Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.4 Brasília 2020 Epub 21-Set-2020
http://dx.doi.org/10.1590/s1679-49742020000400012
ORIGINAL ARTICLE
Health conditions and weight change among the older adults over ten years of the SABE Survey*
1Universidade Federal de Uberlândia, Faculdade de Medicina, Uberlândia, MG, Brazil
2Universidade de São Paulo, Faculdade de Saúde Pública, São Paulo, SP, Brazil
Objective
To analyze the relationship between health conditions and weight changes among elderly people monitored by the SABE Survey over a ten-year period in São Paulo/SP.
Methods
This was a longitudinal study that followed (2000-baseline, 2006 and 2010) change in body weight (outcome variable) and associated health conditions (exposure variables) in the elderly (n=571); multinomial logistic regression analyses were employed.
Results
Average weight increase in the evaluated period was 29.0%. 34.0% (2006) and 12.5% (2010) lost weight and 18.2% (2006) and 39.9% (2010) gained weight. Prevalence of chronic diseases increased from 34.1% (2000) to 51.9% (2006) and 60.1% (2010). Older people with weight gain also rated their overall health as poorer in 2006 (RR:3.15; 95%CI 1.21;8.17) and 2010 (RR:2.46; 95%CI 1.02;5.94). The higher numbers of diseases (RR:2.12; 95%CI 1.00;4.46) and hospitalizations (RR:3.50; 95%CI 1.40;8.72) were associated with a decrease in weight in 2010.
Key words: Aging; Body Weight Changes; Chronic Disease; Nutritional Status; Longitudinal Studies
Introduction
Lower likelihood of disease and good functional capacity are fundamental components for successful aging.(1) Diet and lifestyle, along with maintaining healthy body weight are also crucial for healthy aging.(2)
The elderly are more susceptible to the appearance of chronic diseases, principally due to physiological changes characteristic of this phase of life, such as increased arterial stiffness, reduction in estrogen levels and reduced muscle mass.(3) These conditions can also affect appetite, functional capacity or swallowing, leading to changes in food intake and impairment of nutritional status.(2)
Replacement of the traditional way of life with an industrialized way of life has also driven, even among the elderly, increased weight and chronic disease prevalence.(4) Data from the Family Budgets Survey reveal, for example, that between 2002/2003 and 2008/2009 prevalence of excess weight (overweight and obesity) increased from 45.1% to 53.9% among people 60 to 74 years old and from 32.5% to 43.6% among those aged 75 or over.(5)
International studies indicate greater frailty and mortality among elderly people whose body weight changed.(6) Little is known, however, about the health profile of elderly people living in developing countries whose body weight has changed. Knowledge of this panorama can assist health decision makers in implementing protective measures. As such, the object of this study was to analyze the relationship between health condition and weight change among elderly people monitored by the SABE Survey over a ten-year period in São Paulo/SP.
Methods
This is a population-based longitudinal study. The data originated from the SABE Survey (Saúde, Bem-estar e Envelhecimento - Health, Well-Being and Aging).(8) The survey began in 2000, with follow-up and data collection in 2006, 2010 and 2015 (not assessed in this paper).
Individuals aged 60 or over from a multiple-stage probabilistic sample representative of the city of São Paulo were visited and assessed in 2000 (n=2,143), revisited and reassessed in 2006 (n=1,115) and in 2010 (n=748). (More details are shown in the flowchart in Supplement 1). In addition, new participants aged between 60 and 64 were included in 2006 (n=298) and in 2010 (n=355), with the aim of maintaining the sample’s original and representative age range, as in 2006 and 2010 there were no longer any elderly people aged between 60 and 64 in the sample. The new participants were not included in this study. Details of the methodology have been described in another publication.(9)
Supplement 1Flowchart of total population and losses during SABE Survey follow-up, São Paulo, 2000-2010a) 347 347 incomplete anthopometric data fields in 2000.b) 79 incomplete anthopometric data fields in 2006.c) 90 incomplete anthopometric data fields in 2010.d) 63 individuals who only took part in 2000 and 2010.
Losses during the course of the survey were due to deaths, refusals, institutionalization, unlocated or change of participants’ addresses (Supplement 1 flowchart). All participants for whom data was collected in the three waves of the survey (2000, 2006 and 2010) were included. Those for whom there was no data on height and/or weight (n=114) were excluded as being bedridden.
The estimates for analyses of association calculated a posteriori indicate that the study has power of 90.7%, considering 30% prevalence of weight gain and 10% prevalence of weight loss, in relation to the 571 individuals assessed and a 95% confidence level.
Trained assessors collected data in household interviews using a structured questionnaire covering socioeconomic, overall health status, living conditions and anthropometric measurement variables.(9) When interviewers were not able to answer, a respondent was requested to help (usually a family member).
Variables
Weight change was assessed according to Body Mass Index (BMI) variations over the periods 2000-2006 and 2006-2010. The health condition variables block was use to check for factors associated with these changes. Sociodemographic characteristics described the sample and, due to potential confounding factors, they were used to adjust the regression models.
Dependent variable
The dependent variable was weight change. An individual’s weight was considered to have changed when the difference between the most current BMI in relation to baseline BMI was greater than 5%. Therefore, people were classified in the “weight gain” category when their BMI difference was greater than or equal to +5% in relation to the previous measurement, or were classified in the “weight loss” category when the difference was less than or equal to -5% in relation to the previous measurement. The remaining participants were classified as having “stable weight” (reference category). BMI (kg/m2) was calculated by dividing body mass (in kilograms) by height squared (in meters). Body weight was measured by a trained interviewer, using calibrated weighing scales (brand name SECA®), and height was measured using a stadiometer placed against a wall, with the person being measured barefoot, wearing light clothes, in accordance with Frisancho standardization.(10)
Independent variables
Nutritional status was classified based on the BMI cutoff points adopted by the Pan American Health Organization for the SABE Study: ≤23kg/m2 = underweight; >23.0; <28.0kg/m2 = normal weight; ≥28.0 and <30.0kg/m2 = overweight; ≥30.0kg/m2 = obese. Given the low frequency of participants with excess weight, the two later categories were grouped together, i.e.: those with BMI ≥28.0kg/m2 were considered to be overweight/obese.
The sociodemographic characteristics were: sex; age (in years); schooling (illiterate, 1-3 years, ≥4 years); and marital status (married or not married, divorced, separated or widowed).
Self-reported health conditions were: hospitalization (yes or no); self-rated health (very good and good; regular; or poor and very poor); chronic diseases diagnosed by a doctor (yes or no): hypertension, diabetes, cancer, pulmonary diseases, cerebrovascular accident, cardiovascular disease and osteoarthritis; number of chronic diseases (none or one; two or more).
Statistical analysis
As the data came from multiple-stage cluster sampling, the sample weightings of each participant were used in all the analyses. The Rao-Scott-χ2 test (chi-squared for complex samples) to describe the sample and compare the sociodemographic proportions and health proportions according to weight change and the years assessed (2000-2006 and 2006-2010). Nutritional status categories (underweight, normal weight and obesity) were only used for data description. Comparison of mean age and BMI between assessed participants and lost participants was done using Student’s t-test. In order to verify the relationship between health conditions and weight change, multinomial logistic regression analysis was used in the survey mode for the years 2000-2006 and 2006-2010, estimated by the relative risk ratio (RR) and 95% confidence intervals (95%CI); differences between β values were estimated using the Wald test. In the multinomial models, stable weight was the dependent variable reference category, and chronic diseases were grouped together in the “number of diseases” variable. All the models were adjusted by sex, age, schooling and marital status. At the end of the analyses, the Hosmer-Lemeshow test was used to check model fit quality. A 5% confidence level was used. The data were analyzed using STATA 13.0.
The study was approved by the University of São Paulo Faculty of Public Health Ethics Committee, under control numbers 315 (approved on May 24th 1999), 83 (approved on March 14th 2006) and 2044 (approved on March 5th 2010). The participants were invited to read, approve and sign a consent letter before the assessments and interviews began.
Results
The final sample of this study was comprised of 571 participants, all of whom were assessed in 2000, 2006 and 2010. Between 2000 and 2006, 48.0% of the sample was lost, and a further 32.9% was lost between 2006 and 2010. In both periods the losses were mainly due to deaths (63.1% and 72.8%, respectively). The data on participants lost due to other causes (institutionalization, refusals, moved to another address and not located) were similar to those of the participants who were assessed, while those who died were older and had lower BMI.
The mean age of the elderly people assessed was 73 years in 2000 (SD: 8.25), 75 years in 2006 (SD: 6.65) and 79 years in 2010 (SD: 6.61). Data on lost participants (deaths and other losses) in 2006 and 2010 refer to the last assessment conducted, i.e. in 2000 and 2006, respectively. The mean age of the participants who died was 78 years (SD:8.02) in 2000 and 82 years (SD:7.38) in 2006; mean age of participants lost because of other causes was 71 years (SD:7.51) in 2000 and 76 years (SD:7.01) in 2006. Mean BMI of assessed participants was 27.16kg/m2 in 2000 (SD:4.73), 26.57kg/m2 in 2006 (SD:4.85) and 27.35kg/m2 in 2010 (SD:5.24). Mean BMI of those who died was 25.13kg/m2 (SD:4.95) in 2000 and 24.41kg/m2 (SD:4.49) in 2006; for other losses, mean BMI was 26.63kg/m2 (SD:4.96) in 2000 and 26.19kg/m2 (SD:4,67) in 2006.
Figure 1 shows the participants’ nutritional status and body weight change. Although the proportion of those who remained with the same body weight practically did not change between the years assessed (48.1% in 2000, 45.4% in 2006 and 42.7% in 2010), the increase in the proportion of those who put on weight stands out (18.2% in 2006 and 39.9% in 2010) as does that of those who became obese (35.9% in 2000, 33.7% in 2006 and 40.7% in 2010).
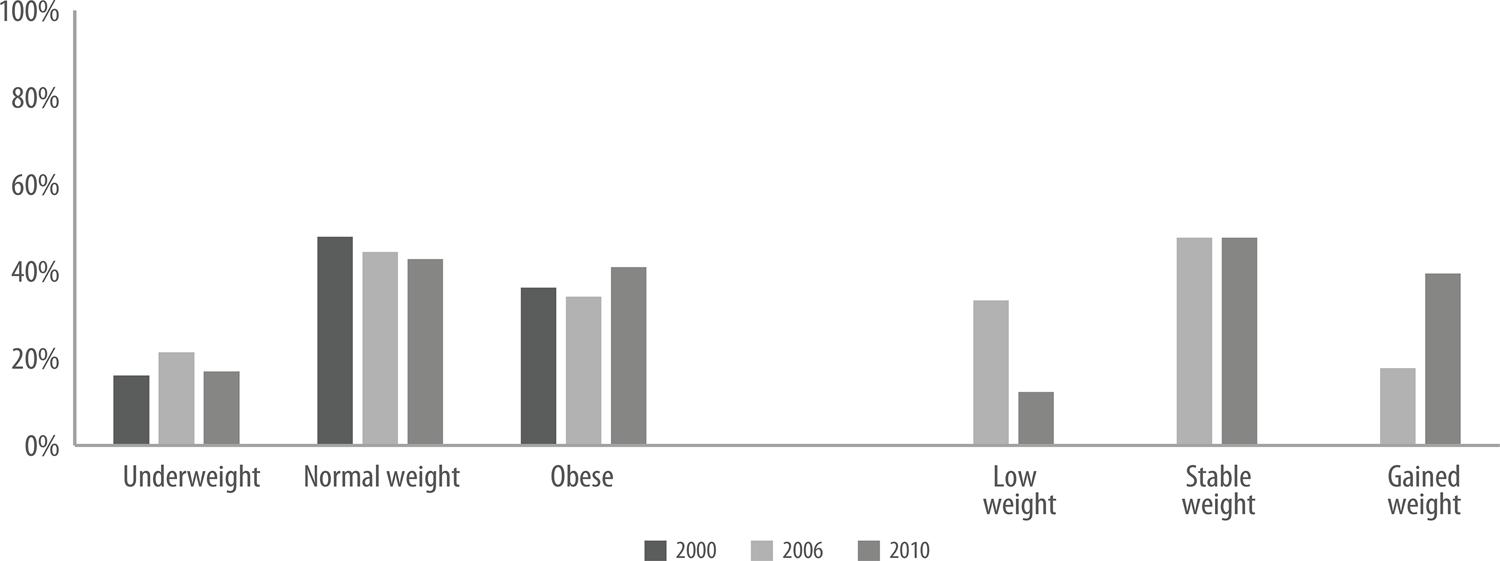
Figure 1 – Nutritional states and change in body weight in elderly people, SABE Survey, São Paulo, 2000, 2006 and 2010ªa) Underweight: BMI ≤23 kg/m2; normal weight: BMI >23 kg/m2 e <28 kg/m2; obese: BMI ≥28 kg/m2 (overweight and obese categories grouped together).
A higher proportion of stable weight was found among those elderly people who self-rated their health as being very good, good or regular, while body weight loss was more frequent among those who had been hospitalized at least once in the last year (Table 1).
Table 1 – Sociodemographic and health characteristics according to weight change in elderly people, SABE Survey, São Paulo, 2000 -2006 and 2006 -2010a
| 2000-2006b | 2006-2010c | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| All participants 2006 | Weight stable | Lost weight | Gained weight | Total 2010 | Weight stable | Lost weight | Gained weight | |
|
|
||||||||
| n=571 | n=271 | n=204 | n=96 | n=571 | n=274 | n=83 | n=214 | |
| Sex | ||||||||
| Female | 63.5 | 46.4 | 35.2 | 18.4 | 63.2 | 43.4 | 14.0 | 42.5 |
| Male | 36.5 | 50.2 | 32.0 | 17.9 | 36.8 | 54.8 | 9.8 | 35.4 |
| Schooling (years) | ||||||||
| Never studied | 15.7 | 44.9 | 36.3 | 18.8 | 17.2 | 54.3 | 14.9 | 30.8 |
| 1-3 years | 29.9 | 48.3 | 32.2 | 19.5 | 31.2 | 40.6 | 8.3 | 51.1* |
| ≥4 years | 54.4 | 48.4 | 34.3 | 17.4 | 51.1 | 49.7 | 14.2 | 36.2 |
| Marital status | ||||||||
| Married | 51.9 | 49.7 | 33.0 | 17.3 | 49.3 | 51.3 | 11.2 | 37.5 |
| Not married | 48.6 | 44.3 | 37.4 | 18.4 | 50.7 | 45.7 | 13.2 | 41.1 |
| Number of diseasesd | ||||||||
| None or 1 | 46.9 | 47.3 | 48.3 | 43.1 | 40.2 | 42.3 | 23.2 | 42.9 |
| ≥2 diseases | 53.1 | 52.7 | 51.7 | 56.9 | 59.8 | 57.7 | 76.8* | 57.1 |
| Hospitalization | ||||||||
| No | 90.9 | 91.9 | 89.0 | 92.1 | 85.3 | 89.5 | 69.9 | 85.0 |
| Yes | 9.1 | 8.1 | 11.0 | 7.9 | 14.7 | 10.5 | 30.1** | 15.0 |
| Self-rated health | ||||||||
| Very good, good | 47.0 | 49.7 | 47.8 | 38.3 | 43.8 | 47.2 | 38.9 | 41.3 |
| Regular | 45.5 | 44.2 | 46.3 | 47.4 | 46.6 | 46.9 | 39.0 | 48.8 |
| Poor, very poor | 7.5 | 6.1 | 5.8 | 14.3 | 9.5 | 5.9 | 22.1 | 9.9** |
| Hypertension | ||||||||
| No | 33.5 | 33.9 | 35.1 | 27.7 | 27.8 | 27.6 | 15.3 | 31.9 |
| Yes | 66.5 | 66.1 | 64.9 | 70.3 | 72.2 | 72.4 | 84.7 | 68.1 |
| Diabetes | ||||||||
| No | 78.0 | 78.9 | 74.8 | 81.9 | 73.0 | 72.7 | 57.1 | 78.3 |
| Yes | 22.0 | 21.1 | 25.2 | 18.1 | 27.0 | 27.3 | 42.9** | 21.7 |
| Cancer | ||||||||
| No | 96.2 | 95.4 | 96.8 | 97.1 | 91.4 | 92.7 | 87.7 | 90.9 |
| Yes | 3.8 | 4.6 | 3.2 | 2.9 | 8.6 | 7.3 | 12.3 | 9.1 |
| Pulmonary diseases | ||||||||
| No | 90.0 | 91.5 | 91.9 | 82.5 | 89.0 | 87.9 | 94.6 | 88.6 |
| Yes | 10.0 | 8.5 | 8.1 | 17.5* | 11.0 | 12.1 | 5.4 | 11.4 |
| Heart disease | ||||||||
| No | 78.0 | 78.6 | 76.2 | 79.5 | 73.2 | 76.7 | 66.1 | 71.3 |
| Yes | 22.1 | 21.4 | 23.8 | 20.5 | 26.8 | 23.3 | 33.9 | 28.7 |
| Stroke/embolism | ||||||||
| No | 92.3 | 93.8 | 91.5 | 90.0 | 89.6 | 90.9 | 85.5 | 89.1 |
| Yes | 7.7 | 6.2 | 8.5 | 10.0 | 10.5 | 9.1 | 14.5 | 10.9 |
| Arthropathies | ||||||||
| No | 62.5 | 61.7 | 65.6 | 58.6 | 63.2 | 61.6 | 63.1 | 65.1 |
| Yes | 37.5 | 38.3 | 34.4 | 41.4 | 36.8 | 38.4 | 36.9 | 34.9 |
a) Rao-Scott-χ2 test for comparisons between groups. The survey method was used in all the analyses.
b) 2000-2006: change in BMI assessed in 2006 compared to BMI in 2000. Weight stable: change in BMI between <-5% and >+5%. Lost weight: change in BMI ≤-5%. Gained weight: change in BMI ≥+5%.
c) 2006-2010: change in BMI assessed in 2010 compared to BMI in 2006. Weight stable: change in BMI between <-5% and >+5%. Lost weight: change in BMI ≤-5%. Gained weight: change in BMI ≥+5.
d) Chronic diseases: hypertension, diabetes, cancer, heart disease, pulmonary diseases, embolism/stroke or arthropathies. The percentages were calculated in relation to the column.
*p<0.05; **p<0.01; ***p<0.001.
Prevalence of non-communicable chronic diseases also increased during the period assessed. Figure 2 shows a proportional increase for all years, above all for diseases such as hypertension (50.9% in 2000, 65.7% in 2006 and 72.6% in 2010) and arthropathies (23.4% in 2000, 36.5% in 2006 and 36.7% in 2010) – these being the most frequent in the period assessed.
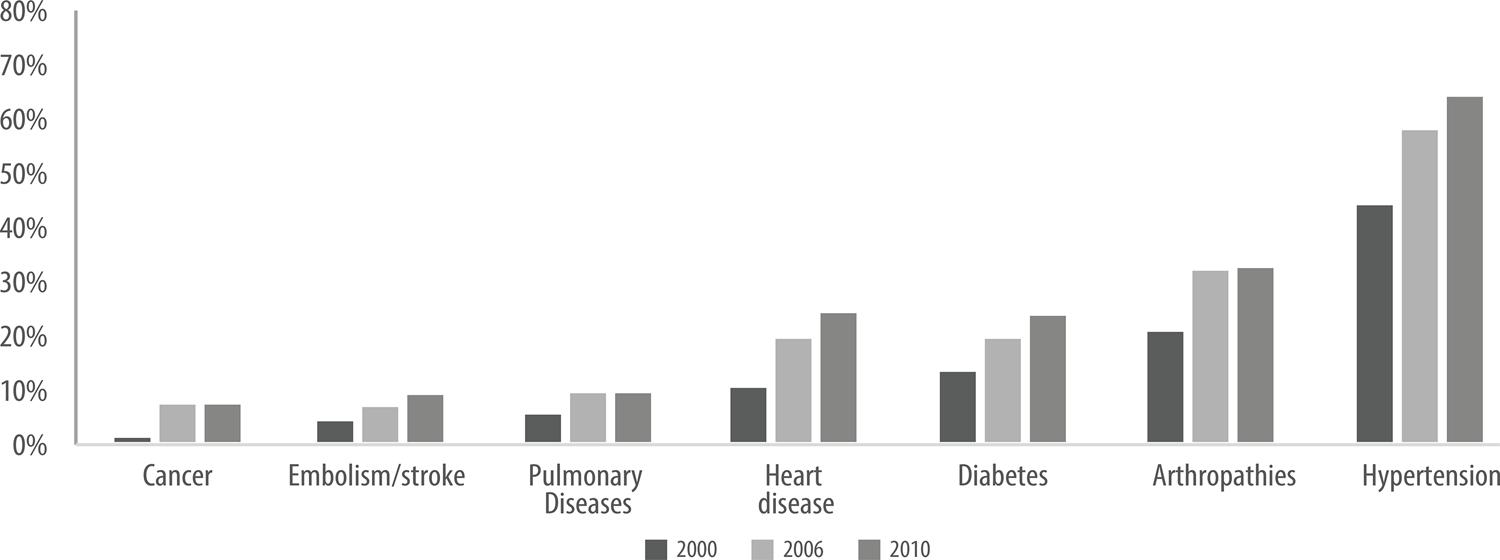
Figure 2 Prevalence of chronic diseases in elderly people, SABE Survey, São Paulo, 2000, 2006 and 2010aa) Total sample: 571. Number (n) of participants per disease in 2000, 2006 and 2010, respectively: Cancer: 9, 22 and 47; embolism/stroke: 25, 42 and 59; pulmonary diseases: 39, 57 and 61; heart disease: 71, 129 and 162; diabetes: 87, 126 and 152; arthropathies: 133, 215 and 210; hypertension: 288, 381 and 414.
In the multiple models, having been hospitalized one or more times in the last year (RR:3.50; 95%CI 1.40;8.72) or having one or more chronic diseases (RR:2.12; 95%CI 1.00;4.46) contributed to weight loss in 2010 (Table 2). On the other hand, poor or very poor self-rated health was a predictor of increased weight in the second wave of the study in 2006 (RR: 3.15; 95%CI 1.21;8.17), and in the third wave in 2010 (RR: 2.46; 95%CI 1.02;5.94), regardless of sex, age, schooling or marital status (Table 3).
Table 2 – Multiple model of association between health conditions and decrease in body weight among elderly people, SABE Survey, São Paulo, 2000, 2006 and 2010ª
| 2000-2006c | 2006-2010d | |||
|---|---|---|---|---|
|
|
|
|||
| RR (95%CI) | p-valueb | RR (95%CI) | p-valueb | |
| Age (continuous) | 1.00 (0.97;1.04) | 0.773 | 1.04 (0.99;1.10) | 0.153 |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 1.04 (0.63;1.73) | 0.871 | 0.53 (0.24;1.16) | 0.110 |
| Schooling | ||||
| Illiterate | 1 | 1 | ||
| 1-3 years | 0.93 (0.48;1.81) | 0.840 | 0.60 (0.22;1.64) | 0.318 |
| ≥ 4 years | 1.04 (0.56;1.91) | 0.907 | 1.14 (0.48;2.71) | 0.758 |
| Marital status | ||||
| Married | 1 | 1 | ||
| Not married | 1.24 (0.77;2.00) | 0.382 | 0.99 (0.47;2.12) | 0.988 |
| Number of diseases | ||||
| None or 1 | 1 | 1 | ||
| ≥ 2 diseases | 0.95 (0.61;1.48) | 0.828 | 2.12 (1.00;4.46) | 0.048* |
| Hospitalizations | ||||
| No | 1 | 1 | ||
| Yes | 1.41 (0.69;2.90) | 0.348 | 3.50 (1.40;8.72) | 0.007** |
| Self-rated health | ||||
| Very good, good | 1 | 1 | ||
| Regular | 1.07 (0.68;1.68) | 0.779 | 0.86 (0.42;1.75) | 0.674 |
| Poor, very poor | 0.95 (0.38;2.36) | 0.905 | 2.54 (0.95;6.80) | 0.064 |
a) Multinomial logistic regression.
b) Wald test.
c) 2000-2006: 2006 BMI reduced ≤-5% compared to BMI in 2000.
d) 2006-2010: 2010 BMI reduced ≤-5% compared to BMI in 2006.
*p<0.05; **p<0.01; ***p<0.001
RR = relative risk; 95%CI: 95% confidence interval.
Table 3 – Multiple model of association between health conditions and increase in body weight among elderly people, SABE Survey, São Paulo, 2000, 2006 and 2010ª
| 2000-2006c | 2006-2010d | |||
|---|---|---|---|---|
|
|
|
|||
| RR (95%CI) | p-valueb | RR (95%CI) | p-valueb | |
| Age (continuous) | 0.98 (0.94;1.03) | 0.483 | 0.95 (0.91;0.99) | 0.014* |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 0.98 (0.51;191) | 0.954 | 0.72 (0.41;1.26) | 0.248 |
| Schooling | ||||
| Illiterate | 1 | 1 | ||
| 1-3 years | 1.38 (0.58;3.30) | 0.467 | 2.18 (1.08;4.41) | 0.031* |
| ≥ 4 years | 1.25 (0.55;2.84) | 0.593 | 1.19 (0.61;2.35) | 0.606 |
| Marital status | ||||
| Married | 1 | 1 | ||
| Not married | 1.15 (0.61;2.16) | 0.663 | 1.29 (0.75;2.22) | 0.349 |
| Number of diseases | ||||
| None or 1 | 1 | 1 | ||
| ≥ 2 diseases | 1.31 (0-73;2.33) | 0.368 | 0.84 (0.52;1.36) | 0.475 |
| Hospitalizations | ||||
| No | 1 | 1 | ||
| Yes | 0,72 (0,26;2,01) | 0.536 | 1.68 (0.82;3.43) | 0.155 |
| Self-rated health | ||||
| Very good, good | 1 | 1 | ||
| Regular | 1.40 (0.77;2.54) | 0.271 | 1.29 (0.79;2.11) | 0.315 |
| Poor, very poor | 3.15 (1.21;8.17) | 0.018* | 2.46 (1.05;5.94) | 0.046* |
a) Multinomial logistic regression.
b) Wald test.
c) 2000-2006: 2006 BMI increased ≤-5% compared to BMI in 2000.
d) 2006-2010: 2010 BMI increased ≤-5% compared to BMI in 2006.
*p<0.05; **p<0.01; ***p<0.001
RR: relative risk; 95%CI: 95% confidence interval.
Discussion
Over the ten years assessed, there was an increase in the proportion of chronic diseases, weight gain and obesity, although in the first period assessed (2000-2006), weight loss was more prevalent. Poor or very poor self-rated health was associated with increase in body weight in both the periods assessed (2006, RR:3.15; p:0.018), (2010, RR:2.46; p:0.046). In turn, hospitalizations (2010, RR:3.50; p:0.007) and greater number of chronic diseases were associated with reduction in body weight.
Reduction in physical activity due to physical limitations or psychosocial aspects(11) is associated with reduced energy expenditure in old age. Living in a large metropolis(12) like São Paulo is also an important factor for people who are more elderly getting out and about less. Moreover, the sample was essentially female (63.5% were women) and, due to generational and structural issues, this population is more subject to being restricted to the household.(13) It is postulated that people susceptible to the negative effects of obesity die earlier,(14) and as this is a sample comprised of survivors, this would also explain the heavier body weight of those who were assessed.
Moreover, obesogenic environments, which have been influencing weight gain in all age ranges, may have contributed to the increase in weight and obesity(5) found in the second wave, contrasting studies that demonstrate weight reduction among elderly people(15) and the results found in the first wave of the study.
Reductions in mobility and prevalence of comorbidities generally associated with weight gain(17), such as cardiovascular diseases, as well as stigmatizing factors of obesity, can favor individuals having a negative perception of their own health. Moreover, given that self-rated health is an important predictor of morbidity and mortality,(18) it is possible that those who reported poorer health are perceiving and anticipating certain diagnoses.
The relationship between hypertension and unfavorable outcomes has been reported previously in other papers on the SABE Survey.(19) In order to reduce risks associated with chronic diseases, changes in diet, such as reducing fat and simple carbohydrates, are encouraged and can result in weight loss.(20) In the case of arthropathies, for instance, intentional weight loss of >10% provides important clinical benefits.(21)
On the other hand, physiological changes that promote catabolic and inflammatory stress and greater energy expenditure,(22) as in the case of pulmonary diseases, can result in unintentional weight loss and cause the health condition of the more elderly to worsen. Exacerbation of these diseases and need for hospital care are important predictors of anorexia in aging.(23)
Deterioration of nutritional status during hospitalization is generally related to metabolic stress, fasting, less acceptance and intake of food.(23) Frailty, increase in disease burden and mortality(15) are some of the many consequences of significant weight loss among the elderly.
Preventing weight loss and anorexia has been the main aim of nutritional care of the elderly for a long time.(24) More recent studies (conducted between 2017 and 2019) have, however, pointed to increased weight, obesity and related consequences in this population.(16) Similarly to the findings of this report, in a study that assessed elderly people in the United Kingdom in the period 1998-2015, those who put on weight also felt that their overall health had become poorer,(16) differently to a Brazilian study that did not find association between excess weight and poorer self-rated health when analyzing adults living in state capitals in the country’s Midwest region and Federal District between 2008 and 2014.(26) According to Hulman et al.,(16) stage of life interferes in self-perception of health, as the importance of conditions that contribute to self-assessment of health changes during the course of life. Among younger people, for example, greater disposition to carry out daily activities and lower prevalence of diseases appear to contribute to better self-rated health results.
Data in the literature also indicate that the number of chronic diseases is generally associated with weight gain.(27) In this study, however, this was a risk factor for weight loss, possibly due to the advanced stage of the diseases. In a study conducted with middle-aged and elderly adults in Costa Rica and England in 2015, pulmonary diseases and diabetes were also associated with weight loss.(28) Furthermore, the relationship between weight loss and hospitalization, although serious, is a common occurrence,(21) as also found in this study and in a study conducted between 2011 and 2012 with elderly people hospitalized in Southeast Brazil (São Paulo, Rio de Janeiro, Minas Gerais and Espírito Santo).(29)
The results of a study that assessed morbidity and mortality trends worldwide in 2015, also demonstrated a high burden of chronic diseases among elderly people in underdeveloped and developing countries.(30) Moreover, despite the existence of few longitudinal studies,(30) several indicators suggest that in those countries health care has not accompanied increased length of life.
The strong points of this study include the representative sample of older adults in the community at the beginning of the period assessed and, despite the losses, the ten years of accompaniment enable greater knowledge of weight changes and associated factors among elderly people. In addition, weight and height were measured (instead of being reported) by trained professionals in all periods of the study. Given that studies involving nutrition and geriatrics in general only assess nutritional status, this study moves forward by taking body weight change into consideration – this being an easy method to use in clinical practice and which can also be a better predictor of elderly people’s health.
The limitations of this study include self-reporting of health assessment, number of hospitalizations and diagnosis of diseases, since, although they are used a great deal, these measurements can be subject to recall bias, especially among the elderly. Certain precautions were taken in order to reduce these sources of errors, such as critically reviewing the interviews conducted and aid provided by respondents. Losses are common in longitudinal studies with elderly people and are also a limitation of this study. However, as lost participant data was not greatly different to that of assessed participants (except for those who died), the results of this study were not influenced by these losses. The data refer to a population of elderly survivors and should be interpreted with this is mind. Future analyses could indicate association between nutritional status and survival, in addition to other outcomes among these elderly people.
Although the progressive increases in chronic disease prevalence as age advances is not exactly an unexpected event, the increase in the proportion of elderly individuals who put on weight and in those who became obese points to new challenges for managing care of the elderly. The consequences of this new nutritional profile are still not clear, but this study has demonstrated that listening to and accompanying the self-rated health of these elderly people can contribute to earlier diagnosis. Moreover, in order to ensure healthy aging, action needs to be taken quickly, preventing obesity and risk factors related to the appearance of diseases and implementing actions for treatment and harm reduction, such as keeping weight stable.
Acknowledgement
To the principal investigator and coordinator of the SABE Survey, Maria Lucia Lebrão, in memoriam, who began and conducted the entire study until 2016.
REFERENCES
1. Rowe JW, Kahn RL. Successful aging. Gerontologist [Internet]. 1997 Aug [cited 2020 Jun 22];37(4):433-40. Available from: https://doi.org/10.1093/geront/37.4.433 [ Links ]
2. Leslie W, Hankey C. Aging, nutritional status and health. Healthcare (Basel) [Internet]. 2015 Sep [cited 2020 Jun 22];3(3):648-58. Available from: https://dx.doi.org/10.3390%2Fhealthcare3030648 [ Links ]
3. Vetrano DL, Foebel AD, Marengoni A, Brandi V, Collamati A, Heckman GA, et al. Chronic diseases and geriatric syndromes: the different weight of comorbidity. Eur J Intern Med [Internet]. 2016 Jan [cited 2020 Jun 22];27:62-7. Available from: https://doi.org/10.1016/j.ejim.2015.10.025 [ Links ]
4. Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O'Donnell M, Sullivan R, et al. The burden of disease in older people and implications for health policy and practice. Lancet [Internet]. 2015 Nov [cited 2020 Jun 22];385(9967):549-62. Available from: https://doi.org/10.1016/S0140-6736(14)61347-7 [ Links ]
5. Silva VSD, Souza I, Silva DAS, Barbosa AR, Fonseca M. Trends and association of BMI between sociodemographic and living conditions variables in the Brazilian elderly: 2002/03-2008/09. Ciên Saúde Coletiva [Internet]. 2018 Mar [cited 2020 Jun 22];23(3):891-901. Available from: https://doi.org/10.1590/1413-81232018233.12532016 [ Links ]
6. So ES. The impacts of weight change and weight change intention on health-related quality of life in the Korean elderly. J Aging Health [Internet]. 2019 Aug [cited 2020 Jun 22];31(7):1106-20. Available from: https://doi.org/10.1177/0898264318761908 [ Links ]
7. Zhang Y, Hou F, Li J, Yu H, Li L, Hu S, et al. The association between weight fluctuation and all-cause mortality: a systematic review and meta-analysis. Medicine (Baltimore) [Internet]. 2019 Oct [cited 2020 Jun 22];98(42):e17513. Available from: https://doi.org/10.1097/md.0000000000017513 [ Links ]
8. Organización Panamericana de la Salud. Salud, bienestar y envejecimiento (SABE) en América Latina y el Caribe: informe preliminar Washington (D.C.): Organización Panamericana de la Salud; 2001 [cited 2020 Jun 22]. Available from: http://envejecimiento.csic.es/documentos/documentos/paho-salud-01.pdf [ Links ]
9. Lebrão ML, Laurenti R. Saúde, bem-estar e envelhecimento: o estudo SABE no Município de São Paulo. Rev Bras Epidemiol [Internet]. 2005 jun [citado 2020 jun 22];8(2):127-41. Disponível em: https://doi.org/10.1590/S1415-790X2005000200005 [ Links ]
10. Frisancho AR. New standards of weight and body composition by frame size and height for assessment of nutritional status of adults and the elderly. Am J Clin Nutr [Internet]. 1984 Oct [cited 2020 Jun 22];40(4):808-19. Available from: https://doi.org/10.1093/ajcn/40.4.808 [ Links ]
11. Jesus-Moraleida FR, Ferreira PH, Silva JP, Andrade AGP, Dias RC, Dias JMD, et al. Relationship between physical activity, depressive symptoms and low back pain related disability in older adults with low back pain: a cross-sectional mediation analysis. J Aging Phys Act [Internet]. 2020 Apr [cited 2020 Jun 22];1-6. Available from: https://doi.org/10.1123/japa.2019-0077 [ Links ]
12. Ramachandran M, D'Souza SA. A cross-sectional survey on older adults' community mobility in an Indian metropolis. J Cross Cult Gerontol [Internet]. 2016 Feb [cited 2020 Jun 22];31(1):19-33. Available from: https://doi.org/10.1007/s10823-015-9276-7 [ Links ]
13. Ko H, Park YH, Cho B, Lim KC, Chang SJ, Yi YM, et al. Gender differences in health status, quality of life, and community service needs of older adults living alone. Arch Gerontol Geriatr [Internet]. 2019 Jul-Aug [cited 2020 Jun 22];83:239-45. Available from: https://doi.org/10.1016/j.archger.2019.05.009 [ Links ]
14. Cetin DC, Nasr G. Obesity in the elderly: more complicated than you think. Cleve Clin J Med [Internet]. 2014 Jan [cited 2020 Jun 22];81(1):51-61. Available from: https://doi.org/10.3949/ccjm.81a.12165 [ Links ]
15. Cereda E, Klersy C, Pedrolli C, Cameletti B, Bonardi C, Quarleri L, et al. The Geriatric Nutritional Risk Index predicts hospital length of stay and in-hospital weight loss in elderly patients. Clin Nutr [Internet]. 2015 Feb [cited 2020 Jun 22];34(1):74-8. Available from: https://doi.org/10.1016/j.clnu.2014.01.017 [ Links ]
16. Fernandez-Barres S, Garcia-Barco M, Basora J, Martinez T, Pedret R, Arija V, Project ATDOM-NUT group. The efficacy of a nutrition education intervention to prevent risk of malnutrition for dependent elderly patients receiving Home Care: a randomized controlled trial. Int J Nurs Stud [Internet]. 2017 May [cited 2020 Jun 22];70:131-41. Available from: https://doi.org/10.1016/j.ijnurstu.2017.02.020 [ Links ]
17. Dent E, Hoogendijk EO, Wright ORL. New insights into the anorexia of ageing: from prevention to treatment. Curr Opin Clin Nutr Metab Care [Internet]. 2019 Jan [cited 2020 Jun 22];22(1):44-51. Available from: https://doi.org/10.1097/mco.0000000000000525 [ Links ]
18. Lartey ST, Magnussen CG, Si L, Boateng GO, de Graaff B, Biritwum RB, et al. Rapidly increasing prevalence of overweight and obesity in older Ghanaian adults from 2007-2015: Evidence from WHO-SAGE Waves 1 & 2. PLoS One [Internet]. 2019 Aug [cited 2020 Jun 22];14(8):e0215045. Available from: https://doi.org/10.1371/journal.pone.0215045 [ Links ]
19. Jerkovic OS, Sauliune S, ¦umskas L, Birt CA, Kersnik J. Determinants of self-rated health in elderly populations in urban areas in Slovenia, Lithuania and UK: findings of the EURO-URHIS 2 survey. Eur J Public Health [Internet]. 2017 May [cited 2020 Jun 22];27(suppl 2):74-9. Available from: https://doi.org/10.1093/eurpub/ckv097 [ Links ]
20. Hulman A, Ibsen DB, Laursen ASD, Dahm CC. Body mass index trajectories preceding first report of poor self-rated health: A longitudinal case-control analysis of the English Longitudinal Study of Ageing. PLoS One [Internet]. 2019 Feb [cited 2020 Jun 22];14(2):e0212862. Available from: https://doi.org/10.1371/journal.pone.0212862 [ Links ]
21. Oliveira IM, Duarte YAO, Zanetta DMT. Prevalence of systemic arterial hypertension diagnosed, undiagnosed, and uncontrolled in elderly population: SABE study. J Aging Res [Internet]. 2019 Sep [cited 2020 Jun 22]:3671869. Available from: https://doi.org/10.1155/2019/3671869 [ Links ]
22. Bruins MJ, Van Dael P, Eggersdorfer M. The role of nutrients in reducing the risk for noncommunicable diseases during aging. Nutrients [Internet]. 2019 Jan [cited 2020 Jun 22];11(1):85. Available from: https://doi.org/10.3390/nu11010085 [ Links ]
23. Messier SP, Resnik AE, Beavers DP, Mihalko SL, Miller GD, Nicklas BJ, et al. Intentional weight loss in overweight and obese patients with knee osteoarthritis: is more better? Arthritis Care Res (Hoboken) [Internet]. 2018 Nov [cited 2020 Jun 22];70(11):1569-75. Available from: https://doi.org/10.1002/acr.23608 [ Links ]
24. Rinninella E, Cintoni M, De Lorenzo A, Anselmi G, Gagliardi L, Addolorato G, et al. May nutritional status worsen during hospital stay? A sub-group analysis from a cross-sectional study. Intern Emerg Med [Internet]. 2019 Jan [cited 2020 Jun 22];14(1):51-7. Available from: https://doi.org/10.1007/s11739-018-1944-5 [ Links ]
25. 2Landi F, Picca A, Calvani R, Marzetti E. Anorexia of aging: assessment and management. Clin Geriatr Med [Internet]. 2017 Aug [cited 2020 Jun 22];33(3):315-23. Available from: https://doi.org/10.1016/j.cger.2017.02.004 [ Links ]
26. 2Souza L, Brunken GS, Segri NJ, Malta DC. Trends of self-rated health in relation to overweight in the adult population in Brazilian Midwest capitals. Rev Bras Epidemiol [Internet]. 2017 Jun [cited 2020 Jun 22];20(2):299-309. Available from: https://doi.org/10.1590/1980-5497201700020010 [ Links ]
27. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 Countries over 25 years. N Engl J Med [Internet]. 2017 Jul [cited 2020 Jun 22];377(1):13-27. Available from: https://doi.org/10.1056/nejmoa1614362 [ Links ]
28. Blue L, Goldman N, Rosero-Bixby L. Disease and weight loss: a prospective study of middle-aged and older adults in Costa Rica and England. Salud Pública Mex [Internet]. 2015 Jul-Aug [cited 2020 Jun 22];57(4):312-9. Available from: https://doi.org/10.21149/spm.v57i4.7574 [ Links ]
29. Cordeiro P, Martins M. Hospital mortality in older patients in the Brazilian Unified Health System, Southeast region. Rev Saúde Pública [Internet]. 2018 Jul [cited 2020 Jun 22];52:69. Available from: https://doi.org/10.11606/s1518-8787.2018052000146 [ Links ]
30. Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults--present status and future implications. Lancet [Internet]. 2015 Nov [cited 2020 Jun 22];385(9967):563-75. Available from: https://doi.org/10.1016/S0140-6736(14)61462-8 [ Links ]
* Article derived from the Ph.D. thesis written by Tânia Aparecida de Araujo, entitled “Body weight change among the elderly between 2000 and 2010: SABE Study”, submitted to the University of São Paulo Faculty of Public Health and defended in 2019. The SABE study is funded by the São Paulo State Research Support Foundation (FAPESP), grant number 99/05125-7. This paper was produced with the support of the Coordination for the Improvement of Higher Education Personnel (CAPES), under number 1570936 – Funding code 001, Ph.D. grant - Araujo TA.
Received: April 06, 2020; Accepted: June 05, 2020











 texto em
texto em 


