in Southeast Brazil at the beginning of the 20thcentury.( 24 )It is therefore essential to address this form of vulnerability with public policies that prioritize effective actions for provision of PPEs to rural workers and raising their awareness as to their use, taking into consideration local aspects of seasonality and farming activities.
Association between snakebite and indigenous populations reinforces the need for studies involving them. It is a complex theme found in scarce scientific studies about snakebites in this ethnic group. Specific knowledge about the epidemiological situation of snake envenoming in these populations is essential for the formulation of effective public policies aimed at improving health care for indigenous people. However, it is also essential to expand the discussion about environmental preservation beyond indigenous areas, as a strategy for avoiding snakes taking refuge and becoming concentrated close to this ethnic group.
The results of this study should be considered in the light of certain limiting conditions, such as underreporting and incompleteness of notification data on the SINAN system, especially with regard to socioeconomic variables. Historically, these attributes have been subject to problems in notification, notwithstanding the quality of data filling-in having improved more recently. Another issue to bear in mind are the methodological limitations inherent to the ecological study design.
We conclude that there is high snakebite incidence in Tocantins and that it is strongly associated with sociodemographic attributes and the municipal farming profile. The study also pointed out areas of greater occurrence. This result can assist with the planning of antiophidic sera distribution in the state. Vulnerable societal groups were strongly associated with snakebites in Tocantins, as were municipal farming and demographic characteristics related to social inequalities, impacts on ways of life and new health needs of rural workers.
Snakebite accident surveillance in Tocantins needs to be prioritized, in the sense of strengthening health education in relation to prevention, provision of first aid, diagnosis and treatment, as well as clinical management and efficient antivenom distribution. As such, it is fundamental to take into consideration risk areas, spatial and seasonal distribution of cases and geographic barriers to access to health care.
REFERENCES
1. World Health Organization - WHO. Guidelines for the management of snakebites [Internet]. 2. ed. New Delhi: World Health Organization; 2016 [cited 2020 Jun 29]. 140 p. Available from: https://www.who.int/snakebites/resources/9789290225300/en/ [ Links ]
2. Williams DJ, Faiz MA, Abela-Ridder B, Ainsworth S, Bulfone TC, Nickerson AD, et al. Strategy for a globally coordinated response to a priority neglected tropical disease: Snakebite envenoming. PLoS Negl Trop Dis [Internet]. 2019 Feb [cited 2020 Jun 29];13(2):e0007059. Available from: https://doi.org/10.1371/journal.pntd.0007059 [ Links ]
3. Silva AM, Bernarde PS, Abreu LC. Acidentes com animais peçonhentos no Brasil por sexo e idade. J Human Grow Dev [Internet]. 2015 [citado 2020 jun 29];25(1):54-62. Disponível em: http://dx.doi.org/10.7322/jhgd.96768 [ Links ]
4. Silva JC, Guimarães CDO, Palha MC. Perfil clínico-epidemiológico dos acidentes ofídicos ocorridos na ilha de Colares, Pará, Amazônia oriental. Semina Ciênc Biol Saúde [Internet]. 2015 jan-jun [citado 2020 jun 29];36(1):67-78. Disponível em: http://dx.doi.org/10.5433/1679-0367.2015v36n1p67 [ Links ]
5. Magalhães SFV, Peixoto HM, Moura N, Monteiro WM, Oliveira MRF. Snakebite envenomation in the Brazilian Amazon: a descriptive study. Trans R Soc Trop Med Hyg [Internet]. 2019 Mar [cited 2020 Jun 29];113(3):143-51. Available from: https://doi.org/10.1093/trstmh/try121 [ Links ]
6. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Casos - OFIDISMO [Internet]. Brasília: Ministério da Saúde; 2019 [citado 2019 out 20]. Disponível em: https://portalarquivos2.saude.gov.br/images/pdf/2019/outubro/16/1--Dados-Epidemiologicos-SiteSVS--Setembro-2019-OFIDISMO-CASOS.pdf [ Links ]
7. Bernarde PS. Serpentes peçonhentas e acidentes ofídicos no Brasil. São Paulo: Anolis Books; 2014. [ Links ]
8. Kasturiratne A, Wickremasinghe R, Silva N, Gunawardena N, Pathmeswaran A, Premaratna R, et al. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med [Internet]. 2008 Nov [cited 2020 Jun 29];5(11):e218. Available from: https://doi.org/10.1371/journal.pmed.0050218 [ Links ]
9. Bochner R, Struchiner CJ. Aspectos ambientais e sócio-econômicos relacionados à incidência de acidentes ofídicos no Estado do Rio de Janeiro de 1990 a 1996. Cad Saúde Pública [Internet]. 2004 ago [citado 2020 jun 29];20(4):976-85. Disponível em: http://dx.doi.org/10.1590/S0102-311X2004000400012 [ Links ]
10. Nascimento JB. História e geografia do Tocantins. Goiânia: Editora Kelpes; 2013. [ Links ]
11. Instituto Brasileiro de Geografia e Estatística - IBGE. Cidades: Tocantins [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2017 [citado 2017 abr 20]. Disponível em: http://www.ibge.gov.br/estadosat/perfil.php?sigla=to [ Links ]
12. Atlas do Desenvolvimento Humano no Brasil. Tocantins [Internet]. [S.l.]: Atlas do Desenvolvimento Humano no Brasil; 2013 [citado 2017 maio 3]. Disponível em: http://www.atlasbrasil.org.br/2013/pt/perfil_uf/tocantins [ Links ]
13. Governo do Estado de Tocantins. Secretaria de Estado da Saúde. Resolução CIB Nº 161/2012, 29 de agosto de 2012. Dispõe sobre a conformação das novas regiões de saúde do Estado do Tocantins e as ações e serviços mínimos a serem ofertados nesses territórios [Internet]. Palmas: Governo do Estado de Tocantins; 2017 [citado 2017 abr 15]. Disponível em: https://central3.to.gov.br/arquivo/244723/ [ Links ]
14. Moura VM, Mourão RHV, Santos MC. Acidentes ofídicos na Região Norte do Brasil e o uso de espécies vegetais como tratamento alternativo e complementar à soroterapia. Scientia Amazonia [Internet]. 2015 mar [citado 2020 jun 29];4(1):73-84. Disponível em: http://scientia-amazonia.org/wp-content/uploads/2016/06/v4-n1-73-84-2015.pdf [ Links ]
15. Bernarde OS, Gomes JO. Serpentes peçonhentas e ofidismo em Cruzeiro do Sul, Alto Juruá, Estado do Acre, Brasil. Acta Amazonica [Internet]. 2012 mar [citado 2020 jun 29];42(1):65-72. Disponível em: http://dx.doi.org/10.1590/S0044-59672012000100008 [ Links ]
16. Longbottom J, Shearer FM, Devine M, Alcoba G, Chappuis F, Weiss DJ, et al. Vulnerability to snakebite envenoming: a global mapping of hotspots. Lancet [Internet]. 2018 Jul [cited 2020 Jun 29];392(10148):673-84. Available from: https://doi.org/10.1016/S0140-6736(18)31224-8 [ Links ]
17. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Coordenação-Geral de Desenvolvimento da Epidemiologia em Serviços. Guia de vigilância em saúde [Internet]. Brasília: Ministério da Saúde; 2016 [citado 2020 jun 29]. 773 p. Disponível em: https://portalarquivos.saude.gov.br/images/pdf/2016/agosto/25/GVS-online.pdf [ Links ]
18. Almeida WF. Trabalho agrícola e sua relação com saúde/doença. In: Mendes R, editor. Patologia do trabalho. Rio de Janeiro: Atheneu; 2013. [ Links ]
19. Mise YF, Lira-da-Silva RM, Carvalho FM. Fatal snakebite envenoming and agricultural work in Brazil: a case–control study. Am J Trop Med Hyg [Internet]. 2019 Jan [cited 2020 Jun 29];100(1):150-4. Available from: https://doi.org/10.4269/ajtmh.18-0579 [ Links ]
20. Silva FL, Silva JR, Silva LRP. Efeito do desmatamento e do programa de transferência de renda “Bolsa Família” na produção da mandioca (Manihot esculenta crantz) no Estado do Pará. Obs Econ Latinoame [Internet]. 2014 [citado 2020 jun 29];197. Disponível em: https://econpapers.repec.org/RePEc:erv:observ:y:2014:i:197:14 [ Links ]
21. Chippaux JP. Incidence and mortality due to snakebite in the Americas. PLoS Negl Trop Dis [Internet]. 2017 Jun [cited 2020 Jun 29];11(6):e0005662. Available from: https://doi.org/10.1371/journal.pntd.0005662 [ Links ]
22. Duarte GA, Lemos LCS, Sozinho RB, Sena TM. As (trans)formações socioespaciais no estado do Tocantins e o (des)envolvimento a partir da implantação da rodovia Belém-Brasília (BR-010). Anais XVI Encontro Nacional de Geógrafos; 2010 out 1, Porto Alegre-RS. Porto Alegre; 2010. [ Links ]
23. Mise YM, Lira-da-Silva RM, Carvalho FM. Agriculture and snakebite in Bahia, Brazil - an ecological study. Ann Agric Environ Med [Internet]. 2016 [citado 2020 jun 29];23(3):416-9. Disponível em: https://repositorio.ufba.br/ri/bitstream/ri/22751/1/Yukari%20Figueroa.%20Agriculture...2016.pdf [ Links ]
24. Mott ML, Fabergé O, Alves S, Dias CESB, Fernandes CS, Ibañez N. A defesa contra o ofidismo de Vital Brazil e a sua contribuição à Saúde Pública brasileira. Cad Hist Ciênc [Internet]. 2011 [citado 2020 jun 29];7(2):89-110. Disponível em: http://periodicos.ses.sp.bvs.br/pdf/chci/v7n2/v7n2a06.pdf. [ Links ]
*Article derived from the Master’s Degree dissertation by Shirley Barbosa Feitosa, entitled ‘Epidemiological profile of people affected by snakebite accidents and their determinants in Tocantins’, defended at the Federal University of Bahia (UFBA) Public Health Postgraduate Program in 2017.
Associate Editor: Bárbara Reis-Santos - orcid.org/0000-0001-6952-0352
Received: March 04, 2020; Accepted: May 24, 2020











 texto em
texto em 
 Curriculum ScienTI
Curriculum ScienTI

