Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.4 Brasília 2020 Epub 21-Sep-2020
http://dx.doi.org/10.1590/s1679-49742020000400022
Original article
Factors associated with COVID-19 hospital deaths in Espírito Santo, Brazil, 2020
1Universidade Federal do Espírito Santo, Laboratório de Epidemiologia, Vitória, ES, Brazil
2Secretaria de Estado de Economia e Planejamento do Espírito Santo, Instituto Jones dos Santos Neves, Vitória, ES, Brazil
3Universidade Federal do Espírito Santo, Departamento de Matemática, Vitória, ES, Brazil
4Universidade Federal do Espírito Santo, Departamento de Medicina Social, Vitória, ES, Brazil
5Universidade Federal do Espírito Santo, Programa de Pós-Graduação em Saúde Coletiva, Vitória, ES, Brazil
6Faculdade de Direito de Vitoria, Vitória, ES, Brazil
Objective
To analyze factors associated with the deaths of individuals hospitalized with COVID-19 in the state of Espírito Santo, Brazil.
Methods
This was a cross-sectional study using secondary data. Logistic regression models were used to estimate crude and adjusted odds ratios (OR).
Results
As at May 14, 2020, 200 individuals had been discharged and 220 had died. Of the total number of people studied, 57.1% were male, 46.4% were >60 years old, 57.9% were cases notified by a private institution, and 61.7% had >1 comorbidity. In the adjusted analysis, hospital mortality was higher for the 51-60 age group (OR=4.33 – 95%CI 1.50;12.46), the over 60 age group (OR=11.84 – 95%CI 4.31;32.54), cases notified by public institutions (OR=8.23 – 95%CI 4.84;13.99) and cases with a greater number of comorbidities (two [OR=2.74 – 95%CI 1.40;5.34] and three [OR=2.90 – 95%CI 1.07;7.81]).
Conclusion
Higher mortality was found in older individuals, those with comorbidities and users of public hospitals.
Key words: Coronavirus Infections; Hospitalization; Health Status Disparities; Cross-Sectional Studies; Epidemics
Introduction
Given the speed with which coronavirus infection spreads and its tragic consequences, the COVID-19 pandemic has affected people’s lives and exposed health system weaknesses worldwide, especially in Brazil. As at May 31st 2020, 514,849 COVID-19 cases and 29,314 COVID-19 deaths had been notified nationally, of which 13,690 cases and 604 deaths corresponded to the state of Espírito Santo.(1) The state’s first case was recorded in February 2020.
Defined by the 1988 Constitution, the Brazilian National Health System (SUS) was founded based on the principles of Social Participation, Universality, Integrality and Equity with regard to Brazilian citizens’ access to health services. These are humanistic principles, based on the values of Democratic Rule of Law. In the factual world, however, the reality faced involves Public Health underfunding, together with public resources being transferred to the private sector, which, in turn, seeks to make profit and consequently results in socioeconomic restriction/exclusion.3
In pandemic situations, countries with universal health systems should present better results, reflected in fewer people being infected and dying. However, in Canada and the United Kingdom, which have universal health systems, the pandemic has not affected the entire population in the same way, and social inequality has shown itself to be a factor more preponderant than universality. In Wales, for example, the COVID-19 mortality rate in its poorest socioeconomic areas has reached 44.6 deaths per 100,000 inhabitants, almost double the rate for the least poorest area, where the mortality rate has reached 23.2/100,000 inhab.(4)
One of the markers of inequality is the proportional distribution of people who use the so-called Supplementary Health system, which in Brazil includes private system hospital health insurance plans. The distinction between SUS users and Supplementary Health system users has been marked by social class, age and health status. According to the most recent World Health Survey (WHS), conducted in 2003 with a sample of five thousand people aged 18 or over, 24.0% of interviewers had private health insurance and this was associated with the number of durable goods and age, education level, having formal employment and reporting good self-rated health. The WHS also revealed that these individuals heave better health status and use health services more, when compared to the population with no health insurance coverage.(5)
The National Supplementary Health Agency (ANS) has monitored this form of coverage in Brazil since 2000. The data for the year 2019 show that in Espírito Santo 1,112,525 people had private health insurance.
The objective of this investigation was to analyze factors associated with deaths of individuals with COVID-19 in public and private hospitals in the state of Espírito Santo, Brazil.
Methods
A cross-sectional study was conducted with people with laboratory-confirmed SARS-CoV-2 infection which resulted in them being hospitalized in public and private hospitals in the state of Espírito Santo, whereby the hospitalization outcome was either discharge or death.
The state of Espírito Santo is located in the Southeastern region of Brazil. In 2019 it had a population of 4,018,650 inhab., with a monthly per capita household income of BRL 1,477.00 and a human development index of 0.740 (2010).(6)
Also in 2019, 1,112,525 people resident in Espírito Santo, i.e. around 27.7% of the state’s population, had private health insurance, according to population estimates produced by the Brazilian Institute of Geography and Statistics (IBGE).(8) According to data held by the Brazilian National Health Establishment Registry, in April 2020, Espírito Santo had 223 health establishments with inpatient facilities, 85 of which belonged to the Brazilian National Health System (SUS).(9)
The study included all people hospitalized with COVID-19 in the state’s public and private hospitals whose hospitalization outcome was either discharge or death as at May 14th 2020. Thirty-two hospitalized individuals were excluded from the analysis because there was no information on case outcome.
The data we used were provided by the Inter-Institutional Epidemiological Studies Center (NIEE), created with the aim of supporting government actions in response to the COVID-19 emergency.(2) Coordinated by the Jones dos Santos Neves Institute of the Espírito Santo State Economy and Planning Department, the NIEE comprises representatives of the State Health Department, the Espírito Santo Military Fire Brigade and the Federal University of Espírito Santo Laboratory of Epidemiology.
The sociodemographic variables analyzed were: sex (male; female); age (in years: up to 30; 31-40; 41-50; 51-60; over 60); race/skin color (black/brown; non-black/brown); and municipality of residence (Greater Vitória region; interior region of the state). The Greater Vitória region is comprised of 7 municipalities: Vitória (state capital), Vila Velha, Serra, Cariacica, Fundão, Guarapari and Viana. The state’s remaining 71 municipalities were grouped into the ‘interior’ category.
An assessment was made of the presence (no; yes) of diseases/health conditions possibly associated with case outcome: lung diseases; heart diseases; kidney diseases; hepatitis; diabetes mellitus; immune system diseases; human immunodeficiency virus (HIV) infection; neoplasms; tobacco use disorder; bariatric surgery; obesity; tuberculosis; and chronic neurological diseases. The ‘number of comorbidities’ variable was included, stratified between 0 and 4 or more comorbidities present in each case.
Given the study’s interest in the nature of the service where cases were hospitalized, the ‘case notifying institution’ (public; private) variable was also included. Private and charitable institutions were categorized as ‘private notifying institutions’, while emergency health centers and public hospitals were categorized as ‘public notifying institutions’.
The variable defined as the study outcome, described at the beginning of this Methods section, had two categories: hospital ‘discharge’ and COVID-19 ‘death’.
Descriptive statistical analyses expressed in percentages were performed on categorical variables, the ‘age’ variable was expressed by calculating the average value and standard deviation and possible association between the variables studied and the outcome – discharge or death – was verified using Pearson’s chi square test; Student’s t-test was used for the ‘age’ variable. Following this crude and adjusted odds ratios (OR) were calculated as were their 95% confidence intervals (95%CI) using the logistic regression model. All variables with a significance level of up to 10% were included in the model. Two adjusted models were built: model A, which included the ‘notifying institution’ variable, and model B, which did not include this variable, because it was considered to be a possible confounding variable when analyzing the ‘death’ or ‘discharge’ outcome. The study adopted a 5% significance level.
Considering the sample size, the 1:1 ratio between the ‘discharge’ or ‘death’ outcome for hospitalized people, and 20% difference in the occurrence of the outcome between the two groups and use of a 5% significance level, statistical power of 98% was calculated for the associations studied.
The data analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 20.0.
The study project was submitted to the Federal University of Espírito Santo Health Sciences Center Research Ethics Committee (CEP/CCS/UFES) and approved as per Opinion No. 3.908.434, issued on May 20th 2020. As it is a study based on secondary data, signature of a Free and Informed Consent form was not required.
Results
As at May 14th 2020, 889 people with confirmed diagnosis of COVID-19 had been admitted to hospital in Espírito Santo 889. The first hospitalization occurred on February 26th and the first death on March 20th. The data on hospitalization in the state’s public and private hospitals due to COVID-19 are shown in Figure 1. The study analyzed people whose outcomes had occurred by May 14th 2020: 200 people had been discharged from hospital and 220 had died.
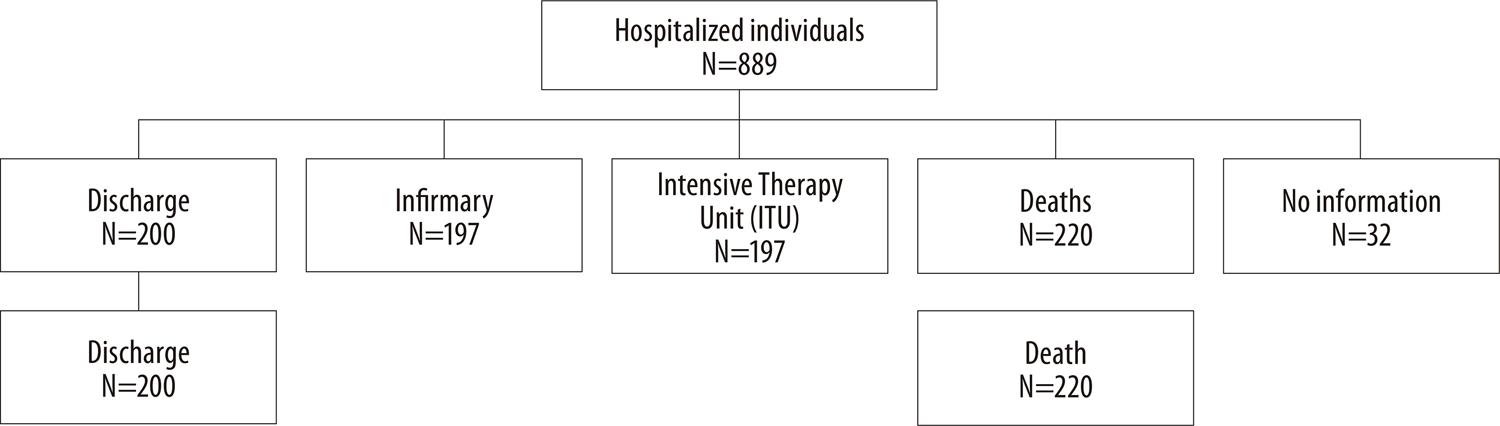
Figure 1 – Flowchart of people hospitalized due to COVID-19 and definition of ‘discharge’ and ‘death’ outcome groups, Espírito Santo, March 1st to May 14th 2020
Table 1 shows the profile of the people who were hospitalized: 57.1% were male, 46.4% were over 60 years old and 81.7% lived in the Greater Vitória region. Information on race/skin color was missing for 33.5% of those hospitalized with COVID-19, 57.9% were notified by private institutions and 61.7% had at least one comorbidity.
Table 1 – Distribution of the characteristics of people hospitalized due to COVID-19 and association with the ‘discharge’ and ‘death’ outcome groups (n=440), March 1st to May 14th 2020, Espírito Santo
| Variable | Totala | ‘Discharge’ group | ‘Death’ group | p-valueb | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| n | % | n | % | n | % | ||
| Sex | |||||||
| Female | 180 | 42.9 | 82 | 45.6 | 98 | 54.4 | 0.463 |
| Male | 240 | 57.1 | 118 | 49.2 | 122 | 50.8 | |
| Age group (years) | |||||||
| ≤30 | 40 | 9.5 | 33 | 82.5 | 7 | 17.5 | 0.001 |
| 31-40 | 44 | 10.5 | 36 | 81.8 | 8 | 18.2 | |
| 41-50 | 58 | 13.8 | 38 | 65.5 | 20 | 34.5 | |
| 51-60 | 83 | 19.8 | 42 | 50.6 | 41 | 49.4 | |
| >60 | 195 | 46.4 | 51 | 26.2 | 144 | 73.8 | |
| Race/skin color | |||||||
| Black/brown | 158 | 37.6 | 63 | 39.9 | 95 | 60.1 | 0.509 |
| Non-black/brown | 121 | 28.8 | 53 | 43.8 | 68 | 56.2 | |
| No information | 141 | 33.5 | |||||
| Municipality of residence | |||||||
| Greater Vitória region | 343 | 81.7 | 165 | 48.1 | 178 | 51.9 | 0.674 |
| Interior | 77 | 18.3 | 35 | 45.5 | 42 | 54.5 | |
| Notifying institution | |||||||
| Public | 175 | 41.7 | 35 | 20.0 | 140 | 80.0 | 0.001 |
| Private | 243 | 57.9 | 165 | 67.9 | 78 | 32.1 | |
| Lung diseases | |||||||
| Yes | 35 | 8.3 | 12 | 34.3 | 23 | 65.7 | 0.094 |
| No | 381 | 90.7 | 187 | 49.1 | 194 | 50.9 | |
| Heart diseases | |||||||
| Yes | 188 | 44.8 | 66 | 35.1 | 122 | 64.9 | 0.001 |
| No | 227 | 54.0 | 134 | 59.0 | 93 | 41.0 | |
| Kidney diseases | |||||||
| Yes | 19 | 4.5 | 3 | 15.8 | 16 | 84.2 | 0.004 |
| No | 396 | 94.3 | 196 | 49.5 | 200 | 50.5 | |
| Hepatitis | |||||||
| Yes | 7 | 1.7 | – | 0.0 | 7 | 100.0 | 0.011 |
| No | 408 | 97.1 | 198 | 48.5 | 210 | 51.5 | |
| Diabetes mellitus | |||||||
| Yes | 101 | 24.0 | 33 | 32.7 | 68 | 67.3 | 0.001 |
| No | 314 | 74.8 | 166 | 52.9 | 148 | 47.1 | |
| Immune system diseases | |||||||
| Yes | 14 | 3.3 | 2 | 14.3 | 12 | 85.7 | 0.010 |
| No | 401 | 95.5 | 197 | 49.1 | 204 | 50.9 | |
| HIVc | |||||||
| Yes | 4 | 1.0 | – | 0.0 | 4 | 100.0 | 0.054 |
| No | 411 | 97.9 | 199 | 48.4 | 212 | 51.6 | |
| Neoplasms | |||||||
| Yes | 15 | 3.6 | 2 | 13.3 | 13 | 86.7 | 0.006 |
| No | 401 | 95.5 | 197 | 49.1 | 204 | 50.9 | |
| Tobacco use disorder | |||||||
| Yes | 28 | 6.7 | 8 | 28.6 | 20 | 71.4 | 0.032 |
| No | 386 | 91.9 | 191 | 49.5 | 195 | 50.5 | |
| Bariatric surgery | |||||||
| Yes | 2 | 0.5 | 1 | 50.0 | 1 | 50.0 | 0.945 |
| No | 408 | 97.1 | 194 | 47.5 | 214 | 52.5 | |
| Obesity | |||||||
| Yes | 36 | 8.6 | 12 | 33.3 | 24 | 66.7 | 0.073 |
| No | 374 | 89.0 | 183 | 48.9 | 191 | 51.1 | |
| Tuberculosis | |||||||
| Yes | 1 | 0.2 | 1 | 100.0 | – | – | 0.296 |
| No | 415 | 98.8 | 198 | 47.7 | 217 | 52.3 | |
| Chronic neurological diseases | |||||||
| Yes | 18 | 4.3 | 2 | 11.1 | 16 | 88.9 | 0.001 |
| No | 398 | 94.8 | 197 | 49.5 | 201 | 50.5 | |
| Number of comorbidities | |||||||
| 0 | 161 | 38.3 | 108 | 67.1 | 53 | 32.9 | 0.001 |
| 1 | 111 | 26.4 | 54 | 48.6 | 57 | 51.4 | |
| 2 | 93 | 22.1 | 27 | 29.0 | 66 | 71.0 | |
| 3 | 39 | 9.3 | 8 | 20.5 | 31 | 79.5 | |
| ≥4 | 16 | 3.9 | 3 | 18.8 | 13 | 81.2 | |
a) The total may not be equal to 100% due to missing data
b) Pearson’s chi-square test p-value.
c) HIV: human immunodeficiency virus).
Factors associated with death were found to be (i) older age group, (ii) being notified by a public institution, (iii) number of comorbidities and (iv) existence of some specific diseases/health conditions (heart, kidney, hepatitis, diabetes mellitus, immune system, HIV infection, neoplasms, tobacco use disorder, chronic neurological diseases).
Average age of those who were discharged was 47.4 years (SD=18.8), while average age of those who died was 66.5 years (SD=17.2) (Student’s t-test; p=0.001). There were more elderly people in the ‘death’ group (Figure 2).
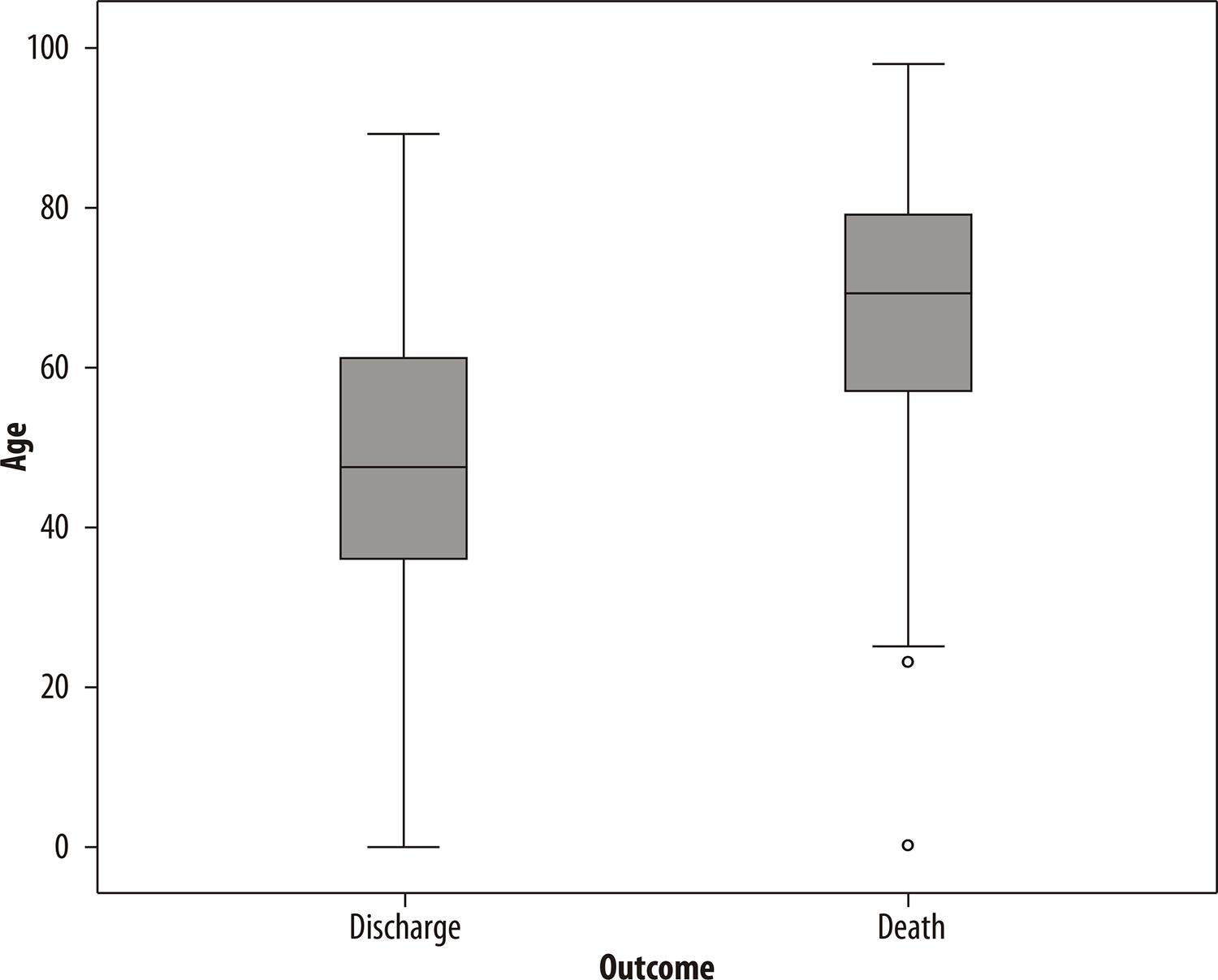
Figure 2 – Box-plot graph of the ‘age’ variable of people hospitalized due to COVID-19, by ‘discharge’ and ‘death’ outcome groups (N=420), Espírito Santo, March 1st to May 14th 2020
Table 2 shows statistically significant association between notifying institution, age group and diverse comorbidities: individuals notified by public institutions were older (over 60 years old) and had more comorbidities.
Table 2 – Distribution of the characteristics of people hospitalized due to COVID-19 and association with institution notifying cases with ‘discharge’ and ‘death’ outcomes (N=420), March 1st to May 14th 2020, Espírito Santo
| Variable | Notifying institution | ||||
|---|---|---|---|---|---|
|
| |||||
| Public | Private | p-valuea | |||
|
| |||||
| n | % | n | % | ||
| Sex | |||||
| Female | 72 | 41.1 | 106 | 43.6 | 0.613 |
| Male | 103 | 58.9 | 137 | 56.4 | @ |
| Age group (years) | |||||
| ≤30 | 13 | 7.4 | 27 | 11.1 | 0.001 |
| 31-40 | 7 | 4.0 | 37 | 15.2 | |
| 41-50 | 20 | 11.4 | 37 | 15.2 | |
| 51-60 | 36 | 20.6 | 47 | 19.3 | |
| >60 | 99 | 56.6 | 95 | 39.1 | |
| Race/skin color | |||||
| Black/brown | 90 | 60.4 | 67 | 52.3 | 0.177 |
| Non-black/brown | 59 | 39.6 | 61 | 47.7 | |
| Municipality of residence | |||||
| Greater Vitória region | 143 | 81.7 | 199 | 81.9 | 0.963 |
| Interior | 32 | 18.3 | 44 | 18.1 | |
| Lung diseases | 21 | 12.1 | 14 | 5.8 | 0.024 |
| Heart diseases | 96 | 55.5 | 90 | 37.5 | 0.001 |
| Kidney diseases | 13 | 7.5 | 6 | 2.5 | 0.017 |
| Hepatitis | 7 | 4.0 | – | 0.0 | 0.002 |
| Diabetes mellitus | 55 | 31.8 | 44 | 18.3 | 0.002 |
| Immune system diseases | 10 | 5.7 | 3 | 1.3 | 0.010 |
| HIVb | 3 | 1.7 | 1 | 0.4 | 0.177 |
| Neoplasms | 4 | 2.3 | 11 | 4.6 | 0.220 |
| Tobacco use disorder | 21 | 12.2 | 7 | 2.9 | 0.001 |
| Bariatric surgery | 1 | 0.6 | 1 | 0.4 | 0.833 |
| Obesity | 15 | 8.6 | 20 | 8.5 | 0.979 |
| Tuberculosis | 1 | 0.6 | – | 0.0 | 0.240 |
| Chronic neurological diseases | 3 | 1.7 | 15 | 6.3 | 0.026 |
| Number of comorbidities | |||||
| 0 | 53 | 30.3 | 108 | 44.4 | 0.001 |
| 1 | 39 | 22.3 | 72 | 29.6 | |
| 2 | 47 | 26.9 | 46 | 18.9 | |
| 3 | 26 | 14.9 | 11 | 4.5 | |
| ≥4 | 10 | 5.7 | 6 | 2.5 | |
a) Pearson’s chi-square test p-value.
b) HIV: human immunodeficiency virus).
Crude and adjusted odds ratios (OR) were calculated using logistic regression, considering inclusion (model A) or non-inclusion (model B) of the ‘notifying institution’ variable. The results of these calculations are shown in Table 3.
Table 3 – Association of discharge and death groups and characteristics of people hospitalized due to COVID-19, with ‘discharge’ and ‘death’ outcomes (N=420), Espírito Santo, March 1st to May 14th 2020
| Variable | Crude odds ratio | Model A Adjusted odds ratioª | Model B Adjusted odds ratiob | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| OR | 95%CIc | OR | 95%CIc | OR | 95%CIc | |||
| Age group (years) | ||||||||
| ≤30 | 1.00 | 1.00 | 1.00 | |||||
| 31-40 | 1.05 | 0.34;3.21 | 1.87 | 0.53;6.55 | 1.14 | 0.36;3.62 | ||
| 41-50 | 2.48 | 0.93;6.60 | 2.43 | 0.79;7.47 | 2.20 | 0.79;6.08 | ||
| 51-60 | 4.60 | 1.83;11.57 | 4.33 | 1.50;12.46 | 3.90 | 1.49;10.18 | ||
| >60 | 13.31 | 5.54;31.96 | 11.84 | 4.31;32.54 | 9.67 | 3.87;24.16 | ||
| Notifying institution | ||||||||
| Public | 8.46 | 5.35;13.38 | 8.23 | 4.84;13.99 | ||||
| Private | 1.00 | 1.00 | ||||||
| Heart diseases | 2.66 | 1.79;3.97 | ||||||
| Kidney diseases | 5.23 | 1.50;18.22 | ||||||
| Diabetes mellitus | 2.31 | 1.44;3.70 | ||||||
| Immune system diseases | 5.79 | 1.28;26.22 | ||||||
| Neoplasms | 6.28 | 1.40;28.17 | ||||||
| Tobacco use disorder | 2.45 | 1.05;5.69 | ||||||
| Chronic neurological diseases | 7.84 | 1.78;34.55 | ||||||
| Number of comorbidities | ||||||||
| 0 | 1.00 | 1.00 | ||||||
| 1 | 2.15 | 1.31;3.53 | 1.70 | 0.92;3.16 | 1.42 | 0.82;2.46 | ||
| 2 | 4.98 | 2.86;8.68 | 2.74 | 1.40;5.34 | 2.85 | 1.55;5.22 | ||
| 3 | 7.90 | 3.40;18.36 | 2.90 | 1.07;7.81 | 4.87 | 1.97;12.03 | ||
| ≥4 | 10.19 | 2.16;48.17 | 4.13 | 0.88;19.39 | 4.71 | 1.19;18.63 | ||
a) All variables with p>0.10 included.
b) ‘Notifying institution’ variable not included.
c) 95%CI: 95% confidence interval.
In model A, which included the ‘notifying institution’ variable, association was found between the 51-60 age group (OR=4.33 – 95%CI 1.50;12.46), the over 60 age group (OR=11.84 – 95%CI 4.31;32.54), notification by a public institution (OR=8.23 – 95%CI 4.84;13.99) and number of comorbidities (two [OR=2.74 – 95%CI 1.40;5.34] and three [OR=2.90 – 95%CI 1.07;7.81]). In model B, which did not include the ‘notifying institution’ variable, risk between age groups decreased, while significant association remained with the 51-60 age group (OR=3.90 – 95%CI 1.49;10.18) and the >60 age group (OR=9.67 – 95%CI 3.87;24.16). As for the number of comorbidities, risk increased when there were two (OR=2.85 – 95%CI 1.55;5.22;), three (OR=4.87 – 95%CI 1.97;12.03) and four or more comorbidities (OR=4.71 – 95%CI 1.19;18.63), suggesting a change in effect (in model A) because of the inclusion of this intermediate variable.
Discussion
In Espírito Santo, people hospitalized with COVID-19 and whose hospitalization outcome had been defined as at May 14th 2020, were for the most part male, over 50 years old, resident in the Greater Vitória region, hospitalized in private institutions and had at least one associated disease/health condition. On the other hand, deaths were more frequent in public institutions.
This study has limitations inherent to the use of secondary data, which are dependent on the quality of the records made by the notifying institutions. There may also be some degree of residual confounding, arising from limited or missing data/variables: e.g. inexistence of records on ‘time elapsed until health service accessed’. Notwithstanding, it is important to highlight that all hospitalized COVID-19 cases in the period considered were included, and that the study outcome, death or discharge, is robust and very unlikely to have classification errors.
Adjusted logistic regression model A revealed that people admitted to public hospitals were over 8 times more at risk of dying, when compared to those admitted to private hospitals. With regard to model B, which did not include the ‘notifying institution’ variable, it can be seen that there was indeed increased association between comorbidities and death, as also reported by other studies.(10)
It can be seen that it was not the fact of being hospitalized in a public or private institution that determined the ‘death’ outcome but rather health status prior to being admitted to hospital, including comorbidities associated with COVID-19, such as tobacco use disorder, diabetes mellitus, hypertension and obesity, among others.(12) Tobacco use disorder, for instance, as a behavior recognized as being more prevalent among the low-income Brazilian population,(14)was found to be more prevalent in individuals notified by public institutions. It is possible that tobacco use disorder may contribute to worse COVID-19 progression, given that besides harm to the lungs the habit of smoking is associated with cardiovascular disease, including predisposition to thrombosis.(15)
Likewise, a higher number of comorbidities and greater average age was found in cases cared for by public institutions who died. If it is reasonable to assume that presence of a higher number of comorbidities among people whose average age is older, it must also be questioned whether individuals using public services did in fact arrive there in a worse state of health, and whether comorbidity prevention and control in public institutions are less adequate. From this point of view, the conclusion is reached that the SUS, with its far-reaching Primary Health Care network, has a fundamental role to play in the prevention and control of these diseases.(16)
In December 2019, some 156 million Brazilians (nothing less than 75% of the country’s population of 208 million) depended on the Primary Health Care network. In the country’s Northeastern region, this coverage accounted for 48 million (85%) of the region’s 57 million inhabitants.(18)These data, in themselves, corroborate the magnitude of the poor Brazilian population, considering that the middle and upper classes either have health insurance or pay directly for private health services. It is however important to recognize that all Brazilians use the SUS to some extent, some exclusively, others to complement their private health insurance.(19)
In view of these data and the results of this study, it is important to highlight the impact of health inequalities on more vulnerable people, who have greater difficulty in perceiving the importance of self-care, access to health services and access to higher complexity levels of SUS services as their right.
Moreover, the comorbidities revealed by the COVID-19 deaths deepen even more the huge divide between rich and poor and realizing health as a right of all people. Socioeconomic inequalities generate profound impacts on social structure. The state of Espírito Santo, when it was at the peak of its urbanization process, in the period covering the late 1970s and the early 1980s, suffered from the absence of social policies and adequate territorial/urban planning. According to Lira & Monteiro,(20) these would be some of the possible determining factors of the serious socioeconomic problems found, especially within cities: irregular land use, increased unemployment and inefficiency of the basic health and education services provided to a rapidly growing urban population in that period. The urbanization process in Espírito Santo indicates that some of its nuances favor the concatenation of processes and factors that worsen territorial inequality, urban degradation and quality of life and health in the city.
In Brazil, access to a quality, comprehensive and equitable Public Health service is constitutionally recognized and guaranteed as a Universal Right. Notwithstanding, other conditions such as funding cuts of BRL 1.7 billion between 2014 and 2015, made worse by Constitutional Amendment No. 95, published in 2016, which established, among other measures, an upper limit for public expenditure on health, imply evident restrictions to the SUS being able to carry out its regular activities,(21) hampering even more an adequate response to the pandemic, especially when the health system is required by Public Opinion to act as a protagonist, as the only system effectively committed to the constitutional guarantee of the Right to Health. Within an iniquitous social context and phenomenon such as this, the existence of the SUS is a determining factor to the extent that, by minimizing health risks, it can avoid a proportionally greater impact and, in an extreme situation, the extinction of groups that are socially more vulnerable. At this time of the health emergency caused by COVID-19, the SUS should be the object of reflection by society in defense of its realignment with the spirit and the reasons why it was created through the 1988 Constitution as one of the leading flagships of the New Democratic Republic.
The pandemic emphasizes the need to create legal mechanisms, for full funding of the National Health System, so that the Brazilian Nation is better prepared for the next health crisis situations, foreseeable in an increasingly globalized world. Undoubtedly it is just a matter of time.
REFERENCES
1. Ministério da Saúde (BR). Painel coronavírus [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 mai0 31]. Disponível em: https://covid.saude.gov.br/ [ Links ]
2. Governo do Estado do Espírito Santo. Instituto Jones dos Santos Neves. Núcleo interinstitucional de estudos epidemiológicos [Internet]. Vitória: Instituto Jones dos Santos Neves; 2020 [citado 2020 jul 3]. Disponível em: http://www.ijsn.es.gov.br/observatorio-covid-19/nucleo-interinstitucional-de-estudos-epidemiologicos [ Links ]
3. Luzuriaga MJ. Privados de la salud: las políticas de privatización de los sistemas de salud en Argentina, Brasil, Chile y Colombia. São Paulo: Hucitec; 2018. p. 121-173 [ Links ]
4. Office for National Statistics. Deaths involving COVID-19 by local area and socioeconomic deprivation: deaths occurring between 1 March and 17 April 2 [Internet]. London: Office for National Statistics; 2020 [cited 2020 May 28]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand17april [ Links ]
5. Viacava F, Souza-Júnior PR, Szwarcwald CL. Coverage of the Brazilian population 18 years and older by private health plans: an analysis of data from the World Health Survey. Cad Saúde Pública [Internet]. 2005 [cited 2020 Jul 27];21:S119-28. Available from: https://doi.org/10.1590/S0102-311X2005000700013 [ Links ]
6. Agência Nacional de Saúde Suplementar - ANS (BR). ANS Tabnet [Internet]. Rio de Janeiro: Agência Nacional de Saúde Suplementar; 2020 [citado 2020 jul 8]. Disponível em: http://www.ans.gov.br/anstabnet/index.htm [ Links ]
7. Instituto Brasileiro de Geografia e Estatística - IBGE. Cidades e estados: Espírito Santo [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2020 [citado 2020 maio 31]. Disponível em: https://www.ibge.gov.br/cidades-e-estados/es/ [ Links ]
8. Agência Nacional de Saúde Suplementar - ANS (BR). ANS Tabnet: informações em saúde suplementar [Internet]. Rio de Janeiro: Agência Nacional de Saúde Suplementar; 2020 [citado 2020 maio 28]. Disponível em: http://www.ans.gov.br/anstabnet/index.htm [ Links ]
9. Ministério da Saúde (BR). CNES: estabelecimentos com tipo de atendimento prestado - internação - Espírito Santo [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 maio 31]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?cnes/cnv/atintes.def [ Links ]
10. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med [Internet]. 2020 May [cited 2020 Jul 27];46(5):846-8. Available from: https://doi.org/10.1007/s00134-020-05991-x [ Links ]
11. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 Novel Corononavirus infected pneumonia in Wuhan, China. JAMA [Internet]. 2020 Feb [cited 2020 Jul 27];323(11):1061-9. Available from: https://dx.doi.org/10.1001%2Fjama.2020.1585 [ Links ]
12. Alkundi A, Mahmoud I, Musa A, Naveed S, Alshawwaf M. Clinical characteristics and outcomes of COVID-19 hospitalized patients with diabetes in the United Kingdom: a retrospective single centre study. Diabetes Res Clin Pract [Internet]. 2020 Jul [cited 2020 Jul 27];165:108263. Available from: https://dx.doi.org/10.1016%2Fj.diabres.2020.108263 [ Links ]
13. Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in Metropolitan Detroit. JAMA Netw Open [Internet]. 2020 Jun [cited 2020 Jul 27];3(6):e2012270. Available from: https://dx.doi.org/10.1001%2Fjamanetworkopen.2020.12270 [ Links ]
14. Bazotti A, Finokiet M, Conti IL, França MT, Waquil PD. Tabagismo e pobreza no Brasil: uma análise do perfil da população tabagista a partir da POF 2008-2009. Ciênc Saúde Coletiva [Internet]. 2016 jan [citado 2020 jul 27];21(1):45-52. Disponível em: https://doi.org/10.1590/1413-81232015211.16802014 [ Links ]
15. Enga KF, Brækkan SK, Hansen-Krone IJ, le Cessie S, Rosendaal FR, Hansen J-B. Cigarette smoking and the risk of venous thromboembolism: the Tromsø Study. J Thromb Haemost [Internet]. 2012 Oct [cited 2020 May 28];10(10):2068-74. Available from: https://doi.org/10.1111/j.1538-7836.2012.04880.x [ Links ]
16. Sarti TD, Lazarini WS, Fontenelle LF, Almeida APSC. Qual o papel da Atenção Primária à Saúde diante da pandemia provocada pela COVID-19? Epidemiol Serv Saúde [Internet]. 2020 abr [citado 2020 jul 03];29(2):e2020166. Disponível em: https://doi.org/10.5123/s1679-49742020000200024 [ Links ]
17. Dunlop C, Howe A, Li D, Allen LN. The coronavirus outbreak: the central role of primary care in emergency preparedness and response. BJGP Open [Internet]. 2020 Jan [cited 2020 Apr 15]:4(1):bjgpopen20X101041. Available from: https://doi.org/10.3399/bjgpopen20x101041 [ Links ]
18. Ministério da Saúde (BR). E-Gestor Atenção Básica. Cobertura da atenção básica [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 jul 27]. Disponível em: https://egestorab.saude.gov.br/paginas/acessoPublico/relatorios/relHistoricoCoberturaAB.xhtml [ Links ]
19. Souza FJPS, Briones FMA, Macambira J. Saúde pública e sua importância na luta contra a pobreza e a exclusão social. In: Castro D, Dal Seno, D, Pochmann M, organizadores. Capitalismo e a Covid-19 um debate urgente [Internet]. São Paulo: Edição do Autor; 2020 [citado 2020 maio 28]. p. 65. Disponível em: http://abet-trabalho.org.br/wp-content/uploads/2020/05/LIVRO.CapitalismoxCovid19.pdf [ Links ]
20. Lira P, Monteiro L. Violência, urbanização e desenvolvimento humano: uma análise espacial nos municípios capixabas. In: Marguti BO, Costa MA, Silva Pinto CV, organizadores. Territórios em números: insumos para políticas públicas a partir da análise do IDHM e do IVS de municípios e Unidades da Federação brasileira [Internet]. Brasília: IPEA; INCT; 2017 [citado 2020 jul 27]. p. 243-70 Disponível em: https://www.ipea.gov.br/portal/images/stories/PDFs/livros/livros/170828_territorios_em_numeros_1.pdf [ Links ]
21. Sistema de Informações Contábeis e Fiscais do Setor Público Brasileiro - SICONFI. Coronavirus (COVID-19). Tesouro nacional [Internet]. Brasília: Sistema de Informações Contábeis e Fiscais do Setor Público Brasileiro; 2020 [citado 2020 jul 27]. Disponível em: https://siconfi.tesouro.gov.br/siconfi/index.jsf;jsessionid=jyfsqZ2CVd3u-fl2MFIE8Ff6.node2 [ Links ]
Received: June 10, 2020; Accepted: July 15, 2020











 texto en
texto en 


