Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.1 Brasília 2021 Epub 07-Dez-2020
http://dx.doi.org/10.1590/s1679-49742021000100019
Original article
Lethality and characteristics of deaths due to COVID-19 in Rondônia: an observational study
1Universidade Federal de Rondônia, Departamento de Medicina, Porto Velho, Rondônia, Brazil
2Universidade Federal de Rondônia, Departamento de Matemática, Porto Velho, Rondônia, Brazil
Methods
This was a descriptive study, with data from the Brazilian National Health System Epidemiological Surveillance System Computerization Strategy (E-SUS-VE, notified between January 1 and August 20, 2020. Statistical tests (Chi-square and Marascuilo procedure) were applied, where differences were considered to be significant when p< 0.05.
Results
184,146 suspected cases were reported, of which 49,804 were confirmed as COVID-19, and 1,020 died (lethality 2.1%). Statistically significant differences were observed between age groups and lethality (p-value <0.001); lethality was greater as age increased (Marascuilo procedure, significant in the comparison between the over 60s and the other age groups); death was higher among males (2.7% lethality); and lethality was higher among Black people (3.0%).
Conclusion
Lethality was greater among the elderly, males and people of brown and black skin color in Rondônia.
Key words: Epidemiology, Descriptive; Mortality; Age Groups; Sex Distribution; Race Factors; Coronavirus Infections
Introduction
Brazil’s highest COVID-19 incidence rates have occurred in the country’s Northern region, with 2,843.1 cases/100,000 inhabitants and a mortality rate of 72.2 deaths/100,000 inhab. As at the 20th week of the epidemic, the state of Rondônia had recorded incidence higher than that found for the rest of the Northern region, with 3,027.5 cases/100,000 inhab. and a mortality rate of 62.4 deaths/100,000 inhab., the latter being slightly below the regional average.1 Rondônia’s first case was recorded on March 20th 2020. When it beginning its course, the pandemic followed a pattern common to other places: a disease brought by travelers arriving by plane. The expectation was that SARS-CoV-2 transmission would be rapidly contained and would not cause significant problems, especially for the state’s health services and those of its municipalities. A slow process of structuring the hospital network was begun, centered on availability of intensive care beds. Health managers frequently appeared in the media, especially on social networks, informing as to the efforts to achieve this, including with regard to diagnosis services centralized at the Central Public Health Laboratory, as well as purchasing of rapid tests
Cumulative weekly case distribution in the state of Rondônia from March 20th to the first week of August followed a rising trend, in line with the overall behavior of the pandemic in Brazil. In the initial weeks, the number of infected people increased rapidly, and the number of cases increased threefold in this period in Rondônia. In the last weeks of August 2020, there was a 10.0 to 15.0% increase over total cases notified for the previous week. At the end of August 2020, every day some 750 cases were notified, increasing considerably the cumulative number of cases in the state. At the end of August 2020, around 10.0% of the previous week’s cases were added to the current week.2
Despite the criteria for COVID-19 case definition having been updated, initially PCR (polymerase chain reaction) laboratory confirmation was required. The initial statistics on the pandemic in Brazil represented a small fraction of the true situation, given that the PCR test was generally requested for hospitalized suspected COVID-19 cases and, in some places, as a post mortem confirmatory test. This criterion was later broadened to include case confirmation using clinical, clinical/epidemiological, clinical/imaging and laboratory parameters (the latter including molecular biology, immunological parameters and antigen testing).3
Studies that investigate and characterize COVID-19 mortality in more depth can contribute to understanding of the disease’s behavior in the population in different places. Such knowledge can lead to timely and appropriate interventions in the sense of avoiding this type of outcome. According to a study conducted to identify possible impacts of social isolation in Rondônia, as isolation restrictions were slackened, the number of cases and speed of transmission increased correspondingly, with a consequent increase in the number of deaths.4 Another relevant aspect is the spread of the pandemic to interior regions, as seen in a variety of places, such as in Rondônia, with considerable potential for affecting isolated populations, especially the indigenous.5
The objective of this study was to describe the characteristics of COVID-19 deaths in the state of Rondônia.
Methods
This is a descriptive cross-sectional study based on secondary data notified between January 1st and August 20th 2020.
It examines the expression of COVID-19 in the population of the state of Rondônia, based on the understanding that the SARS-CoV-2 pandemic can be better controlled when there is more knowledge about the local variables determining that expression. Rondônia has 52 municipalities. Its estimated population in 2020 is approximately 1,796,460 inhabitants, 50.4% of whom are aged between 10 and 39 years old. It is therefore a young and predominantly urban population.
The data on COVID-19 cases produced by the Municipal Health Departments are consolidated by the Rondônia State Health Department (SESAU-RO) and publicized through daily SESAU-RO bulletins.2 These data are included on the flu-like syndrome database available on the OpenDATASUS platform. The data used are derived from the e-SUS VE system, developed to record Flu-like syndrome cases suspected of having COVID-19. The system is comprised of notification form data and information on place of residence, as well as demographic and clinical/epidemiological characteristics of these cases.
This study used the database provided by SESAU-RO on its Coronavirus Portal, available at https://covid19.sesau.ro.gov.br/. The data were retrieved on August 28th 2020.6 The database is operated by the Ministry of Health, via its Health Surveillance Secretariat, based on incorporation of the e-SUS VE Notifica system, which has been in place since March 2020.
The study included all notified flu-like syndrome cases in the state of Rondônia between January 1st and August 20th 2020, twenty weeks after the first COVID-19 cases were recorded in the state
This study considered the following variables: age group (in years); sex (male; female); race/skin color (white; yellow [Asian]; indigenous; brown; or black); and outcome (death; non-death)
The data were treated using Excel, version 365. The chi-square test for K proportions was used to analyze comparisons between categories. These analyses were then submitted to the Marascuilo precedure,7 which works as a complement to the chi-square test with the aim of establishing which proportions had statistically significant differences between each other, two at a time, in groups with more than two components in which the chi-square test showed significant difference in the variables studied between the group members. Proportional mortality rates were also calculated for each age group and for sex, as well as between reported race/skin color categories. The statistical analyses were performed using the XLStat Excel supplement, assuming a 0.05 significance level.
The research project from which this article originated was submitted to the Federal University of Rondônia Health Sector Research Ethics Committee and was approved by it on May 29th 2020 (Certificate of Submission for Ethical Appraisal No. 32198620.7.0000.5300, Report No. 4.058.458).
Results
The sample studied was comprised of 184,146 suspected cases. Of these, 134,342 were considered not to have COVID-19 according to the case definition criteria in force at the time of notification. A total of 49,804 COVID-19 cases were confirmed. Seventy-three of the unconfirmed cases and 1,020 of the confirmed cases died, with a lethality rate of 0.05 and 2.05% respectively.
The general data, distributed according to age range, sex and race/skin color, are shown in Table 1. It should be noted that the results of the chi-square test for K proportions confirmed the existence of statistically significant differences between age groups and occurrence of death (chi-squared = 10371.123; p-value <0.001). Equal COVID-19 death distribution was found between males (82 – 47.1%) and females (92 – 52.9%) up to 40 years old. After this age, deaths were predominant among males (534/846 – 63.1%) in all age groups.
Table 1 – Distribution of notified flu-like syndrome cases according to COVID-19 confirmation, demographic variables, outcome (death or non-death) and lethality, Rondônia, 01/01/2020 – 20/08/2020
| Variable | Confirmed COVID-19 cases | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| No | Yes | |||||
|
| ||||||
| Death | Death | |||||
|
| ||||||
| No | Yes | Lethality (%) | No | Yes | Lethality (%) | |
| Age group (in years) | ||||||
|
| ||||||
| < 1 | 561 | 1 | 0.18 | 188 | 2 | 1.05 |
| 1 - 9 | 2,539 | 0 | 0.00 | 994 | 2 | 0.20 |
| 10 - 19 | 8,075 | 0 | 0.00 | 2,990 | 6 | 0.20 |
| 20 - 39 | 63,837 | 7 | 0.01 | 22,709 | 78 | 0.34 |
| 40 - 59 | 47,172 | 21 | 0.04 | 16,973 | 281 | 1.63 |
| 60 - 69 | 7,922 | 16 | 0.20 | 3,146 | 222 | 6.59 |
| 70 - 79 | 2,989 | 11 | 0.37 | 1,289 | 265 | 17.05 |
| 80 ou mais | 1,174 | 17 | 1.43 | 495 | 164 | 24.89 |
|
| ||||||
| Sex | ||||||
|
| ||||||
| Female | 73,900 | 24 | 0.03 | 26,282 | 394 | 1.48 |
| Male | 60,334 | 49 | 0.08 | 22,501 | 626 | 2.71 |
| Undefined or not informed | 35 | 0 | 0.00 | 1 | 0 | 0.00 |
|
| ||||||
| Race/skin color | ||||||
|
| ||||||
| Yellow | 17,302 | 6 | 0.03 | 6,974 | 106 | 1.50 |
| White | 33,065 | 18 | 0.05 | 10,882 | 183 | 1.65 |
| Indigenous | 983 | 3 | 0.30 | 831 | 12 | 1.42 |
| Brown | 70,704 | 39 | 0.06 | 26,101 | 597 | 2.24 |
| Black | 4,794 | 2 | 0.04 | 1,789 | 53 | 2.88 |
| Not informed | 7,421 | 5 | 0.07 | 2,207 | 69 | 3.03 |
|
| ||||||
| Grand total | 134,342 | 73 | 0.05 | 49,804 | 1,020 | 2.05 |
When applying the Marascuilo procedure in order to identify differences between age groups (Table 2 and Figure 1), greater lethality differences were found as age increased. The age groups above 60 years old had significant differences in relation to all the age groups younger than 60. The 40-59 age group had differences in relation to all the other age groups except the under-one-year-olds.
Table 2 – Results of the Marascuilo procedure, contrasting lethality between age groups, Rondônia, 01/01/2020 – 20/08/2020
| Age class | Proportion difference | Critical value |
|---|---|---|
| p(80 or over) | ||
|
| ||
| p(70 - 79)a | 0.601 | 0.106 |
| p(60 - 69)a | 0.793 | 0.094 |
| p(40 - 59)a | 0.855 | 0.092 |
| p(20 - 39)a | 0.863 | 0.092 |
| p(10 - 19)a | 0.866 | 0.092 |
| p(1 - 9)a | 0.866 | 0.093 |
| p(< 1)a | 0.864 | 0.093 |
|
| ||
| p(70 - 79) | ||
|
| ||
| p(60 - 69)a | 0.192 | 0.056 |
| p(40 - 59)a | 0.254 | 0.053 |
| p(20 - 39)a | 0.262 | 0.053 |
| p(10 - 19)a | 0.265 | 0.053 |
| p(1 - 9)a | 0.265 | 0.053 |
| p(< 1)a | 0.263 | 0.054 |
|
| ||
| p(60 - 69) | ||
|
| ||
| p(40 - 59)a | 0.062 | 0.018 |
| p(20 - 39)a | 0.070 | 0.018 |
| p(10 - 19)a | 0.072 | 0.018 |
| p(1 - 9)a | 0.073 | 0.018 |
| p(< 1)a | 0.070 | 0.021 |
|
| ||
| p(40 - 59) | ||
|
| ||
| p(20 - 39)a | 0.008 | 0.003 |
| p(10 - 19)a | 0.010 | 0.004 |
| p(1 - 9)a | 0.011 | 0.005 |
| p(< 1) | 0.008 | 0.011 |
|
| ||
| p(20 - 39) | ||
|
| ||
| p(10 - 19) | 0.003 | 0.003 |
| p(1 - 9) | 0.003 | 0.005 |
| p(< 1) | 0.001 | 0.011 |
|
| ||
| p(10 - 19) | ||
|
| ||
| p(1 - 9) | 0.000 | 0.005 |
| p(< 1) | 0.002 | 0.011 |
|
| ||
| p(1 - 9) | ||
|
| ||
| p(< 1 year) | 0.002 | 0.011 |
a) Difference with significant p(reference class).
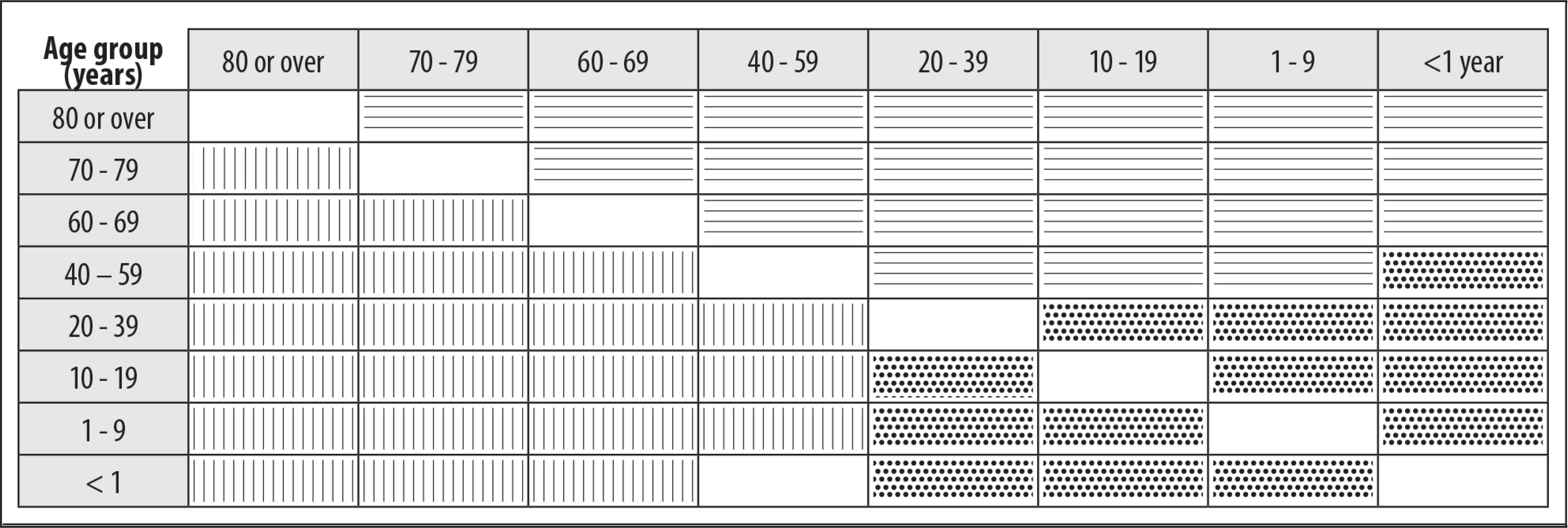
Figure 1 – Comparisons of COVID-19 lethality by age group, according to the Marascuilo procedure, Rondônia, 01/01/2020 – 20/08/2020Legend: Lethality is significantly greater for the age group row than for the corresponding age group column. Lethality is significantly less for the age group row than for the corresponding age group column . There is no significant difference between the age group row and the corresponding age group column.
When comparing deaths according to sex, all those recorded without their sex being defined were excluded (there were no deaths among those whose sex was recorded as being unknown), as they were insignificant in relation to the size of the notified samples of the male and female sex. When comparing lethality between males and females, a statistically significant difference was found in relation to sex, with greater probability of males dying than females: lethality rates of 2.71 and 1.48%, respectively (chi-squared = 93.391; p-value <0.001). The Marascuilo procedure was not necessary in this case as there were only two categories.
When comparing lethality according to race/skin color, we did not consider 2,276 notified COVID-19 cases for which there was no information on this variable. Sixty-nine COVID-19 deaths had no information on race/color and accounted for the largest proportion of lethality (3.03%); as for notifications that did have information on race/color, the highest proportion identified referred to Black people (2.88%). Notification forms with missing information may have resulted in possible limitations in the results of the statistical analyses presented here. Even so, the differences between lethality rates by race/skin color were tested and were found to be statistically significant between each other (chi-square = 32.139; p-value <0.001) in at least two categories.
The Marascuilo procedure produced the results presented in Table 3 and Figure 2. Bearing in mind the limitation of 69 deaths not having race/skin color identified, the chi-square test and the Marascuilo procedure only revealed significant difference for yellow (Asian) race/skin color in relation to brown and Black race/skin color, and for White race/skin color in relation to brown race/skin color. The differences were not statistically significant for the other strata.
Table 3 – Results of the Marascuilo procedure, contrasting race/skin color categories between each other, according to lethality, Rondônia, 01/01/2020 – 20/08/2020
| Race/skin color | Value | Critical value |
|---|---|---|
| p(yellow) | ||
|
| ||
| p(white) | 0.002 | 0.006 |
| p(indigenous) | 0.001 | 0.013 |
| p(brown)a | 0.007 | 0.005 |
| p(black)a | 0.014 | 0.013 |
|
| ||
| p(white) | ||
|
| ||
| p(indigenous) | 0.002 | 0.013 |
| p(brown)a | 0.006 | 0.005 |
| p(black) | 0.012 | 0.013 |
|
| ||
| p(indigenous) | ||
|
| ||
| p(brown) | 0.008 | 0.013 |
| p(black) | 0.015 | 0.017 |
|
| ||
| p(brown) | ||
|
| ||
| p(black) | 0.006 | 0.012 |
a) Difference with significant p(reference class).
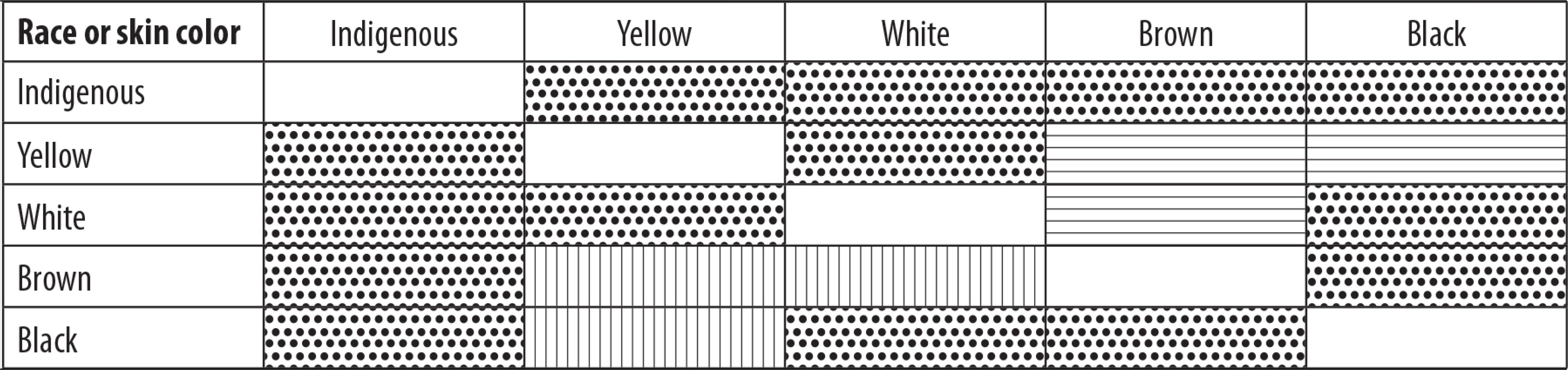
Figure 2 – Comparisons of the COVID-19 lethality by race/skin color categories, according to the Marascuilo procedure, Rondônia, 01/01/2020 – 20/08/2020Legend: Lethality is significantly greater for the race/skin categories color row than for the corresponding race/skin color categories column. Lethality is significantly less for the race/skin color categories row than for the corresponding race/skin color categories column. There is no significant difference between the race/skin color categories row and the corresponding race/skin color categories column.
Discussion
When analyzing COVID-19 lethality in Rondônia from the beginning of the pandemic until August 20th, we sought to identify differentials regarding deaths of confirmed COVID-19 cases and other SARS cases, between males and females, between age groups and between different races/skin colors.
Use of secondary data is a limitation of this study, especially when estimating underreporting and restrictive criteria for case confirmation. An important role in this sense is also played by the incompleteness of notification forms with regard to age, sex and race/skin color.
The difference between lethality among confirmed and unconfirmed COVID-19 cases is very evident, demonstrating greater COVID-19 lethality when compared to that of other flu-like diseases among the notified individuals. In Brazil as a whole, the mortality rate was 54.5 deaths per 100,000 inhabitants as at epidemiological week 34, while the rate in Rondônia was 59.7 and was higher than the Brazilian average.8
Higher COVID-19 lethality rates found repeatedly among older people and males also occur with regard to other flu-like diseases, according to data published in the Special Epidemiological Bulletin as at epidemiological week 34.8 The data analyzed in relation to the state of Rondônia demonstrated that COVID-19 lethality was greater, with statistical significance, among more elderly people in the over 60s age group.
This result is corroborated by European studies. Until recently, Europe was the epicenter of the epidemic and, as at epidemiological week 32, deaths were concentrated among people aged over 65 (89%).9 In China it has been demonstrated that people over 60 years old were at greater risk of death.11 In Mexico, a COVID-19 lethality rate of 6.53% was found in the population over 60 years old.12 Although in Brazil the age structure is not so old as in European countries, whereby elderly people account for 14.3% of the Brazilian population in 2020, nevertheless 52.7% of those aged 60 or over with COVID-19 have died.8 This may be associated with the comorbidity profile of this population, as well as factors related to access to health care, alongside lack of public policies on active integration of the elderly in society, with low availability of programs providing healthier lifestyles for this population, thus making them more susceptible to pandemic situations like this one.
Moreover, some authors13indicate that the mortality rate among elderly people tends to be nine times higher than among other age groups. This occurs principally because there is greater prevalence of comorbidities in this age range, resulting in greater complications and more severe forms of COVID-19, thus raising lethality among this segment of the population.
Although the lethality rate identified in this study for the population in the 20-39 and 40-49 age groups (0.3% and 1.6%, respectively) is not particularly pronounced when compared to that found in the population aged 60 and over (13.2%), nevertheless it draws attention and raises the hypothesis of association involving presence of comorbidities and chronic diseases in a population in which these conditions were not to be expected. The data of this study are in line with those of Costa et al.,13 identifying that in Brazil the younger population under 60 years old is presenting comorbidities that place it in the high risk group. In other words, people comprising the economically active age group are also exposed to death from COVID-19.
In general, mortality is lower among females than among males, among distinct populations, and from different causes.14 This pattern usually remains even during pandemics.15 In the Brazilian case, a greater number of cases has been observed among males during the COVID-19 pandemic, in which 57.9% of deaths relate to males. It is noteworthy that a similar result has been reported in Europe, with males being predominant among the number of deaths (58%).9 Lethality tends to be similar among males and females in age groups under 20 years old, while among people aged over 60, it is greater among males than among females.16 The present study found similar differences, with mortality predominating among males. Although more females are affected by COVID-19 (53.5% of cases), lethality is seen to be more intense among males (2.7%).
World Health Organization (WHO) data for Europe, Asia and North America indicate higher COVID-19 lethality among males, which may be explained by geographic, cultural and genetic factors.17 In Brazil, COVID-19 has presented a more female characteristic. There are signs that this happens, among other reasons, due to greater risk and exposure faced by health workers, the majority of whom are female, as well as their being on the frontline of efforts to mitigate the pandemic in diverse communities.16 Moreover, many women are the breadwinners of their homes, working on the informal labor market16 and need to move from one place to another in order to work.
Although these data are insufficient to demonstrate this situation, nevertheless they corroborate studies19 that indicate that there is difficulty in assessing whether individuals notified as being positive or diagnosed as having the disease were working, the places where they worked and the circumstances of their work, which might mean a delay in identifying potential sources of spread of infection related to work activities.
With regard to race/skin color, it falls to the different Brazilian National Health Service management levels to ensure this data is included on health information system forms. Providing this information became obligatory with effect from 2017.20Despite this, race/skin color was not among the categories used to analyze the COVID-19 epidemiological situation in the initial epidemiological bulletins. The race/skin color analysis category was only included in Health Ministry bulletins following complaints and pressure from civil society. Incompleteness of this variable is also found with regard to other health complaints, as well as among specific population groups, such as the elderly.21
Among the data reported in the Health Ministry’s Special Epidemiological Bulletin No. 288, it is stated that:
brown race/skin color is the most frequent among SARS deaths (57,290; 35.5%), followed by White (51,833; 32.1%), Black (8,662; 5.4%), yellow (1,840; 1.1%) and indigenous (563; 0.3%)". It is important to highlight that this information is missing for 18,499 (11.5%) deaths. The race/skin color profile for SARS deaths due to COVID-19 remained the same, with brown being the most frequent (40,537; 36.4%), followed by White (33,531; 30.1%), Black (5,899; 5.3%), yellow (1,279; 1.1%) and indigenous (455; 0.3%).
It is noteworthy that the 2019 National Household Sample Survey found that 42.7% of Brazilians self-reported themselves as being of White race/skin/color, 46.8% brown, 9.4% Black and 1.1% yellow or indigenous.23
The data notified in Rondônia do not differ from the situation portrayed in the Health Ministry Bulletin referred to above. Our study found that information on race/skin color was missing for almost 10,000 notifications, being the main potential source of bias in the analyses of race/skin color distribution. In relation to these cases with no information, 2,276 were people with COVID-19. Sixty-nine of them died, indicating 3.03% lethality. It should be noted that this is the highest rate among all the categories informed. Among the notifications that did have information on race/skin color, lethality was identified as being highest among Black people (2.9%), and this was statistically significant. Analysis comparing the different categories revealed significant difference only for yellow race/skin color in relation to brown and Black, as well as White race/skin color in relation to brown. In other words, COVID-19 affects people of brown and Black race/skin color more and is more lethal among them, thus emphasizing that COVID-19 in Brazil is very much “darker”.14 With regard to age and race/skin color distribution in Brazil, 50.7% of indigenous people are up to 29 years old, differing from those of White race/skin color (42.0%), Black (39.4%), brown (48.3%) and yellow (31.8%), whereas people aged over 60 account for 10.5% of indigenous people, 16.6% of people of White race/skin color, 14.8% Black, 11.9% brown and 25.5% yellow.24
Data on mortality according to cause of death need to be accurate and notification needs to be timely, in order for measures to control the spread of COVID-19 to be adequately defined, in addition to improving health service organization and management.7 This aspect is even more important given that there are estimates that for just one single death in a given place, there are probably countless unidentified cases of the disease among the population there.25
It is not the objective of this article to study the geographic distribution of COVID-19 deaths or cases. However, it should be highlighted that the distribution of Rondônia’s population is different to that of other places. Around a 1/3 of the population lives in Porto Velho,26 the state capital, and this is the municipality with the highest number of cases and deaths six months after the start of the pandemic. In addition to a considerable proportion of the population living there, other factors may interfere with the concentration of cases and deaths, especially the fact that the greater part of the state’s high complexity medical equipment is located in Porto Velho. Race/skin color distribution in Rondônia is different to that found for Brazil as a whole, above all with regard to the higher proportion of people of brown race/skin color (60.1% and 44.1%, respectively). The age pyramid is also different. There is a higher proportion of males than females: 50.6% in Rondônia and 48.9% in Brazil. Age group composition is also different: the proportion of young people up to 15 years old is 32.5% in Rondônia and 30.8% for Brazil as a whole, while the proportion of elderly people aged 65 or over also differs, being 8.9% and 14.2%, respectively.27 These characteristics may be determinants of the differentials with regard to disease and death found in Rondônia’s population.
In this study, the hypotheses of greater occurrence of deaths in older age groups, among males in relation to females, a higher percentage among people of brown and Black race/skin color, as well as much greater lethality among those infected with SARS-COV-2 in comparison with other etiologies, were statistically proven for the state of Rondônia.
REFERENCES
1. Ministério da Saúde (BR). Painel coronavirus [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 ago 28]. Disponível em: https://covid.saude.gov.br/ [ Links ]
2. Secretaria de Estado da Saúde de Rondônia. Boletim diário sobre coronavírus em Rondônia [Internet]. Rondônia: Secretaria de Estado da Saúde; 2020 [citado 2020 ago 28]. Disponível em: http://www.rondonia.ro.gov.br/edicao-162-boletim-diario-sobre-coronavirus-em-rondonia/ [ Links ]
3. Ministério da Saúde (BR). Definição de caso e notificação [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 ago 27]. Disponível em: https://coronavirus.saude.gov.br/index.php/definicao-de-caso-e-notificacao [ Links ]
4. Rodriguez TDM, Escobar AL. Taxa de variação diária da COVID-19: possível efeito das medidas de mitigação social [Internet]. Rondônia: Universidade Federal de Rondônia; 2020 [citado 2020 set 22]. Disponível em: http://www.coronavirus.unir.br/uploads/81688986/arquivos/impacto%20do%20isolamento%20social.pdf [ Links ]
5. Escobar AL. A interiorização da pandemia: potenciais impactos em populações em situação de vulnerabilidade na Amazônia. Revista NAU Social [Internet]. 2020 maio-out [citado 2020 nov 17];11(20):137-43. Disponível em: http://dx.doi.org/10.9771/ns.v11i20.36614 [ Links ]
6. Secretaria de Estado da Saúde de Rondônia. Boletim diário sobre coronavírus em Rondônia [Internet]. Rondônia: Secretaria de Estado de Saúde; 2020 [citado 2020 ago 28]. Disponível em: http://covid19.sesau.ro.gov.br/ [ Links ]
7. Marascuilo LA. Large-sample multiple comparisons. Psychol Bull [Internet]. 1996 May [cited 2020 Nov 17];65(5):280-90. Available from: https://doi.org/10.1037/h0023189 [ Links ]
8. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Doença pelo coronavírus COVID-19: semana epidemiológica 34 (16 a 22/08). Bol Epidemiol Esp [Internet]. 2020 ago [citado 2020 ago 28];28. Disponível em: http://antigo.saude.gov.br/images/pdf/2020/August/27/Boletim-epidemiologico-COVID-28-FINAL-COE.pdf [ Links ]
9. World Health Organization - WHO. COVID-19: WHO european region operational update epi weeks 31–32 (27 July–9 August) [Internet]. Geneva: World Health Organization; 2020 [cited 2020 Aug 28]. Available from: https://www.euro.who.int/__data/assets/pdf_file/0008/460196/COVID-19-operational-update-weeks-31-32-eng.pdf [ Links ]
10. Barbosa IR, Galvão MHR, Souza, TA, Gomes SM, Medeiros AA, Lima KC. Incidência e mortalidade por COVID-19 na população idosa brasileira e sua relação com indicadores contextuais: um estudo ecológico. Rev Bras Geriatr Gerontol [Internet]. 2020 [citado 2020 set 6] 23(1):200171. Disponível em: https://www.rbgg dições/edicoes/v23n1/RBGG%20v23n1%20PORT_2020-0171.pdf [ Links ]
11. Wu D, Wu T, Liu Q, Yang Z. The SARS-CoV-2 outbreak: what we know. Int J Infect Dis [Internet]. 2020 Mar [cited 2020 Nov 17];94:44-8. Available from: https://doi.org/10.1016/j.ijid.2020.03.004 [ Links ]
12. Bello-Chavolla OY, González-Díaz A, Antonio-Villa1 NE, Fermín-Martínez CA, Márquez-Salinas A, Vargas-Vázquez A, et al. Unequal impact of structural health 1 determinants and comorbidity on COVID-19 severity and lethality in older Mexican adults: Looking beyond chronological aging. J Gerontol A Biol Sci Med Sci [Internet]. 2020 [cited 2020 Sep 6];20(20):1–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7337730/pdf/glaa163.pdf [ Links ]
13. Costa JA, Silveira JA, Santos SCM, Nogueira PP. Implicações cardiovasculares em pacientes infectados com Covid-19 e a importância do isolamento social para reduzir a disseminação da doença. Arq Bras Cardiol [Internet]. 2020 maio [citado 2020 ago 28];114(5):834-8. Disponível em: http://dx.doi.org/10.36660/abc.20200243 [ Links ]
14. Kalache A, Silva A, Giacomin KC, Lima KC, Ramos LR, Louvison M, et al. Envelhecimento e desigualdades: políticas de proteção social aos idosos em função da pandemia Covid-19 no Brasil. Rev Bras Geriatr Gerontol [Internet]. 2020 [citado 2020 ago 28];23(6):e200122. Disponível em: https://doi.org/10.1590/1981-22562020023.200122 [ Links ]
15. Souza LG, Randow R, Siviero PCL. Reflexões em tempos de COVID-19: diferenciais por sexo e idade. Com Ciências Saúde [Internet]. 2020 [citado 2020 ago 28];31 Suppl 1:75-83. Disponível em: http://www.escs.edu.br/revistaccs/index.php/comunicacaoemcienciasdasaude/article/view/672/294 [ Links ]
16. Zarulli V, Jones JAB, Oksuzyan A, Lindahal-Jacobsen R, Christensen K, Vaupel JW. Women live longer than men even during severe famines and epidemics. Proc Natl Acad Sci USA [Internet]. 2018 Jan [cited 2020 Nov 17];115(4):E832-40. Available from: https://doi.org/10.1073/pnas.1701535115 [ Links ]
17. Salvati L, Biagioni B, Vivarelli E, Parronchi P. A gendered magnifying glass on COVID‑19. Clin Mol Allergy [Internet]. 2020 [cited 2020 Sep 09];18:14. Available from: https://doi.org/10.1186/s12948-020-00129-2 [ Links ]
18. Matos M. Pandemia COVID-19 e as mulheres. Bol Cientistas Sociais [Internet]. 2020 abr [citado 25 set 2020];11. Disponível em: http://www.anpocs.com/index.php/ciencias-sociais/destaques/2322-boletim-n-11-pandemia-covid-19-e-as-mulheres [ Links ]
19. Jackson Filho JM, Assunção AA, Algranti E, Garcia EG, Saito CA, Maeno M. A saúde do trabalhador e o enfrentamentissoa COVID-19. Rev Bras Saude Ocup [Internet]. 2020 [citado 2020 ago 28];45:e14. Disponível em: http://dx.doi.org/10.1590/2317-6369ed0000120 [ Links ]
20. Brasil. Ministério da Saúde. Portaria MS/GM n. 344, de 1º de fevereiro de 2017. Dispõe sobre o preenchimento do quesito raça/cor nos formulários dos sistemas de informação em saúde [Internet]. Diário Oficial da União, Brasília (DF), 2017 fev 2 [citado 2020 ago 28];Seção Extra:62. Disponível em: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2017/prt0344_01_02_2017.html [ Links ]
21. Romero DE, Maia L, Muzy J. Tendência e desigualdade na completude da informação sobre raça/cor dos óbitos de idosos no Sistema de Informações sobre Mortalidade no Brasil, entre 2000 e 2015. Cad. Saúde Pública [Internet]. 2019 [citado 2020 set 6];35(12):e00223218. Disponível em: https://scielosp.org/article/csp/2019.v35n12/e00223218/ [ Links ]
22. Santos MPA, Nery JS, Goes EF, Silva A, Santos AB, Batista LE, et al. População negra e Covid-19: reflexões sobre racismo e saúde. Estud Av [Internet]. 2020 maio-ago [citado 2020 ago 28];34(99):225-44. Disponível em: http://dx.doi.org/10.1590/s0103-4014.2020.3499.014 [ Links ]
23. Instituto Brasileiro de Geografia e Estatística - IBGE. Conheça o Brasil: raça ou cor [Internet]. Rio de Janeiro: IBGE; 2020 [citado 2020 set 24]. Disponível em: https://educa.ibge.gov.br/jovens/conheca-o-brasil/populacao/18319-cor-ou-raca.html [ Links ]
24. Instituto de Pesquisa Econômica Aplicada – IPEA (BR). Retratos das desigualdades de gênero e raça [Internet]. Brasília: IPEA; 2020 [citado 24 set 2020]. Disponível em: https://www.ipea.gov.br/retrato/indicadores_populacao.html [ Links ]
25. Jombart T, Zandvoort K, Russell T, Jarvis C, Gimma A, Abbott S, et al. Inferring the number of COVID-19 cases from recently reported deaths. medRxiv [Internet]. 2020 [cited 2020 Nov 17]. Available from: https://doi.org/10.1101/2020.03.10.20033761 [ Links ]
26. Instituto Brasileiro de Geografia e Estatística - IBGE. Cidades: 2020 [Internet]. Rio de Janeiro: IBGE; 2020 [citado 2020 set 24]. Disponível em: https://cidades.ibge.gov.br/brasil/ro/panorama [ Links ]
27. Instituto Brasileiro de Geografia e Estatística - IBGE. Projeção da população do Brasil e das Unidades da Federação [Internet]. Rio de Janeiro: IBGE; 2020 [citado 2020 set 24]. Disponível em: https://www.ibge.gov.br/apps/populacao/projecao/index.html?utm_source=portal&utm_medium=popclock&utm_campaign=novo_popclock [ Links ]
Received: September 11, 2020; Accepted: October 11, 2020











 texto em
texto em 
 Curriculum ScienTI
Curriculum ScienTI

