Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.5 Brasília 2020 Epub 21-Sep-2020
http://dx.doi.org/10.1590/s1679-49742020000500011
Research Note
Description of COVID-19 hospitalized health worker cases in the first nine weeks of the pandemic, Brazil, 2020
1Ministério da Saúde, Secretaria de Vigilância em Saúde, Brasília, DF, Brazil
Methods:
This was a descriptive case series study; it included cases that became ill between February 21st and April 15th, 2020 registered on the Influenza Surveillance Information System (SIVEP-Gripe, acronym in Portuguese).
Results:
Of the 184 cases, 110 (59.8%) were female and median age was 44 years (min-max: 23-85); 89 (48.4%) were nursing professionals and 50 (27.2%) were doctors. Ninety-two (50.0%) presented comorbidity, with heart disease predominating (n=37; 40.2%). Of the 112 professionals with a record of case progression, 85 (75.9%) were cured and 27 (24.1%) died, 18 of whom were male.
Conclusion:
The profile of COVID-19 hospitalized health workers is similar to that of the general population with regard to age and comorbidities, but different in relation to sex. The most affected areas were nursing and medicine.
Keywords: Health Personnel; Coronavirus Infections; Health Profile; Epidemiology; Descriptive
Introduction
As at April 16th 2020, the world had recorded over two million COVID-19 cases and 156,141 deaths.1 The emergence of the disease and the resulting global health crisis increased demand for health care services and, consequently, health worker exposure to SARS-CoV-2 infection.2
Addressing the disease gives rise to diverse occupational risk situations: repeated exposure to the pathogen; long working hours, associated with multiple employment relationships; fatigue; occupational stress; stigmatization; physical and psychological violence;3 incipient training and insufficient/unavailable personal protective equipment (PPE).4
The clinical spectrum of COVID-19 infection ranges from asymptomatic infection or mild flu-like syndromes, to more severe respiratory conditions, such as severe acute respiratory syndrome (SARS), depending on the person’s constitution and comorbidities they may have. Brazil has a surveillance system for respiratory virus infections that aims to identify, record and monitor the clinical and epidemiological characteristics of these cases.5
Describing the profile of the profile of health workers hospitalized due to novel coronavirus infection in Brazil may inform actions to prevent and control this disease in this population which is so essential for addressing the pandemic.
The objective of this study was to describe COVID-19 hospitalized health worker cases in Brazil.
Methods
This is a descriptive study of cases hospitalized due to SARS, and with COVID-19 confirmed by real-time polymerase chain reaction testing (RT-PCR).
The Brazilian population is estimated to be 212 million people in 2020,6 and in January 2020 there were 1,535,523 health professionals working in Brazil,7 distributed among some 219,000 public and private health services.8
The study included as its participants health workers identified by the ‘occupation’ and ‘observations’ variable, classified according to the categories contained in Ministry of Health Ordinance MS/GM 639, dated March 31st de 2020, which provides for the Strategic Action entitled ‘Brazil can count on me – Health Workers’ (‘O Brasil conta comigo – Profissionais de Saúde’).9
The source used was the Influenza Surveillance Information System (SIVEP-Gripe). Its public domain data are available on the Ministry of Health electronic portal (https://covid.saude.gov.br/) and the data for the study were retrieved on April 28th 2020.
The study used the concept of the Epidemiological Week (EW), a form of international standardization of weeks from Sunday to Saturday, starting with the first week with most days in January and ending with the last week with most days in December. The study covered EW 8 to EW 17, 2020.
The variables studied were:
a) date of symptom onset;
b) Federative Unit of residence;
c) age (in years: 23-29; 30-39; 40-49; 50-59; 60 or over);
d) sex (female; male; unknown);
f) race/skin color (white; black; yellow; brown; indigenous; unknown);
g) presence (no; yes; unknown) of comorbidities (heart disease; asthma; diabetes mellitus; obesity);
h) signs and symptoms (fever; cough; sore throat; dyspnea; breathing difficulty; low saturation; diarrhea; vomiting; other);
i) disease progression (cure; death; unknown);
j) date of admission to hospital;
k) date of admission to an intensive therapy unit (ITU);
l) chest x-ray (normal; interstitial infiltrate; consolidation; mixed; other; not performed; unknown); and
m) use of ventilatory support (yes, invasive; yes, non-invasive; no; unknown)
It should be noted that the ‘occupation’ variable was added to the SIVEP-Gripe system on March 31st 2020.
The analyses were performed by calculating measurements of absolute and relative frequency, central tendency and dispersion, with the aid of the Microsoft Excel®, Epi Info 7.2 and QGIS 2.18 computer programs.
The study was conducted using only public-access secondary data with no personal identification of cases.
Results
During the period analyzed, 15,317 cases hospitalized due to SARS were confirmed as having COVID-19 in Brazil. Occupation was recorded for 379 (2.5%) of these cases, 184 (1.2%) of whom were health workers. The first health worker case became ill on March 2nd during EW 10. Most health workers became ill in EW 13 (Figure 1).
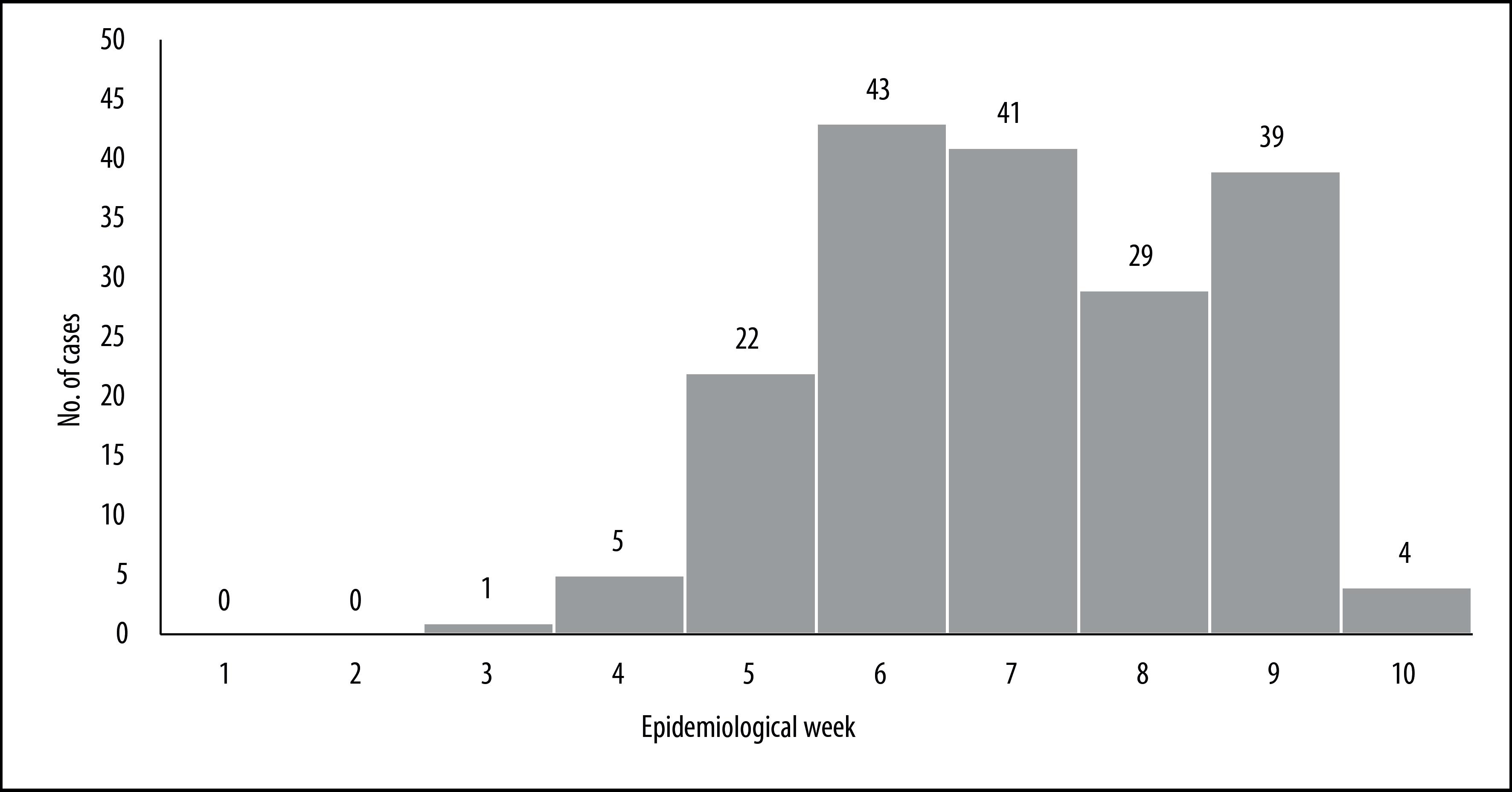
Figure 1 Distribution of health worker cases (N=184) hospitalized due to severe acute respiratory syndrome and confirmed as having COVID-19, by epidemiological week of symptom onset, Brazil, 2020
The Federative Units with most health workers hospitalized with COVID-19 were São Paulo (n=101; 54.9%), Amazonas (n=15; 8.2%) and Santa Catarina (n=13; 7.1%) (Figure 2).
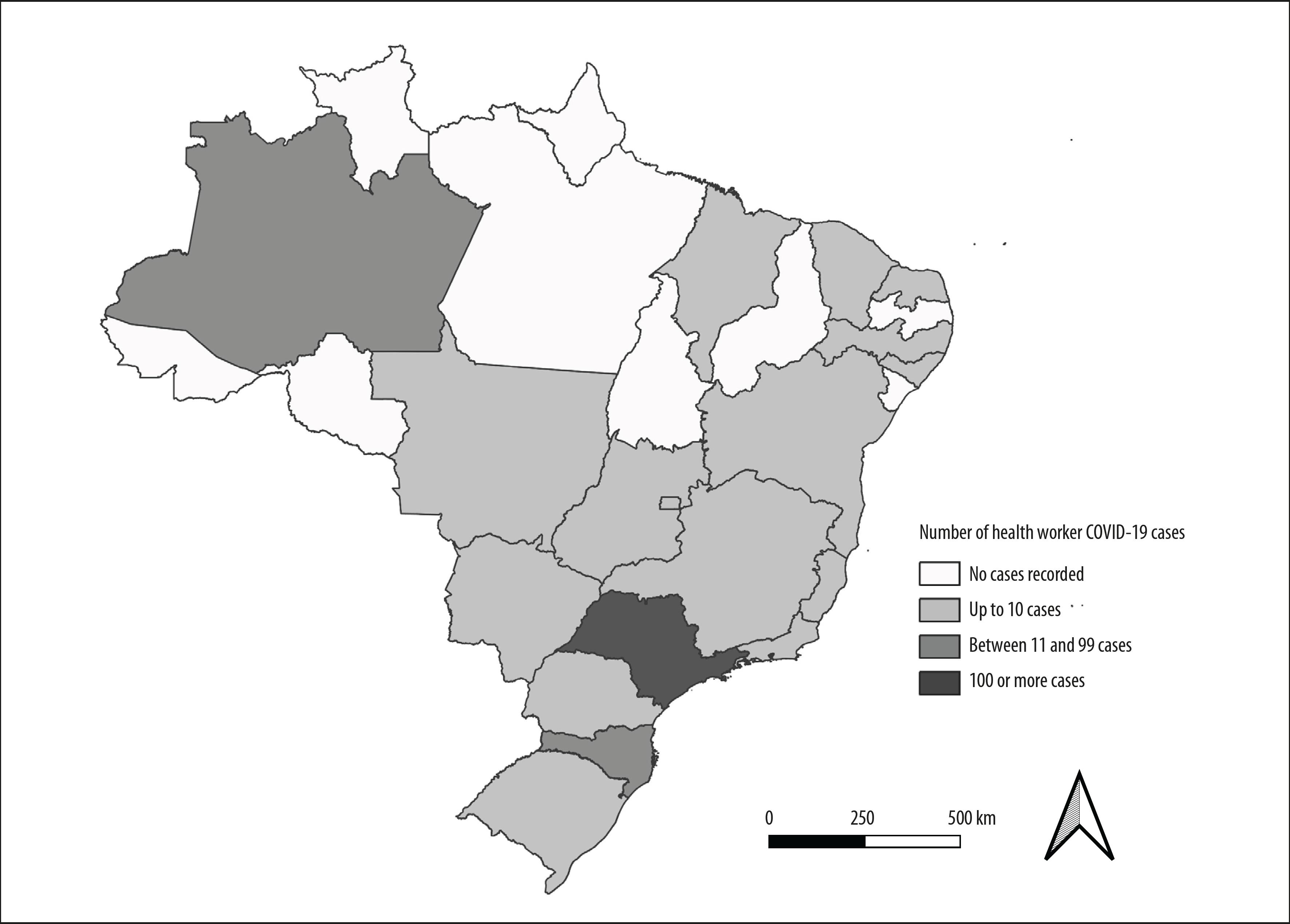
Figure 2 Distribution of health worker cases (N=184) hospitalized due to severe acute respiratory syndrome and confirmed as having COVID-19, by Federative Unit of notification, Brazil, 2020
Median age of ill health workers was 44 years (variation: 23 to 85), with greater concentration in the 30-49 years (n=113; 61.4%). Females (n=110; 59.8%) and White race/skin color (n=74; 40.2%) were predominant. Information with regard to race/skin color was blank/unknown for 67 cases (36.4%). Half the hospitalized health workers (n=92) had comorbidities, 37 of whom had heart disease (including hypertension), 24 had diabetes and 16 had asthma.
Nursing (n=89; 48.4%) and medicine (n=50; 27.2%) were the main affected occupation areas. A further 29 (15.8%) cases were only recorded as ‘health workers’ (Table 1).
Table 1 Absolute and relative frequencies of health worker cases (N=184) hospitalized due to severe acute respiratory syndrome and confirmed as having COVID-19, according to sociodemographic variables, Brazil, 2020
| Sociodemographic variables | N | % | ||
|---|---|---|---|---|
| Sex | ||||
| Female | 110 | 59.8 | ||
| Male | 74 | 40.2 | ||
| Age group (years) | ||||
| 23-29 | 7 | 3.8 | ||
| 30-39 | 52 | 28.3 | ||
| 40-49 | 61 | 33.1 | ||
| 50-59 | 38 | 20.7 | ||
| ≥60 | 26 | 14.1 | ||
| Race/skin color | ||||
| White | 74 | 40.2 | ||
| Black | 8 | 4.4 | ||
| Brown | 32 | 17.4 | ||
| Indigenous | 1 | 0.5 | ||
| Yellow | 2 | 1.1 | ||
| Blank/Unknown | 67 | 36.4 | ||
| Comorbidities | 92 | 50.0 | ||
| Heart disease (including arterial hypertension) | 37 | 40.2 | ||
| Diabetes mellitus | 24 | 64.9 | ||
| Asthma | 16 | 66.7 | ||
| Obesity | 11 | 68.8 | ||
| Lung diseases | 4 | 36.4 | ||
| Immunodepression | 3 | 75.0 | ||
| Occupational area | ||||
| Nursing | 89 | 48.4 | ||
| Nursing technician | 47 | 52.8 | ||
| Nurse | 33 | 37.1 | ||
| Nursing auxiliary | 9 | 10.1 | ||
| Medicine | 50 | 27.2 | ||
| Dentistry | 4 | 2.2 | ||
| Veterinary medicine | 1 | 0.5 | ||
| Physiotherapy | 2 | 1.1 | ||
| Biomedicine | 5 | 2.7 | ||
| Pharmacy | 4 | 2.2 | ||
| Health workera | 29 | 15.7 | ||
aThose for whom occupational area was not specified.
Fever (n=153; 83.6%), cough (n=151; 82.5%) and dyspnea (n=136; 74.3%) were the most frequent signs and symptoms, followed by breathing difficulty (n=120; 65.6%), oxygen saturation below 95% (n=90; 49.2%) and sore throat (n=49; 26.8%). Of the 96 (52.2%) health workers who had chest x-rays, 39 (49.6%) had interstitial infiltrates; 23 (12.5%) did not have x-rays and this information had been left blank or was unknown for 65 (35.3%) of them. Of the 87 (47.3%) who needed ventilatory support, 31 (35.6%) had invasive support, 74 (40.2%) did not use ventilatory support and information for 23 (12.5%) had been left blank or was unknown with regard to this.
The median period between first signs and symptoms and hospitalization was 6 days, varying between zero and 32. For cases hospitalized in ITUs, the median period was 7 days, varying between zero and 19. Of the total health worker cases, 27 (14.7%) died and 85 (46.2%) were cured, while this information was left blank or was unknown for 72 (39.1%) of them.
Median age of those who died was 44 years (minimum-maximum: 35-85), and most of them were male (n=18). The majority worked in the area of nursing (n=12) or in the area of medicine (n=9). Moreover, 24 of these health workers had comorbidities, the most frequent of which were heart disease (n=12), diabetes mellitus (n=7) and obesity (n=5). Eleven deaths were recorded in São Paulo and nine in Amazonas.
Discussion
This study described the first health workers to be hospitalized, notified and confirmed as having COVID-19 in Brazil. The cases occurred predominantly among females, young adults, those who worked in the areas of medicine and nursing, and those who had fever, cough and dyspnea and reported heart disease, diabetes mellitus and asthma more frequently.
These findings corroborate Wang et al. and their description of 138 COVID-19 cases from a hospital in Wuhan, China, whereby the most reported symptoms were fever and cough, and similar comorbidities.10 Our findings also validate the findings of Grasselli et al. who described 1,591 cases in Lombardy in Northern Italy, also with similar age ranges and comorbidities.11
This study also ratifies data regarding sex, average age, race/skin color and COVID-19 case signs and symptoms among health workers in the United States, as published by the CDC (Centers for Disease Control and Prevention).12 Despite the female sex being predominant, justified by more women dedicating themselves to these activities,13,14 most deaths occurred among males, which also confirms the results found by Wang et al. and Grasselli et al.10,11
More than 75% of cases were medicine and nursing workers, given their greater exposure to clinical and emergency care. Promoting and preserving the health of these workers is fundamental for maintaining essential services, such as health care, on all levels.
Work process and working conditions can represent risk to health workers as potential sources of exposure to the etiological agent and also, indirectly, risk to their families and other contacts. Increased closeness and more time spent caring for infected people, as a necessary part of their work processes, use and/or provision of inadequate PPEs and, consequently, exposure to the diverse forms of transmission of the pathogen, can lead to these workers becoming ill.15 As such, use of facemasks, adequate hand sanitization, use of eye protection and surgical caps, are measures recommended for protection against infection in the workplace.15–19
The data source used by this study only records hospitalized cases that progressed to SARS; it does not reflect the true magnitude of health workers affected by COVID-19, consequent sick leave and proportion of mild cases.
Another limitation relates to the different forms of notification adopted since the advent of the epidemic: the first cases were notified using REDCap (Research Electronic Data Capture); later mild (non-hospitalized) cases were notified via the e-SUS VE system, a recently created tool for recording suspected and confirmed COVID-19 cases, provided by the SUS Information Technology Department (DATASUS);5 while cases that developed SARS were notified on the SIVEP-Gripe system. At the time this paper went to press, no linkage of these databases had been performed.
Moreover, the recent inclusion of the ‘occupation’ variable on the notification form may explain late recording of COVID-19 cases among health workers (five weeks after the first confirmed case in Brazil was notified), as well as the small number of notified cases among the data retrieved and the the low use of 'occupation' field on the records we have described; as well as notification form input onto the SIVEP-Gripe system not always being timely.
It is appropriate to note that density of health workers in the territory, along with other variables, contributes to identifying response capacities in relation to the pandemic scenario.2 Notwithstanding, the true number of health workers working in this context is uncertain, as is the number of these workers who have become ill due to their work. This knowledge assist the estimation of supplies and equipment needed for health care, so as to ensure safety at work, as well as revealing the true magnitude of the risks faced by this group of workers.
As such, the following recommendations are made: (i) continuous monitoring COVID-19 cases among health workers and their description (flu-like syndrome and SARS); (ii) database linkage (SIVEP-Gripe, e-SUS VE and RedCAP), with the aim of assessing the true magnitude of COVID-19 among these workers; and (iii) standardize the use of the ‘occupation’ variable on SIVEP-Gripe system notifications.
Referências
1. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Situação epidemiológica da COVID-19: doença pelo coronavírus 2019. Bol Epidemiol [Internet]. 2020 abr [citado 2020 ago 17];10. Disponível em: https://portalarquivos.saude.gov.br/images/pdf/2020/April/17/2020-04-16---BE10---Boletim-do-COE-21h.pdf [ Links ]
2. Lopez FG, Palotti PLDM, Barbosa SCT, Koga NM. Mapeamento dos profissionais de saúde no Brasil: alguns apontamentos em vista da crise sanitária da COVID-19. Brasília: Instituto de Pesquisa Econômica Aplicada; 2020 [citado 2020 abr 19]. 13 p. Disponível em: http://desafios2.ipea.gov.br/portal/index.php?option=com_content&view=article&id=35426:nota-tecnica-2020-marco-numero-30-diest-mapeamento-dos-profissionais-de-saude-no-brasil-alguns-apontamentos-em-vista-da-crise-sanitaria-da-COVID-19&catid=189:diest&directory=1 [ Links ]
3. World Health Organization - OMS. Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health 2020 [Internet]. Geneva: World Health Organization; 2020 [cited 2020 Aug 17]. Available from: https://www.who.int/publications/i/item/coronavirus-disease-(covid-19)-outbreak-rights-roles-and-responsibilities-of-health-workers-including-key-considerations-for-occupational-safety-and-health [ Links ]
4. Associação Médica Brasileira - AMB.Faltam EPIs em todo o país [Internet]. São Paulo: Associação Médica Brasileira; 2020 [citado 2020 abr 19]. Disponível em: https://amb.org.br/epi/ [ Links ]
5. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Guia de vigilância epidemiológica: emergência de saúde pública de importância nacional pela doença pelo coronavírus 2019. Vigilância integrada de síndromes respiratórias agudas doença pelo coronavírus 2019, influenza e outros vírus respiratórios [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 abr 20]. Disponível em: https://portaldeboaspraticas.iff.fiocruz.br/biblioteca/guia-de-vigilancia-epidemiologica-emergencia-de-saude-publica-de-importancia-nacional/ [ Links ]
6. Instituto Brasileiro de Geografia e Estatística – IBGE. Diretoria de Pesquisas. Coordenação de População e Indicadores Sociais. Projeção da população do Brasil e Unidades da Federação por sexo e idade para o período 2000-2030 [Internet] Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2020 [citado 2020 ago 17]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/projpopuf.def [ Links ]
7. Ministério da Saúde (BR). DATASUS. Recursos humanos: profissionais. Indivíduos segundo CBO 2002 [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 ago 17]. Disponível em: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?cnes/cnv/prid02br.def [ Links ]
8. Ministério da Saúde (BR). DATASUS. Estabelecimentos por tipo [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 ago 17]. Disponível em: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?cnes/cnv/estabbr.def [ Links ]
9. Brasil. Ministério da Saúde. Portaria MS/GM nº 639, de 31 de março de 2020. Dispõe sobre a ação estratégica ‘O Brasil Conta Comigo - Profissionais da Saúde’, voltada à capacitação e ao cadastramento de profissionais da área de saúde, para o enfrentamento à pandemia do coronavírus (COVID-19) [Internet]. Diário Oficial União, Brasília (DF), 2020 abr 2 [citado 2020 ago 17];Seção 1:76. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2020/prt0639_02_04_2020.html [ Links ]
10. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama [Internet]. 2020 Mar [cited 2020 Aug 17];323(11):1061-9. Available from: https://dx.doi.org/10.1001%2Fjama.2020.1585 [ Links ]
11. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. Jama [Internet]. 2020 Apr [cited 2020 Aug 17];323(16):1574-81. Available from: https://doi.org/10.1001/jama.2020.5394 [ Links ]
12. Burrer SL, de Perio MA, Hughes MM, Kuhar DT, Luckhaupt SE, McDaniel CJ, et al. Characteristics of health care personnel with COVID-19 – United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep [Internet]. 2020 Apr [cited 2020 Aug 17];69(15):477-81. Available from: https://doi.org/10.15585/mmwr.mm6915e6 [ Links ]
13. Machado MH, Aguiar Filho W, Lacerda WF, Oliveira E, Lemos W, Wermelinger M, et al. Características gerais da enfermagem: o perfil sócio demográfico. Enferm Foco [Internet]. 2016 [cited 2020 ago 17];6(1/4):11-7. Disponível em: https://doi.org/10.21675/2357-707X.2016.v7.nESP.686 [ Links ]
14. Scheffer M, Cassenote A, Guilloux AGA, Biancarelli A, Miotto BA, Mainardi GM. Demografia médica no Brasil 2018: número de médicos aumenta e persistem desigualdades de distribuição e problemas na assistência [Internet]. São Paulo: Associação Médica Brasileira; 2018 [citado 2020 ago 17]. Disponível em: https://amb.org.br/wp-content/uploads/2018/03/DEMOGRAFIA-M%C3%89DICA.pdf [ Links ]
15. Ng K, Poon BH, Puar THK, Quah JLS, Loh WJ, Wong YJ, et al. COVID-19 and the risk to health care workers: a case report. 2020. Ann Intern Med [Internet]. 2020 Jun [cited 2020 Aug 17];172(11):766-7. Available from: https://doi.org/10.7326/L20-0175 [ Links ]
16. Wang J, Zhou M, Liu F. Exploring the reasons for healthcare workers infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect [Internet]. 2020 Mar [cited 2020 Aug 17];105:100-1. Available from: https://doi.org/10.1016/j.jhin.2020.03.002 [ Links ]
17. Siegel JD, Rhinehart E, Jackson M, Chiarello L. Health Care Infection Control Practices Advisory Committee. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control [Internet]. 2019 [cited 2020 Aug 17];35(10):S65. Available from: https://www.cdc.gov/infectioncontrol/pdf/guidelines/isolation-guidelines-H.pdf [ Links ]
18. Centers for Disease Control and Prevention - CDC. Use of cloth face coverings to help slow the spread of COVID-19 [Internet]. Washington, D.C.: CDC; 2020 [cited 2020 Aug 17]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html [ Links ]
19. Fiho JMJ, Assunção AA, Algranti E, Garcia EG, Saito CA, Maeno M. A saúde do trabalhador e o enfrentamento da COVID-19. Rev Bras Saúde Ocup [Internet]. 2020 abr [citado 2020 abr 20];45:e14. Disponível em https://doi.org/10.1590/2317-6369ed0000120 [ Links ]
Received: May 08, 2020; Accepted: August 08, 2020











 texto en
texto en 


