Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.5 Brasília 2020 Epub 02-Nov-2020
http://dx.doi.org/10.1590/s1679-49742020000500006
Research Note
Medicinal plants and people with tuberculosis: description of care practices in Northern Bahia, 2017*
1Universidade Federal do Vale do São Francisco, Programa de Pós-Graduação em Ciências da Saúde e Biológicas, Petrolina, PE, Brazil
2Ministério da Saúde, Secretaria de Atenção Primária à Saúde, Brasília, DF, Brazil
3Fundação Oswaldo Cruz, Instituto René Rachou, Belo Horizonte, MG, Brazil
4Universidade Federal da Bahia, Instituto de Saúde Coletiva, Salvador, BA, Brazil
5Universidade de Brasília, Programa de Pós-Graduação em Saúde Coletiva, Brasília, DF, Brazil
6Ministério da Saúde, Secretaria de Vigilância em Saúde, Brasília, DF, Brazil
Objective:
To describe medicinal plants used by people with tuberculosis (TB) in municipalities in Northern Bahia, in 2017.
Methods:
A descriptive study was carried out with primary data on medicinal plants used by people with TB ≥18 years old, presented according to botanical nomenclature and frequency of consumption.
Results:
Of the 80 people interviewed, 50 reported consuming some kind of medicinal plant; these were mainly male (34), ≥47 years old (22), of brown/black skin color (34), with up to complete primary education (25), married (26), not economically active (30), earning up to BRL 300/month (26), with coughs (33) and with no previous history of TB (44). Two species stood out in the citations, Chenopodium ambrosioides L. (worm-seed: 23 citations), and Solanum capsicoides All. (cockroach berry: 17 citations).
Conclusion:
There was widespread use of medicinal plants as a TB care practice in six municipalities in Northern Bahia.
Keywords: Plants, Medicinal; Tuberculosis; Complementary Therapies; Cross-Sectional Studies
Introduction
Currently, some 70,000 new tuberculosis (TB) cases are diagnosed in Brazil every year,1 whereby people with greater social vulnerability are more susceptible to becoming ill.2,3 TB is a disease requiring long treatment, with different drugs that can cause adverse effects.4,5
In the quest for well-being and quality of life, medicinal plants have become an alternative, given their therapeutic credibility and low cost. These conditions loom as an invitation for the introduction of alternative therapies in the search for a cure or even to relieve adverse effects of medication.
There is increasing use of complementary therapies within the Brazilian National Health System (SUS), in particular use of medicinal plants and phytotherapeutic drugs;6-10 however, no recommendations exist in Brazil regarding these care practices for treating TB. Despite this, in the quest for well-being and quality of life, medicinal plants have become an alternative, given their therapeutic credibility and low cost.11 These conditions loom as an invitation for the introduction of alternative therapies in the search for a cure or even to relieve adverse effects of medication.
The objective of this study was to describe consumption of medicinal plants used by people diagnosed with TB in municipalities in the north of Bahia state in 2017.
Methods
This is a descriptive study based on household interviews with people diagnosed as having TB (new and retreatment cases), resident in municipalities in the north of the state of Bahia in 2017.
Bahia is comprised of 417 municipalities, distributed over nine Regional Health Areas (RHA), and its estimated population in 2017 was 15,344,447 inhabitants.11 the Northern Bahia RHA covers 27 municipalities and a population that accounted for approximately 7% of Bahia’s population in the year studied.12-14
The study population was comprised of all individuals notified as having TB in 2017, resident in municipalities in the northern region of Bahia which had (i) a population >50,000 inhabitants and/or (ii) >10 notified TB cases in 2016. These criteria were adopted to ensure the existence of cases and the feasibility of the study in the territory. The household interviews took place between October 1st and December 30th 2017, by means of a semi-structured questionnaire, which a single interviewer used to ask about the practice of consuming medicinal plants before being diagnosed with TB or after treatment had started. Individuals who had been in treatment for more than two months, those under 18 years old and those with cognitive limitations were excluded from the study.
The open questions were answered freely by the interviewees, and what they said was summarized by the researchers after compiling their answers. The summary of the citations was done based on the answers to the following questions:
“Have you used any medicinal plant before or after starting treatment for TB?”
“Which plant?”
“Why have you used a medicinal plant?”
and
“From whom did you learn to use medicinal plants?”
Data were also collected regarding the person’s independent variables during the interview:
sex (male; female);
age range (in years: 18-36; 37-46; 47 or over);
marital status (single; married; other);
schooling (up to complete primary school; up to complete middle school; high school education or above);
race/skin color (self-reported: brown/black; white/yellow/indigenous);
occupation (self-reported: economically active; not economically active);
personal income (BRL [R$]/month);
alcohol consumption (yes; no);
tobacco consumption (yes; no);
household status (own; not own);
prior history of TB (yes; no);
presence of coughing (yes; no);
presence of fever (yes; no);
sweating (yes; no); and
weight loss (yes; no).
The variables were grouped together according to prior knowledge of the scientific literature and their distribution. The data sources were (i) records of the population12 of the 27 municipalities within the administrative region and (ii) the Notifiable Health Conditions Information System (SINAN),15 which was consulted in order to confirm notified cases.
The descriptive analyses were performed using the Stata/MP 12.0 computer program, to provide absolute values for plant consumption measurement and to present the species cited. The botanical nomenclature of these species was retrieved from the online version of the Missouri Botanical Garden Tropicos® database.16
The study project was approved by the Federal University of the São Francisco Valley Research Ethics Committee (CEP-UNIVASF): Certificate of Submission for Ethical Appraisal (CAAE) No. 67456117.3.0000.5196, dated September 23rd 2017. All participants signed a Free and Informed Consent form.
Results
The Northern Bahia municipalities meeting the study’s eligibility criteria were Campo Formoso, Casa Nova, Juazeiro, Paulo Afonso, Pindobaçu and Senhor do Bonfim. In 2017, a total of 199 TB cases were notified on the SINAN system for these municipalities. Of this total number of notified cases, the outcome for 29 (14.6%) was death, 36 (18.0%) had been transferred to other places, 10 (5.0%) had been deprived of liberty and 10 (5.0%) had been lost to follow-up at the time of data collection. In the study period, 114 cases were considered to be feasible for investigation; however 12 people (6.0%) were excluded because they were not found at their residence, 10 (5.0%) because they were under 18 years old, 5 (2.5%) because they had cognitive limitations at the time of the interview and 7 (3.5%) because they refused to take part in the study.
We interviewed 80 people with TB, 50 of whom reported use of medicinal plants as a TB care practice. Higher frequency of medicinal plant use was found among males (34), those aged 47 or over (22), those of brown or black race/skin color (34), those who had up to complete primary education (25), were married (26), were not economically active (30), had income of up to BRL 300/month (26), had a cough (33) and had no prior history of TB (44) (Table 1).
Table 1 Characterization of people with tuberculosis regarding socioeconomic and demographic information, lifestyle, symptoms and medicinal plant use in six municipalities in Northern Bahia, 2017
| Characteristics of the interviewees | n | Plant use | ||
|---|---|---|---|---|
| Yes | No | |||
| 50 | 30 | |||
| Sex | ||||
| Male | 56 | 34 | 22 | |
| Female | 24 | 16 | 8 | |
| Age range (in years) | ||||
| 18-36 | 21 | 12 | 9 | |
| 37-46 | 22 | 16 | 6 | |
| ≥47 | 37 | 22 | 15 | |
| Race/skin color | ||||
| Brown/black | 58 | 34 | 24 | |
| White/yellow/indigenous | 22 | 16 | 6 | |
| Schooling | ||||
| Up to complete primary education | 38 | 25 | 13 | |
| Up to complete middle school education | 28 | 15 | 13 | |
| High school education or above | 14 | 10 | 4 | |
| Marital statusa | ||||
| Married | 39 | 26 | 13 | |
| Single | 28 | 14 | 14 | |
| Other | 13 | 10 | 3 | |
| Occupationb | ||||
| Economically active | 32 | 20 | 12 | |
| Not economically active | 48 | 30 | 18 | |
| Personal income (BRL(R$)/month) | ||||
| R$ 0,00 a R$ 300,00 | 40 | 26 | 14 | |
| R$ 301,00 a R$ 937,00 | 28 | 18 | 10 | |
| Maior que R$ 937,00 | 12 | 6 | 6 | |
| Household statusc | ||||
| Own home | 50 | 30 | 20 | |
| Not own home | 30 | 20 | 10 | |
| Prior history of tuberculosis | ||||
| Yes | 12 | 6 | 6 | |
| No | 68 | 44 | 24 | |
| Alcohol consumption | ||||
| Yes | 15 | 11 | 4 | |
| No | 65 | 39 | 26 | |
| Tobacco consumption | ||||
| Yes | 13 | 11 | 2 | |
| No | 67 | 39 | 28 | |
| Presence of cough | ||||
| Yes | 44 | 33 | 11 | |
| No | 36 | 17 | 19 | |
| Presence of fever | ||||
| Yes | 21 | 16 | 5 | |
| No | 59 | 34 | 25 | |
| Sweatin | ||||
| Yes | 37 | 23 | 14 | |
| No | 43 | 27 | 16 | |
| Weight loss | ||||
| Yes | 46 | 28 | 18 | |
| No | 34 | 22 | 12 | |
a)Marital status: ‘other’ category = separated, widowed and other.
b)Occupation: ‘economically active’ category = employed, retired and social security beneficiary; ‘not economically active’ category = unemployed and housewife without monthly income.
c)Household status: ‘own’ category = 1. Owner of the property or 2. Living free of charge in a property belonging to a friend or relative.
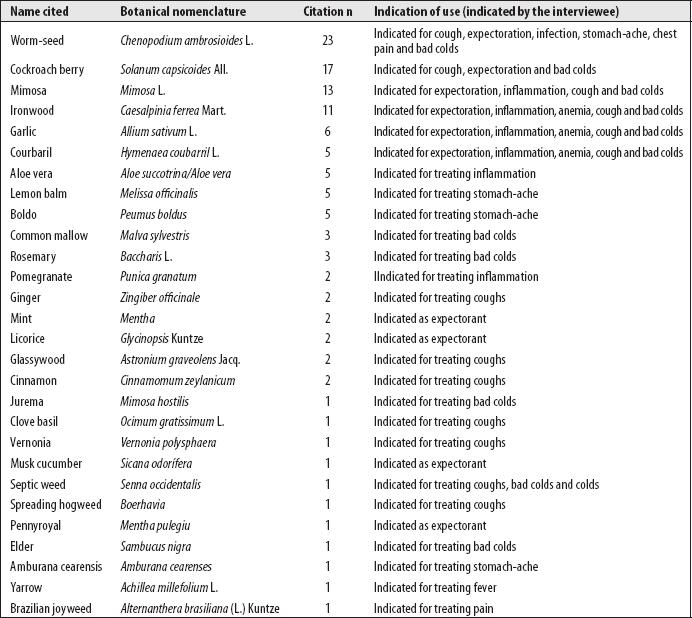
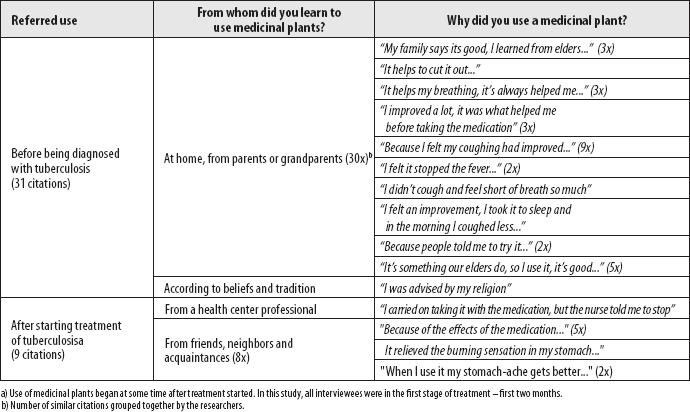
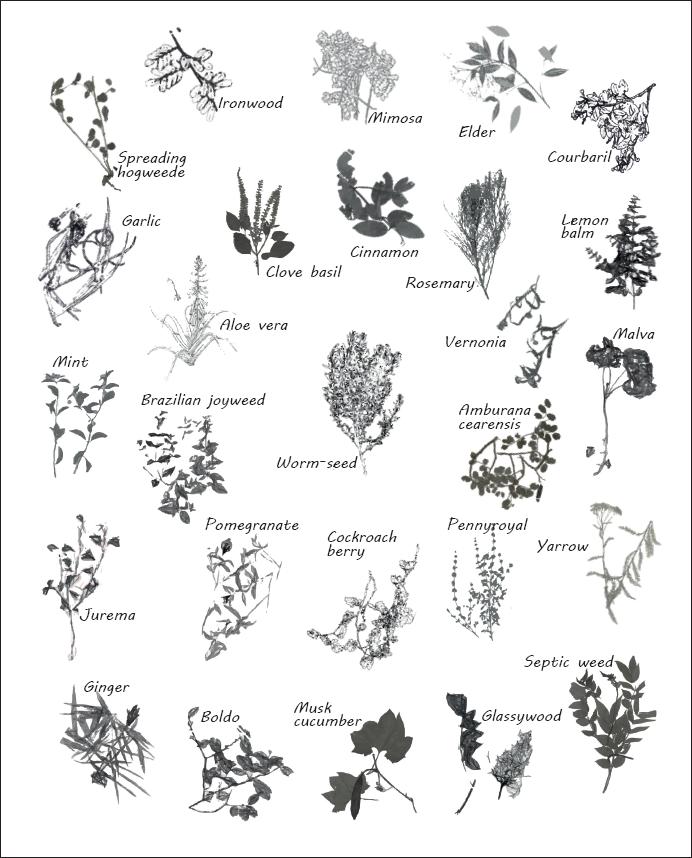
Standing out among the plants were: Chenopodium ambrosioides L. (worm-seed), cited by 23 people; and Solanum capsicoides All. (cockroach berry), cited by 17 people. Notwithstanding, use of other medical plants was also cited as a TB care practice (Figures 1 and 2). The interviewees reported that medicinal plants relived coughing (13) or helped with expectoration (10), controlling fever and other TB symptoms (7), and their use was also related to controlling adverse effects of medication used to treat TB. Knowledge about use of medicinal plants was mainly attributed to having learned from parents and grandparents (30), and from friends, neighbors and acquaintances (8) (Figure 3).
Source: Tropicos®. Missouri Botanical Garden.
Figure 1 Medicinal plants used by people with tuberculosis in six municipalities in Northern Bahia, 2017
Discussion
This study found high prevalence of medicinal plant consumption among people with TB, motivated by coughing and other symptoms of the disease. Family influence was found with regard to this knowledge being passed down from generation to generation, as widely discussed in the scientific literature.17,18 The most cited plant, worm-seed (Chenopodium ambrosioides L.), is used in popular medicine for a variety of purposes;19 its antimicrobial activity against strains of M. tuberculosis relieves TB symptoms because it inhibits bacillus growth,20 and this fact can encourage the incorporation of this species in the care provision for people living with TB. However, under no circumstances whatsoever should it be used to replace treatment proven to lead to cure.4
Used in the form of a “lambedor”, similar to homemade syrup, cockroach berry (Solanum capsicoides All.) was the second most cited plant in the interviews: its use was related to relieving coughing, expectoration and bad colds, although no scientific evidence was found relating it to TB care practice; given the frequency with which its consumption was cited, we suggest that further investigation of this species be conducted.
The people who were interviewed were being treated with medication. The interviews took place at the beginning of treatment in an attempt to minimize recall bias when retrieving information about use of medicinal plants before treatment started. It is also important to highlight the sample size, which was insufficient to analyze associations between use of medicinal plants during treatment and variables of interest. Despite these limitations, besides broadening the discussion on forms of care and care practices, the data obtained provide evidence of use of vegetable species in the TB scenario.
For over 40 years, the World Health Organization has encouraged incorporation of traditional knowledge into Primary Health Care activities.7 In Brazil, the publication in 2006, of the National Policy on Integrative and Complementary Practices within the SUS, pointed to the need to provide training for health workers in the adequate management of these practices.6 SUS managers need to collaborate to make this policy effective, through financial incentives and by keeping the subject on the continuing education agenda. Similarly, universities and faculties can consider and discuss the possibility of including this knowledge on Health teaching curricula.21
Medicinal plant use was found to be widespread as a TB care practice in Northern Bahia municipalities. In view of this, we recommend that individuals should be questioned and guided on their adequate use and, in the absence of scientific evidence confirming benefits provided by them during TB treatment, that continuing with combination therapy should be advised against.
REFERENCES
1. Souza Júnior EV, Nunes GA, Cruz DP, Boery EN, Boery RNSO. Internações hospitalares e impacto financeiro por tuberculose pulmonar na Bahia, Brasil. Enferm Actual Costa Rica [Internet]. 2018 dez [citado 2020 jul 3];(35):38-51. Disponível em: http://dx.doi.org/10.15517/revenf.v0i35.31868 [ Links ]
2. Andrade KVF, Nery JS, Araújo GS, Barreto ML, Pereira SM. Associação entre desfecho do tratamento, características sociodemográficas e benefícios sociais recebidos por indivíduos com tuberculose em Salvador, Bahia, 2014-2016*. Epidemiol Serv Saúde [Internet]. 2019 jun [citado 2020 jul 3];28(2):e2018220. Disponível em: https://doi.org/10.5123/s1679-49742019000200004 [ Links ]
3. Oliosi JGN, Reis-Santos B, Locatelli RL, Sales CMM, Silva Filho WG, Silva KC, et al. Effect of the Bolsa Familia Programme on the outcome of tuberculosis treatment: a prospective cohort study. Lancet Glob Health [Internet]. 2019 Dec [cited 2020 Jul 2];7(2):e219-26. Available from: https://doi.org/10.1016/S2214-109X(18)30478-9 [ Links ]
4. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Manual de recomendações para o controle da tuberculose no Brasil [Internet]. 2. ed. atual. Brasília: Ministério da Saúde; 2019 [citado 2019 out 23]. 364 p. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/manual_recomendacoes_controle_tuberculose_brasil_2_ed.pdf [ Links ]
5. Rabahi MF, Silva Júnior JLR, Ferreira ACG, Tannus-Silva DGS, Conde MB. Tuberculosis treatment. J Bras Pneumol [Internet]. 2017 Nov-Dec [cited 2020 Jul 3];43(6):472-86. Available from: http://jornaldepneumologia.com.br/detalhe_artigo.asp?id=2741 [ Links ]
6. Ministério da Saúde (BR). Departamento de Atenção Básica. Política nacional de práticas integrativas e complementares no SUS: atitude de ampliação de acesso [Internet]. Brasília: Ministério da Saúde; 2006 [citado 2020 jul 3]. 92 p. Disponível em: http://189.28.128.100/dab/docs/publicacoes/geral/pnpic.pdf [ Links ]
7. Ministério da Saúde (BR). Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Política e programa nacional de plantas medicinais e fitoterápicos [Internet]. Brasília: Ministério da Saúde; 2016 [citado 2019 jul 12]. 190 p. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/politica_programa_nacional_plantas_medicinais_fitoterapicos.pdf [ Links ]
8. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Política nacional de práticas integrativas e complementares no SUS: atitude de ampliação de acesso [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2020 abr 13]. 96 p. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/politica_praticas_integrativas_complementares_sus_2ed_1_reimp.pdf [ Links ]
9. Tesser CD, Sousa IMC, Nascimento MC. Práticas integrativas e complementares na atenção primária à saúde brasileira. Saúde Debate [Internet]. 2018 [citado 2020 jul 3];42(n. esp):174-88. Disponível em: https://doi.org/10.1590/0103-11042018s112 [ Links ]
10. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Manual de implantação de serviços de práticas integrativas e complementares no SUS [Internet]. Brasília: Ministério da Saúde; 2018 [citado 2020 jun 2]. Disponível em: http://189.28.128.100/dab/docs/portaldab/publicacoes/manual_implantacao_servicos_pics.pdf [ Links ]
11. Organización Mundial de la Salud - OMS. Estrategia de la OMS sobre medicina tradicional 2002–2005 [Internet]. Ginebra: Organización Mundial de la Salud; 2002 [citado 2019 jul 17]. Disponível em: https://www.paho.org/bra/index.php?option=com_docman&view=download&alias=796-estrategia-oms-sobre-medicina-tradicional-2002-2005-6&category_slug=vigilancia-sanitaria-959&Itemid=965 [ Links ]
12. Instituto Brasileiro de Geografia e Estatística - IBGE. Conheça cidades e Estados do Brasil [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2017 [citado 2020 jul 3]. Disponível em: https://cidades.ibge.gov.br/ [ Links ]
13. Governo do Estado da Bahia. Casa Civil. Lei n. 13.204, de 11 de dezembro de 2014. Modifica a estrutura organizacional da Administração Pública do Poder Executivo Estadual e dá outras providências [Internet]. Diário Oficial do Estado da Bahia; Salvador (BA); 2014 maio 11 [citado 2020 abr 17]. Disponível em: http://www.secom.ba.gov.br/arquivos/File/LEI13204.pdf [ Links ]
14. Secretaria da Saúde do Estado da Bahia - SESAB. Superintendência de Estudos Econômicos e Sociais da Bahia. A regionalização da Secretaria de Saúde do Estado da Bahia [Internet]. Salvador: SESAB; 2018 [citado 2020 jul 3]. Disponível em: http://www.sei.ba.gov.br/index.php?option=com_content&view=article&id=2597&Itemid=701,%20acessado%20em%2003/07/2018 [ Links ]
15. Ministério da Saúde (BR). DATASUS: informações de saúde (TABNET) - demográficas e socioeconômicas [Internet]. Brasília: Ministério da Saúde; 2017 [citado 2017 dez 3]. Disponível em: http://www.datasus.gov.br/informacoes-de-saude/tabnet [ Links ]
16. Tropicos. Missouri botanical garden [Internet]. Saint Louis: Tropicos; 2019 [cited 2020 Apr 18]. Available from: http://legacy.tropicos.org/home.aspx [ Links ]
17. Pio IDSL, Lavor AL, Damasceno CMD, Menezes PMN, Silva FS, Maia GLA. Traditional knowledge and uses of medicinal plants by the inhabitants of the islands of the São Francisco river, Brazil and preliminary analysis of Rhaphiodon echinus (Lamiaceae). Braz J Biol [Internet]. 2018 Jan-Mar [cited 2020 Jul 3];79(1):87-99. Available from: https://doi.org/10.1590/1519-6984.177447 [ Links ]
18. Silva AR, Sousa AI, Sant’Anna CC. Práticas de cuidado empregadas no tratamento de crianças e adolescentes com infecção latente por tuberculose. Epidemiol Serv Saúde [Internet]. 2014 jul-set [citado 2020 jul 3];23(3):547-52. Disponível em: https://doi.org/10.5123/S1679-49742014000300018 [ Links ]
19. Penido AB, Morais SM, Ribeiro AB, Silva AZ. Ethnobotanical study of medicinal plants in Imperatriz, State of Maranhão, Northeastern Brazil. ACTA Amaz [Internet]. 2016 Oct-Dec [cited 2020 Jul 3];46(4):345-54. Available from: https://doi.org/10.1590/1809-4392201600584 [ Links ]
20. Jesus RS, Piana M, Freitas RB, Brum TF, Alves CFS, Belke BV, et al. In vitro antimicrobial and antimycobacterial activity and HPLC–DAD screening of Jun [cited 2020 Jul 3];49(2):296-302. Available from: https://doi.org/10.1016/j.bjm.2017.02.012 [ Links ]
21. Zeni ALB, Parisotto AV, Mattos G, Helena ETS. Utilização de plantas medicinais como remédio caseiro na Atenção Primária em Blumenau, Santa Catarina, Brasil. Ciênc Saúde Coletiva [Internet]. 2017 ago [citado 2020 jul 3];22(8):2703-12. Available from: https://doi.org/10.1590/1413-81232017228.18892015 [ Links ]
*Study derived from the Master’s Degree dissertation by Walter Ataalpa de Freitas Neto, entitled ‘Living conditions and medicinal plant consumption in the therapeutic itinerary of people with tuberculosis in Northern Bahia, 2017’, submitted to the Federal University of the São Francisco Valley (UNIVASF) Health and Biological Sciences Postgraduate Program in 2019.
4
Erratum
In the article “Medicinal plants and people with tuberculosis: description of care practices in Northern Bahia, 2017” doi: 10.1590/S1679-49742020000500006, published on Epidemiology and Health Services, 29(5):1-9, in the pages 2 and 3:
Original text:
“27 municipalities within the administrative region”
Corrected text:
“28 municipalities within the administrative region”
Received: March 03, 2020; Accepted: June 03, 2020











 texto em
texto em