Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.29 no.5 Brasília 2020 Epub 25-Nov-2020
http://dx.doi.org/10.1590/s1679-49742020000500015
Tools for health management and surveillance
Congenital anomalies from the health surveillance perspective: compilation of a list based on ICD-10
1Universidade Federal do Rio Grande Sul, Departamento de Genética, Porto Alegre, RS, Brazil
2Ministério da Saúde, Secretaria de Vigilância em Saúde, Brasília, DF, Brazil
Objective:
To propose a list of congenital anomalies having corresponding codes in the International Statistical Classification of Diseases and Related Health Problems, 10thRevision (ICD-10), with the aim of applying it in health surveillance.
Methods:
In December 2019, the following data sources were searched: ICD-10; ICD-11; anomalies monitored by three surveillance programs; and a database of rare diseases (Orphanet). Anomalies were retrieved from these data sources, processed to check for correspondence with ICD-10 and reviewed manually to compile the list.
Results:
898 codes were identified, of which 619 (68.9%) were contained in ICD-10 Chapter XVII. Of the 279 codes contained in other chapters, 19 were exclusive to the ICD-11 search, 72 to the surveillance programs, 79 to Orphanet and 36 to the search for terms in ICD-10.
Conclusion:
The codes contained in ICD-10 Chapter XVII do not capture the totality of congenital anomalies, indicating the need to adopt an expanded list.
Keywords: Congenital Abnormalities; Rare Diseases; International Classification of Diseases; Epidemiological Monitoring
Introduction
The World Health Organization (WHO) defines congenital anomalies (birth defects) as structural or functional changes in the embryo or fetus, derived from factors prior to birth, which can be identified during prenatal monitoring, at birth or later during life.(1)Globally it is estimated that some 3% of live births have some kind of anomaly every year,(2),(3)and at least 3.3 million children under five years old die every year because of severe congenital anomalies. Among those affected who survive, many have disabilities over the course of their lives.(4)
A comprehensive and robust coding and classification system is essential for surveillance of congenital anomalies, however there is no agreed list that brings together all these health conditions.(5)The International Statistical Classification of Diseases and Related Health Problems (ICD) contains the codes adopted internationally for epidemiological purposes. In its tenth revision (ICD-10), chapter XVII (Congenital malformations, deformations and chromosomal anomalies) refers exclusively to congenital anomalies.(6)Despite this chapter being widely used as a reference for surveillance, there are other health conditions that fall into the concept of congenital anomalies but which are listed in other chapters of ICD-10. Despite the updates to the eleventh edition, ICD-11, international institutions, such as the International Clearinghouse for Birth Defects Surveillance and Research (ICBDSR) and the European Network of Population-Based Registries for the Epidemiological Surveillance of Congenital Anomalies (EUROCAT), note that the latest version will not be sufficient to encompass all congenital anomalies in a single chapter.(5)
Some international congenital abnormality surveillance programs include health conditions that are not included in ICD-10 chapter XVII, according to their objectives and priorities. In Brazil, ICD-10 chapter XVII codes are used to record congenital abnormality cases on information systems, such as the Live Birth Information System (SINASC). Proposing a list using multiple sources of information aims to enable the establishment of a comprehensive set of congenital anomalies, so as to list those that are a priority for monitoring. In this way it will be possible to expand the list of codes eligible for inclusion on the system and, consequently, enhance surveillance of anomalies identified at birth.
The objective of this paper was to propose a list of congenital anomalies expanded beyond ICD-10 chapter XVII, with the aim of making it available for application within health surveillance.
Building the list
The following sources of information were used: ICD-10, published in 2007 and currently in force in Brazil; ICD-11, released by WHO in 2019, to be implemented with effect from 2022; congenital anomalies monitored by selected surveillance models, identified by means of a narrative literature review;(7)and a repository/information base on rare diseases, namely Orphanet.(8)The codes were retrieved from the different sources in December 2019.
We included conditions that met the concept of congenital anomalies adopted by WHO.(1)Although by definition they are not congenital anomalies, congenital infections were included, given that some of them have important outcomes within the context of health surveillance.(9)Conditions for which there were no corresponding ICD-10 codes were excluded, in particular to maintain correspondence with case recording on the Ministry of Health information systems.
The codes for congenital anomalies contained in ICD-10 chapter XVII were included. A search was also performed for the terms ‘congênit’, ‘malforma’, ‘displas’, ‘disrup’ and ‘genétic’, and all corresponding codes were included.
ICD-11 congenital abnormality codes were taken from chapter 20, which lists developmental anomalies, as well as all codes related to inborn errors of metabolism – these being congenital anomalies by definition.
In addition, we used the anomaly lists of three surveillance models: EUROCAT,(10),(11)ECLAMC (Latin American Collaborative Study of Congenital Malformations)(12),(13)and CREC (Costa Rican Birth Defects Register).(14)The ECLAMC and EUROCAT networks were selected for their being a reference for Latin America and Europe, respectively. CREC was chosen because it includes a large number of functional anomalies and monitors the largest number of congenital anomalies outside of ICD-10 chapter XVII, when compared to the other programs analyzed.(13)ECLAMC does not have a specific list of anomalies for surveillance, but provides a consultation atlas containing a defined list of conditions.(13)
Two strategies were applied for retrieving congenital anomalies from Orphanet.(8)The first strategy found six out of 35 rare disease classifications that met the concept of congenital anomalies: (i) Rare development defect during embryogenesis; (ii) Rare heart malformation; (iii) Rare inborn errors of metabolism; (iv) Rare genetic disease; (v) Rare teratogenic disorder; and (vi) Chromosomal anomalies sorted by chromosome. The second search strategy sought to capture congenital anomalies in addition to these classifications, using the type of disorder hierarchical classification model ( http://www.orpha.net/orphacom/cahiers/docs/GB/Orphanet_linearisation_rules.pdf ), considering malformation syndromes and morphological anomalies as congenital anomalies.
The ICD-11 and Orphanet congenital anomaly codes were mapped to check for correspondence with ICD-10, in accordance with guidance provided by these sources. We included Orphanet codes that corresponded exactly to ICD-10. All the congenital abnormality codes we retrieved were later compiled as a single list and duplications were removed.
Following processing, the list was reviewed manually (Bremm JM and Cardoso-dos-Santos AC), in order to exclude conditions that did not met the concept of congenital anomalies. The list obtained following this review was validated by two specialist geneticists (Sanseverino MTV and Schüler-Faccini L). Finally, in order to classify the anomalies in the final list, we used the ICD-11 model, which provides a more up to date and comprehensive classification than ICD-10.
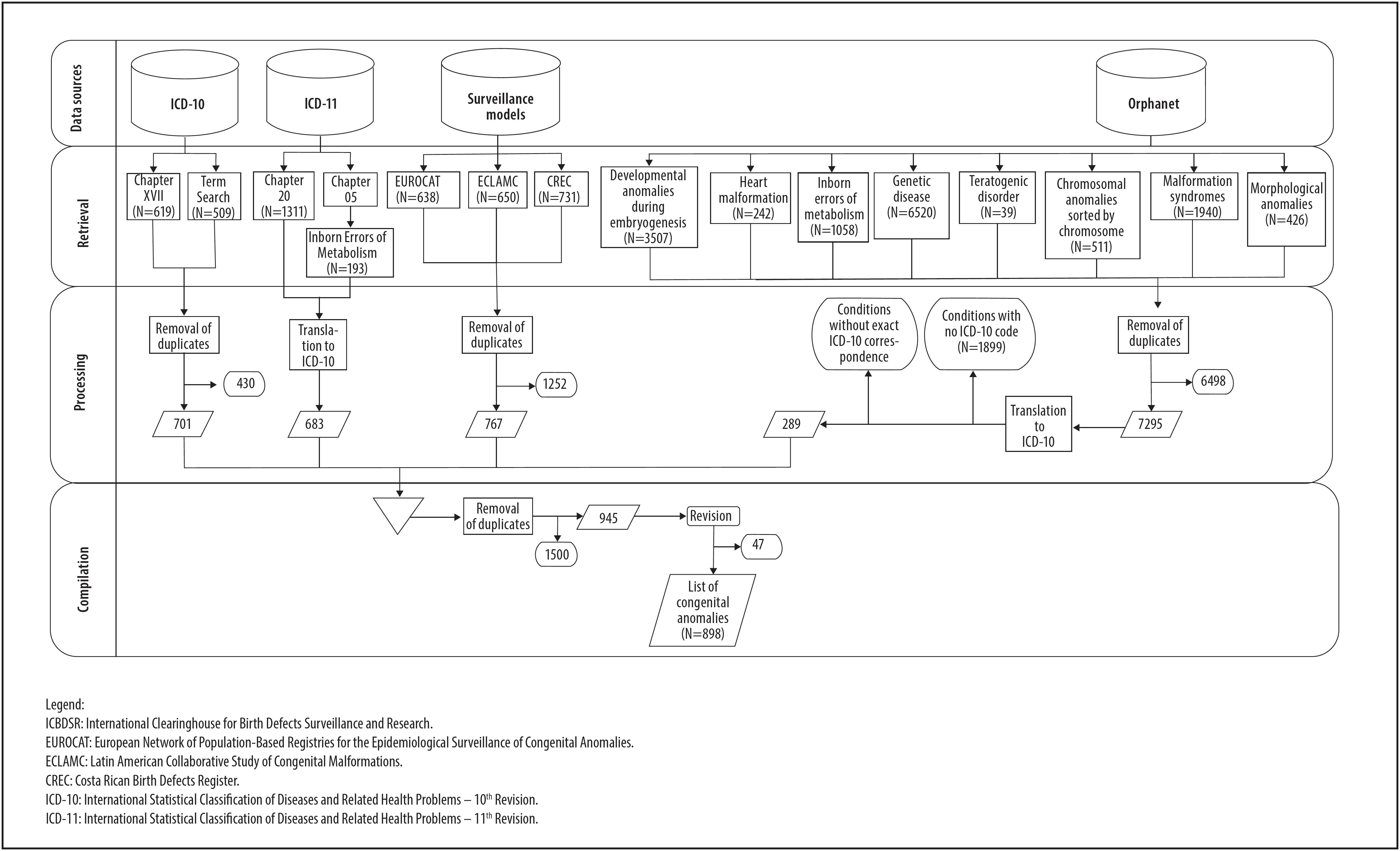
Figure 1 shows the sources consulted and the process used to obtain the data. With regard to ICD-10, in addition to the 619 codes contained in chapter XVII, a further 509 codes were identified by means of searching for terms; once both code sets had been compiled and duplicated codes had been removed, a total of 701 codes remained. With regard to ICD-11, chapter 20 (Developmental Anomalies) contains 1311 congenital anomaly codes, as well as 193 codes related to inborn errors of metabolism which, after checking for correspondence with ICD-10, resulting in 683 unique codes. With regard to the surveillance models, 638 codes were included from EUROCAT, 650 from ECLAMC and 731 from CREC. 767 unique codes remained after compilation and removal of duplicates.
As for the Orphanet classifications, codes were identified in relation to rare development defect during embryogenesis (3507 codes), rare heart malformation (242), rare genetic disease (6520), rare inborn errors of metabolism (1058), rare teratogenic disorder (39) and chromosomal anomalies sorted by chromosome (511 codes). With regard to type of disorder, there were 1940 codes for malformation syndromes and 426 codes for morphological anomalies. 6498 Orphanet codes were excluded following compilation and removal of duplicates. Only 289 Orphanet codes (3.96% of the total) corresponded exactly to ICD-10.
Following this the list of anomalies having ICD-10 codes, obtained from different sources, was compiled and duplicates were removed and 1500 codes were excluded. The remaining 945 codes were submitted to a manual review, whereby 47 were excluded because they did not meet the concept of congenital anomalies. This process resulted in a list of 898 anomaly codes, classified into 21 distinct groups in keeping with ICD-11 ( Figure 2 ).
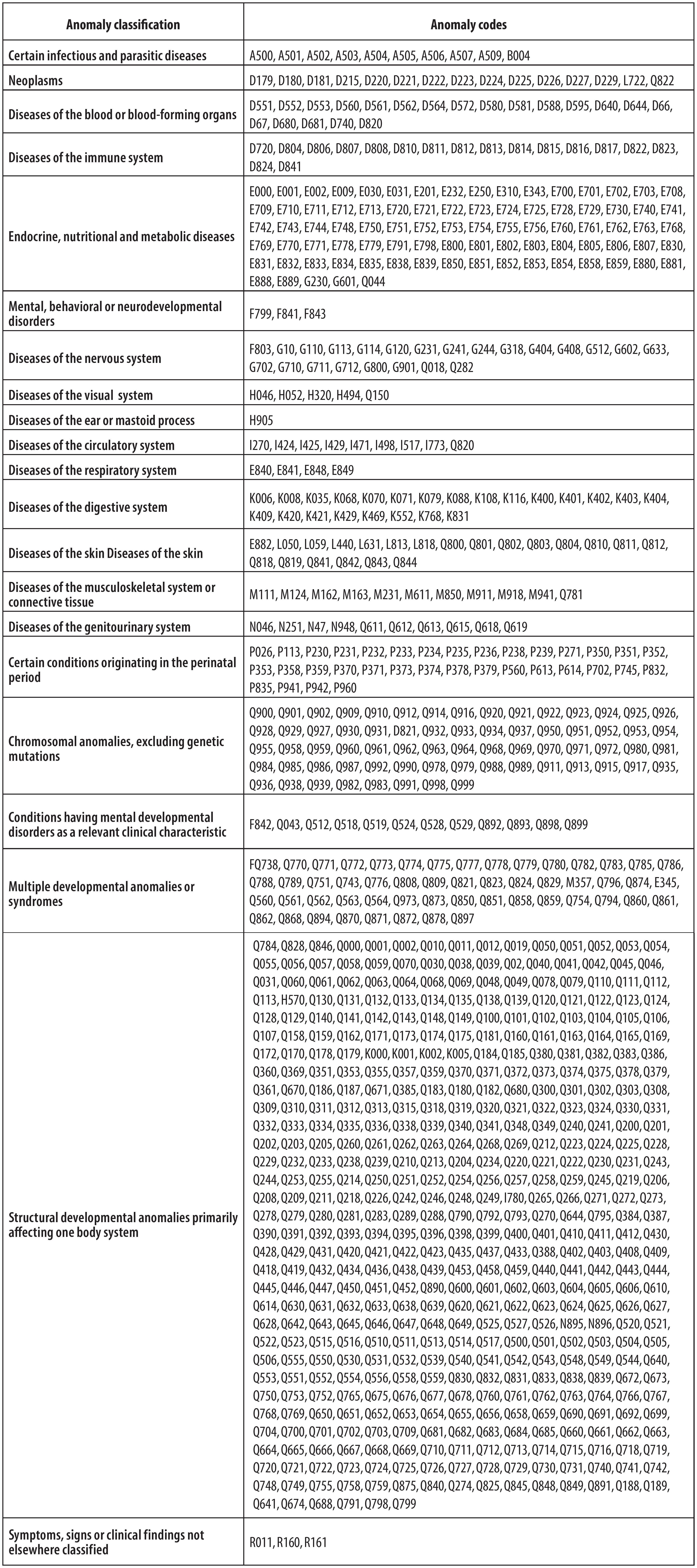
Figure 2 Classification of congenital anormalies according to the chapters of the International Statistical Classification of Diseases and Related Health Problems – Eleventh Revision (ICD-11)
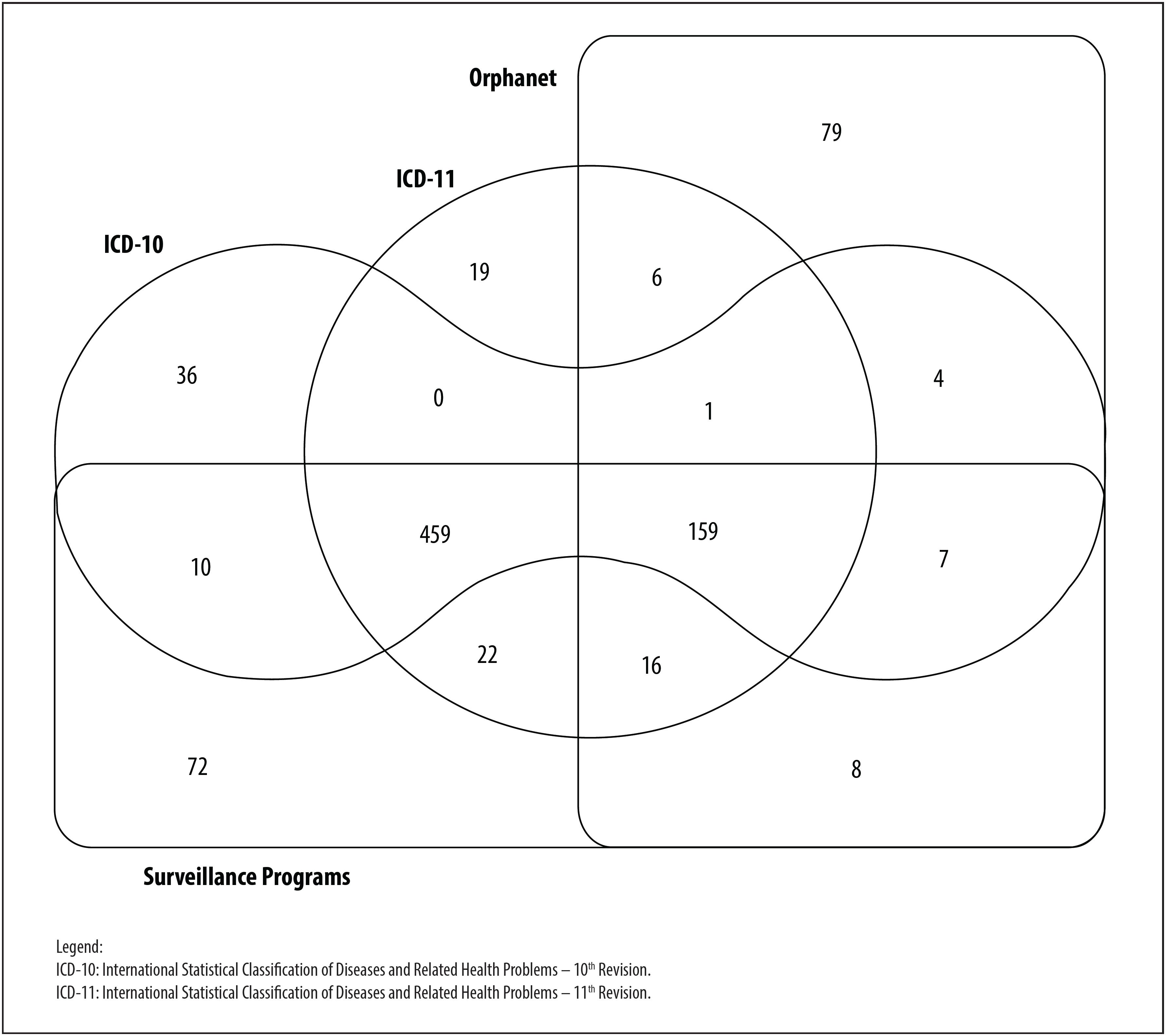
The final list brought together the 619 codes of ICD-10 chapter XVII, plus 279 codes from other ICD chapters, of which 19 came exclusively from the search on ICD-11, 72 codes came from the surveillance models, 79 from Orphanet and 36 from term searches on ICD-10. In particular, 87 congenital anomalies were shared by at least two of these different sources ( Figure 3 ).
Discussion
This paper proposes a list comprised of de 898 anomalies with corresponding ICD-10 codes, to enable the concept of congenital anomalies provided by WHO to be put into practice. When compared to ICD-10 chapter XVII,(6)the list we prepared includes 279 new conditions. The Brazilian Live Birth Information System (SINASC) only allows codes contained in ICD-10 chapter XVII to be input, thus limiting surveillance of congenital anomalies in Brazil.
A comprehensive list of ICD-10 coded congenital anomalies is important for health surveillance. Congenital anomaly coding is widely performed by health professionals to record cases on information systems. Notwithstanding, mapping the codes was challenging. In many cases, we did not find exact correspondence between ICD-10 codes and the codes contained in the sources we used, and this can lead to errors. In order to minimize this limitation, only anomalies corresponding exactly to ICD-10 were selected. The codes were then checked manually in order to enhance their accuracy.
Allowing the inclusion of new ICD-10 codes in order to input congenital anomalies on information systems, especially the SINASC system, will be extremely relevant for health surveillance.(4)The current version does not provide coding for some conditions, and the ICD-10 chapter on congenital anomalies (XVII) is basically restricted to structural anomalies. Although new conditions have been added to ICD-11 chapter 20, this measure has not been sufficient to cover all conditions that can be defined as congenital anomalies. The data we retrieved and analyzed corroborate the joint statement made by the two biggest international congenital anomaly surveillance networks, EUROCAT and ICBDSR.(5)
Within this context, the expanded list proposed here provides a broader scope of congenital anomalies which is useful for surveillance of these conditions and for surveillance objectives and priorities. In conclusion, the incorporation of new data sources brings this list closer to the total amount of congenital anomalies needing to be recorded in Brazil.
Referências
1. World Health Organization - WHO. Birth defects surveillance atlas of selected congenital anomalies [Internet]. Geneva: World Health Organization; 2014 [cited 2020 Aug 31]. 28 p. Available from: https://apps.who.int/iris/handle/10665/127941 [ Links ]
2. Harris BS, Bishop KC, Kemeny HR, Walker JS, Rhee E, Kuller JA. Risk factors for birth defects. Obstet Gynecol Surv [Internet]. 2017 Feb [cited 2020 Aug 31];72(2):123-35. Available from: https://doi.org/10.1097/ogx.0000000000000405 [ Links ]
3. Carmichael SL. Birth defects epidemiology. Eur J Med Genet [Internet]. 2014 Aug [cited 2020 Aug 31];57(8):355-8. Available from: https://doi.org/10.1016/j.ejmg.2014.03.002 [ Links ]
4. March of Dimes. March of Dimes global report on birth defects [Internet]. Arlington: March of Dimes; 2020 [cited 2020 Mar 10]. Available from: https://www.marchofdimes.org/mission/march-of-dimes-global-report-on-birth-defects.aspx [ Links ]
5. EUROCAT, ICBDSR. Statement of EUROCAT and ICBDSR on ICD11 [Internet]. [S.l.]: EUROCAT; 2009 [cited 2020 Jan 28]. Available from: https://eu-rd-platform.jrc.ec.europa.eu/sites/default/files/EUROCAT-Joint-Statement-ICD11-June-2009.pdf [ Links ]
6. Organização Mundial da Saúde - OMS. CID-10: Classificação estatística internacional de doenças. 10. ed. São Paulo: Edusp; 2007. (Com disquete, vol. 1) [ Links ]
7. Cardoso-dos-Santos A, Magalhães V, Medeiros-de-Souza A, Bremm JM, Alves RFS, Araujo VEM, et al. Redes internacionais de colaboração para a vigilância das anomalias congênitas: uma revisão narrativa. Epidemiol Serv Saúde [Internet]. 2020 jul [citado 2020 ago 31];29(4):e2020093. Disponível em: https://doi.org/10.5123/s1679-49742020000400003 [ Links ]
8. Orphanet. Orphanet: an online database of rare diseases and orphan drugs [Internet]. [S.l.]: Orphanet; 1997 [cited 2020 Jan 28]. Available from: https://www.orpha.net/consor/cgi-bin/index.php [ Links ]
9. Neu N, Duchon J, Zachariah P. TORCH infections. Clin Perinatol [Internet]. 2015 Mar [cited 2020 Aug 31];42(1):77-103. Available from: https://doi.org/10.1016/j.clp.2014.11.001 [ Links ]
10. Tucker FD, Morris JK, JRC Management Committee, Neville A, Garne E, Kinsner-Ovaskainen A, et al. EUROCAT: an update on its functions and activities. J Community Genet [Internet]. 2018 Oct [cited 2020 Aug 31];9(4):407-10. Available from: https://doi.org/10.1007/s12687-018-0367-3 [ Links ]
11. EUROCAT. EUROCAT Guide 1.4: Instruction for the registration of congenital anomalies [Internet]. Ispra: EUROCAT Central Registry; University of Ulster; 2013 [cited 2020 Jan 28]. Available from: https://eu-rd-platform.jrc.ec.europa.eu/sites/default/files/Full_Guide_1_4_version_28_DEC2018.pdf [ Links ]
12. Poletta FA, Gili JA, Castilla EE. Latin American collaborative study of congenital malformations (ECLAMC): a model for health collaborative studies. Public Health Genomics [Internet]. 2014 [cited 2020 Aug 31];17(2):61-7. Available from: https://doi.org/10.1159/000356568 [ Links ]
13. ECLAMC. Congenital malformations browser [Internet]. [S.l.]: ECLAMC; 2013 [citado 2020 jan 28]. Disponível em: http://en.atlaseclamc.org/ [ Links ]
14. Ministerio de la Salud de Costa Rica. Protocolo de vigilancia de defectos congénitos en Costa Rica [Internet]. San José; Ministerio de la Salud de Costa Rica; 2018 [citado 2020 jan 28]. Disponível em: https://www.ministeriodesalud.go.cr/index.php/vigilancia-de-la-salud/normas-protocolos-y-guias/malformaciones-congenitas/3785-protocolo-de-vigilancia-de-defectos-congenitos-marzo-2018/fileAbstract [ Links ]
Received: April 14, 2020; Accepted: July 14, 2020











 texto em
texto em 
 Curriculum ScienTI
Curriculum ScienTI