Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.5 Brasília 2020 Epub 27-Out-2020
http://dx.doi.org/10.1590/s1679-49742020000500013
Original Article
Health Academy Program: correlation between noncommunicable chronic disease hospitalizations and program adherence in Brazilian municipalities, 2011-2017*
1Universidade de Brasília, Faculdade de Ciências da Saúde, Brasília, DF, Brasil
2Universidade Federal do Rio Grande do Sul, Programa de Pós-Graduação em Saúde Coletiva, Porto Alegre, RS, Brazil
3Universidade de Brasília, Programa de Pós-Graduação em Ciência Política, Brasília, DF, Brazil
Objective:
To analyze the correlation between municipalities adhering to the Health Fitness Center Program, noncommunicable chronic disease (NCD) hospitalizations and socioeconomic levels from 2011 to 2017.
Methods:
This was an ecological study; HFCP adherence indicators for 2,837 municipalities were calculated, as were NCD hospitalization indicators, according to funding categories and the Firjan Socioeconomic Development Index.
Results:
The HFCP adherence indicator was higher for municipalities that received Congress funding (1.18), had moderate to high Firjan Socioeconomic Development Indices (0.94) and high NCD hospitalization indicators (1.03) (p<0.001). There were positive correlations (p<0.05) between the two indicators in municipalities receiving Ministry of Health funding (r=0.14) and those receiving both Congress and Ministry of Health funding (r=0.12); whereas correlation was negative in municipalities with moderate to low Firjan Socioeconomic Development Indices (r=-0.09; p=0.013).
Conclusion:
The main form of adherence to the HFCP, according to population size, was through Congress funding. Municipalities with poorer socioeconomic and NCD indicators had lower adherence to the HFCP.
Keywords: Primary Health Care; Health Programs and Plans; Health Equity; Chronic Disease; Ecological Study
Introduction
Brazilian Primary Care has achieved success in improving access to health services, in addition to support for putting municipal programs into place focused on disease prevention and health promotion.1 One of these initiatives is the Health Fitness Center Program (HFCP), brought into being in 2011 to help to address high prevalence of chronic noncommunicable diseases (NCDs).
NCDs are responsible for approximately 70% of deaths worldwide. They have direct impact on the economically active population2 and are an emerging challenge for health systems.3 The Strategic Action Plan to Address NCDs in Brazil, 2011-20224 includes the HFCP as one of its initiatives. The Federal Government encourages implementation of the Program at the local level, by transferring funds for building and operating centers,5 carrying out individual and group activities and services, health education, promoting healthy eating, active lifestyles and body practices, among other actions. These characteristics might contribute to a perspective of HFCP success, given that population-based programs are more inclined to achieving better results when diverse activities are offered and targeted on both an individual and a collective level.6
One of HFCP's critical aspects lies in funding adherence through public-sector building. In this case, adherence is conditioned to the transfer of financial resources from the Federal Government to municipal governments, known as “voluntary transfers”. These fund transfers bestow power and advantages on political stakeholders and groups at the Federal level, and preferentially benefit municipalities with greater technical capacity to negotiate and which comprise electoral and political party constituencies, rather than benefit municipalities that are economically more vulnerable. As such, it has been noted that political and party-political factors and technical capacities stand out in the redistribution of resources that should benefit places in greater need.7,8
With regard to the choice of municipalities to adhere to the HFCP, there is no formal and official definition of criteria that take into consideration the socioeconomic status and epidemiological situation of municipalities as being a priority in the implementation process, which would be the ideal as it would ensure coherence with the Program's social purpose. Added to this is the fact of the HFCP being a Brazilian National Health System (SUS) public policy, anchored in the System's principle of equality while, at the same time, depending on Congress funding to build infrastructure and maintain activities, the original purpose of which is to allocate public funds and meet the needs of more socioeconomically vulnerable populations and territories. Notwithstanding, the precarious nature of the criteria used in relation to need and technical and political feasibility interferes with the fulfillment of this commitment.8
The adherence procedure, i.e. allocation, is linked to funding of building works and is classified in two phases. In the first phase, from 2011 to 2012, building works were funded through Ministry of Health resources, referred to here as ‘Program’; in the second phase, with effect from 2013, building works received funding through Congress resources allocated by individual parliamentarians. The only documented justification for this change is that the HFCP, as a health promotion and therefore intersectoral initiative, was not considered to be health expenditure.9 The share of the Legislative Body in allocating investment resources up until 2017 was considerable, equivalent to BRL 205.6 million – versus over BRL 300 million for adherence via Program transfers, according to Ministry of Health information.10
None of the studies on the HFCP available in the scientific literature has analyzed the relationship between Program resource distribution and health and socioeconomic indicators.11–14 The objective of this study was precisely that of analyzing the correlation between municipal adherence to the HFCP, NCD hospitalizations and local socioeconomic levels between 2011 and 2017.
Methods
This was an ecological study, the aggregate units of analysis of which were the Brazilian municipalities. The study used secondary data on 2,837 municipalities that had their adherence to the HFCP approved according to public-sector building works in the period 2011-2017.
The data were retrieved in 2018 and 2019. Brazilian Institute of Geography and Statistics (IBGE) data were used to comprise the indicators used. HFCP technical data were obtained from the Ministry of Health. The following variable categories were used: epidemiological NCD indicator (low; moderate; high); Firjan Socioeconomic Development Indicator (low to regular; moderate to high); and types of HFCP funding (Congress funding; Program funding; both).
The municipal adherence indicator was calculated as the ratio between total number of municipalities adhering and average municipal population between 2011 and 2017, multiplied by 10,000 (population adjustment). The NCD hospitalization indicator was built using NCD hospitalizations as per the list of Ambulatory Care Sensitive Conditions (ACSC). The NCDs used in the analysis were those of epidemiological relevance,15 as per the Ministry of Health morbidity, in accordance with the International Statistical Classification of Diseases and Health Related Problems, 10th Edition (ICD-10): essential (primary) hypertension (ICD-10: I10); other hypertensive diseases (ICD-10: I11-I15); diabetes mellitus (ICD-10: E10-E14); heart failure (ICD-10: I50); intracranial hemorrhage (ICD-10: I60-I62); cerebral infarction (ICD-10: I63); stroke, not specified as hemorrhage or infarction (ICD-10: I64); and other cerebrovascular diseases (ICD-10: I65-I69).16
The NCD hospitalization indicator refers to the ratio between the total number of NCD hospitalizations as per the ACSC e list and the average monthly population between 2011 and 2017, multiplied by 10,000, corresponding to the hospitalization rate. Hospitalization data were retrieved from the Brazilian National Health System Hospital Information System (SIH/SUS) using the Tabnet instrument (SUS Information Technology Department [DATASUS]/Ministry of Health), taking the ‘Health Information – Epidemiological and Morbidity’ field, by place of residence, with effect from 2008. A dummy variable was used for this indicator based on dividing the data into tertiles: 1st tertile, up to 189.798 (low); 2nd tertile, 189.799 to 335.066 (moderate); 3rd tertile, above 335.068 (high).
The Firjan Socioeconomic Development Indicator was used as the socioeconomic criterion. The Firjan Socioeconomic Development Indicator is prepared by the Federation of Industries of the State of Rio de Janeiro based on official public statistics and reflects municipal socioeconomic development, using data on employment, income, education and health.17 the Firjan Socioeconomic Development Indicator data for 2011 to 2016 (last year available) were retrieved from the Firjan platform. If indices were missing for a municipality, their respective Firjan Socioeconomic Development Indicator annual state averages were used. Data for 2016 and 2017 were imputed. Following this, the average municipal Firjan Socioeconomic Development Indicator was calculated for the period studied and classification was performed according to the categories stipulated by the index's developers: low development (0-0.4); regular development (0.4-0.6); moderate development (0.6-0.8); and high development (0.8-1).
Funding categories were applied according to the types of funding available for adherence to public-sector building works: (i) only Congress funding (parliamentarian); (ii) only Program funding (funding from the Ministry of Health budget); (iii) both types of funding. Considering data distribution between the Firjan Socioeconomic Development Indicator ranges, we opted to analyze these data in a dichotomous manner, into the ‘low to regular’ category (0-0.6) and the ‘moderate to high’ category (0.6-0.8).
For the purpose of analysis, the types of funding and the socioeconomic and epidemiological indicators were used to classify the municipalities. The R computer program was used for data tabulation and analysis. The results are shown in absolute, relative and measures and quartiles (first and third). The Kruskal-Wallis test was used in order to compare the adherence indicator according to funding category, and the Wilcoxon-Mann-Whitney test was used in order to compare the Firjan Socioeconomic Development Indicator categories and the NCD hospitalization indicator categories. Spearman (two-sided) correlation tests were performed to verify the relationship between adherence indicators and NCD indicators, according to the funding categories and the Firjan Socioeconomic Development Indicator categories. A 5% significance level was established for all tests. The study project was not submitted to a Research Ethics Committee as it used public domain secondary data with no nominal identification.
Results
A total of 2,837 municipalities adhered to the HFCP through public-sector building works in the period 2011 to 2017. The Northern and Southeastern macro-regions had the highest (58%) and the lowest (44%) proportion of municipalities adhering to the HFCP, respectively. The absolute number of adhering municipalities was highest in the Northeast (1,338), compared to the other macro-regions, although adherence indicators were highest in the Midwestern and Southern regions (both having 1.36 and standard deviation [SD]=1.2), and in the Northern region (1.33; SD=1.3) (Table 1). Among the municipalities analyzed, 349 (12%) had adhered to more than one program per 9,000 inhabitants.
Table 1 Distribution of adherence to the Health Fitness Center Program by macro-region, Brazil, 2011-2017
| Macro-region | Municipalities n |
Adhering municipalities n (%) |
Adherence n |
Mean adherence indicator (standard deviation) |
|---|---|---|---|---|
| Northeast | 1,794 | 979 (55) | 1,338 | 1.07 (0.9) |
| North | 450 | 261 (58) | 383 | 1.33 (1.3) |
| Midwest | 467 | 255 (55) | 343 | 1.36 (1.2) |
| Southeast | 1,668 | 736 (44) | 1,102 | 1.18 (1.3) |
| South | 1,191 | 606 (51) | 775 | 1.36 (1.2) |
Regarding funding categories, the majority (57%) of municipalities had ‘Program’ type funding, while those that had both types of funding – Program and Congress – accounting for just 11% of the total. Municipalities with a moderate to high Firjan Socioeconomic Development Indicator accounted for the highest proportion of adherence (72%). With regard to the NCD hospitalization indicator, the municipal percentages were similar in all three adherence categories (Table 2).
Table 2 Number of municipalities adhering to the Health Fitness Center Program by variable category, Brazil, 2011-2017
| Variables | Municipalities | ||
|---|---|---|---|
| n | % | ||
| Funding | |||
| Congress | 927 | 33 | |
| Program (Ministry of Health budget resources) | 1,605 | 57 | |
| Both | 305 | 11 | |
| Firjan Socioeconomic Development Indicator | |||
| Low to regular | 802 | 28 | |
| Moderate to high | 2,035 | 72 | |
| Chronic noncommunicable disease indicator | |||
| Low | 951 | 34 | |
| Moderate | 942 | 33 | |
| High | 944 | 33 | |
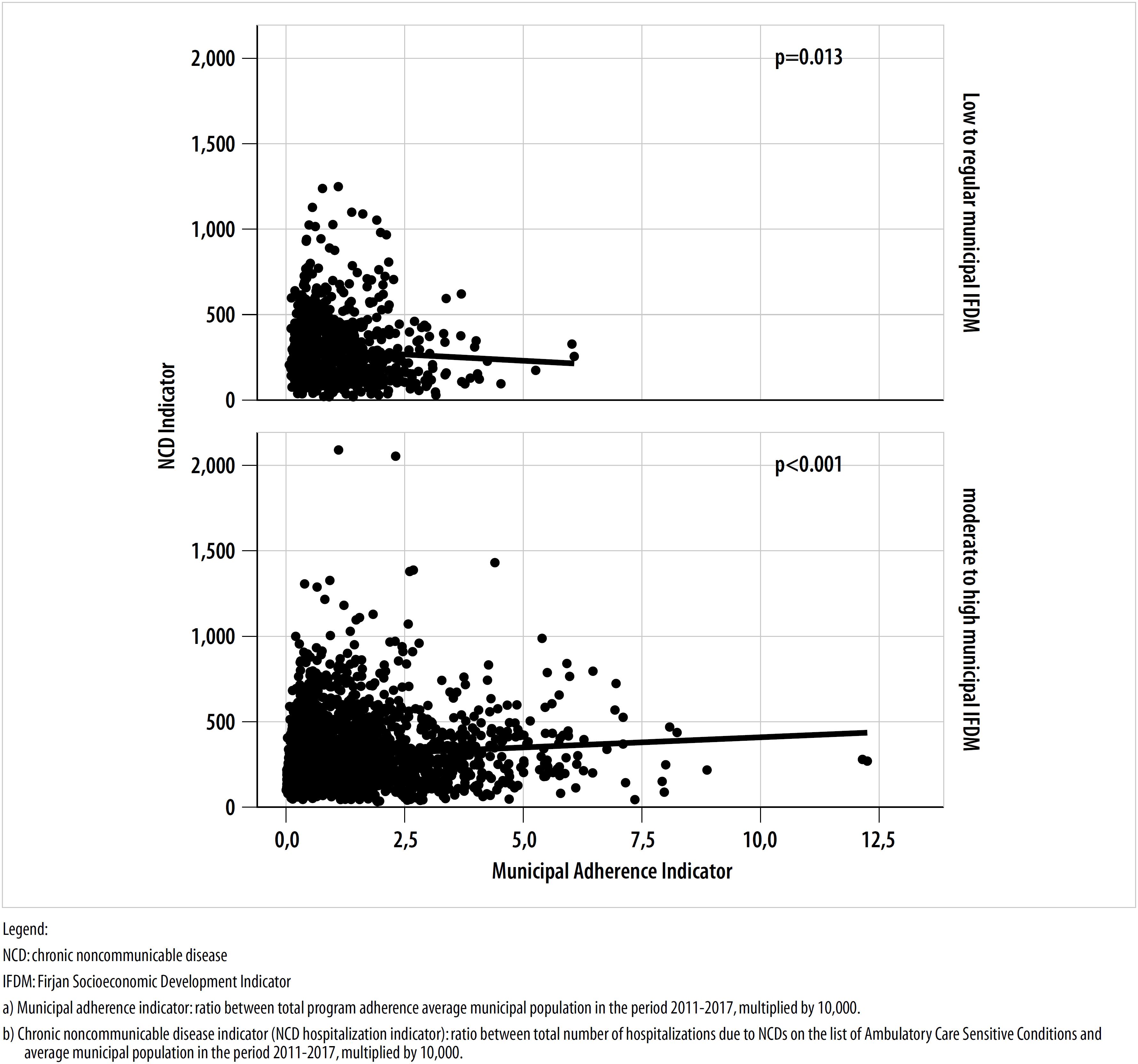
The adherence indicator had higher values in municipalities with Congress funding (1.18), moderate to high Firjan Socioeconomic Development Indicators (0.94) and high NCD hospitalization indicators (1.03) (p<0.001) (Table 3). Correlations between adherence indicators and NCD indicators, according to funding categories, are shown in Figure 1. Correlations were significant for the ‘Program’ form of funding (r = 0.14; p<0.001) and joint Congress and Program funding (r=0.12; p=0.043) (Figure 1).
Table 3 Distribution of the Health Fitness Center Program adherence indicator by type of funding, socioeconomic development index and chronic noncommunicable disease indicator category, Brazil, 2011-2017
| Variables | Adherence indicator | ||
|---|---|---|---|
| Median (Quartile 1 and Quartile 3) | p-valuea | ||
| Funding | |||
| Congress | 1.18 (0.60;2.05) | <0,001 | |
| Program (Ministry of Health budget resources) | 0.81 (0.34;1.70)b | ||
| Both | 0.82 (0.38;1.43)b | ||
| Índice Firjan de Desenvolvimento Socioeconômico – IFDM | |||
| Baixo a regular | 0.87 (0.60;2.05) | <0.001 | |
| Moderado a alto | 0.94 (0.38;1.95) | ||
| Indicador de doenças crônicas não transmissíveis – IND-DCNT | |||
| Baixo | 0.90 (0.36;1.72)c | <0.001 | |
| Moderado | 0.87 (0.36;1.75)c | ||
| Alto | 1.03 (0.52;1.94) | ||
a)The Wilcoxon-Mann-Whitney test was used for the Firjan Socioeconomic Development Indicator categories and for the NCD hospitalization indicator categories, while the Kruskal-Wallis test was used for funding categories.
b)Difference for Congress (p-value<0.001).
c)Difference for the NCD hospitalization indicator in the ‘high’ category (p-value<0.001).
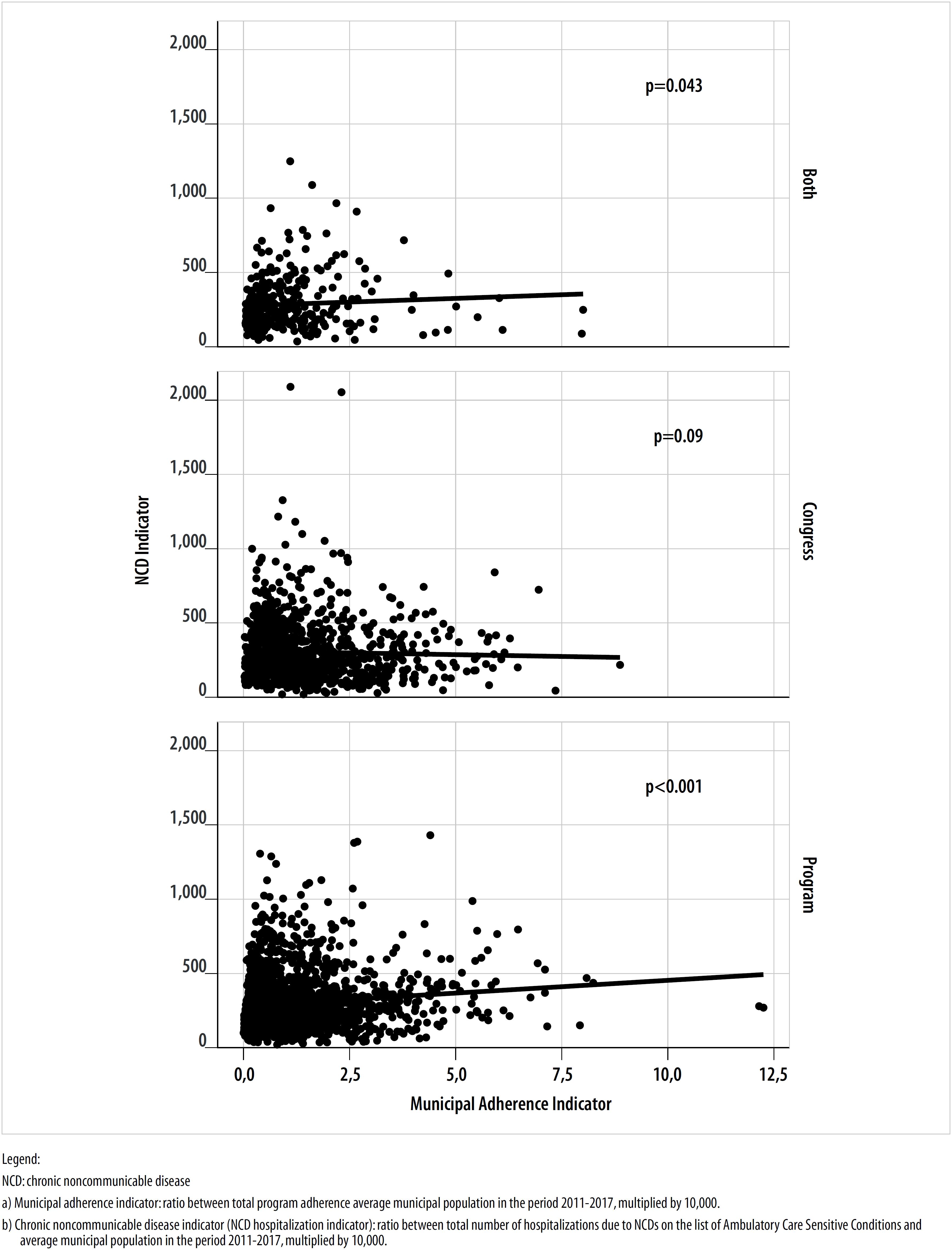
Figure 1 Correlation between the municipal adherence indicatora for the Health Fitness Center Program and the chronic noncommunicable disease indicator,b by type of funding, Brazil, 2011-2017
Figure 2 shows the relationships between adherence indicators and NCD indicators according to socioeconomic development situation. In the case of municipalities with a low to regular Firjan Socioeconomic Development Indicator, the correlation coefficient was negative (r=-0.09; p=0.013), demonstrating an inverse relationship between the adherence indicator and the NCD hospitalization indicator, whereas correlation was positive (r=0.13; p<0.001) for municipalities with a moderate to high Firjan Socioeconomic Development Indicator.
Discussion
The results of this study provided evidence of the higher indicator of HFCP adherence through Congress funding, when associated with municipalities with moderate to high Firjan Socioeconomic Development Indicators and high NCD indicators. Moreover, in the case of municipalities receiving Program funding or both types of funding (Congress and Ministry Program), correlation between adherence indicators and NCDs was positive, while in the case of municipalities with low to regular Firjan Socioeconomic Development Indicators, the adherence indicator reduced proportionately to the increase in the NCD indicator.
The higher adherence indicator found in the group of municipalities with Congress funding – despite the predominance of adherence with Program funding in absolute and proportional numbers – means that Congress funding had the power to concentrate more than one HFCP adherence per municipality. No initiatives were found in the scientific literature with mixed funding similar to the case of the HFCP, for the purposes of comparison. However, studies indicate that Congress funding tends to be directed towards municipalities where there is political party affinity between the mayor and the Federal Government,18 and between the mayor and the parliamentarian allocating Congress funding.19
The following finding stands out with regard to HFCP adherence distribution, from the perspective of municipal socioeconomic development, in general, municipalities with higher adherence indicators fall into the group with moderate to high Firjan Socioeconomic Development Indicators, while municipalities with low to regular Firjan Socioeconomic Development Indicators showed a negative relationship between adherence indicators and NCD indicators. These findings differ from those of another recent study, which demonstrated that almost half the municipalities taking part in the HFCP fell into the category of the lowest Municipal Human Development Index (IDHM).20 Although that study and our study did not use the same indices, the characteristics of the IDHM and the Firjan Socioeconomic Development Indicator are similar and can therefore be compared.
Socioeconomic inequalities exacerbate and directly influence the process of the population becoming ill.21–23 There is scientific evidence that low levels of schooling23 and low levels of socioeconomic development21 are related to high NCD prevalence. Moreover, low-income people have more risk factors and face more barriers to health service access.22 The socioeconomic development dimension, as represented either by the IDHM or by the Firjan Socioeconomic Development Indicator, was also used by another study to analyze voluntary transfers made by the Federal Government24 and the authors concluded that the volume of funds transferred was not related to the IDHM but rather to party political alignment.
Particularly with regard to our study, as the HFCP transfers fall into the health investment category, their being allocated to municipalities should comply with equality criteria, in order to reduce inequalities in health service availability and ensure comprehensive health care provided by the HFCP.25 Notwithstanding, it is known that the mechanism for increasing SUS voluntary transfers results from adherence by municipalities to Ministry of Health programs.26
This study found that the adherence indicator was higher for municipalities with a high NCD hospitalization indicator. Municipalities receiving Program funding and mixed funding showed a direct relationship between the indicators studied, which pointed to increased resource allocation to municipalities with more critical NCD hospitalization indicators.
The results of this study are in line with the objectives of the Strategic Action Plan to Address NCDs in Brazil, 2011-2022,4 in that they corroborate the findings of other authors regarding the NCD burden in Brazil.27 NCDs have reached a high level of priority on the governmental Public Health agenda in Brazil, and are integrated with diverse initiatives under way. It is therefore fundamental that resource allocation management be qualified. Considering the purpose of ensuring equity inherent to HFCP adherence formalization, with the aim of avoiding disparities and unfairness among the populations benefitted,28 it is essential to extend the program to more critical municipalities, whether this be with regard to the epidemiological aspect of NCDs, or whether it be with regard to their socioeconomic situation, regardless of the type of funding.
During the period selected, the maximum number of program adherences per municipality was based on the Ministry of Health administrative criterion of one HFCP per 9,000 inhabitants. Health service technical personnel and managers involved with HFCP were aware of this fact, although it was not standardized. Aware that this criterion could bias the indicator used in this study, we requested additional information from the Ministry of Health. The Ministry replied that the rule only applied up until 2012. For this reason, we analyzed compliance with the rule by taking the total number of adherences and the average population from 2011 to 2017, with the aim of identifying this situation and achieving a better discussion of the results thereof.
The results related to this criterion counter the information received from the Ministry of Health and minimize interpretation bias. Moreover, the overall findings of this study enable us to state that this criterion, regardless of whether it was used only up until 2012 or in any year during the period analyzed, was used in an erroneous manner, from the epidemiological and socioeconomic point of view. Although the scope of this study was not to point to the reasons underlying HFCP distribution over the national territory, comparing the results found with the evidence gives rise to questioning as to the link between HFCP allocation and the logic of the flow of Federal Government voluntary transfers. This logic points to resources being allocated as a priority to places where political gains are greater,7,24,29,30 without adopting a redistribution model with the purpose of equalizing public revenue inequalities30 which imply generation of social inequalities.
Among the limitations of this study, firstly we highlight the need for caution in interpreting its results. It is a cross-sectional ecological study, whereby it is not possible to establish a causal relationship between HFCP adherence and NCD hospitalizations, or any inferences regarding the speculative relationships found supported by the available literature. A second limitation lies in the data found being analyzed on a collective level; when considered on an individual level, there may be differences due to causal bias and ecological fallacy.
In conclusion, the main form of HFCP adherence, during the period studied, was by means of Congress funding in terms of the size of the population benefitted, while lower adherence corresponded to municipalities with the poorest socioeconomic and NCD indicators. The HFCP was created as an alternative intervention for prevention and/or treatment of NCD risk factors, within Primary Health Care. However, the study's findings demonstrate that there is a contradiction in the adherence process when taking the socioeconomic and epidemiological perspectives together and the source of the funding used for municipal implementation of the program. The challenge for HFCP management therefore lies in the definition and implementation of equitable allocation criteria, in keeping with the Health sector's budgetary capacity, in order to benefit more vulnerable municipalities and, consequently, people more exposed to chronic noncommunicable diseases.
*Article derived from the academic thesis entitled ‘Study of Health Fitness Center Program implementation in Brazil from 2011 to 2017 from a process perspective’, defended by Dalila Tusset at the University of Brasília Health Sciences Faculty Health Sciences Postgraduate Program in December 2019.
REFERENCES
1. Paim J, Travassos C, Almeida C, Bahia L, Macinko J. O sistema de saúde brasileiro: história, avanços e desafios. Lancet (Série Brasil) [Internet]. 2011 maio [citado 2018 dez 17];1:11-31. Disponível em: http://download.thelancet.com/flatcontentassets/pdfs/brazil/brazilpor1.pdf [ Links ]
2. World Health Organization - WHO. Global action plan for the prevention and control of NCDs 2013-2020 [Internet]. Geneva: World Health Organization; 2013 [cited 2018 Aug 23]. Available from: http://www.who.int/nmh/events/ncd_action_plan/en/ [ Links ]
3. Barros MBA, Francisco PMSB, Zanchetta LM, César CLG. Trends in social and demographic inequalities in the prevalence of chronic diseases in Brazil, PNAD: 2003- 2008. Ciênc Saúde Coletiva [Internet]. 2011 Sep [cited 2020 Jul 15];16(9):3755–68. Available from: https://doi.org/10.1590/S1413-81232011001000012 [ Links ]
4. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise e Situação de Saúde. Plano de ações estratégicas para o enfrentamento das doenças crônicas não transmissíveis (DCNT) no Brasil, 2011-2022 [Internet]. Brasília: Ministério da Saúde; 2011 [citado 2020 jul 15]. (Série B. Textos básicos de saúde). 160 p. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/plano_acoes_enfrent_dcnt_2011.pdf [ Links ]
5. Brasil. Ministério da Saúde. Portaria de Consolidação n° 6, de 28 de setembro de 2017. Consolidação das normas sobre o financiamento e a transferência dos recursos federais para as ações e os serviços de saúde do Sistema Único de Saúde [Internet]. Diário Oficial da União, Brasília (DF), 2017 out 3 [citado 2020 jul 15]; Suplemento:569. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2017/prc0006_03_10_2017.html [ Links ]
6. Philip PM, Kannan S, Parambil NA. Community-based interventions for health promotion and disease prevention in noncommunicable diseases: a narrative review. J Educ Health Promot [Internet]. 2018 Nov [cited 2019 May 03];7:141. Available from: https://dx.doi.org/10.4103%2Fjehp.jehp_145_18 [ Links ]
7. Soares MM, Melo BG. Condicionantes políticos e técnicos das transferências voluntárias da União aos municípios brasileiros. Rev Adm Pública [Internet]. 2016 ago [citado 2019 abr 16];50(4):539-62. Disponível em: https://doi.org/10.1590/0034-7612138727 [ Links ]
8. Baptista TWF, Machado CV, Lima LD, Garcia M, Andrade CLT, Gerassi CD. As emendas parlamentares no orçamento federal da saúde. Cad Saúde Pública [Internet]. 2012 dez [citado 2019 abr 16];28(12):2267-79. Disponível em: https://doi.org/10.1590/S0102-311X2012001400006 [ Links ]
9. Câmara dos Deputados (BR). Regulamentação da emenda constitucional n° 29, de 2000 (Piso Constitucional de Aplicação em Saúde). Análise das principais inovações trazidas pela Lei Complementar n° 141, de 13 de janeiro de 2012, que regulamentou a Emenda Constitucional n° 29, de 2000 [Internet]. Brasília: Câmara dos Deputados; 2012 [citado 2019 mar 04]. 39 p. Disponível em: http://www2.camara.leg.br/orcamento-da-uniao/estudos/2012/nt14.pdf [ Links ]
10. Ministério da Saúde (BR). Sala de Apoio à Gestão Estratégica. Academia da saúde - obras [Internet]. Brasília: Ministério da Saúde; 2019 [citado 2019 maio 04]. Disponível em: http://sage.saude.gov.br/# [ Links ]
11. Carvalho FFB, Jaime PC. O Programa Academia da Saúde – um estabelecimento de saúde da atenção básica. J Manag Prim Healh Care [Internet]. 2015 [citado 2020 jul 15];6(1):47-64. Disponível em: https://pdfs.semanticscholar.org/1d84/e72d6659d7ac633391a5c52e8ff4cd713d58.pdf [ Links ]
12. Sá GBAR, Dornelles GC, Cruz KG, Amorim RCA, Andrade SSCA, Oliveira TP, et al. O Programa Academia da Saúde como estratégia de promoção da saúde e modos de vida saudáveis: cenário nacional de implementação. Ciênc Saúde Coletiva [Internet]. 2016 jun [citado 2019 abr 17];21(6):1849-60. Disponível em: https://doi.org/10.1590/1413-81232015216.09562016 [ Links ]
13. Florindo AA, Reis RS, Farias Junior JC, Siqueira FV, Nakamura, Hallal PC. Description of health promotion actions in Brazilian cities that received funds to develop “Academia da Saúde” program. Rev Bras Cineantropometria Desempenho Hum [Internet]. 2016 Jul-Aug [cited 2020 Jul 15];18(4):483-92. Available from: https://doi.org/10.5007/1980-0037.2016v18n4p483 [ Links ]
14. Florindo AA, Nakamura PM, Farias Júnior JC, Siqueira FV, Reis RS, et al. Promotion of physical activity, healthy eating and family health in municipalities with health gym. Rev Bras Educ Fís Esporte [Internet]. 2016 Oct-Dec [cited 2020 Jul 15];30(4):913-24. Available from: https://doi.org/10.1590/1807-55092016000400913 [ Links ]
15. Mello JM, Borges PKO, Muller EV, Grden CRB, Pinheiro FK, Borges WS. Hospitalizations for ambulatory care sensitive noncommunicable diseases of the circulatory system. Texto Contexto Enferm [Internet]. 2017 Apr [cited 2019 Feb 15];26(1). Available from: https://doi.org/10.1590/0104-07072017003390015 [ Links ]
16. Brasil. Ministério da Saúde. Portaria MS/GM n° 221, de 17 de abril de 2008. Lista de condições sensíveis à atenção primária [Internet]. Diário Oficial da União, Brasília (DF), 2008 abr 18 [citado 2020 jul 15];Seção I:70. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/sas/2008/prt0221_17_04_2008.html [ Links ]
17. Firjan. Índice Firjan de Desenvolvimento Municipal [Internet]. [S.l.]: Firjan; 2019 [citado 2019 maio 01]. Disponível em: https://www.firjan.com.br/ifdm/destaques/brasil/ [ Links ]
18. Santana VL. Atraindo o Pork: que fatores explicam a execução das emendas orçamentárias no Brasil? [dissertação]. Brasília (DF): Universidade de Brasília; 2011. Disponível em: https://repositorio.unb.br/bitstream/10482/8702/1/2011_VitorLealSantana.pdf [ Links ]
19. Baião AL, Couto CG. A eficácia do pork barrel: a importância de emendas orçamentárias e prefeitos aliados na eleição de deputados. Opin Pública [Internet]. 2017 dez [citado 2020 jul 15];23(3):714-53. Disponível em: https://doi.org/10.1590/1807-01912017233714 [ Links ]
20. Ministério da Saúde (BR). Panorama nacional de implementação do Programa Academia da Saúde: monitoramento do programa academia da saúde, ciclo 2017 [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2019 maio 01]. 60 p. Disponível em: http://189.28.128.100/dab/docs/portaldab/documentos/pse/panorama_academia_saude_monitoramento_programa.pdf [ Links ]
21. Lotufo PA, Goulart AC, Passos VMA, Satake FM, Souza MFM, França EB, et al. Doença cerebrovascular no Brasil de 1990 a 2015: Global Burden of Disease 2015. Rev Bras Epidemiol [Internet]. 2017 May [citado 2019 abr 15];1 suppl 20:129-41. Disponível em: https://doi.org/10.1590/1980-5497201700050011 [ Links ]
22. Malta DC, Morais Neto OL, Silva Junior JB. Apresentação do plano de ações estratégicas para o enfrentamento das doenças crônicas não transmissíveis no Brasil, 2011 a 2022. Epidemiol Serv Saúde [Internet]. 2011 dez [citado 2019 abr 17];20(4):425-38. Disponível em: http://dx.doi.org/10.5123/S1679-49742011000400002 [ Links ]
23. Malta DC, Bernal RTI, Souza MFM, Szwarcwald CL, Lima MG, Barros MBA. Social inequalities in the prevalence of self-reported chronic non-communicable diseases in Brazil: national health survey 2013. Int J Equity Health [Internet]. 2016 Nov [cited 2019 May 13];15(1):153. Available from: https://doi.org/10.1186/s12939-016-0427-4 [ Links ]
24. Moutinho JA, Kniess CT. Transferências voluntárias como ferramentas para descentralização de políticas públicas: identificação de correlação entre variáveis. In: Anais do IV SINGEP e III S2IS [Internet]; 2015 nov 08-10; São Paulo. São Paulo: SINGEP; 2015 [citado 2019 maio 13]. Disponível em: https://singep.org.br/4singep/resultado/59.pdf [ Links ]
25. Brasil. Presidência da República. Lei Complementar n° 141, de 13 de janeiro de 2012. Regulamenta o § 3° do art. 198 da Constituição Federal para dispor sobre os valores mínimos a serem aplicados anualmente pela União, Estados, Distrito Federal e Municípios em ações e serviços públicos de saúde; estabelece os critérios de rateio dos recursos de transferências para a saúde e as normas de fiscalização, avaliação e controle das despesas com saúde nas 3 (três) esferas de governo; revoga dispositivos das Leis nos 8.080, de 19 de setembro de 1990, e 8.689, de 27 de julho de 1993; e dá outras providências [Internet]. Diário Oficial da União, Brasília (DF); 2012 jan 13 [citado 2020 jul 15]. Disponível em: http://www.planalto.gov.br/ccivil_03/leis/LCP/Lcp141.htm [ Links ]
26. Simão JB, Orellano VIF. Um estudo sobre a distribuição das transferências para o setor de saúde no Brasil. Estud Econ [Internet]. 2015 jan-mar [citado 2020 jul 15];45(1):33-63. Disponível em: https://doi.org/10.1590/0101-4161201545133jbv [ Links ]
27. Schmidt MI, Duncan BB, Silva GA, Menezes AM, Monteiro CA, Barreto SM, et al. Doenças crônicas não transmissíveis no Brasil: carga e desafios atuais. Lancet (Saúde Brasil) [Internet]. 2011 [citado 2020 jul 15];4:61-74. Disponível em: http://www.idec.org.br/pdf/schmidtetal_lancet2011.pdf [ Links ]
28. Almeida-Filho N. A problemática teórica da determinação social da saúde. In: Nogueira RP, organizador. Determinação social da saúde e reforma sanitária [Internet]. Rio de Janeiro: CEBES; 2010 [citado 2020 jul 15]. p. 13-36. Disponível em: http://renastonline.ensp.fiocruz.br/sites/default/files/arquivos/recursos/Determinação%20Social%20da%20Saúde%20e%20Reforma%20Sanitária.pdf [ Links ]
29. Amorim Neto O, Simonassi AG. Bases políticas das transferências intergovernamentais no Brasil (1985-2004). Rev Econ Polit [Internet]. 2013 out-dez [citado 2020 jul 15];33(4):704-25. Disponível em: http://dx.doi.org/10.1590/S0101-31572013000400010 [ Links ]
30. Baião AL, Cunha ASM, Souza FSRN. Papel das transferências intergovernamentais na equalização fiscal dos municípios brasileiros. Rev Serv Público [Internet]. 2017 set [citado 2020 jul 15];68(3):583-610. Disponível em: https://doi.org/10.21874/rsp.v68i3.1406 [ Links ]
Received: January 08, 2020; Accepted: June 03, 2020











 texto em
texto em