Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.5 Brasília 2020 Epub 19-Nov-2020
http://dx.doi.org/10.1590/s1679-49742020000500009
Original article
Characterization of notifications of exogenous pesticide poisoning in Rio Grande do Sul, Brazil, 2011-2018
1Escola de Saúde Pública do Rio Grande do Sul, Programa de Residência Integrada em Saúde com Ênfase em Vigilância em Saúde, Porto Alegre, RS, Brazil
2Secretaria de Estado da Saúde do Rio Grande do Sul, Centro Estadual de Vigilância em Saúde, Porto Alegre, RS, Brazil
Objective:
To describe the profile of exogenous pesticide poisoning notifications in Rio Grande do Sul, Brazil, from 2011 to 2018.
Methods:
This was a descriptive study of data retrieved from the Notifiable Health Conditions Information System. Sociodemographic, clinical and pesticide-related variables were included and presented in absolute and relative frequencies.
Results:
3,122 suspected cases of exogenous pesticide poisoning were reported. The main toxic agent was pesticide for agricultural use (60%). Spraying (42%) and dilution (18%) proved to be the activities with greatest pesticide exposure. Most pesticide poisoning occurred at home (59%), and accidental contamination (40%) was the main cause of poisoning. Most poisoning was of the acute single kind (82%) and clinical evaluation (61%) was the criterion most used for diagnosis.
Conclusion:
Most of records of exogenous pesticide poisoning in Rio Grande do Sul were related to its agricultural production model.
Keywords: Agrochemicals; Poisoning; Epidemiology, Descriptive; Information Systems
Introduction
Exogenous poisonings are pathologic manifestations caused by interaction between the biological system and toxic substances, and may occur through intake or contact of the toxic agent with skin, eyes or mucous membranes.1 Pesticides are substances developed to intervene in natural biological processes. They are toxic products extremely harmful to human health and the environment. Pesticides are involved in many cases of exogenous poisoning, principally in middle and low-income developing and/or emerging countries.2
Brazil is one of the world's main pesticide consumers. According to the Ministry of Agriculture, Livestock and Food Supply, between 2005 and mid 2019, 2,940 products classified as pesticides were registered.3 Agriculture is the sector that most uses these chemical compounds, as well as Public Health itself for controlling disease vectors, veterinary medicine and the household environment, especially for controlling insects and infestations.4
In Rio Grande do Sul, farming and livestock activities are of great relevance for the economy. The predominant agricultural model is conventional, agrochemical and based on monoculture plantations. It uses a large volume of pesticides and is one of the leading states in terms of pesticide commercialization in Brazil.5 This extensive use of pesticides in the rural production system increases not only worker exposure to toxic agents, but also exposure of the population, through contaminated water, soil, air and food.6
Among the main objectives of exogenous pesticide poisoning health surveillance is the reduction of its morbidity and mortality among exposed populations, through actions to promote and protect health and prevent illness. Notification of cases exposed to toxic agents enables monitoring of the occurrence of these health conditions in order to plan strategic control actions.7 Notwithstanding, there is a scarcity of recent studies that include factors related to human exposure to pesticides in Rio Grande do Sul capable of informing health surveillance actions.
The objective of this study was to describe the profile of notifications of exogenous pesticide poisoning in Rio Grande do Sul between 2011 and 2018.
Methods
This is a descriptive study analyzing secondary data on exogenous pesticide poisoning in the state of Rio Grande do Sul, Brazil, between 2011 and 2018.
Rio Grande do Sul has over 11 million inhabitants distributed over 497 municipalities. The state is located in Southern Brazil and covers an area of 281,707.151km.2,8 The greater part of its economy is based on agriculture and livestock. In 2014, Rio Grande do Sul was in fifth place among the Brazilian states in terms of pesticide commercialization and pesticide poisoning lethality, with 3.77 cases per 100,000 inhab., this being above the annual national rate.9
The Ministry of Health added exogenous poisoning (including pesticide poisoning) to the list of compulsorily notifiable health conditions by means of Ministerial Ordinance No. GM/MS 2472, dated August 31st 2010, making it obligatory to record all suspected cases of pesticide poisoning on the Notifiable Health Conditions Information System (SINAN). Notification must be made of any suspected case, defined as any person who has been exposed to chemical substances, has clinical signs and symptoms of poisoning and/or probably or possibly compatible laboratory test results.10
The Tabnet computer program was used to collect the data. It is a generic tabulator devised by the Ministry of Health National Health System Information Technology Department (DATASUS), which provides public data based on SINAN system exogenous poisoning data. The data are generated through exogenous poisoning investigation forms input to SINAN by Municipal Health Departments, with data unification at state level and consolidation in a national database. Data tabulation using this database was performed by selecting records of suspected cases of exogenous poisoning in which the toxic agent involved was classified as belonging to any one of the following five pesticide groups (pesticide for agricultural use; pesticide for domestic use; pesticide for Public Health use; veterinary product; rodenticide). We analyzed cases occurring in Rio Grande do Sul between January 1st 2011 and December 31st 2018. All the data were retrieved on July 27th 2019 (updated on SINAN on July 25th 2019) from the following web page: http://200.198.173.165/scripts/deftohtm.exe?snet/iexogrs.
The following variables were assessed:
-
Sociodemographic variables
age range (in years: under 10; 10-19; 20-39; 40-59; 60 or over);
sex (male; female);
race/skin color (white; black; yellow; brown; indigenous);
schooling (no schooling; grade 1 to 4, incomplete; grade 4, complete; grade 5 to 8, incomplete; complete elementary education; incomplete high school education; complete high school education; incomplete higher education; complete higher education; not applicable).
-
Variables related to pesticide exposure
place of occurrence (residence; work environment; outside environment; other);
exposure zone (urban; rural; peri-urban);
toxic agent group (general classification) involved in poisoning (agricultural pesticide; pesticide for domestic use; pesticide for Public Health use; rodenticide; veterinary product);
purpose of pesticide use (insecticide; herbicide; bug spray; rodenticide; fungicide; wood preserver; other);
activity involving current exposure to pesticide (dilution; spraying; seed treatment; storage; crop growing; transportation; insect control; production; other; not applicable);
circumstances of pesticide exposure/contamination (normal use; accidental; environmental; suicide attempt; other [therapeutic use, inappropriate medical prescription, administrative error, self-medication, abuse, food or drink intake, attempted abortion, violence, homicide or other described circumstance]);
type of exposure (acute-single; acute-repetitive; chronic; acute on top of chronic).
Poisoning confirmation criterion (laboratory; clinical-epidemiological; clinical)
Month of occurrence of poisoning
Variable completeness and absolute and relative frequencies (%) were calculated using Microsoft Office Excel® version 2007.
The notification rate for each year studied (2011-2018) was calculated by dividing the total number of exogenous pesticide poisoning notifications in Rio Grande do Sul by the resident population expressed per 100,000 inhab. The population data on Rio Grande do Sul were obtained from intercensal estimates made by the Brazilian Institute of Geography and Statistics and used by the Federal Audit Court.
The study was conducted using secondary data only, with no identification of the people involved and obtained from a public domain database. As such, submission to a Research Ethics Committee was not necessary
Results
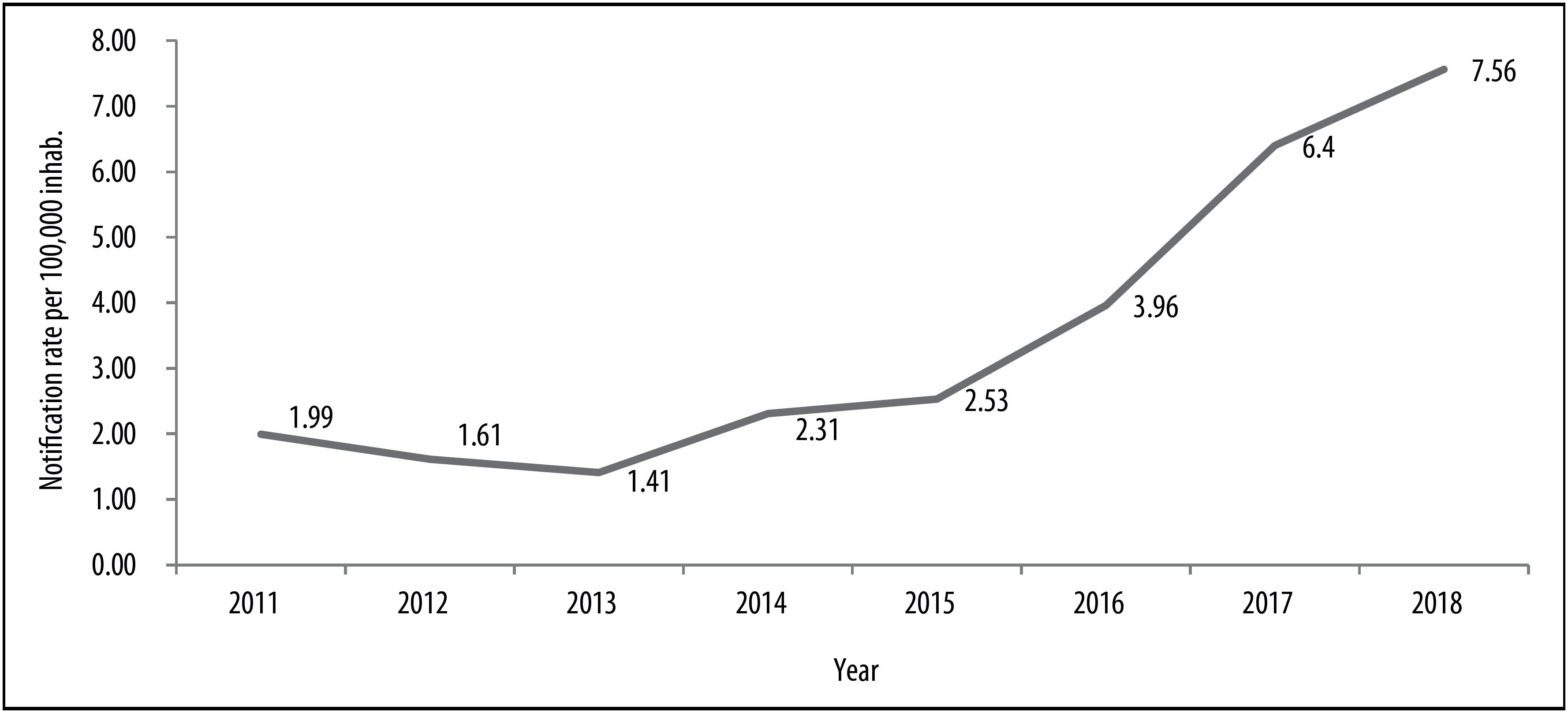
In the period 2011-2018, 3,122 suspected cases of exogenous pesticide poisoning were notified Rio Grande do Sul. Figure 1 shows the increase in pesticide poisoning notification incidence over the years, with a noticeable increase with effect from 2015. The highest notification rate was found in 2018: 7.56 cases per 100,000 inhab.
Completeness of information with regard to the variables analyzed varied between 66% and 100%. The majority of cases were male (1,987; 64%), while the 20-49 year age range was most frequent, corresponding to 56% of cases (1,740). With regard to race/skin color, White individuals accounted for 87% of notifications (2,574). In relation to schooling, people who had studied up to the 5th to 8th grade were most frequent, accounting for 23% (524); 1.5% of cases had no schooling (Table 1).
Table 1 Distribution of the sociodemographic characteristics of notified cases of exogenous pesticide poisoning, Rio Grande do Sul, 2011-2018
| Sociodemographic characteristics | n | % | |
|---|---|---|---|
| Age range, in years (n=3,122) | |||
| <10 | 345 | 11.0 | |
| 10-19 | 253 | 8.1 | |
| 20-29 | 633 | 20.3 | |
| 30-39 | 558 | 17.9 | |
| 40-49 | 549 | 17.6 | |
| 50-59 | 466 | 14.9 | |
| ≥60 | 318 | 10.2 | |
| Sex (n=3,121)a | |||
| Male | 1,987 | 63.7 | |
| Female | 1,134 | 36.3 | |
| Race/skin color (n=2,961)a | |||
| White | 2,574 | 86.9 | |
| Black | 121 | 4.1 | |
| Yellow | 4 | 0.2 | |
| Brown | 249 | 8.4 | |
| Indigenous | 13 | 0.4 | |
| Schooling (n=2,263)a | |||
| No schooling | 34 | 1.5 | |
| Grade 1 to 4, incomplete | 318 | 14.0 | |
| Grade 4, complete | 193 | 8.5 | |
| grade 5 to 8, incomplete | 524 | 23.2 | |
| Complete elementary education | 237 | 10.5 | |
| Incomplete high school education | 212 | 9.4 | |
| Complete high school education | 314 | 13.9 | |
| Incomplete higher education | 45 | 2.0 | |
| Complete higher education | 53 | 2.3 | |
| Not applicable | 333 | 14.7 | |
a)Variables for which fields filled in as ‘unknown’ were excluded from the frequency calculation.
Most records occurred in the summer (Figure 2). When comparing case occurrence in June and July (winter) with occurrences in December alone (summer), the number of records in December was almost four times greater.
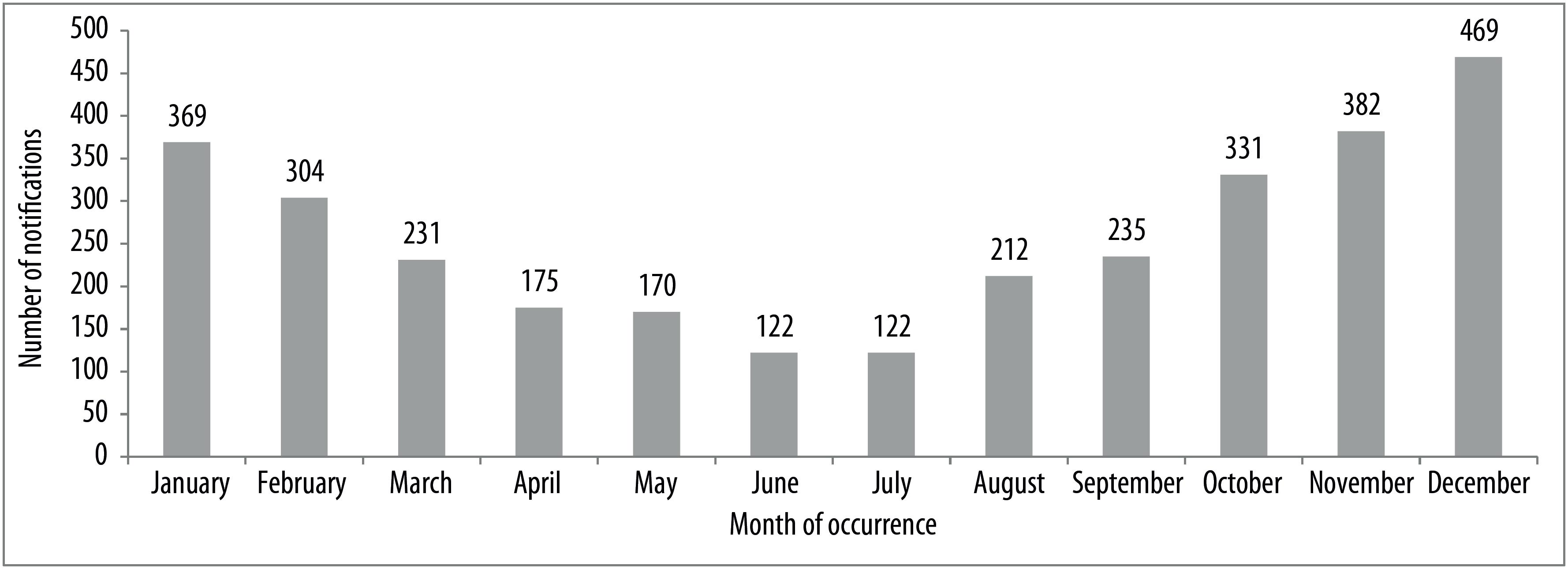
Figure 2 Distribution of notifications of exogenous pesticide poisoning by month of occurrence, Rio Grande do Sul, 2011-2018
In Table 2 it can be seen that a large number of records reported the toxic agent as being substances classified as ‘pesticide for agricultural use’, corresponding to approximately 60% (1,860) of total cases investigated. The main toxic agent involving children under 10 years old was rodenticide, accounting for 51% of cases (176). With regard to the purpose for which pesticides were used, more than a third (36%) of the records were incomplete. Notwithstanding, herbicides (47%; 936) and insecticides (36%; 731) were the main classes of pesticides related to exogenous poisoning. Spraying (42%; 860) and dilution (18%; 374) were the main activities involving pesticide use in suspected cases of poisoning.
Table 2 Distribution of the characteristics of the toxic agent involved in notified cases of exogenous pesticide poisoning, Rio Grande do Sul, 2011-2018
| Toxic agent characteristics | Total cases (3,222) | Children <10 years (345) | |||
|---|---|---|---|---|---|
| Toxic agent | n | % | n | % | |
| Pesticide for agricultural use | 1,860 | 59.6 | 48 | 13.9 | |
| Pesticide for domestic use | 375 | 12.0 | 62 | 18.0 | |
| Pesticide for Public Health use | 68 | 2.2 | 1 | 0.3 | |
| Rodenticide | 545 | 17.4 | 176 | 51.0 | |
| Product for veterinary use | 274 | 8.8 | 58 | 16.8 | |
| Purpose of use (2,010)a | n | % | |||
| Insecticide | 731 | 36.4 | |||
| Herbicide | 936 | 46.6 | |||
| Bug spray | 34 | 1.7 | |||
| Rodenticide | 14 | 0.7 | |||
| Fungicide | 149 | 7.4 | |||
| Wood preserver | 1 | 0.0 | |||
| Other | 129 | 6.4 | |||
| Not applicable | 16 | 0.8 | |||
| Exposure activity (2,071)a | n | % | |||
| Dilution | 374 | 18.1 | |||
| Spraying | 860 | 41.5 | |||
| Seed treatment | 65 | 3.1 | |||
| Storage | 29 | 1.4 | |||
| Crop growing | 236 | 11.4 | |||
| Transportation | 22 | 1.1 | |||
| Insect control | 127 | 6.1 | |||
| Production | 14 | 0.7 | |||
| Other | 213 | 10.3 | |||
| Not applicable | 131 | 6.3 | |||
a)Variables for which fields filled in as ‘unknown’ were excluded from the frequency calculation.
With regard to the place where poisoning occurred, the highest frequencies were found at home and in the work environment, accounting for 59% (1,785) and 34% (1,021), respectively (Table 3). In relation to the circumstances in which pesticide contamination occurred, accidental poisoning (40%; 1,230) and suicide attempts (26%; 801) stood out. The majority of notifications were attributed to acute-single poisoning (82%; 2,387), i.e. arising from just one exposure.
Table 3 Distribution of notifications of exogenous pesticide poisoning according to contamination circumstances, type of exposure and confirmation criterion, Rio Grande do Sul, 2011-2018
| Variable | n | % | |
|---|---|---|---|
| Place of occurrence (n=3,027)a | |||
| Residence | 1,785 | 59.0 | |
| Work environment | 1,021 | 33.7 | |
| Outside environment | 120 | 4.0 | |
| Other | 101 | 3.3 | |
| Exposure zone (n=2,727)a | |||
| Urban | 1,286 | 47.2 | |
| Rural | 1,410 | 51.7 | |
| Peri-urban | 31 | 1.1 | |
| Contamination (n=3,065)a | |||
| Normal use | 588 | 19.2 | |
| Accidental | 1,230 | 40.1 | |
| Environmental | 262 | 8.6 | |
| Suicide attempt | 801 | 26.1 | |
| Other | 184 | 6.0 | |
| Type of exposure (n=2,917)a | |||
| Acute-single | 2,387 | 81.8 | |
| Acute-repetitive | 423 | 14.5 | |
| Chronic | 78 | 2.7 | |
| Acute on top of chronic | 29 | 1.0 | |
| Confirmation criterion (n=2,799)a | |||
| Clinical-laboratory | 226 | 8.1 | |
| Clinical-epidemiological | 868 | 31.0 | |
| Clinical | 1,705 | 60.9 | |
a)Variables for which fields filled in as ‘unknown’ were excluded from the frequency calculation.
Discussion
An increase in pesticide poisoning notifications on the SINAN system was found for Rio Grande do Sul between 2011 and 2018, with a sharp increase with effect from 2015. Records of pesticide poisoning were predominant among males, economically active adults, involving agricultural pesticides (herbicides and insecticides) and as a result of occupational activities.
The increase in records of pesticide poisoning may be associated with the increase in the commercialization of these substances in Rio Grande do Sul, as well as the increase in health surveillance actions to ensure recording in this area. In 2018, Rio Grande do Sul was in third place among all the 27 Brazilian states in terms of crop growing areas, with 9,071,056 hectares used for this purpose.11 Despite such a large area used for agriculture, in 2014 Rio Grande do Sul was in 21st place with regard to pesticide poisoning notification, suggesting underreporting.12 The current scenario continues to be of concern, since according to World Health Organization estimates, only one in fifty pesticide poisoning cases is notified.13
With the aim of raising the awareness of health workers to recognize and notify pesticide poisoning cases in Rio Grande do Sul, a Technical Group on Pesticides was created in 2015 within the State Health Surveillance Center, with the purpose of discussing, preparing and proposing actions for the State Program for Health Surveillance of Populations Exposed to Pesticides (State Ordinance No. 514, dated April 20th 2015).14
Distribution of pesticide poisoning notifications over the months of the year coincides with the seasonality of the main crops produced in Rio Grande do Sul: soy beans, maize and rice. These crops adapt best to hotter months and, consequently, are subject to greater pesticide application on a large scale in extensive monoculture plantations.15 On the other hand, the winter months usually comprise the off-season period, with fewer insects due to the cold, resulting in reduced use of pesticides classified as insecticides.
Pesticide spraying and dilution were the exposure activities with greatest risk of poisoning. Both activities facilitate greater contact with pesticides, possibly made worse by lack of technical guidance, lack of information about correct use of these products and lack of use of personal protective equipment (PPE). A study that assessed work safety procedures among workers on small and medium-sized farms in the municipality of Araras in São Paulo state, demonstrated that 22% of farm workers did not use any kind of PPE, proving the need to increase information among farm workers about the health problems to which they are exposed in their work environment and the importance of using PPE as a prevention measure.16
The majority of notified poisonings occurred at home, followed by the work environment, suggesting the existence of problems with pesticide storage and not complying with the minimum recommended distance between crops and housing when applying pesticides. It is common for small-scale farmers to store their supplies, including pesticides, in sheds near to their homes or even inside their homes. Moreover, Agostinetto et al. conclude that there can be ‘drift’ depending on wind speed when pesticides are applied, this being one of the main circumstances in which those applying pesticides are poisoned and nearby environments are contaminated. Hence the importance of keeping a minimum distance between plantations and houses so as to avoid this form of harm.17 Monquero et al. demonstrated that the houses of those who applied pesticides on small and medium-sized farms were very close to plantations: in 75% of cases this distance was less than 50 meters.14 Moreover, pesticides are kept inside homes, whether in urban or rural areas, to be used as insecticides, rodenticides and products intended for treatment of nits and other parasites, increasing even more the risk of poisoning in the domestic environment.
Children having easy access to places where pesticides are stored, inadequate handling and failure to use PPE are among the factors contributing to the occurrence of accidental poisoning.18 Moreover, reuse of pesticide packaging is one of the factors that contributes to accidental poisoning.18
Suicide attempts were the second leading cause of pesticide poisoning in Rio Grande do Sul in the period studied. Scientific evidence associates exposure to insecticides, especially organophosphates, with symptoms of anxiety and depression.19,20 In the study they conducted in the municipalities of Antônio Prado and Ypê, both in Rio Grande do Sul, Faria et al. found high prevalence of minor psychiatric disorders among rural workers who made intensive use of pesticides.21 In relation to this, Bombardi added the hypothesis of a relationship between suicide and financial indebtedness of farm workers due to the cost of buying pesticide, exerting psychological pressure on them to the point of their attempting suicide.22
Most cases of pesticide poisoning recorded in Rio Grande do Sul were of the acute type, i.e. when symptoms appear immediately following excessive contact with the toxic agent. In these cases, seeking emergency health services to relief the symptoms is more likely. This does not occur in chronic cases, when clinical pictures are undefined, unspecific, subtle, take a long time to develop, are often irreversible, and may manifest themselves in the form of different illnesses over the course of time.10
Despite the cause-effect relationship being more visible in cases of acute poisoning, diagnosis still has shortcomings and for the most part is based on clinical signs and symptoms presented, as well as prior history. There are huge limitations to confirming pesticide poisoning diagnosis with laboratory tests, which would help in prescribing more specific treatment. There are no biomarkers available for the main substances used in farming. Laboratory diagnosis is only available in health services for the organophosphate and carbamate chemical group, by means of plasma and/or erythrocyte cholinesterase tests, the result of which is strongly influenced by exposure to alcohol, other drugs, comorbidities and liver diseases; furthermore, specific laboratory diagnosis for this chemical group is only indicated for recent exposure.23,24
Among this study's limitations, underreporting is one of the weaknesses of information systems, and achieving satisfactory completeness of SINAN notification form fields is an objective that has yet to be met, thus hindering a more fruitful analysis of the records. Moreover, the results presented do not express the true dimension of the problem, as records of chronic poisoning cases are scarce, given the lack of knowledge and difficult diagnosis.
In Rio Grande do Sul, the majority of pesticide poisoning notifications are related to the indiscriminate and widespread use of these products, in view of the strength of agribusiness in the state, which mainly affects rural workers directly involved in their use. As control of exposure is not an exclusive attribute of the Health sector, control actions should always be articulated with society in general and, especially, with the other sectors involved, in order for them to be more effective. Likewise, a sustainable model of agriculture and development should be sought.
Referências
1. Romão MR, Vieira LJES. Tentativas suicidas por envenenamento. Rev Bras Promoção Saúde [Internet]. 2004 [citado 2020 ago 29];17(1):14-20. Disponível em: https://periodicos.unifor.br/RBPS/article/download/340/2039 [ Links ]
2. International Labor Organization - ILO. World day for safety and health at work: a background paper. In: Focus programme on safework [Internet]. Geneva: International Labour Office; World Health Organization; 2005 [cited 2020 Aug 29]. Available from: https://www.who.int/occupational_health/mediacentre/pr280405/en/ [ Links ]
3. Ministério da Agricultura, Pecuária e Abastecimento – MAPA (BR). Informações técnicas: registro concedido de 2005 a 2019 [Internet]. Brasília: MAPA; 2019 [citado 2019 jul 10]. Disponível em: http://www.agricultura.gov.br/assuntos/insumos-agropecuarios/insumos-agricolas/agrotoxicos/informacoes-tecnicas [ Links ]
4. Cassal VB, Azevedo LF, Ferreira RP, Silva DG, Simão RS. Agrotóxicos: uma revisão de suas consequências para a saúde pública. REGET [Internet]. 2014 abr [citado 2020 ago 29];18(1):437-45. Disponível em: https://doi.org/10.5902/2236117012498 [ Links ]
5. Ervilha IC. Relatório: vigilância em saúde de populações expostas a agrotóxicos no estado do Rio Grande do Sul [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2020 ago 29]. 13 p. Disponível em: http://www.saude.gov.br/images/pdf/2015/julho/08/Relat--rio-Rio-Grande-do-Sul.pdf [ Links ]
6. Moreira JC, Jacob SC, Peres F, Lima JS, Meyer A, Oliveira-Silva JJ, et al. Avaliação integrada do impacto do uso de agrotóxicos sobre a saúde humana em uma comunidade agrícola de Nova Friburgo, RJ. Ciênc Saúde Coletiva [Internet]. 2002 [citado 2020 ago 29];7(2):299-311. Disponível em: http://dx.doi.org/10.1590/S1413-81232002000200010 [ Links ]
7. Ministério da Saúde (BR). Relatório: vigilância em saúde de populações expostas a agrotóxicos no estado do Rio Grande do Sul [Internet]. Brasília: Ministério da Saúde; 2015 [citado 2019 dez 10]. 13 p. Disponível em: https://portalarquivos2.saude.gov.br/images/pdf/2015/julho/08/Relat--rio-Rio-Grande-do-Sul.pdf [ Links ]
8. Instituto Brasileiro de Geografia e Estatística - IBGE. Panorama Rio Grande do Sul [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2019 [citado 2020 fev 23]. Disponível em: https://cidades.ibge.gov.br/brasil/rs/panorama [ Links ]
9. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância em Saúde Ambiental e Saúde do Trabalhador. Relatório nacional de vigilância em saúde de populações expostas a agrotóxicos [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2019 jun 15]. 191 p. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/relatorio_nacional_vigilancia_populacoes_expostas_agrotoxicos.pdf [ Links ]
10. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância em Saúde Ambiental e Saúde do Trabalhador. Diretrizes nacionais para a vigilância em saúde das populações expostas a agrotóxicos [Internet]. Brasília: Ministério da Saúde; 2017 [citado 2019 jul 21]. 28 p. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/diretrizes_vigilancia_populacoes_expostas_agrotoxicos.pdf [ Links ]
11. Instituto Brasileiro de Geografia e Estatística - IBGE. Área plantada ou destinada à colheita, área colhida, quantidade produzida, rendimento médio e valor da produção das lavouras temporárias e permanentes [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2018 [citado 2020 fev 04]. Disponível em: https://sidra.ibge.gov.br/tabela/5457 [ Links ]
12. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância em Saúde Ambiental e Saúde do Trabalhador. Agrotóxicos na ótica do Sistema Único de Saúde [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2020 ago 29]. 248 p. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/agrotoxicos_otica_sistema_unico_saude_v2.pdf [ Links ]
13. Carneiro FF, Augusto LGS, Rigotto, RM, Friedrich K, Burigó AC. Dossiê ABRASCO: um alerta sobre os impactos dos agrotóxicos na saúde [Internet]. Rio de Janeiro: ABRASCO; 2015 [citado 2020 ago 29]. Disponível em: https://www.abrasco.org.br/site/noticias/institucional/dossie-abrasco-um-alerta-sobre-os-impactos-dos-agrotoxicos-na-saude/9898/ [ Links ]
14. Rio Grande do Sul. Secretaria de Saúde. Portaria n° 514, de 20 de abril de 2015 [Internet]. Porto Alegre: Secretaria de Saúde; 2015 [citado 2019 ago 2]. Disponível em: https://saude.rs.gov.br/upload/arquivos/carga20170441/13054141-1448285820-514-20cevs.pdf [ Links ]
15. Manosso FC. A produtividade de soja, trigo e milho e suas relações com a precipitação pluviométrica no município de Apucarana-PR no período de 1968 a 2002. Geografia [Internet]. 2005 jan-jun [citado 2020 ago 29]:14(1):87-98. Disponível em: http://dx.doi.org/10.5433/2447-1747.2005v14n1p87 [ Links ]
16. Monquero PA, Inácio EM, Silva AC. Levantamento de agrotóxicos e utilização de equipamento de proteção individual entre os agricultores da região de Araras. Arq Inst Biol [Internet]. 2009 jan-mar [citado 2020 ago 29];76(1):135-9. Disponível em: http://www.biologico.sp.gov.br/uploads/docs/arq/v76_1/monquero.pdf [ Links ]
17. Agostinetto D, Puchalki LEA, Azevedo R, Storch G, Bezerra AJA, Grützmacher AD. Utilização de equipamentos de proteção individual e intoxicação por agrotóxicos entre fumicultores do Município de Pelotas-RS. Pesticidas: R Ecotoxicol Meio Ambiente [Internet]. 1998 jan-dez [citado 2020 ago 29];8:45-56. Disponível em: http://dx.doi.org/10.5380/pes.v8i0.39515 [ Links ]
18. Queiroz PR, Lima KC, Oliveira TC, Santos MM, Jacob JF, Oliveira AMBM. Sistema de Informação de Agravos de Notificação e as intoxicações humanas por agrotóxicos no Brasil. Rev Bras Epidemiol [Internet]. 2019 abr [citado 2020 ago 29];22:e190033. Disponível em: http://dx.doi.org/10.1590/1980-549720190033 [ Links ]
19. Rehner TA, Kolbo JR, Trump R, Smith C, Reid D. Depression among victims of south Mississippi's methyl parathion disaster. Health Soc Work [Internet]. 2000 Feb [cited 2020 Aug 29];25(1):33-40. Available from: https://doi.org/10.1093/hsw/25.1.33 [ Links ]
20. Stallones L, Beseler C. Pesticide poisoning and depressive symptoms among farm residents. Ann Epidemiol [Internet]. 2002 Aug [cited 2020 Aug 2020];12(6):389-94. Available from: https://doi.org/10.1016/s1047-2797(01)00298-8 [ Links ]
21. Faria NMX, Facchini LA, Fassa ACG, Tomasi E. Processo de produção rural e saúde na serra gaúcha: um estudo descritivo. Cad Saúde Pública [Internet]. 2000 jan-mar [citado 2020 ago 29];16(1):115-28. Disponível em: https://doi.org/10.1590/S0102-311X2000000100012 [ Links ]
22. Bombardi LM. A intoxicação por agrotóxicos no Brasil e a violação dos direitos humanos. In: Merlino T, Mendonça ML, editores. Direitos humanos no Brasil 2011: relatório da rede social de justiça e direitos humanos [Internet]. São Paulo: Rede Social de Justiça e Direitos Humanos; 2011 [citado 2020 ago 29]. p. 71-84. Disponível em: https://www.social.org.br/DH_2011_ALTA.pdf [ Links ]
23. Faria NMX, Fassa AG, Facchini LA. Intoxicação por agrotóxicos no Brasil: os sistemas oficiais de informação e desafios para a realização de estudos epidemiológicos. Ciênc Saúde Coletiva [Internet]. 2007 jan-mar [citado 2020 ago 29];12(1):25-38. Disponível em: https://doi.org/10.1590/S1413-81232007000100008 [ Links ]
24. Soares W, Almeida RM, Moro S. Trabalho rural e fatores de risco associados ao regime de uso de agrotóxicos em Minas Gerais, Brasil. Cad Saúde Pública [Internet]. 2003 ago [citado 2020 ago 29]; 19(4):1117-27. Disponível em: https://doi.org/10.1590/S0102-311X2003000400033 [ Links ]
Received: March 27, 2020; Accepted: July 28, 2020











 texto em
texto em