Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.1 Brasília 2021 Epub 07-Dic-2020
http://dx.doi.org/10.1590/s1679-49742021000100023
Original article
COVID-19: a cross-sectional study of suspected cases admitted to a federal hospital in Rio de Janeiro, Brazil, and factors associated with hospital death
1Hospital Federal dos Servidores do Estado, Serviço de Epidemiologia, Rio de Janeiro, RJ, Brazil
2Universidade Federal do Rio de Janeiro, Instituto de Estudos em Saúde Coletiva, Rio de Janeiro, RJ, Brazil
Objective
To describe the clinical and epidemiological profile of suspected COVID-19 cases admitted to a federal hospital in Rio de Janeiro, RJ, Brazil, and to identify factors associated with death.
Methods
This was a cross-sectional study using local epidemiological surveillance data as at epidemiological week 27 of 2020 and logistic regression.
Results
376 hospitalized suspected COVID-19 cases were included; 52.9% were female, 57.4% were 50 years old or over and 80.1% had comorbidities. 195 (51.9%) COVID-19 cases were confirmed and their lethality was higher (37.9%) than among discarded cases (24.2%). In the adjusted analysis, death among confirmed cases was associated with being in the 50-69 age group (OR=11.65 – 95%CI 1.69;80.33), being aged 70 or over (OR=8.43 – 95%CI 1.22;58.14), presence of neoplasms (OR=4.34 – 95%CI 1.28;14.76) and use of invasive ventilatory support (OR=70.20 - 95%CI 19.09;258.19).
Conclusion
High prevalence of comorbidities and lethality was found; the main factors associated with death were being older, neoplasms and invasive ventilatory support.
Key words: Coronavirus Infections; Severe Acute Respiratory Syndrome; Hospital Mortality; Epidemiology; Pandemics; Cross-Sectional Studies
Introduction
Having spread from the Chinese province of Hubei in December 2019 and reached a further 196 countries, the current COVID-19 pandemic, as declared by the World Health Organization (WHO) on March 11th 2020, poses critical challenges for Public Health and the international scientific community.1 In general, betacoronavirus infections have mild progression; however, lethality rates of between 10% and 37% were found in the Severe Acute Respiratory Syndrome epidemic in 2002/2003 and in the Middle East Respiratory Syndrome (MERS) epidemic in 2012.4 Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection causes Coronavirus Disease 2019 (COVID-19) and can behave like flu-like syndrome (FLS) or progress to more severe forms characterized as severe acute respiratory syndrome (SARS).2
In Brazil, community transmission of SARS-CoV-2 was recognized by the Ministry of Health, initially in the municipalities of São Paulo and Rio de Janeiro, and later throughout the national territory, with effect from March 20th 2020.8As at September 19th 2020, WHO had recorded 30,370,875 confirmed COVID-19 cases and 948,797 deaths.2 In the same period, Brazil had 4,528,240 confirmed cases and 136,532 deaths, with a 3.0% lethality rate, coming in second place worldwide with regard to the national number of COVID-19 cases and deaths.10 As at the same date (19/9/2020), the state of Rio de Janeiro had recorded 251,261 confirmed cases and 17,634 deaths, with a 7.0% lethality rate.10 These figures are potentially underestimated due to underreporting and the shortfall in availability of mass laboratory testing.9
As at July 18th, a total of 441,194 SARS cases had been notified nationwide, 48.4% of which were confirmed as COVID-19 cases. Of the total of 115,654 SARS deaths in the period, 66.1% were confirmed as being COVID-19 cases. The majority of deaths due to SARS COVID-19 occurred among males (58.2%), people between 70 and 79 years old (25.0%), and people with associated comorbidities, in particular heart disease, diabetes mellitus and kidney disease.13
When describing the clinical and epidemiological profile of confirmed COVID-19 cases and factors associated with their severity and death, recent studies have shown variability, even when taking into consideration differences in the time periods analyzed, sample sizes and data standardization.3 Notwithstanding the majority of cases having favorable prognosis, it is acknowledged that there is relative consensus that elderly individuals and people with underlying chronic conditions can have a poorer prognosis.With regard to social issues, unequal distribution of conditions such as access to health care and treatment, type of work, housing and sanitation affects the spread of the pandemic in Brazil.12
In view of this pandemic emergency and its huge impact on Public Health, epidemiological surveillance takes on a fundamental role, not only with regard to case notification, investigation and closure, but also with regard to identifying the characteristics of the affected population and factors associated with greater severity and lethality of the new disease, thus contributing to planning of care and actions to address the pandemic.
The objective of this study was to describe the clinical and epidemiological profile of suspected COVID-19 cases admitted to a federal hospital located in the municipality of Rio de Janeiro and to identify factors associated with death.
Methods
This was a cross-sectional observational study using epidemiological surveillance data from the Hospital Federal dos Servidores do Estado (HFSE) in Rio de Janeiro, RJ, starting with the first suspected notified COVID-19 case admitted to the hospital on March 5th 2020 through to July 4th 2020 at the end of epidemiological week 27.
The HFSE is a general and a teaching hospital, as well as being a high complexity reference unit for several specialties, including high risk pregnancy. It is located in the municipality of Rio de Janeiro and is part of the Hospital Epidemiological Surveillance Network of National Interest. The HFSE has capacity for 398 hospital beds; however, during the study period it operated with 200 beds on average, in particular because of the impact of human resources being on leave from work due to the pandemic.
The study included all hospitalized cases that met the SARS and FLS criteria as defined by the Ministry of Health, notified on specific SARS and FLS forms. Either the Reverse-Transcriptase Polymerase Chain Reaction (RT-PCR) laboratory criterion or the clinical/epidemiological criterion were used for confirmation of COVID-19 cases.8
The independent variables analyzed were:
sex (female; male);
age (years: up to 19; 20-49; 50-69; 70 or over);
case closure (COVID-19 case confirmed, discarded or under investigation);
presence of comorbidity (yes or no, for each category: cardiovascular disease, diabetes mellitus, neoplasm, obesity, chronic neurological disease, chronic lung disease, chronic blood disorder, chronic liver disease, human immunodeficiency virus (HIV) infection);
use of intensive care (ICU: yes; no);
ventilatory support (invasive; non-invasive; no support);
results of an ordinary chest x-ray or computerized tomography of the chest (with or without ground glass imaging).
The outcome analyzed was hospital death or otherwise, as at the data of the end of the study period.
The HFSE Epidemiology Service uses a local database comprised of epidemiological investigation forms filled in on an electronic spreadsheet. That database was used for this study.
Bivariate and multiple descriptive analysis was performed using logistic regression with the aid of the SPSS version 18 computer program in order to study factors associated with hospital death. Pearson’s chi-square test or Fisher’s exact test were used in the crude analysis of the categorical variables. A p-value <0.05 was considered to be statistically significant. Variables showing association with death in the crude analysis (p<0.10) and variables considered to be of clinical importance were included in the logistic regression. We studied two models: model 1 took into consideration all hospitalized suspected cases; while model 2, only took into consideration confirmed COVID-19 cases. We used the enter method, Wald’s test for independent variable significance, agreement analysis and the Hosmer-Lemeshow test. Odds ratios (OR) and their 95% confidence intervals (95%CI) were used in order to estimate probability of death.
Considering the total sample of cases, an outcome prevalence ratio between groups with or without the variable of interest equal to 1.8 (in the case of neoplasms) and a difference of 22% in the distribution of the outcome between these groups, statistical power was estimated as being 92%. Taking the set of confirmed cases and using similar parameters, power was 67%.
This study is part of the larger study entitled ‘Epidemiological surveillance and clinical/epidemiological profile of cases with compulsorily notifiable health conditions cared for at the Hospital Federal dos Servidores do Estado since its Epidemiology Service was set up’, approved by the HFSE Research Ethics Committee on July 14th 2014: Detailed Report No. 000.534
Results
During the study period, 1482 suspected COVID-19 cases were notified at the HFSE. Figure 1 shows the participant definition process flowchart. This study included all 376 hospitalized cases, 361 (96.0%) of which met the SARS criteria. Monthly distribution of notifications made up until July 4th 2020 was as follows: March, 13 (3.5%); April, 79 (21.0%); May, 157 (41.8%); June, 116 (30.9%); and July, 11 (2.9%). The time interval between symptom onset and notification varied from less than 24 hours to 51 days, with a median interval of 4 days.
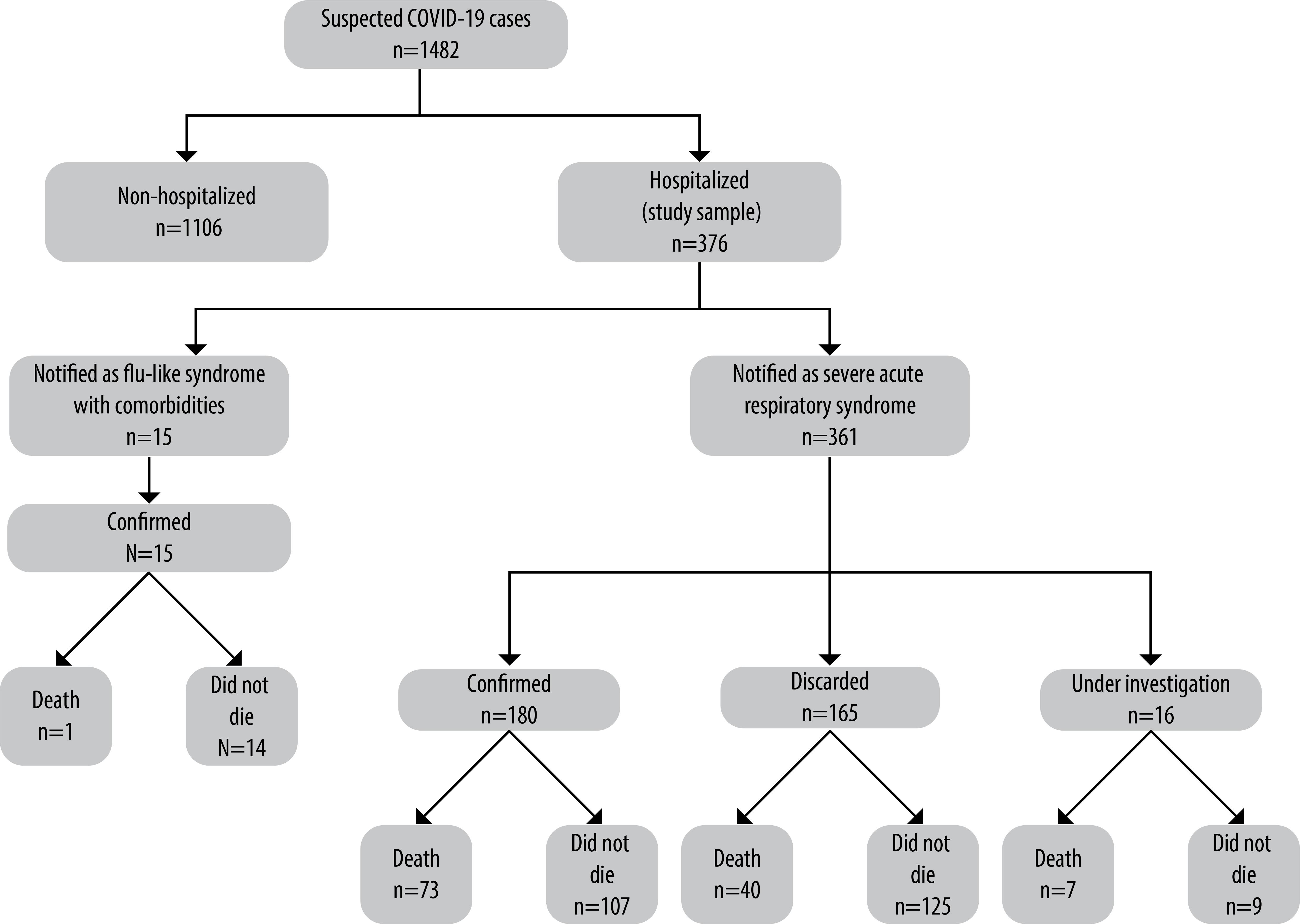
Figure 1 – Flowchart of participants in study of suspected COVID-19 cases according to notification criterion, confirmed diagnosis of the disease and its progression, hospitalized at the Hospital Federal dos Servidores do Estado, Rio de Janeiro, March 5th 2020 – July 4th 2020
Two hundred and seventy five (73.1%) cases suspected of having COVID-19 attended HFSE for treatment of other diseases, 229 (83.3%) of whom were outpatients and 46 of whom (16.7%) were inpatients; 92 (24.5%) were referred by the hospital bed control service and 9 (2.4%) were hospital staff. Of the 92 cases referred by the hospital bed control service, 21 (22.8%) were identified as COVID-19 patients and 71 (77.2%) as patients with other diseases; 43 (60.6%) of these were confirmed as having COVID-19 at the HFSE, with onset of symptoms compatible with infection at the hospital service where they were being treated beforehand.
One hundred and ninety five (51.9%) cases were confirmed as having COVID-19, 181 (92.8%) of whom were laboratory-confirmed while 14 (7.2%) were confirmed according to clinical/epidemiological criteria (all of the latter had suggestive radiology images); 165 cases (43.9%) were discarded and 16 (4.3%) were under investigation at the end of the study period.
Table 1 shows the profile of notified cases according to COVID-19 diagnosis confirmation. Females were predominant (52.9%). Eighty (40.2%) of these women were of childbearing age, 18 (22.5%) of whom were pregnant and 6 (7.5%) of whom were in the postpartum period, whereby 11 (61.1%) and 3 (50.0%), respectively, were confirmed as having COVID-19. Eighteen (75.0%) of the pregnant and postpartum women were high risk, with predominance of cardiovascular disease (8; 33.3%), obesity (6; 25.0%) and diabetes mellitus (3;12.5%); none of them died.
Table 1 – Clinical and epidemiological profile of hospitalized suspected COVID-19 cases (n=376), according to COVID-19 diagnosis, at the Hospital Federal dos Servidores do Estado, Rio de Janeiro, March 5th 2020 – July 4th 2020
| Variable | Confirmed COVID-19 n (%) | Discarded COVID-19 n (%) | Under investigation N (%) | Total n (%) | p-valuea |
|---|---|---|---|---|---|
| Sex | 0.009 | ||||
|
| |||||
| Female | 112/195 (57.4) | 84/165 (50.9) | 3/16 (18.8) | 199/376 (52.9) | |
| Male | 83/195 (42.6) | 81/165 (49.1) | 13/16 (81.3) | 177/376 (47.1) | |
|
| |||||
| Age group (years) | 0.001 | ||||
|
| |||||
| ≤19 | 15/195 (7.7) | 41/165 (24.8) | 1/16 (6.3) | 57/376 (15.2) | |
| 20-49 | 60/195 (30.8) | 38/165 (23.0) | 5/16 (31.3) | 103/376 (27.4) | |
| 50-69 | 67/195 (34.4) | 51/165 (30.9) | 5/16 (31.3) | 123/376 (32.7) | |
| ≥70 | 53/195 (27.2) | 35/165 (21.2) | 5/16 (31.3) | 93/376 (24.7) | |
|
| |||||
| Comorbidity (at least 1) | 162/195 (83.1) | 127/165 (77.0) | 12/16 (75.0) | 301/376 (80.1) | 0.308 |
|
| |||||
| Cardiovascular disease | 93/195 (47.7) | 53/165 (32.1) | 5/11 (45.5) | 151/376 (40.2) | 0.008 |
| Diabetes mellitus | 65/195 (33.3) | 27/165 (16.4) | 3/16 (18.8) | 95/376 (25.3) | 0.001 |
| Neoplasm | 25/195 (12.8) | 30/165 (18.2) | 6/16 (37.5) | 61/376 (16.2) | 0.024 |
| Obesity | 19/195 (9.7) | 9/165 (5.5) | 1/16 (6.3) | 29/376 (7.7) | 0.307 |
| Chronic neurological disease | 11/195 (5.6) | 18/165 (10.9) | 0/16 (0.0) | 29/376 (7.7) | 0.087 |
| Chronic kidney disease | 11/195 (5.6) | 9/165 (5.5) | 1/16 (6.3) | 21/376 (5.6) | 0.990 |
| Chronic lung disease | 10/195 (5.1) | 18/165 (10.9) | 0/16 (0.0) | 28/376 (7.4) | 0.058 |
| Blood disorder | 10/195 (5.1) | 13/165 (7.9) | 1/16 (6.3) | 24/376 (6.4) | 0.568 |
| Chronic liver disease | 6/195 (3.1) | 8/165 (4.8) | 0/16 (0.0) | 14/376 (3.7) | 0.489 |
| HIV infectionb | 5/195 (2.6) | 6/165 (3.6) | 0/16 (0.0) | 11/376 (2.9) | 0.649 |
|
| |||||
| Use of ICUc | 88/195 (45.1) | 53/165 (32.1) | 3/16 (18.8) | 144/376 (38.3) | 0.011 |
|
| |||||
| Ventilatory supportc | 0.007 | ||||
|
| |||||
| Invasive | 60/191 (31.4) | 27/165 (16.4) | 2/16 (12.5) | 89/372 (23.9) | |
| Non-invasive | 69/191 (36.1) | 67/165 (40.6) | 5/16 (31.3) | 141/372 (37.9) | |
| No support | 62/191 (32.5) | 71/165 (43.0) | 9/16 (56.3) | 142/372 (38.2) | |
|
| |||||
| Ground glass imaging | <.001 | ||||
|
| |||||
| Yes | 92/195 (47.2) | 21/165 (12.7) | 4/16 (25.0) | 117/376 (31.1) | |
| No | 60/195 (30.8) | 53/165 (32.1) | 7/16 (43.8) | 120/376 (31.9) | |
| Not performed/unknown | 43/195 (22.1) | 91/165 (55.2) | 5/16 (31.3) | 139/376 (37.0) | |
|
| |||||
| Death | 74/195 (37.9) | 40/165 (24.2) | 7/16 (43.8) | 121/376 (32.2) | 0.013 |
a) Pearson’s chi-square test p-value.
b) HIV: human immunodeficiency virus.
c) ICU: intensive care unit.
d) 4 cases with no information on ventilatory support were excluded.
The age of the cases varied between under 1 year old and 94 years old, with median age being 55 years. Age distribution was heterogeneous between confirmed and discarded cases; the percentage of confirmed child and adolescent cases was approximately one third of the percentage of them among discarded cases. Presence of comorbidities was high in all age groups, including the up to 19 year-old age group, in which 73.7% (42/76) had at least one comorbidity. Taking all the age groups for confirmed cases, 83.1% had at least one comorbidity, whereby cardiovascular disease, diabetes mellitus and neoplasms were predominant.
ICU use occurred in 45.1% of confirmed cases and was significantly greater than among discarded cases. Likewise, use of invasive ventilatory support was significantly greater among confirmed cases. With regard to imaging examinations, for 119 cases (31.6%) they were not performed or there was no information on the result as at the end of the study. Among confirmed cases, 92 of the 152 who had examinations (60.5% excluded because the result was unknown) had a ground glass pattern considered to be suggestive of coronavirus infection. However, ground glass imaging was also described in some of the discarded cases, especially those with lung neoplasms.
Overall lethality was 32.2%, while it was 37.9% among confirmed cases versus 24.2% among discarded cases (p=0.013); lethality was very high among cases which were still under investigation.
Table 2 shows the progression of notified cases (death; did not die) according to the variables analyzed. Likelihood of death was higher among males and people in older age groups. COVID-19 confirmation was associated with greater lethality, in relation to discarded cases (OR=2.52 – 95%CI1.60;3.96). With regard to comorbidities, these were significantly associated with greater lethality in the presence of neoplasms (OR=2.58 – 95%CI 1.48;4.52) and chronic liver disease (OR=4.02 – 95%CI 1.32;12.26). Prior presence of chronic lung disease was associated with lower lethality; eight of these cases had asthma and none of them died.
Table 2 – Progression of hospitalized suspected COVID-19 cases (n=376), according to selected variables, at the Hospital Federal dos Servidores do Estado, Rio de Janeiro, March 5th 2020 – July 4th 2020
| Variable | Death | Did not die | p-valuea | ORb (95%CIc) |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Sex | 0.028 | |||
|
| ||||
| Female | 54/199 (27.1) | 145/199 (72.9) | 1.00 | |
| Male | 67/177 (37.9) | 110/177 (62.1) | 1.64 (1.06;2.53) | |
|
| ||||
| Age group (years) | <0.001 | |||
|
| ||||
| ≤19 | 6/57 (10.5) | 51/57 (89.5) | 1.00 | |
| 20-49 | 19/103 (18.4) | 84/103 (81.6) | 1.92 (0.70;5.13) | |
| 50-69 | 48/123 (39.0) | 75/123 (61.0) | 5.44 (2.17;13.65) | |
| ≥70 | 48/93 (51.6) | 45/93 (48.4) | 9.07 (3.55;23.18) | |
|
| ||||
| COVID-19 diagnosis | 0.013 | |||
|
| ||||
| Confirmed | 74/195 (37.9) | 121/195 (62.1) | 2.52 (1.60;3.96) | |
| Discarded | 40/165 (24.2) | 125/165 (75.8) | 1.00 | |
| Under investigation | 7/16 (43.8) | 9/16 (56.3) | 3.20 (1.13;9.14) | |
|
| ||||
| Notified condition | 0.044h | |||
|
| ||||
| SARSd | 120/361 (33.2) | 241/361 (66.8) | 6.97 (0.91;53.64) | |
| FLSe with comorbidity | 1/15 (6.7) | 14/15 (93.3) | 1.00 | |
|
| ||||
| Cardiovascular disease | 0.135 | |||
|
| ||||
| Yes | 54/151 (35.8) | 97/151 (64.2) | 1.31 (0.85;2.04) | |
| No | 67/225 (29.8) | 158/225 (70.2) | 1.00 | |
|
| ||||
| Diabetes mellitus | 0.106 | |||
|
| ||||
| Yes | 36/95 (37.9) | 59/95 (62.1) | 1.41 (0.87;2.29) | |
| No | 85/281 (30.2) | 196/281 (69.8) | 1.00 | |
|
| ||||
| Neoplasm | 0.001 | |||
|
| ||||
| Yes | 31/61 (50.8) | 30/61 (49.2) | 2.58 (1.48;4.52) | |
| No | 90/315 (28.6) | 225/315 (71.4) | 1.00 | |
|
| ||||
| Chronic lung disease | 0.003 | |||
|
| ||||
| Yes | 2/28 (7.1) | 26/28 (92.9) | 0.15 (0.04;0.63) | |
| No | 119/348 (34.2) | 229/348 (65.8) | 1.00 | |
|
| ||||
| Chronic liver disease | 0.016 | |||
|
| ||||
| Yes | 9/14 (64.3) | 5/14 (35.7) | 4.02 (1.32;12.26) | |
| No | 112/362 (30.9) | 250/362 (69.1) | 1.00 | |
|
| ||||
| Use of ICU f | <0.001 | |||
|
| ||||
| Yes | 69/144 (47.9) | 75/144 (52.1) | 3.19 (2.03;4.99) | |
| No | 52/232 (22.4) | 180/232 (77.6) | 1.00 | |
|
| ||||
| Ventilatory supportg | <0.001 | |||
|
| ||||
| Invasive | 66/89 (74.2) | 23/89 (25.8) | 21.10 (10.54;42.25) | |
| Non-invasive | 35/141 (24.8) | 106/141 (75.2) | 2.49 (1.29;4.58) | |
| No support | 17/142 (12.0) | 125/142 (88.0) | 1.00 | |
|
| ||||
| Ground glass imaging | 0.005 | |||
|
| ||||
| Yes | 50/117 (42.7) | 67/117 (57.3) | 2.40 (1.40;4.10) | |
| No | 33/139 (23.7) | 106/139 (76.3) | 1.00 | |
| Not performed/unknown | 38/120 (31.7) | 82/120 (68.3) | 1.49 (0.86;2.58) | |
a) Pearson’s chi-square test p-value, except when other specified.
b) OR: odds ratio.
c) 95%CI: 95% confidence interval.
d) SARS: severe acute respiratory syndrome.
e) FLS: flu-like syndrome.
f) ICU: intensive care unit.
g) 4 cases with no information on ventilatory support were excluded.
h) Fisher’s exact test p-value.
Use of ICU, use of some form of ventilatory support and radiology images with ground glass patterns were also significantly related to a poorer prognosis.
Table 3 shows the results of the multivariate models. Including SARS or FLS did not change the models, remembering that 96.0% of the sample accounted for SARS. In Model 1, containing all the cases included in the analysis, the variables associated with a significantly higher likelihood of death were the ≥50 years age group (with an increasing effect as age increased, taking ≤19 years as a reference), presence of neoplasms (OR=3.47 – 95%CI1.69;7.13)and use of some form of ventilatory support (especially invasive support: OR=23.65 – 95%CI10.55;53.02). Presence of lung diseases was associated with a significantly lower probability of death (OR=0.13 – 95%CI 0.02;0.72). The effect of being of the male sex was of borderline significance in increasing likelihood of death. COVID-19 diagnosis confirmation lost statistical significance, probably due to the fact of discarded cases and cases under investigation also having high prevalence of comorbidities.
Table 3 – Multiple logistic regression analysis of factors associated with death among hospitalized suspected COVID-19 cases (n=376) and confirmed cases (n=195), at the Hospital Federal dos Servidores do Estado, Rio de Janeiro, Rio de Janeiro State, March 5th 2020 – July 4th 2020
| Model/variable | Crude odds ratio | 95%CIa | Adjusted odds ratio | 95%CIa | p-valueb |
|---|---|---|---|---|---|
| Model 1: all cases (agreement: 80.6%) | |||||
|
| |||||
| Sex male (reference: female) | 1.64 | 1.06;2.53 | 1.78 | 1.00;3.15 | 0.051 |
|
| |||||
| Age group (reference: ≤19 years) | |||||
|
| |||||
| 20-49 | 1.92 | 0.70;5.13 | 2.76 | 0.86;8.83 | 0.088 |
| 50-69 | 5.44 | 2.17;13.65 | 6.39 | 2.13;19.11 | 0.001 |
| ≥70 | 9.07 | 3.55;23.18 | 8.18 | 2.65;25.20 | 0.000 |
|
| |||||
| Neoplasm (reference: no) | 2.58 | 1.48;4.52 | 3.47 | 1.69;7.13 | 0.001 |
|
| |||||
| Chronic lung disease (reference: no) | 0.15 | 0.04;0.63 | 0.13 | 0.02;0.72 | 0.020 |
|
| |||||
| Ventilatory support (reference: none) | |||||
|
| |||||
| Invasive | 21.10 | 10.54;42.25 | 23.65 | 10.55;53.02 | 0.000 |
| Non-invasive | 2.49 | 1.29;4.58 | 2.02 | 1.01;4.05 | 0.049 |
|
| |||||
| Confirmed COVID-19 (reference: no) | 2.52 | 1.60;3.96 | 1.09 | 0.61;1.95 | 0.784 |
|
| |||||
| Model 2: only confirmed COVID-19 cases (agreement: 84.8%) | |||||
|
| |||||
| Sex male (reference: female) | 1.63 | 0.91;2.93 | 1.39 | 0.60;3.24 | 0.439 |
|
| |||||
| Age group (reference: ≤19 years) | |||||
|
| |||||
| 20-49 | 1.63 | 0.32;8.19 | 3.22 | 0.45;23.32 | 0.246 |
| 50-69 | 4.67 | 0.97;22.34 | 11.65 | 1.69;80.33 | 0.013 |
| ≥70 | 9.90 | 2.03;48.44 | 8.43 | 1.22;58.14 | 0.031 |
|
| |||||
| Neoplasm (reference: no) | 2.82 | 1.19;6.67 | 4.34 | 1.28;14.76 | 0.019 |
|
| |||||
| Ventilatory support (reference: none) | |||||
|
| |||||
| Invasive | 57.00 | 18.25;180.00 | 70.20 | 19.09;258.19 | 0.000 |
| Non-invasive | 3.44 | 1.18;10.05 | 3.05 | 0.96;9.77 | 0.060 |
a) 95%CI: 95% confidence interval.
b) Wald test p-value.
Note: Values adjusted for all variables included in the models.
Model 2 only included the 195 confirmed COVID-19 cases. Significant association remained in this model with regard to increased probability of death among the 50-69 age group (OR=11.65 – 95%CI1.69;80.33) and the 70 or over age group (OR=8.43 – 95%CI1.22;58.14), presence of neoplasm (OR=4.34 – 95%CI 1.28;14.76) and use of invasive ventilatory support (OR=70.20 – 95%CI 19.09;258.19). Being of the male sex and use of non-invasive ventilatory support were associated with greater probability of death, although this was not statistically significant. Among the confirmed cases, ten had lung disease and none of these died; the effect lost its statistical significance.
Discussion
In this study, suspected COVID-19 cases hospitalized at the HFSE were for the most part female, aged 50 or over, people who had comorbidities, and patients already being treated at the hospital. Among confirmed cases, use of ICU and invasive ventilatory support was significantly greater than among other cases. Lethality was also higher among confirmed cases when compared to discarded cases. Factors associated with death in cases diagnosed as having COVID-19 were age ≥50 years, presence of neoplasms and use of invasive ventilatory support.
The majority of cases were notified based on identification of SARS criteria, both for spontaneous health service notification and also for active tracing by the HFSE Epidemiology Service. Spontaneous notification was often linked to the need to fill in the notification form in order to be able to perform PCR for SARS-Cov-2. During the investigation, 195 confirmed cases and 165 discarded cases were classified. The latter were for the most part unspecified SARS cases, and no assessment was done for other viruses. With regard to cases ‘under investigation’ at the end of the study, they had high lethality and may meet COVID-19 criteria when the epidemiological investigation is concluded. This context exemplifies the importance of making differential diagnosis available quickly, given that initially all notified cases required COVID-19 care safety protocols to be followed, which is related to greater cost and greater strain on health care teams.8
Among the findings, age group distribution was consistent with diverse international and national studies which reported median or average age above 50 years old.8 When elderly people are infected with SARS-Cov-2, they have greater risk of progressing to complicated forms of the disease and may need to be hospitalized.8
Variations were found with regard to sex. Males were predominant is some studies conducted in China, Italy, Spain, United Kingdom and the United States.7 Similarly, 55% of suspected notified cases hospitalized as at epidemiological week 29 in Brazil were of the male sex.13 Nevertheless, other studies have described greater frequency among females among both suspected and confirmed cases.19 The predominance of females at the HFSE and cases among pregnant women may be related to the profile of the hospital as a reference service for high risk pregnancies.27
With regard to presence of comorbidities, which was very high in this study, great variation was found in the literature we consulted, ranging from 25% of cases in a Chinese study14 to 60.5% of cases hospitalized in ICUs in Italy25 and 77% of hospitalized cases in the United Kingdom;18 and even around 94% of cases hospitalized in New York and Detroit in the United States.17 In Brazil, among cases that had died as at epidemiological week 29, The Ministry of Health reported that 61% had at least one comorbidity, with heart disease and diabetes mellitus being the most frequent.13
Generally speaking, the corbidities most mentioned in the publications we reviewed were cardiovascular diseases, arterial hypertension, diabetes mellitus, obesity, respiratory diseases, chronic kidney disease and cancer.15Al these conditions are related to greater risk of COVID-19 complications and may coexist in a single individual. Existence of more than one comorbidity is associated with even greater risk of an unfavorable prognosis.8
The most frequent comorbidity in this study was cardiovascular disease, this being a finding consistent with the reports of various authors,14 even though there is great variation between them, including with regard to whether or not arterial hypertension is included among these cases (we included it in this study). Prevalence of diabetes mellitus in confirmed cases was close to that found by North American studies (33.8 to 38.4%),17 higher than that found in the United Kingdom (28.1%)18and much higher than the estimate for the general Brazilian adult population (6.2%).21 Percentage obesity among confirmed cases was close to that reported in the United Kingdom (10.5%)18 but considerably lower than that found in the above mentioned study in New York (41.7%).17 In our study, this condition may have been underrecorded in view of the difficulty in assessing its presence at the time care was provided and value not being placed on its diagnosis within the context of SARS notification.
Neoplasm prevalence among confirmed cases was double that reported in the New York study (6%)17 and close to that reported in the United Kingdom (10.0%).18 HIV/AIDS infection frequency of 2.9% is higher than that reported by those studies (0.8% and 0.5% respectively)17 and may be related to the profile of the HFSE, which is also a reference service for HIV/AIDS cases.27
When analyzing hospitalization in the ICU and use of mechanical ventilation, the percentages found among confirmed cases were higher than those registered in the United Kingdom (17% and 10.0% respectively)18 and in New York (14.2% and 12.2% respectively),17while being close to those found in Detroit (39.7% and 32.1% respectively).19 The cases cared for at the HFSE were found to have high comorbidity presence and overlapping comorbidities, which may have contributed to worse clinical progression of SARS-Cov-2 infection and, consequently, greater need for intensive support.
Lethality among the total cases analyzed was high and was above the overall lethality for suspected hospitalized cases notified in Brazil as at epidemiological week 29 (26.2%), although it was close to the lethality rate of suspected hospitalized cases in the state of Rio de Janeiro in the same period (33.1%).13 Differences related to health facility profiles (hospital beds provided for more severe cases, reference ICU) and hospitalized cases (comorbidities, hospitalization when the disease was already at an advanced stage) need to be considered when making comparative analyses of lethality.
The majority of the studies we reviewed on suspected or confirmed hospitalized COVID-19 cases reported lethality rates of between 21 and 28.3%, whereby part of the cohorts monitored were still in hospital at the time the results were published, as also happened in our study.15 Higher lethality among cases admitted to ICUs and with invasive ventilatory support has also been described by other authors.17
In this study older age groups, presence of neoplasms and use of ventilator support stood out as having an independent effect associated with greater odds of death, both for all cases and for the confirmed case subgroup. The unfavorable prognosis found in association with older age groups has been described in China and also in countries on the European and American continents, including Brazil.13 Association between being of the male sex male and greater likelihood of death among hospitalized cases has also been reported.13
Poorer prognosis associated with neoplasms has also been found and described .14 A Chinese study reported that cases with some form of malignant disease were 3.5 times more likely to be hospitalized in ICUs, having to use invasive ventilation or dying.14
Other studies have found association between chronic obstructive pulmonary disease and greater risk of death from COVID-19.18 In our analysis, presence of chronic lung disease was associated with less likelihood of death. This is an unexpected finding, possibly related to the fact of the ‘chronic lung disease’ category including people with asthma, which has not been associated with unfavorable prognosis in COVID-19 cases.28 In this case, it is appropriate to note that long-term use of topical anti-inflammatory drugs by asthmatic patients could be a protective factor against the spread and replication of the virus. Another explication for a poorer prognosis associated with asthma not being found involves the reduction in SARS-CoV-2 virus receptor expression (referred to as ACE2) among asthmatic people, while expression of these receptors appears to be greater among people with diabetes mellitus and arterial hypertension, as well as among smokers.29
Other factors that have been described as being associated with unfavorable prognosis among hospitalized COVID-19 cases are chronic heart disease, chronic kidney disease, obesity, chronic neurological disease and chronic liver disease.18
With regard to imaging examinations, suggestive patterns can assist with case assessment, possible complications and reaching diagnosis. A Chinese study described ground glass opacity in 71% of cases, with greater frequency among those who died (81.0%) versus survivors (67%).15 At the HFSE, ground glass opacity was a frequent radiological finding in computerized tomography of the chest among confirmed cases; however, the ground glass pattern was also found in discarded cases. The high percentage of unperformed imaging examinations or examinations with no results informed limited this analysis.
The pandemic placed huge challenges on the hospital where this study was conducted, even though it was not a COVID-19 reference service in the state of Rio de Janeiro. For the researchers, these challenges included the impact of the increased number of cases, initial low availability of diagnostic tests, especially for staff with flu-like syndrome, and the need for continuous health team training, including with regard to rational use of personal protective equipment.
This study is the fruit of active hospital epidemiological surveillance which, besides contributing to timely notification and keeping up to date the information system which even during a pandemic was able to inform this study, was equally important for planning, advisory and evaluation activities for addressing COVID-19 at the HFSE. Its limitations mainly relate to the quality of information provided by epidemiological surveillance, especially in the context of an event of this magnitude. Other possible limitations include underreporting, data incompleteness and non-standardization of variables such as comorbidities and imaging examinations. Furthermore, the sample size and the study’s non-probabilistic design limit analysis of the impact of some of the comorbidities studied on death.
The possibility of underreporting was minimized by the good active searching coverage achieved by the HFSE Epidemiology Service, which was intensified in response to the disease.27 The percentage of unknown data was minimal for the majority of variables analyzed, representing a considerable joint effort in terms of epidemiological investigation of cases in this context; all the forms were reviewed by at least two of the team’s epidemiologists. Also worthy of note is the relevance of the multidisciplinary teams, as well as the importance of integrated health information systems.
This study has collaborated with knowledge of the profile of COVID-19 cases hospitalized at the Hospital Federal dos Servidores do Estado in Rio de Janeiro, with high prevalence of comorbidities. The main predictive factors of death from COVID-19 were being 50 years old or over, presence of neoplasms and patients using ventilatory support. The conclusion as to high lethality stresses the need for early diagnosis and treatment, as well as compliance with biosafety measures recommended for health services and their staff.
REFERENCES
1. Fauci AS, Lane HC, Redfield RR. Covid-19 – Navigating the uncharted. N Engl J Med [Internet]. 2020 Feb [cited 2020 Nov 3];382:1268-9. Available from: https://doi.org/10.1056/NEJMe2002387 [ Links ]
2. World Health Organization - WHO. Coronavirus disease 2019 (COVID-19) – WHO Coronavirus Disease (COVID-19) dashboard [Internet]. Geneve: WHO; 2020 [cited 2020 Sep 9]. Available from: https://covid19.who.int/ [ Links ]
3. Li R, Pei S, Chen B, Song Y, Zhang T, Yang W et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science [preprint]. 2020 [cited 2020 Nov 3]. Available from: https://doi.org/10.1126/science.abb3221 [ Links ]
4. Wu Ym Chen C, Chan Y. The outbreak of COVID-19: an overview. J Chinese Med Assoc [Internet]. 2020 [cited 2020 Nov 3];83(3):217-20. Available from: https://doi.org/10.1097/JCMA.0000000000000270 [ Links ]
5. Peeri NC, Shrestha N, Rahman S, Zaki R, Tan Z, Bibi S, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol [Internet]. 2020 Feb [cited 2020 Nov 3];49(3):717-26. Available from: https://doi.org/10.1093/ije/dyaa033 [ Links ]
6. Zhonghua L, Xing B, Zhi Z. Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. China CDC Wkly [Internet]. 2020 [cited 2020 Nov 3];41(2):145-51. Available from: https://doi.org/10.3760/cma.j.issn.0254-6450.2020.02.003 [ Links ]
7. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet [Internet]. 2020 Feb [cited 2020 Nov 3];395(10223):497-506. Available from: https://doi.org/10.1016/S0140-6736(20)30183-5 [ Links ]
8. Ministério da Saúde (BR). Secreataria de Vigilância em Saúde e Ambiente. Coronavírus COVID-19: diretrizes para diagnóstico e tratamento da COVID-19 [Internet]. Versão 4. Brasília: Ministério da Saúde; 2020 [citado 2020 nov 3]. Disponível em: https://portalarquivos.saude.gov.br/images/pdf/2020/May/08/Diretriz-Covid19-v4-07-05.20h05m.pdf [ Links ]
9. Croda J, Oliveira WK, Frutuoso RL, Mandetta LH, Baia-da-Silva DC, Brito-Sousa JD, et al. COVID-19 in Brazil: advantages of a socialized unified health system and preparation to contain cases. Rev Soc Bras Med Trop [Internet]. 2020 Apr [cited 2020 Nov 3];53:e20200167. Available from: http://dx.doi.org/10.1590/0037-8682-0167-2020 [ Links ]
10. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Painel coronavírus [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2020 jul 27]. Disponível em: https://covid.saude.gov.br/ [ Links ]
11. Secretaria Estadual de Saúde (RJ). Painel coronavírus COVID-19 [Internet]. Rio de Janeiro: Secretaria Estadual de Saúde; 2020 [citado 2020 set 20]. Disponível em: http://painel.saude.rj.gov.br/monitoramento/covid19.html [ Links ]
12. Barreto ML, Barros AJD, Carvalho MS, Codeço CT, Halla PRC, Medronho RA, et al. O que é urgente e necessário para subsidiar as políticas de enfrentamento da pandemia de COVID-19 no Brasil? Rev Bras Epidemiol [Internet]. 2020 abr [citado 2020 nov 3];23:E200032. Disponível em: https://doi.org/10.1590/1980-549720200032 [ Links ]
13. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Especial: doença pelo coronavírus 2019. Bol Epidemiol [Internet]. 2020 jul [citado 2020 jul 26];23(especial). Disponível em: https://saude.gov.br/images/pdf/2020/July/22/Boletim-epidemiologico-COVID-23-final.pdf [ Links ]
14. Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J [Internet]. 2020 May [cited 2020 Nov 3];55(5):2000547. Available from: https://doi.org/10.1183/13993003.00547-2020 [ Links ]
15. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet [Internet]. 2020 Mar [cited 2020 Nov 3];395(10229):1054-62. Available from: https://doi.org/10.1016/S0140-6736(20)30566-3 [ Links ]
16. Puerta-Alcalde P, García-Vidal C. El perfil del paciente COVID-19 atendido en los servicios de urgencias españoles durante la pandemia de 2020. Emergencias (Sant Vicenç dels Horts) [Internet]. 2020 ago [citado 2020 nov 3];32(4):225-6. Disponible en: http://emergencias.portalsemes.org/descargar/el-perfil-del-paciente-covid19-atendido-en-los-servicios-de-urgencias-espaoles-durante-la-pandemia-de-2020/ [ Links ]
17. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, Northwell COVID-19 Research Consortium. Presenting characteristics comorbidities and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA [Internet]. 2020 [cited 2020 Nov 3];323(20):2052. Available from: http://dx.doi.org/10.1001/jama.2020.6775 [ Links ]
18. Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 hospitalized UK patients with COVID-19 using the ISARIC WHO Clinical Characterization Protocol: prospective observational cohort study. BMJ [Internet]. 2020 [cited 2020 Nov 3];369:m1985. Available from: https://doi.org/10.1136/bmj.m1985 [ Links ]
19. Suleyman G, Fadel RA, Malette KM, Hamond C, Abdulla H, Entz A, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a Series of patients in metropolitan Detroit. JAMA Netw Open [Internet]. 2020 Jun [cited 2020 Nov 3];3(6):e2012270. Available from: https://doi.org/10.1001/jamanetworkopen.2020.12270 [ Links ]
20. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun [Internet]. 2020 May [cited 2020 Nov 3];109:102433. Available from: https://doi.org/10.1016/j.jaut.2020.102433 [ Links ]
21. Niquini RP, Lana RM, Pacheco AG, Cruz OG, Coelho FC, Carvalho LM, et al. SRAG por COVID-19 no Brasil: descrição e comparação de características demográficas e comorbidades com SRAG por influenza e com a população geral. Cad Saúde Pública [Internet]. 2020 [citado 2020 nov 3];36(7):e00149420. Disponível em: http://dx.doi.org/10.1590/0102-311X00149420 [ Links ]
22. Gil-Rodrigo A, Miró Ò, Piñera P, Jiménez S, Martín A, Martín-Sánchez FJ, et al. Analysis of clinical characteristics and outcomes in patients with COVID-19 based on a series of 1000 patients treated in Spanish emergency departments. Emergencias (Sant Vicenç dels Horts) [Internet]. 2020 Aug [cited 2020 Nov 3];32(4):233-41. Available from: http://emergencias.portalsemes.org/descargar/evaluacin-de-las-caractersticas-clnicas-y-evolucin-de-pacientes-con-covid19-a-partir-de-una-serie-de-1000-pacientes-atendidos-en-servicios-de-urgencias-espaoles/ [ Links ]
23. Gupta S, Hayek SS, Wang W, Chan L, Mathews KS, Melamed ML, et al. Factors associated with death in critically Ill patients with coronavirus disease 2019 in the US. JAMA Intern Med [Internet]. 2020 Jul [cited 2020 Nov 3];180(11):1436-46. https://doi.org/10.1001/jamainternmed.2020.3596 [ Links ]
24. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis [Internet]. 2020 May [cited 2020 Nov 3];94:91-5. Available from: https://doi.org/10.1016/j.ijid.2020.03.017 [ Links ]
25. Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care Units in Lombardy, Italy. JAMA Intern Med [Internet]. 2020 Jul [cited 2020 Nov 3];180(10):1345-55. Available from: https://doi.org/10.1001/jamainternmed.2020.3539 [ Links ]
26. Soares RCM, Mattos LR, Raposo LM. Risk factors for hospitalization and mortality due to COVID-19 in Espírito Santo State, Brazil. Am J Trop Med Hyg [Internet]. 2020 Sep [cited 2020 Nov 3];103(3):1184-90. Available from: https://doi.org/10.4269/ajtmh.20-0483 [ Links ]
27. Escosteguy CC, Pereira, AGL, Medronho RA. Três décadas de epidemiologia hospitalar e o desafio da integração da Vigilância em Saúde: reflexões a partir de um caso. Ciênc Saúde Coletiva [Internet]. 2017 [citado 2020 nov 3];22(10):3365-79. Disponível em: https://dx.doi.org/10.1590/1413-812320172210.17562017 [ Links ]
28. Jackson DJ, Busse WW, Bacharier LB, Togias A, Gern JE, Altman MC, et al. Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2. J Allergy Clin Immunol [Internet]. 2020 [cited 2020 Nov 3];146(1):203-6.e3. Available from: https://doi.org/10.1016/j.jaci.2020.04.009 [ Links ]
29. Tay MZ, Poh CM, Rénia L, ManAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol [Internet]. 2020 [cited 2020 Nov 3];20:363-74. Available from: https://doi.org/10.1038/s41577-020-0311-8 [ Links ]
30. Morais-Almeida M, Pité H, Aguiar R, Ansotegui I, Bousquet J. Asthma and the coronavirus disease 2019 pandemic: a literature review. Int Arch Allergy Immunol [Internet]. 2020 [cited 2020 Nov 3];181(9):680-8. Available from: https://doi.org/10.1159/000509057 [ Links ]
Received: September 05, 2020; Accepted: October 18, 2020










 texto en
texto en 
 Curriculum ScienTI
Curriculum ScienTI

