Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.4 Brasília 2020 Epub 13-Jul-2020
http://dx.doi.org/10.5123/s1679-49742020000300003
Research note
Waist circumference, waist-to-height ratio and overweight cut-off points: a cross-sectional study with elderly people in seven Brazilian cities, 2008-2009
1Universidade Estadual de Campinas, Faculdade de Ciências Médicas, Campinas, SP, Brazil
Objective
to identify cut-off points for waist circumference (WC) and waist-to-height ratio (WHtR) with better sensitivity, specificity and accuracy to distinguish overweight elderly people by sex, using three body mass index criteria as anthropometric references.
Methods
this was a cross-sectional study that analyzed weight, height and WC measurements of 3,477 elderly people (2008-2009); receiver operating characteristic (ROC) curves were used to define the cut-off points.
Results
WC cut-off points were 86.5cm, 88.7cm and 91.5cm in women, and 93.0cm, 96.0cm and 97.5cm in men, according to World Health Organization/WHO, Nutrition Screening Initiative/NSI and Pan American Health Organization/PAHO criteria, respectively; WHtR cut-off points corresponded to 0.57, 0.58, 0.59 in the female sex, and 0.56, 0.58 and 0.59 in the male sex; highest absolute overall accuracy values: PAHO (men) and WHO (women).
Key words: Aged; Waist Circumference; Body Mass Index; Waist-Height Ratio; Health Surveys; Cross-Sectional Studies
Introduction
Aging is associated with changes in body composition, revealed by reduction in lean mass, increase in fat mass and redistribution of these tissues in the body, with greater accumulation of intra-abdominal and intramuscular fat.1 Data from the Framingham Heart Study (2002-2005) show that both subcutaneous adipose tissue and intra-abdominal/visceral tissue are correlated with cardiometabolic risk factors, especially among women; when considering subcutaneous fat, the study found a strong correlation with waist circumference (WC) ( r =0.87 and r =0.88) and with body mass index (BMI) ( r =0.88 and r =0.83) in women and men, respectively.3
Different anthropometric measurements are used in clinical practice and in epidemiological studies to assess body adiposity, owing to their practicality and low cost, such as WC, BMI and waist-to-height ratio (WHtR). Some characteristics of these measurements will be dealt with in the next paragraph.
BMI does not differentiate between lean and fat body mass, nor does it assess body fat distribution; in addition, loss of muscle tissue affects its validity as an indicator of adiposity in elderly people, regardless of changes in weight.4 WC represents accumulated abdominal fat and is strongly correlated with visceral adipose tissue. This fat is assessed by imaging methods, such as computerized tomography.4 WHtR has been proposed as a more robust indicator of central adiposity than WC, since it results in an estimate that is not biased by height.6
Use of these measurements in elderly people requires definition of cut-off points (COPs) that take into consideration changes in body composition due to aging. Diverse criteria are used to classify the nutritional status of elderly people based on BMI, but there is no consensus in the literature as to the COPs adopted.7 With regard to WC, the Ministry of Health does not provide specific COPs for the elderly, but only for adults in general.8 In relation to WHtR, a COP was proposed in 2017 as a marker of overweight in elderly Brazilian people (age ≥60 years), using two BMI classifications as anthropometric references.11 Based on information from a cohort study which began in 2008, researchers proposed a WC COP for diagnosing obesity in elderly people (≥60 years) who used Brazilian National Health System (SUS) services in Goiânia/GO.12 Despite their relevance, studies in the literature that define specific COPs for the elderly in relation to overweight are rare.
Considering changes in body composition, the objective of this study was to identify cut-off points for WC and WHtR with greater sensitivity, specificity and accuracy to distinguish elderly people by sex, using three body mass index criteria as anthropometric references.
Methods
This was a cross-sectional multi-center study of Frailty in Elderly Brazilians (FIBRA Study, 2008/2009). The FIBRA Study was conducted with elderly community members resident in the urban areas of seven Brazilian cities, namely: Campinas/SP, Belém/PA, Poços de Caldas/MG, Ermelino Matarazzo/SP, Campina Grande/PB, Parnaíba/PI and Ivoti/RS.
The cities were selected by convenience. In each city the samples were obtained by means of clusters and in two stages: census tract and household. The eligibility criteria were: being ≥65 years old; being a permanent resident of the household/census tract; and not having serious impairment of cognition, physical health, communication or mobility (such as the bedridden and those with severe stroke sequelae). The description of sampling and further information about it, the quotas estimated and obtained by age and sex in each city and field research have already been published.13
The variables of interest were sex (male; female) and weight, height and WC measurements, measured in accordance with classic protocols.14
When measuring their weight, the elderly wore light clothing, with no objects in their pockets, took their shoes off and were positioned standing on platform scales, facing the scale, upright, looking straight ahead, with their feet parallel and slightly apart. When measuring their height, the elderly took their shoes off, stood upright, with their back to the scales, with their feet together and with their head in the Frankfurt Plane position.
Weight and height were used to calculate BMI [weight (kg)/height2(m)]. In order to assess overweight (overweight/obesity), the BMI values were dichotomized according to the criteria COPs: NSI (BMI >27kg/m2),7 recommended by the Ministry of Health/Food and Nutrition Surveillance System (SISVAN);8 PAHO (BMI ≥28kg/m2);9 and WHO (BMI ≥25kg/m2).10
In order to measure WC, the participant had to be standing up. Positioned facing the elderly person, the interviewer passed a measuring tape around their body, at the midpoint between the lower edge of the lowest rib and the iliac crest.14
WHtR was determined by dividing WC by height, in centimeters. A systematic review detected a 0.5 WHtR COP as a marker of cardiometabolic risk for adults in general.15 Our study intended to establish specific WHtR COPs for the elderly of both sexes, taking into consideration the alterations that occur in body composition owing to physiological, metabolic, socio-economic and psychological factors.16
For the purpose of analysis, ROC curve graphs were used to define WC and WHtR COPs corresponding to the condition of being overweight, according to three BMI classification criteria. Sensitivity (proportion of positive diagnostic tests among individuals having the condition of interest), specificity (proportion of negative diagnostic tests among individuals who did not have the condition) and accuracy (proportion of correct results of a diagnostic test) were obtained using Stata software. Overweight/obesity was considered to be the condition of interest. Comparisons were made between proportions by means of Pearson’s chi-square test, taking a 5% significance level and 95% confidence intervals (95%CI). The statistical analyses were performed using Stata, version 14.0.
The FIBRA Study was approved by the Campinas State University Faculty of Medical Sciences Research Ethics Committee on May 22nd2007 and registered on the Plataforma Brasil (Opinion: 208/2007; Certification of Submission for Ethical Appraisal – CAAE: 39547014.0.1001.5404). The elderly participants signed a Free and Informed Consent form.
Results
The data refer to 3,477 elderly people, 67.7% of whom were women (n=2,353). Among men, age varied between 65 and 97 years and average age was 73.3 years, while among women age varied between 65 and 101 years and average age was 72.8 years. Average BMI among men was 26.2kg/m2(95%CI 26.0; 26.5), while among women it was 27.4kg/m2(95%CI 27.2; 27.6). In relation to proportion of overweight, significant difference was found between the sexes: the proportions among women were 51.4%, 42.9% and 67.7%, while among men they were 40.0%, 31.0% and 60.3%, according to the NSI, PAHO and WHO criteria, respectively (p<0.001).
The COPs obtained for WC, using the WHO, NSI and PAHO criteria, were equal to 86.5cm, 88.7cm and 91.5cm for women, and equal to 93.0cm, 96.0cm and 97.5cm for men. For both sexes, the NSI criterion resulted in higher score estimates for sensitivity, corresponding to a COP of 88.7cm for women and 96.0cm for men ( Table 1 ), with no statistically significant difference and overlapping 95%CIs. With regard to WHtR, the COPs were 0.57, 0.58 and 0.59 for females, and 0.56, 0.58 and 0.59 for males, considering the WHO, NSI and PAHO criteria. Specificity and positive predictive value (PPV) were higher among women according to the WHO classification. Among men, the PAHO criterion had greater sensitivity, while the WHO criteria had greater PPV ( Table 1 ).
Table 1 – Sensitivity and specificity of cut-off points for waist circumference (WC) and waist-to-height ratio (WHtR) in relation to three gold standard body mass index (BMI) criteria among elderly people of both sexes, FIBRA Study, 2008/2009
| Sex | Cut-off point | Sensitivity (%) | Specificity (%) | Area under the curve (95%CI) | Positive predictive value (%) |
|---|---|---|---|---|---|
| Waist circumference (WC) | |||||
|
| |||||
| Female | ≥86.5a | 79.39 | 79.02 | 0.87 (0.86;0.89) | 88.82 |
| ≥88.7b | 83.00 | 76.69 | 0.87 (0.85;0.88) | 79.03 | |
| ≥91.5c | 75.71 | 82.12 | 0.87 (0.85;0.88) | 76.10 | |
|
| |||||
| Masculino | ≥93.0a | 80.42 | 82.39 | 0.89 (0.87;0.91) | 87.41 |
| ≥96.0b | 83.72 | 83.16 | 0.90 (0.88;0.92) | 76.85 | |
| ≥97.5c | 81.55 | 84.05 | 0.90 (0.88;0.92) | 69.72 | |
|
| |||||
| Waist-to-height ratio (WHtR) | |||||
|
| |||||
| Female | ≥0.57a | 79.03 | 81.54 | 0.87 (0.85;0.88) | 89.99 |
| ≥0.58b | 80.42 | 78.28 | 0.87 (0.86;0.89) | 79.67 | |
| ≥0.59c | 79.49 | 79.06 | 0.87 (0.86;0.87) | 74.06 | |
|
| |||||
| Masculino | ≥0.56a | 82.63 | 81.94 | 0.90 (0.88;0.92) | 87.43 |
| ≥0.58b | 82.26 | 85.84 | 0.91 (0.89;0.93) | 79.50 | |
| ≥0.59c | 88.02 | 83.66 | 0.92 (0.91;0.94) | 70.81 | |
a) Cut-off point considering the overweight/obesity category proposed by WHO (BMI ≥25 Kg/m2).
b) Cut-off point considering the overweight category proposed by NSI/Lipschitz (BMI >27 Kg/m2).
c) Cut-off point considering the overweight/obesity category proposed by PAHO (BMI ≥28 Kg/m2).
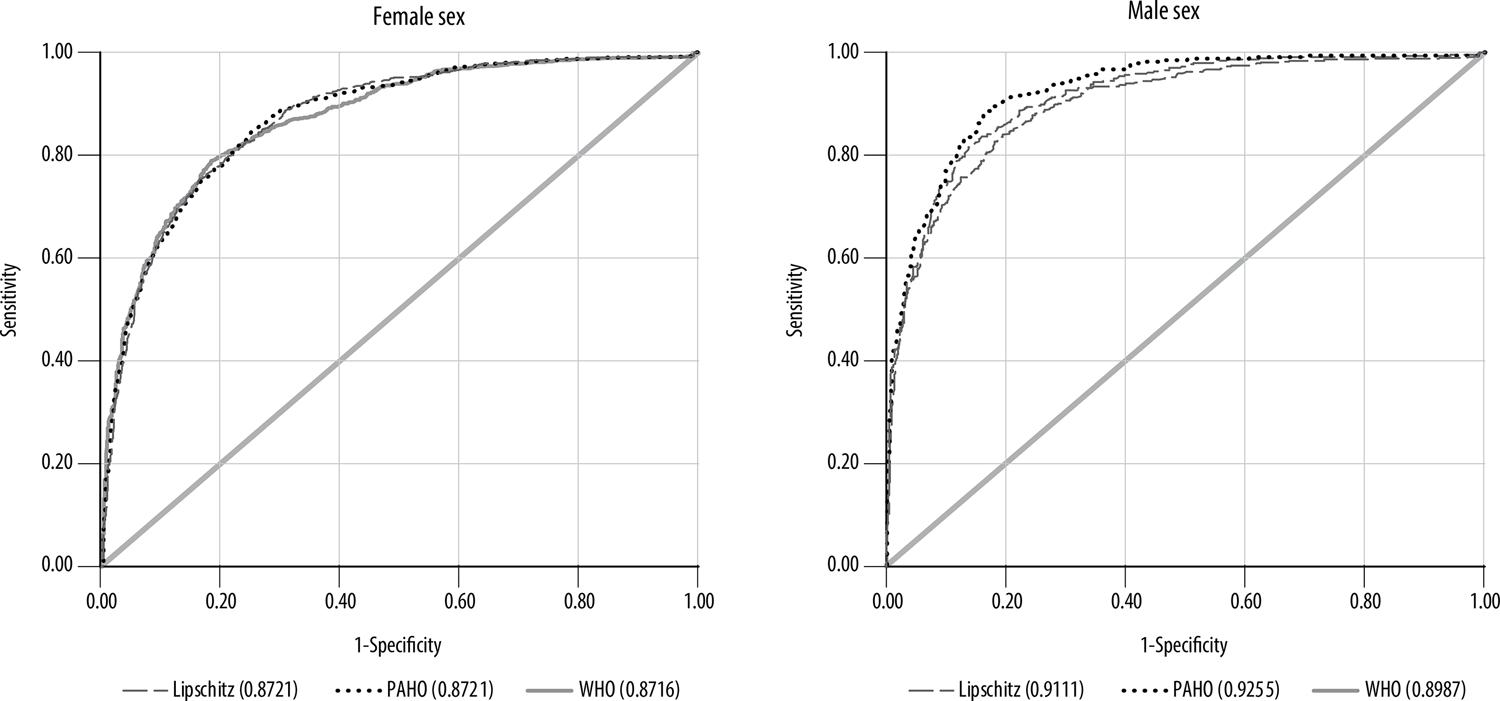
Although they were substantial for both sexes, the values of the areas under the ROC curves (overall accuracy) were not statistically different and the 95% CIs overlapped ( Table 1 , Figure 1 ). With regard to WHtR, overall accuracy was 0.87 for the three BMI classification criteria among the women, while among the men it varied between 0.90 (WHO) and 0.92 (PAHO). In relation to WC, overall accuracy was 0.87 for women and around 0.90 for men. No significant differences were detected for the results of the area under the curve for either sex, given the overlapping 95%CIs ( Table 1 , Figure 2 ).
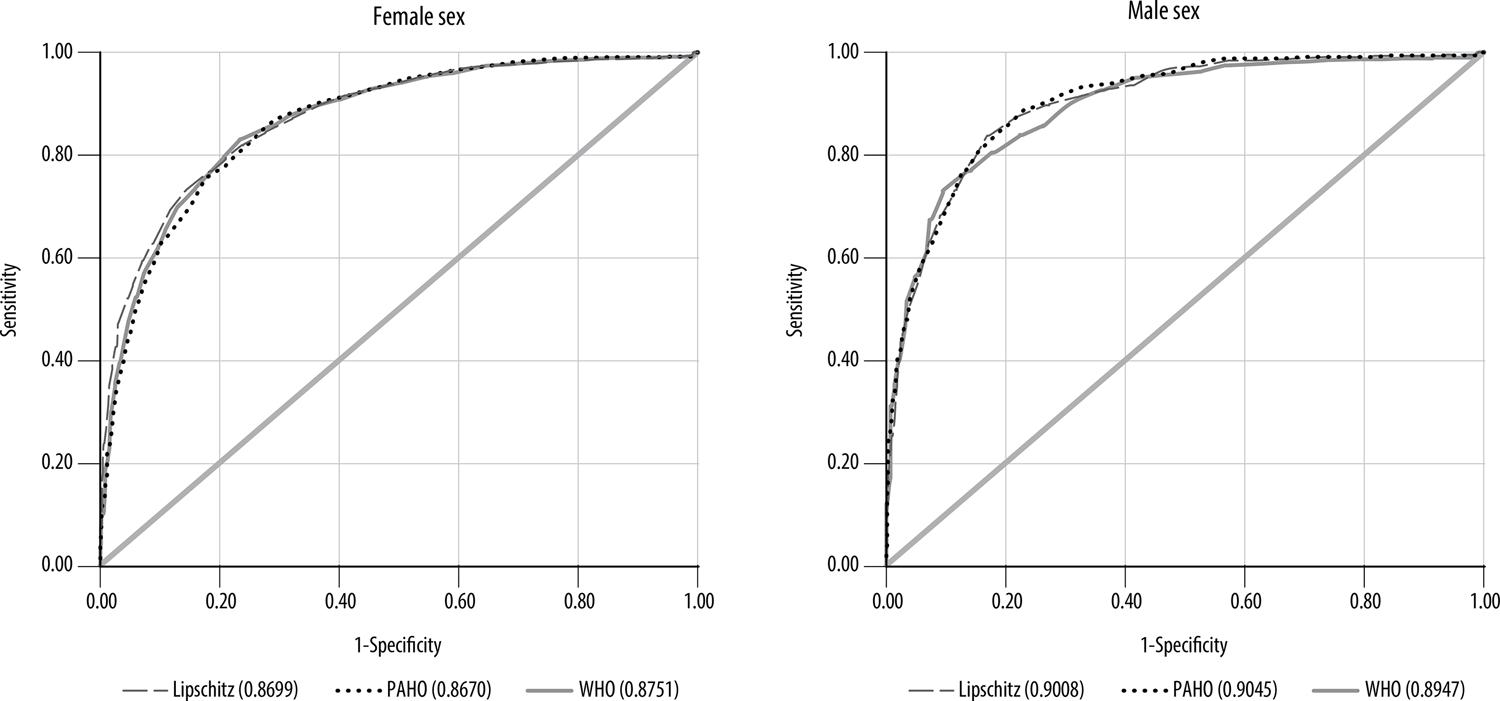
Figure 1 – Receiver operating characteristic (ROC) curves for waist circumference (WC), by sex and according to three gold standard body mass index (BMI) criteria, FIBRA Study, 2008/2009
Discussion
The main findings were: verifying WC and WHtR COPs for diagnosing overweight among the elderly according to three BMI classification criteria; the cut-off values obtained using NSI and PAHO criteria were found to be higher when compared to the WHO criterion, although with no significant differences.
Overweight was greater in women for all BMI references. The same result has been widely described in the literature,18 and is explained by physiological differences that determine fat accumulation and redistribution as part of aging.1 The BMI criteria produced similar WC and WHtR values for both sexes. The COPs detected for WC were higher than those established by WHO for the adult population (males ≥94cm; females ≥80cm).10 When analyzing a sample of elderly (≥60 years old) SUS service users in Goiânia/GO, Silveira et al.12 proposed a WC COP of 98.8cm for males and 90.5cm for females. The COPs obtained in this study were between 6.5cm and 11.5cm greater than that recommended by WHO for adult women, and between 1cm less and 3.5cm more than its COP established for adult men, in general. In relation to the COP proposed by Silveira et al.,12 our study identified differences of around 1cm for both men and women, when considering the WC COP resulting from the PAHO criterion.
With regard to WHtR, COPs were identified close to the 0.55 found by Corrêa et al.11 in 2008/2009, in a sample that was representative of the Brazilian population (≥60 years), with sociodemographic characteristics similar to those of the elderly people included in our study. The study conducted by Corrêa et al.11 was the first in Brazil to detect a WHtR COP for identifying overweight among the elderly using the NSI and WHO BMI classifications as anthropometric references. Our study has added information to the literature and can contribute to scientific discussion on the use of these anthropometric measurements with the elderly.
Compared to BMI, WC is a more robust predictor of mortality and risk of cardiovascular disease.2 Prospective cohort study data have detected greater incidence of heart disease in overweight individuals (BMI ≥25kg/m2) and with increased WC (≥94cm; ≥80cm),4 and with greater risk of overall mortality and mortality due to specific causes when WC and BMI increase.21 Use of WHtR has been recommended instead of WC and BMI measurements (on their own or together), because it provides better prediction of cardiometabolic risk factors.5
A possible selection bias should be considered as a limitation. The FIBRA Study opted for elderly people who attended data collection sites by their own means, so that it is likely that most of the participants belonged to the stratum with greater physical ability, while excluding elderly people who were bedridden or had severe stroke sequelae.
The conclusion is reached that regardless of the BMI criterion used to define overweight, the WC and WHtR COPs were similar. When undertaking anthropometric assessment of the elderly, consideration should be given to the COPS most appropriate for their nutritional profile. Progress in this field of science can contribute to improved diagnosis of chronic diseases related to obesity both in specific populations and in outpatient service contexts. Standing out among the implications for health services is the use of COPs that are more accurate for diagnosis and surveillance of elderly people with cardiometabolic risk.
REFERENCES
1. Beaufrere B, Morio B. Fat and protein redistribution with aging: metabolic considerations. Eur J Clin Nutr [Internet]. 2000 Jun [cited 2020 May 22];54 Suppl 3:S48-53. Available from: https://doi.org/10.1038/sj.ejcn.1601025 [ Links ]
2. Scafoglieri A, Provyn S, Bautmans I, Van Roy P, Clarys JP. Direct relationship of body mass index and waist circumference with body tissue distribution in elderly persons. J Nutr Health Aging [Internet]. 2011 Dec [cited 2020 May 22];15(10):924-31. Available from: https://doi.org/10.1007/s12603-010-0272-x [ Links ]
3. Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu C-Y, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the framingham heart study. Circulation [Internet]. 2007 Jul [cited 2020 May 22];116(1):39-48. Available from: https://doi.org/10.1161/circulationaha.106.675355 [ Links ]
4. Flint AJ, Rexrode KM, Hu FB, Glynn RJ, Caspard H, Manson JE, et al. Body mass index, waist circumference, and risk of coronary heart disease: a prospective study among men and women. Obes Res Clin Pract [Internet]. 2010 Jul [cited 2020 May 22];4(3):e171-e181. Available from: https://dx.doi.org/10.1016%2Fj.orcp.2010.01.001 [ Links ]
5. Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica - ABESO. Diretrizes brasileiras de obesidade 2016 [Internet]. 4. ed. São Paulo: Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica; 2016 [citado 2019 mar 5]. 186 p. Disponível em: https://portaldeboaspraticas.iff.fiocruz.br/biblioteca/diretrizes-brasileiras-de-obesidade-2016-abeso/ [ Links ]
6. Schneider HJ, Klotsche J, Silber S, Stalla GK, Wittchen H-U. Measuring abdominal obesity: effects of height on distribution of cardiometabolic risk factors risk using waist circumference and waist-to-height ratio. Diabetes Care [Internet]. 2011 Jan [cited 2020 May 22];34(1):e7. Available from: https://doi.org/10.2337/dc10-1794 [ Links ]
7. Cervi A, Franceschini SCC, Priore SE. Análise crítica do uso do índice de massa corporal para idosos. Rev Nutr [Internet]. 2005 nov-dez [citado 2020 maio 22];18(6):765-75. Disponível em: http://dx.doi.org/10.1590/S1415-52732005000600007 [ Links ]
8. Ministério da Saúde (BR). Orientações para coleta e análise de dados antropométricos em serviços de saúde: norma técnica do sistema de Vigilância Alimentar e Nutricional - SISVAN [Internet]. Brasília: Ministério da Saúde; 2011 [citado 2019 fev 12]. 76 p. Disponível em: http://dab.saude.gov.br/portaldab/biblioteca.php?conteudo=publicacoes/orientacoes_coleta_analise_dados_antropometricos [ Links ]
9. Organización Panamericana de la Salud. XXXVI Reunión del Comité Asesor de Investigaciones en Salud. Encuesta Multicéntrica: Salud Bienestar y Envejecimiento (SABE) en América Latina y el Caribe [Internet]. Washington, D.C: Organización Panamericana de la Salud; 2001 [citado 2019 fev 15]. 93 p. Disponível em: http://envejecimiento.csic.es/documentos/documentos/paho-salud-01.pdf [ Links ]
10. World Health Organization - WHO. Obesity: preventing and managing the global epidemic [Internet]. Geneva: World Health Organization; 2000 [cited 2019 Fev 12]. 252 p. Available from: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ [ Links ]
11. Corrêa MM, Tomasi E, Thumé E, Oliveira ERA, Facchini LA. Razão cintura-estatura como marcador antropométrico de excesso de peso em idosos brasileiros. Cad Saúde Pública [Internet]. 2017 [citado 2020 maio 22];33(5):e00195315. Disponível em: http://dx.doi.org/10.1590/0102-311x00195315 [ Links ]
12. Silveira EA, Pagotto V, Barbosa LS, Oliveira C, Pena GG, Velasquez-Melendez G. Acurácia de pontos de corte de IMC e circunferência da cintura para a predição de obesidade em idosos. Ciên Saúde Coletiva [Internet]. 2020 mar [citado 2020 maio 22];25(3):1073-82. Disponível em: http://dx.doi.org/10.1590/1413-81232020253.13762018 [ Links ]
13. Neri AL, Yassuda MS, Araújo LF, Eulálio MC, Cabral BE, Siqueira MEC, et al. Metodologia e perfil sociodemográfico, cognitivo e de fragilidade de idosos comunitários de sete cidades brasileiras: Estudo FIBRA. Cad Saúde Pública [Internet]. 2013 abr [citado 2020 maio 22];29(4):778-92. Disponível em: http://dx.doi.org/10.1590/S0102-311X2013000400015 [ Links ]
14. World Health Organization. Physical status: the use and interpretation of anthropometry [Internet]. Geneva: World Health Organization; 2003 [cited 2019 Feb 12]. 452 p. Available from: https://www.who.int/childgrowth/publications/physical_status/en/ [ Links ]
15. Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev [Internet]. 2010 Dec [cited 2020 May 22];23(2):247-269. Available from: https://doi.org/10.1017/s0954422410000144 [ Links ]
16. Amarya S, Singh K, Sabharwal M. Changes during aging and their association with malnutrition. J Clin Gerontol Geriatr [Internet]. 2015 Sep [cited 2020 May 22];6(3):78-84. Available from: https://doi.org/10.1016/j.jcgg.2015.05.003 [ Links ]
17. Ahmed T, Haboubi N. Assessment and management of nutrition in older people and its importance to health. Clin Interv Aging [Internet]. 2010 Aug [cited 2020 May 22];9(5):207-16. Available from: https://doi.org/10.2147/cia.s9664 [ Links ]
18. Pereira IFS, Spyrides MHC, Andrade LMB. Estado nutricional de idosos no Brasil: uma abordagem multinível. Cad Saúde Pública [Internet]. 2016 maio [citado 2020 maio 22];32(5):e00178814. Disponível em: http://dx.doi.org/10.1590/0102-311X00178814 [ Links ]
19. Rezende FAC, Ribeiro AQ, Priore SE, Franceschinni SCC. Anthropometric differences related to genders and age in the elderly. Nutr Hosp [Internet]. 2015 Aug [cited 2020 May 22];32(2):757-64. Available from: https://doi.org/10.3305/nh.2015.32.2.8641 [ Links ]
20. Lima-Costa MF, Firmo JOA, Uchôa E. The Bambuí cohort study of aging: methodology and health profile of participants at baseline. Cad Saúde Pública [Internet]. 2011 [cited 2020 May 22];27 Suppl 3:327-35. Available from: http://dx.doi.org/10.1590/S0102-311X2011001500002 [ Links ]
21. Leitzmann MF, Moore SC, Koster A, Harris TB, Park Y, Hollenbeck A, et al. Waist circumference as compared with body-mass index in predicting mortality from specific causes. PLoS One [Internet]. 2011 Apr [cited 2020 May 22];6(4):e18582. Available from: https://doi.org/10.1371/journal.pone.0018582 [ Links ]
* The research that gave rise to this article received funding from the National Council for Scientific and Technological Development (CNPq, Process No. 55.5082/2006-7), the Coordination for the Improvement of Higher Education Personnel (CAPES, Process No. 02-P-4532/2017) and the São Paulo State Research Support Fund (FAPESP, Process No. 2017/23245-0).
Received: December 14, 2019; Accepted: May 13, 2020











 texto em
texto em