Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.1 Brasília 2021 Epub 31-Jan-2021
http://dx.doi.org/10.1590/s1679-49742021000100005
Original Article
Sources of access to medication and its use in the rural area of Pelotas, Rio Grande do Sul, Brazil, in 2016: a cross-sectional population-based study*
1Universidade Federal de Pelotas, Programa de Pós-Graduação em Epidemiologia, Pelotas, RS, Brazil
2Universidade Federal de Pelotas, Departamento de Fisiologia e Farmacologia, Pelotas, RS, Brazil
Objective
To analyze the prevalence of medication use, sources of access, and associated factors among rural residents in Pelotas, RS, Brazil.
Methods
This was a cross-sectional study conducted in 2016 with adults ≥18 years old. Participants reported on medication use and sources of access to medication in the month prior to the interview. Poisson regression was used.
Results
Among the 1,519 respondents, 54.7% (95%CI 48.7;60.5) used some form of medication and 3.3% (95%CI 2.4;4.5) stopped taking necessary medication. Higher prevalence of use occurred in: women (PR=1.23 - 95%CI 1.12;1.34), the elderly (PR=2.36 - 95%CI 2.05;2.73), people with poorer self-perceived health (PR=1.29 - 95%CI 1.14;1.46) and people with a higher number of diseases (PR=2.37 - 95%CI 2.03;2.77). A total of 14.0% (95%CI 11.2;17.4) obtained medication exclusively from the Brazilian National Health System, prevalence of which was higher among those who self-reported themselves to be non-white and from lower economic classification.
Conclusion
A low number stopped taking medication they needed to take. Use of free-of-charge medication was greater in groups with lower income.
Keywords: Health Surveys; Rural Areas; Rural Health; Pharmacoepidemiology; Pharmaceutical Services; Drug Utilization
Introduction
There are determinants of access to medication and its use, including health services, geographical access to these places and pharmacy service acceptability in the opinion of those who use them (service user expectations and characteristics of the products and the service).1 2 The pattern of medication use also differs according to people’s sociodemographic, cultural, behavioral and health characteristics.3 4
Studies based on data from countries with contrasting socioeconomic situations have found lower prevalence of medication use in rural areas in comparison to urban areas.5 6 Moreover, there is a connection between availability, accessibility, medication use and health results which, especially in low- and middle-income countries, still poses an important challenge for public health.1 7
Brazil has a pharmaceutical system intended to ensure that its population has universal and free-of-charge access to medication considered to be essential.4 8 However, in many situations health service users need medications that are not available free of charge via the public health system, so that they have to pay for it, which may seriously compromise their income or interfere the continuity of the drug treatment.9
We found few studies that assessed medication use in rural areas of Brazil.10 11 Limitations of a logistical and financial nature hinder studies being conducted in rural areas,12 where there is also less availability of health services and pharmacies close to people’s homes.13 These factors can interfere in the pattern of medication use.
Apart from the scarcity of studies on this theme in rural areas, it is fundamental to gain knowledge of possible factors associated with medication use and sources from where medication is obtained. This knowledge can contribute to the establishment of priorities and planning and public policies planning, targeting the rural population.
The objective of this study was to analyze the prevalence of medication use, sources of access and associated factors among people living in the rural area of Pelotas, located in the state of Rio Grande do Sul, in Southern Brazil.
Methods
A cross-sectional population-based study was conducted in the rural area of Pelotas, RS, Brazil. The study is part of a broader research project on the health of the rural population.12 The municipality of Pelotas has a population of around 340,000 inhabitants. Approximately 7% of those individuals live in the rural area of the municipality.14 The rural area is comprised of eight districts, divided into 50 census tracts and has 14 primary healthcare centers.
To be eligible in this study, participants had to be 18 years old or over, routinely living in the rural area of Pelotas - i.e. living in a household which was their usual residence on the date of the interview; or temporarily absent for a period not greater than 12 months from that date. Individuals were excluded from the study if they had any cognitive/mental disabilities, unaided by helpers or family members, those hospitalized or institutionalized during the data collection process, as well as those who did not speak/understand Portuguese (part of the population has Pomeranian origin.).
The sample size was calculated aiming to meet the objectives of all research projects, whereby the largest size needed was 1,458 individuals for the ‘tobacco use’ outcome. The sample size was estimated using the OpenEpi statistical analysis program. The parameters used were 20% prevalence,15) 95% confidence level, a 3 percentage point margin of error and a 2.0 design effect. A further 10% was added for possible losses/refusals and 15% to adjust for possible confounding factors.
The sampling process took place in two stages. Firstly, 24 census tracts were selected randomly in a number proportional to the number of households in each district. Thirty households were then selected in each census tract, all of which were identified in community groups (largest number of households close together) in each tract, summing up 720 households. Further details on the methodology can be found in a previous publication.12
Data collection took place by means of face-to-face interviews in each participant’s household between January and June 2016. The questionnaire comprised sociodemographic and behavioral questions and questions on health. It was administered via the REDCap platform,16 using Samsung Galaxy Tab E tablets.
The interviewers received training on administering the questionnaires which had been tested beforehand in a pilot study with 19 participants (not included in the sample) conducted in Arroio do Padre, formerly an area of Pelotas and transformed into a separate municipality in 1996, which also has rural characteristics.
Losses to the study were defined as residents not found after at least three attempts to make contact on different days and at different times. The field work was supervised by the researchers. Quality control was carried out with 10% of randomly selected respondents by telephone, by readministering a shorter version of the questionnaire (ten questions from the original questionnaire), with the aim of checking repeatability and data quality.
The dependent variables analyzed were ‘use of medication’, ‘source of access to medication used’ and ‘non-use of necessary medication’, all within the 30 days prior to the interview. First of all respondents were asked whether during the last month they had stopped taking medication they needed to take. The answer options to this question, which was read to the participants, were: yes; no; did not need to take medication in the last month. If the answer was ‘did not need to take medication in the last month’, the remaining questions about medication were not asked.
With regard to the ‘source of access to medication used’ outcome, the following question was asked:
“In the last month, where did you get the medication you took?”
The sources of access to medication were categorized into: (i) Brazilian National Health system (SUS), totally free of charge; (ii) private establishment, such as private sector pharmacies, upon payment; or (iii) mixed, i.e. both from the SUS and from private establishments or the Farmácia Popular. Analysis of association was based on dichotomization of this information, between ‘SUS’ (free-of-charge source) and ‘private/mixed establishment’, in order to be able to assess whether medication had been obtained totally free of charge or not.
The outcome variable ‘use of medication in the last 30 days’ was built based on the answers to the two preceding questions, about having stopped taking medication and sources of access to medication. Those who reported not needing to take medication in the last 30 days were considered not to be medication users, while those who indicated a source where they had got medication in the last 30 days were considered to be medication users.
The ‘non-use of necessary medication’ outcome was built based on a positive answer to the initial question, i.e. ‘Yes, stopped taking medication that needed to take’. These respondents were asked why they did not take their medication and the name(s) of the medication not taken, later classified according to the World Health Organization (WHO) Anatomical Therapeutical Chemical classification system - ATC Level 1.17 When respondents could not remember the name of the medication, they were asked to show the medication package or prescription to the interviewer.
The independent variables encompassed sociodemographic factors related to health and health services:
-
Sociodemographic factors
- Sex (male; female);
- Age (completed years: 18-39; 40-59; 60 or over);
- Self-reported skin color (White; non-white);
- Marital status (no partner; had a partner);
- Schooling (completed years of study: no schooling/incomplete elementary education; complete elementary education/incomplete high school education; complete high school education/ incomplete higher education; complete higher education or above);
- Economic classification (A/B [wealthier]; C; D/E [poorer]), according to the Associação Brasileira de Empresas de Pesquisa;18
- Current work situation (not working; working).
-
Health-related factors
- Self-perceived health (very good/good; regular; poor/very poor);
- Number of chronic diseases present (none; one or two; three or more), obtained by asking the following question, “Has a doctor or a health professional ever told you that you have...?” including cardiocirculatory system diseases, diabetes mellitus, cancer, among others.
-
Health service-related factors
- Registered with the Family Health Strategy (FHS), created by the Ministry of Health as a strategy to support Primary Health Care (yes; no);
- Perception of distance between household and nearest pharmacy (Far, but easy to access; far and hard to access; close and easy to access; close, but hard to access). As the proportion of individuals who considered that this distance was ‘close, but hard to access’ was very low (n=22; 1.5%), for the purposes of analysis, this variable was dichotomized into easy to access or hard to access, regardless of distance;
- Perception of distance between household and nearest Primary Healthcare Center (PHC) (Far, but easy to access; far and hard to access; close and easy to access; close, but hard to access).
The sample was described and the proportions and respective 95% confidence intervals (95%CI) of medication use and sources of access were presented according to independent variables. Poisson regression was used to obtain crude and adjusted prevalence ratios (PR) for these two outcomes. The adjusted analysis followed the three-layer hierarchical model built based on the literature.2 4 10 11 19 20 The first level included sociodemographic variables; the second level contained the ‘self-perceived health’ and ‘number of chronic diseases’ variables; while the third and final level contained the variables related to health services, ‘registered with the FHS’, ‘distance from home to pharmacy’ and ‘distance from home to the nearest PHC’. The variables were adjusted to those on the same level and those on the next level up; backward selection was used, whereby only those with a p-value <0.20 were kept in the model. The data were weighted according to the number of households sampled, in relation to the total number of permanent households in each district (svy command). A 5% significance level was used. The data were analyzed using the Stata 14.0 statistical package (Stata Corporation, College Station, USA).
The study was approved by the Federal University of Pelotas Faculty of Medicine Research Ethics Committee on December 11th 2015, number 1.363.979.Participants signed a Free and Informed Consent form before starting the interview.
Results
A total of 1,697 individuals were considered eligible for this research. After losses and refusals (n=178), the final sample resulted in 1,519 (89.5%) individuals to be interviewed (Figure 1). The majority of losses and refusals were males and in the 18-24 age group (p<0.05).
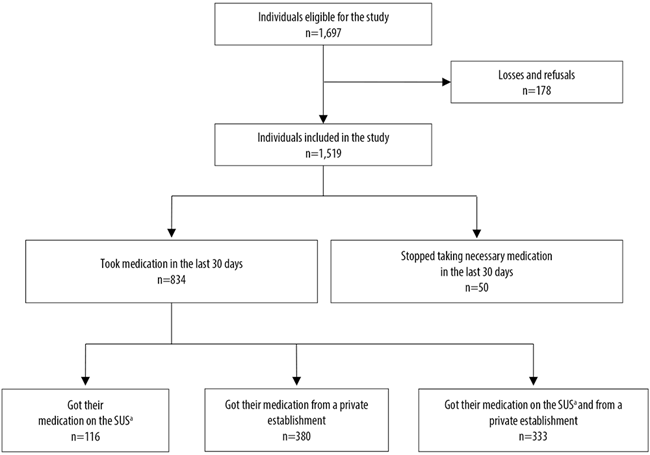
a) SUS: Brazilian National Health System.
Figure 1 Selection process of interviewed individuals, rural area of Pelotas, Rio Grande do Sul, 2016
Among the participants, 51.7% were females individuals aged 40-59 years old (39.2%), those self-reporting white skin color (85.1%), those who lived with a partner (70.8%), those who had no schooling/incomplete elementary education (66.1%), those belonging to economic classification C (53.7%) and those who had a job (59.5%). A total of 64.1% of respondents had very good/good self-perception of their health, 41.8% had no chronic diseases, 71.4% were registered with the FHS, 62.8% considered the distance between their home and the closest pharmacy to be easy to access and 74.3% considered the distance between their home and the closest PHC to be easy to access (Table 1).
Over half the participants (54.7% - 95%CI 48.7;60.5) had taken medication in the month prior to the interview. Prevalence of medication use was higher among women, individuals aged 60 or over, those with less schooling, those who did not work, those who had poor/very poor self-perceived health and those who had more chronic diseases (Table 1).
Table 1 Description of the sample (n=1,519) and frequency of medication use (n=834) among people living in the rural area of Pelotas, Rio Grande do Sul, 2016
| Variables | Total | Medication use | ||
|---|---|---|---|---|
| n | % | n | % (95%CIa) | |
| Sex | ||||
| Male | 734 | 48.3 | 349 | 47.2 (40.8;53.7) |
| Female | 785 | 51.7 | 485 | 61.6 (54.9;67.8) |
| Age (years) | ||||
| 18-39 | 515 | 34.0 | 166 | 32.0 (27.1;37.3) |
| 40-59 | 593 | 39.2 | 332 | 55.7 (50.9;60.4) |
| ≥60 | 411 | 26.8 | 336 | 81.9 (71.1;89.2) |
| Self-reported skin color | ||||
| White | 1.296 | 85.1 | 714 | 54.9 (48.9;60.7) |
| Non-white | 223 | 14.9 | 120 | 53.4 (41.4;65.0) |
| Lives with partner | ||||
| No | 443 | 29.2 | 228 | 51.0 (44.6;57.3) |
| Yes | 1.076 | 70.8 | 606 | 56.2 (49.4;62.7) |
| Schooling | ||||
| No schooling/incomplete elementary education | 996 | 66.1 | 609 | 60.7 (52.2;68.7) |
| Complete elementary education/incomplete high school education | 233 | 15.4 | 92 | 39.2 (31.0;48.1) |
| Complete high school education/incomplete higher education | 213 | 14.0 | 89 | 41.9 (36.0;48.1) |
| Complete higher education or above | 67 | 4.5 | 36 | 53.4 (42.4;64.0) |
| Economic classification | ||||
| A/B | 301 | 20.0 | 170 | 56.5 (49.9;62.9) |
| C | 814 | 53.7 | 436 | 53.4 (46.2;60.4) |
| D/E | 388 | 26.3 | 221 | 56.3 (47.5;64.8) |
| Current work situation | ||||
| Not working | 613 | 40.5 | 420 | 68.3 (62.0;74.0) |
| Working | 906 | 59.5 | 414 | 45.3 (39.3;51.6) |
| Self-perceived health | ||||
| Very good/good | 964 | 64.1 | 404 | 41.6 (36.0;47.5) |
| Regular | 461 | 30.4 | 349 | 75.6 (64.2;84.3) |
| Poor/very poor | 82 | 5.5 | 72 | 87.7 (78.7;93.2) |
| Number of chronic diseases | ||||
| None | 631 | 41.8 | 162 | 25.6 (21.0;30.8) |
| 1 - 2 | 614 | 40.2 | 426 | 69.2 (63.0;74.7) |
| 3 or more | 274 | 18.0 | 246 | 89.6 (72.5;96.6) |
| Registered with Family Health Strategy | ||||
| No | 423 | 28.6 | 212 | 49.9 (37.5;62.3) |
| Yes | 1.070 | 71.4 | 608 | 56.6 (52.2;60.9) |
| Distance from home to pharmacy | ||||
| Easy to access | 941 | 62.8 | 497 | 52.4 (46.2;58.6) |
| Hard to access | 563 | 37.2 | 325 | 57.8 (50.0;65.1) |
| Distance from home to nearest primary healthcare center | ||||
| Far, but easy to access | 179 | 11.7 | 94 | 51.8 (42.7;60.8) |
| Far and hard to access | 121 | 7.9 | 66 | 54.8 (45.4;63.8) |
| Close and easy to access | 1.107 | 74.3 | 606 | 54.5 (48.3;60.5) |
| Close, but hard to access | 92 | 6.1 | 56 | 61.0 (47.4;73.2) |
| Total | 1,519 | 100.0 | 834 | 54.7 (48.7;60.5) |
a) 95%CI: 95% confidence interval.
In the adjusted analysis, medication use was higher among women (PR: 1.23 - 95%CI 1.12;1.34), in older respondents (≥60 years old: PR=2.36 - 95%CI 2.05;2.73), in those with more chronic diseases (3 or more: PR=2.37 - 95%CI 2.03;2.77) and with regular and poor/very poor self-perceived health (PR= 1.29 - 95%CI: 1.14;1.46). The prevalence of medication use was lower among individuals who did not live with a partner (PR= 0.88 - 95%CI 0.80;0.98) and those who had a job (PR= 0.82 - 95%CI 0.71;0.94) (Table 2).
Table 2 Crude and adjusted analysis of prevalence of medication use in relation to the independent variables, among a sample of adults (n=834) living in the rural area of Pelotas, Rio Grande do Sul, 2016
| Variables | Medication use | |||
|---|---|---|---|---|
| Crude analysis | Adjusted analysis | |||
| PRa (95%CIb) | p-valuec | PRa (95%CIb) | p-valuec | |
| Sex | <0.001 | <0.001 | ||
| Male | 1.00 | 1.00 | ||
| Female | 1.30 (1.18;1.45) | 1.23 (1.12;1.34) | ||
| Age (years) | <0.001d | <0.001d | ||
| 18-39 | 1.00 | 1.00 | ||
| 40-59 | 1.74 (1.54;1.97) | 1.74 (1.54;1.97) | ||
| ≥60 | 2.56 (2.23;2.84) | 2.36 (2.05;2.73) | ||
| Self-reported skin color | 0.800 | 0.483 | ||
| White | 1.00 | 1.00 | ||
| Non-white | 0.97 (0.79;1.20) | 1.07 (0.89;1.28) | ||
| Schooling | <0.001d | 0.623 | ||
| No schooling/incomplete elementary | 1.00 | 1.00 | ||
| Complete elementary/incomplete high school | 0.65 (0.51;0.82) | 0.92 (0.73;1.17) | ||
| Complete high school/incomplete higher education | 0.69 (0.60;0.80) | 0.92 (0.80;1.07) | ||
| Complete higher education or above | 0.88 (0.70;1.11) | 0.98 (0.75;1.27) | ||
| Lives with partner | 0.079 | 0.016 | ||
| No | 0.91 (0.81;1.01) | 0.88 (0.80;0.98) | ||
| Yes | 1.00 | 1.00 | ||
| Economic classification | 0.586 | 0.667 | ||
| A/B | 1.00 | 1.00 | ||
| C | 0.94 (0.80;1.12) | 0.94 (0.80;1.11) | ||
| D/E | 1.00 (0.83;1.20) | 0.93 (0.80;1.09) | ||
| Current work situation | <0.001 | 0.005 | ||
| Not working | 1.00 | 1.00 | ||
| Working | 0.66 (0.59;0.75) | 0.82 (0.71;0.94) | ||
| Self-perceived health | <0.001d | <0.001 | ||
| Very good/good | 1.00 | 1.00 | ||
| Regular | 1.82 (1.62;2.04) | 1.29 (1.17;1.42) | ||
| Poor/very poor | 2.11 (1.85;2.39) | 1.29 (1.14;1.46) | ||
| Number of chronic diseases | <0.001d | <0.001d | ||
| None | 1.00 | 1.00 | ||
| 1 - 2 | 2.71 (2.31;3.16) | 2.23 (1.92;2.58) | ||
| 3 or more | 3.50 (2.98;4.12) | 2.37 (2.03;2.77) | ||
| Registered with Family Health Strategy | 0.292 | 0.270 | ||
| No | 1.00 | 1.00 | ||
| Yes | 1.13 (0.89;1.44) | 1.15 (0.89;1.47) | ||
| Distance from home to pharmacy | 0.120 | 0.222 | ||
| Easy to access | 1.00 | 1.00 | ||
| Hard to access | 1.10 (0.97;1.25) | 1.06 (0.96;1.17) | ||
| Distance from home to nearest primary healthcare center | 0.384 | 0.459 | 0,459 | |
| Far, but easy to access | 1.00 | 1.00 | ||
| Far and hard to access | 1.06 (0.86;1.30) | 0.98 (0.83;1.15) | ||
| Close and easy to access | 1.05 (0.90;1.22) | 1.08 (0.95;1.23) | ||
| Close, but hard to access | 1.18 (0.98;1.42) | 1.02 (0.86;1.21) | ||
a) PR: prevalence ratio.
b) 95%CI: 95% confidence interval.
c) Wald test for heterogeneity.
d) Wald linear trend test.
Among individuals who took medication, 14.0% (95%CI 11.2;17.4) reported that they were able to get their medication on the SUS, 45.8% (95%CI 40.3;51.4) from private establishments and 40.2% (95%CI 35.5;45.0) from mixed sources (SUS plus private establishment). The highest percentage of medication provided by the SUS was found among individuals of non-white skin color (22.9%) and those belonging to economic classification D/E (20.8%) (Table 3).
Table 3 Description of sources of access to medication taken in the last month among adults (n=829a) living in the rural area of Pelotas, Rio Grande do Sul, 2016
| Variables | Sources of access to medication | ||
|---|---|---|---|
| SUSb | Private establishment | Mixed (SUS and private establishment) | |
| (n=116) | (n=380) | (n=333) | |
| %(IC95%c) | %(IC95%c) | %(IC95%c) | |
| Sex | |||
| Male | 17.3 (13.1;22.5) | 49.3 (43.0;55.7) | 33.3 (27.4;39.9) |
| Female | 11.6 (8.5; 15.8) | 43.3 (36.7; 50.2) | 45.0 (40.0; 50.2) |
| Age (years) | |||
| 18-39 | 17.4 (12.0;24.6) | 57.9 (48.0;67.2) | 24.7 (18.3;32.4) |
| 40-59 | 14.5 (11.4;18.2) | 43.7 (38.0;49.6) | 41.8 (36.1;47.8) |
| ≥60 | 11.9 (8.4;16.5) | 41.9 (34.4;49.9) | 46.2 (38.5;54.1) |
| Self-reported skin color | |||
| White | 12.5 (9.8;15.8) | 47.8 (42.2;53.5) | 39.7 (34.5;45.0) |
| Non-white | 22.9 (16.4;31.1) | 33.9 (24.5;44.9) | 43.2 (35.4;51.3) |
| Lives with partner | |||
| No | 15.5 (10.9;21.7) | 40.3 (35.1;45.8) | 44.1 (39.3;49.1) |
| Yes | 13.4 (10.6;16.9) | 47.9 (41.6;54.2) | 38.7 (33.2;44.4) |
| Schooling | |||
| No schooling/incomplete elementary | 14.0 (10.9;17.9) | 41.3 (35.1;47.7) | 44.8 (38.8;50.9) |
| Complete elementary/incomplete high school | 12.1 (5.8;23.3) | 54.8 (40.5;68.4) | 33.1 (21.8;46.8) |
| Complete high school /incomplete higher education | 18.0 (10.2;29.9) | 53.3 (42.4;64.0) | 28.6 (18.6;41.4) |
| Complete higher education or above | 9.2 (3.0;24.9) | 79.1 (64.2;88.8) | 11.7 (5.4;23.5) |
| Economic classification | |||
| A/B | 9.9 (6.0;15.9) | 60.3 (53.3;67.0) | 29.8 (22.3;38.7) |
| C | 12.3 (9.1;16.5) | 43.3 (36.0;50.9) | 44.3 (37.6;51.3) |
| D/E | 20.8 (15.3;27.7) | 37.9 (30.8;45.7) | 41.3 (35.6;47.1) |
| Current work situation | |||
| Not working | 12.4 (8.9;17.1) | 36.5 (30.9;42.5) | 51.1 (45.4;56.9) |
| Working | 15.7 (12.3;19.7) | 55.5 (49.5;61.3) | 28.9 (23.4;35.1) |
| Self-perceived health | |||
| Very good/good | 17.2 (14.1;20.9) | 50.3 (44.4;56.2) | 32.5 (27.2;38.3) |
| Regular | 10.1 (6.7;14.9) | 42.9 (36.1;50.0) | 47.0 (39.9;54.1) |
| Poor/very poor | 13.2 (5.7;27.8) | 35.0 (21.0;52.3) | 51.8 (39.2;64.1) |
| Number of chronic diseases | |||
| None | 16.2 (10.6;24.1) | 69.6 (59.0;78.5) | 14.2 (8.3;23.1) |
| 1 - 2 | 15.3 (12.0;19.2) | 45.2 (39.2;51.4) | 39.5 (33.7;45.7) |
| 3 or more | 10.3 (6.5;16.0) | 31.1 (23.7;39.6) | 58.6 (50.7;66.2) |
| Registered with Family Health Strategy | |||
| No | 12.1 (7.8;18.3) | 54.0 (46.5;61.4) | 33.9 (30.1;37.9) |
| Yes | 14.7 (11.6;18.4) | 42.6 (36.6;48.9) | 42.7 (36.6;49.0) |
| Distance from home to pharmacy | |||
| Easy to access | 15.0 (11.5;19.4) | 45.4 (38.8;52.0) | 39.6 (33.6;46.0) |
| Hard to access | 12.7 (9.4;16.9) | 46.4 (40.6;52.3) | 40.9 (35.7;46.4) |
| Distance from home to nearest Primary Healthcare Center | |||
| Far, but easy to access | 10.7 (5.5;19.7) | 49.7 (37.5;61.9) | 39.6 (29.2;51.1) |
| Far and hard to access | 12.4 (6.5;22.6) | 52.7 (39.8;65.3) | 34.9 (25.1;46.1) |
| Close and easy to access | 15.0 (11.9;18.8) | 43.7 (38.6;49.0) | 41.2 (35.8;46.9) |
| Close, but hard to access | 13.1 (7.3;22.3) | 49.9 (32.2;67.7) | 37.0 (23.4;53.1) |
| Total | 14.0 (11.2;17.4) | 45.8 (40.3;51.4) | 40.2 (35.5;45.0) |
a) The variable has 5 missing items.
b) SUS: Brazilian National Health System.
c) 95%CI: 95% confidence interval.
Following adjustment, the prevalence of obtaining medication totally free of charge was higher among those of non-white skin color (PR= 1.82 - 95%CI 1.24;2.66) and was lower among those with regular self-perceived health (PR= 0.53 - 95%CI 0.35;0.80). The lower the economic classification, the greater the probability of getting medication free of charge (Table 4).
Table 4 Crude and adjusted analysis of prevalence of obtaining only free of charge medication in relation to the independent variables among adults (n=829a) living in the rural area of Pelotas, Rio Grande do Sul, 2016
| Variables | Adjusted analysis | |||
|---|---|---|---|---|
| PRa (IC95%b) | p-valuec | PRa (IC95%b) | p-valuec | |
| Sex | 0.040 | 0.055 | ||
| Male | 1.00 | 1.00 | ||
| Female | 0.67 (0.46;0.98) | 0.68 (0.46;1.01) | ||
| Age (years) | 0.178 | 0.441 | ||
| 18-39 | 1.00 | 1.00 | ||
| 40-59 | 0.83 (0.54;1.28) | 0.84 (0.54;1.30) | ||
| ≥60 | 0.68 (0.45;1.05) | 0.72 (0.43;1.20) | ||
| Self-reported skin color | 0.004 | 0.004 | ||
| White | 1.00 | 1.00 | ||
| Non-white | 1.83 (1.24;2.71) | 1.82 (1.24;2.66) | ||
| Schooling | 0.612 | 0.197 | ||
| No schooling/incomplete elementary | 1.00 | 1.00 | ||
| Complete elementary/incomplete high school | 0.86 (0.41;1.81) | 0.82 (0.39;1.74) | ||
| Complete high school /incomplete higher education | 1.29 (0.70;2.39) | 1.65 (0.91;2.97) | ||
| Complete higher education or above | 0.66 (0.23;1.88) | 1.09 (0.33;3.64) | ||
| Lives with partner | 0.405 | 0.777 | ||
| No | 1.15 (0.81;1.64) | 1.05 (0.73;1.52) | ||
| Yes | 1.00 | 1.00 | ||
| Economic classification | 0.010e | 0.004e | ||
| A/B | 1.00 | 1.00 | ||
| C | 1.25 (0.71;2.19) | 1.34 (0.76;2.37) | ||
| D/E | 2.11 (1.21;3.70) | 2.48 (1.30;4.76) | ||
| Current work situation | 0.176 | 0.192 | ||
| Not working | 1.00 | 1.00 | ||
| Working | 1.26 (0.89;1.78) | 1.30 (0.87;1.94) | ||
| Self-perceived health | 0.053 | 0.013 | ||
| Very good/good | 1.00 | 1.00 | ||
| Regular | 0.59 (0.38;0.91) | 0.53 (0.35;0.80) | ||
| Poor/very poor | 0.77 (0.38;1.56) | 0.69 (0.33;1.44) | ||
| Number of chronic diseases | 0.153 | 0.254 | ||
| None | 1.00 | 1.00 | ||
| 1 - 2 | 0.94 (0.58;1.53) | 0.99 (0.67;1.47) | ||
| 3 or more | 0.63 (0.37;1.10) | 0.68 (0.39;1.20) | ||
| Registered with Family Health Strategy | 0.391 | 0.368 | ||
| No | 1.00 | 1.00 | ||
| Yes | 1.21 (0.77;1.92) | 1.21 (0.79;1.84) | ||
| Distance from home to pharmacy | 0.318 | 0.312 | ||
| Easy to access | 1.00 | 1.00 | ||
| Hard to access | 0.84 (0.60;1.19) | 0.83 (0.57;1.20) | ||
| Distance from home to nearest primary healthcare center | 0.777 | 0.952 | 0,952 | |
| Far, but easy to access | 1.00 | 1.00 | ||
| Far and hard to access | 1.16 (0.54;2.50) | 1.08 (0.53;2.20) | ||
| Close and easy to access | 1.41 (0.70;2.84) | 1.14 (0.61;2.13) | ||
| Close, but hard to access | 1.22 (0.55;2.72) | 0.96 (0.46;1.99) | ||
a) The variable has 5 missing items.
b) PR: prevalence ratio.
c) 95%CI: 95% confidence interval.
d) Wald test for heterogeneity.
e) Wald linear trend test.
A total of 3.3% (95%CI 2.4;4.5) of the individuals in the sample (n=50) reported having stopped taking at least one type of medication in the last 30 days, and the main reasons reported for this were: unable to get it on the SUS or from the Farmácia Popular (n=26; 52.0%); own free will (n=15; 30.0%); prescription out of date (n=4; 8.0%); upon medical recommendation (n=5; 10%) (data not shown in tables).
Types of medication for the nervous system were those most frequently not taken (n=16) among necessary medicine, followed by types of medication for the cardiovascular system (n=10), those for the alimentary tract and the metabolism (n=7) and those for the musculoskeletal system (n=6). Although with less frequency, respondents also stopped taking medication for the blood and hematopoietic organs (n=3); for the genitourinary system and sex hormones (n=3); anti-infectives (n=2); antiparasitics, insecticides and repellents (n=1); and dermatological medication (n=2) (data not shown in tables). Some participants stopped taking a further two kinds of medication, which were unable to be classified as they were not found in the WHO/ATC.
Discussion
Over half the respondents had taken some kind of medication in the month prior to the interview. Use of medication was greater among women, older individuals, those with more chronic diseases and poorer self-perceived health; whilst it was less frequent among those who did not have a partner and those who were working. Approximately one in seven got their medication totally free of charge, prevalence of which was greater among males, those who self-reported non-white skin color, those belonging to lower economic classifications and those with good/very good self-perceived health. Few interviewees reported not having taken medication considered to be necessary in the 30 days prior to the interview and only half of these reported not taking medication because of difficulty in getting it on the SUS or via the Farmácia Popular.
This study had limitations. The questionnaire used was not validated and, specifically, the indirect way in which the information on use of medication was collected, based on questions about not taking medication and sources for getting medication, may have led to underestimated prevalence of medication use, thus making comparisons difficult.
Another limitation lies on the possibility of a selection bias that occurs when residences that are easier to access are chosen. In these cases, prevalence of medication use could be overestimated, while failure to use necessary medication could be underestimated. Moreover, losses and refusals were higher among younger people and males, while the literature indicates that women and older individuals are those who most take medication.9 Another possible limitation of this study is memory bias: the recall period for the questions was the last 30 days before the interview, and participants may have forgotten whether they took the medication or not. Finally, the cross-sectional nature of the study does not allow temporality of events to be analyzed, making them susceptible to reverse causality bias in some associations (e.g.: use of medication and self-perceived health).
Estimated prevalence of medication use in this study (54.7%) was lower when compared to that found by another study also conducted in Pelotas, around ten years earlier (2002), although that study was conducted in the urban area of Pelotas and had a 15-day recall period: 65.9%.19 Research conducted with individuals aged 35-70 years old, between 2003 and 2009, analyzed use of medication to prevent cardiovascular diseases in urban and rural areas of four Latin American countries - Argentina, Brazil, Chile and Colombia -, where in general lower prevalence of medication use was found in rural areas in comparison with urban areas.5
According to a literature review conducted by Gomes et al.,20 only one of the 14 studies included assessed use of medication by adults living in an urban area in the last 30 days and they found a prevalence of 70%. Data from a study of the 2015 National Survey on Access, Use and Rational Medication Use Promotion (urban area) found 76.2% prevalence of medication use in the 30 days prior to the survey.4
There are some hypotheses for the disagreement between these studies’ prevalence. Prevalence of medication use in the urban area of Pelotas was higher because it relates to a period around a decade earlier than the study in the rural area;19 furthermore, the awarness regarding rational use of medication has increased in recent years, and the use of antimicrobial products has also decreased due to greater health control.21 Another hypothesis to be considered is that possible reduced access to health services in rural areas would mean less diagnosis and fewer medication prescriptions;22 less access to medication could be explained by the few pharmacies located in rural area, compared to urban ones as well as the need to travel further to get medication. Finally, there is yet another hypothesis, namely that of prevalence of medication use in rural areas being lower in rural areas compared to urban areas as a natural result of healthier lifestyles in the countryside in relation to lifestyles in cities.23 24
Higher prevalence of medication use by women, older people, those with poorer self-perceived health and those with a greater number of chronic diseases corroborates the literature.2-4 Having found lower prevalence of medication use among those who did not have a partner raises the hypothesis of partners providing more attention and care, thus leading to someone with a partner using health services more and thus increasing the chances of diagnosis of health problems requiring medication. However, other studies did not find these differences related to marital status.19 25 Lower prevalence found among those who worked may be associated with the fact that in order to be working they would tend to be in better health (“the healthy worker effect”),26 whereas the fact of not working, associated with illness or a health condition, would lead to greater need to take medication.
Prevalence of medication use was higher among women. It has already been documented in the literature that women are more concerned about their health, have greater perception of signs and symptoms of diseases and, consequently, attend health services more frequently,27 28 which may explain their greater use of medication as a result of greater probability of disease diagnosis.
Regarding the sources of access to medication, the results found are in consonant with the findings of the 2008 National Household Sample Survey (PNAD), conducted with individuals who had medication prescribed via the public health system. A study that analyzed the PNAD 2008 data found that less than half the sample got their medication free of charge (via the public system), and that this number was higher among those with lower schooling and income, of black skin color and living in households registered with the FHS;11 whereas greater access to medication purchased in the private sector was found among the wealthier, those with more schooling and of white skin color. It is important to note that in the case of that study, there were no differences in prevalence of access to medication, regardless of living in urban or rural areas.11
Use and sources of medication in Campinas, SP, were investigated according to sociodemographic variables. That population-based study was conducted in 2008 and included people who lived in the urban area aged 20 years old or more. Prevalence of medication use during the three days before the survey was 57.2%, which was close to the rate found by our study, although its recall period was shorter. In Campinas, prevalence of getting medication on SUS was 30%, almost double of what was found in other studies in Pelotas,29 which also found higher prevalence of medication obtained via SUS among individuals with lower income. These results reflect the importance of health service coverage to meet the needs of more vulnerable populations.
The present study did not find association between (i) use of medication or getting medication free of charge and (ii) the variables related to health services, such as being registered with the FHS and the distance between home and the nearest pharmacy or PHC. An investigation with national representativeness, although conducted exclusively in urban areas, did not find important differences regarding geographical accessibility of medication provided by the SUS, private pharmacies or the Farmácia Popular.2 A reasonable explanation for that finding is that around two thirds of the sample of the present study was registered with the FHS and few participants rated the distance between their homes and services as being ‘hard to access’. However, it is appropriate to highlight the results of other studies, in which over 60% of those interviewed were registered with the FHS and were found to have greater access to medication.11 30
The frequency of individuals who stopped taking necessary medication was low. As they were from a rural area, greater prevalence was to be expected, considered the inequities found in access to health services.9 This finding may reflect the low percentage of individuals without access to medication, especially when the reason for not taking it was not having been able to get it on the SUS. Corroborating this finding, the National Survey on Access, Use and Promotion of Rational Use of Medicines revealed that 94.3% of participants had total access to medications.2 It is likely that facilitated access to medication is related to increased primary healthcare center coverage, along with the existence of government programs intended to provide universal and free-of-charge access.
Use of medication in rural areas in Brazil is still little explored, hence why we recommend future studies on this theme, in order to better understand the regional health characteristics. The findings of this study are particularly important for the design of specific public policies and strategies targeting the rural population. We highlight the importance of equity in healthcare for more vulnerable subgroups. Even though this study demonstrated that individuals belonging to lower economic classifications got their medication free of charge, nevertheless prevalence was low.
REFERENCES
1. Bigdeli M, Jacobs B, Tomson G, Laing R, Ghaffar A, Dujardin B, et al. Access to medicines from a health system perspective. Health Policy Plan [Internet]. 2013 Oct [cited 2020 Sep 3];28(7):692-704. Available from: https://doi.org/10.1093/heapol/czs108 [ Links ]
2. Oliveira MA, Luiza VL, Tavares NUL, Mengue SS, Arrais PSD, Farias MR, et al. Access to medicines for chronic diseases in Brazil: a multidimensional approach. Rev Saúde Pública [Internet]. 2016 [cited 2020 Sep 3];50(suppl 2):6s. Available from: https://doi.org/10.1590/s1518-8787.2016050006161 [ Links ]
3. Bertoldi AD, Arrais PSD, Tavares NUL, Ramos LR, Luiza VL, Mengue SS, et al. Use of generic medicines by the Brazilian population: an evaluation of PNAUM 2014. Rev Saúde Pública [Internet]. 2016 [cited 2020 Sep 3];50(suppl 2):11s. Available from: https://doi.org/10.1590/s1518-8787.2016050006120 [ Links ]
4. Costa CMFN, Silveira MR, Acurcio FA, Guerra Junior AA, Guibu IA, Costa KS, et al. Use of medicines by patients of the primary health care of the Brazilian Unified Health System. Rev Saúde Pública [Internet]. 2017 [cited 2020 Sep 3];51(suppl.2):18s. Available from: https://doi.org/10.11606/s1518-8787.2017051007144 [ Links ]
5. Avezum A, Oliveira GBF, Lanas F, Lopez-Jaramillo P, Diaz R, Miranda JJ, et al. Secondary CV prevention in South America in a community setting. Global Heart [Internet]. 2017 Dec [cited 2020 Sep 3];12(4):305-13. Available from: https://doi.org/10.1016/j.gheart.2016.06.001 [ Links ]
6. Khatib R, McKee M, Shannon H, Chow C, Rangarajan S, Teo K, et al. Availability and affordability of cardiovascular disease medicines and their effect on use in high-income, middle-income, and low-income countries: an analysis of the PURE study data. Lancet [Internet]. 2016 Jan [cited 2020 Sep 3];387(10013):61-9. Available from: https://doi.org/10.1016/s0140-6736(15)00469-9 [ Links ]
7. Attaei MW, Khatib R, McKee M, Lear S, Dagenais G, Igumbor EU, et al. Availability and affordability of blood pressure-lowering medicines and the effect on blood pressure control in high-income, middle-income, and low-income countries: an analysis of the PURE study data. Lancet Public Health [Internet]. 2017 Sep [cited 2020 Sep 3];2(9):e411-9. Available from: https://doi.org/10.1016/s2468-2667(17)30141-x [ Links ]
8. Wirtz VJ, Hogerzeil HV, Gray AL, Bigdeli M, Joncheere CP, Ewen MA, et al. Essential medicines for universal health coverage. Lancet. 2017 Jan [cited 2020 Sep 3];389(10067):403-76. Available from: https://doi.org/10.1016/S0140-6736(16)31599-9 [ Links ]
9. Boing AC, Bertoldi AD, Peres KG. Desigualdades socioeconômicas nos gastos e comprometimento da renda com medicamentos no Sul do Brasil. Rev Saúde Pública [Internet]. 2011 out [citado 2020 set 3];45(5):897-905. Disponível em: https://doi.org/10.1590/S0034-89102011005000054 [ Links ]
10. Dal Pizzol TS, Pons ES, Hugo FN, Bozzetti MC, Sousa MLR, Hilgert JB. Uso de medicamentos entre idosos residentes em áreas urbanas e rurais de município no Sul do Brasil: um estudo de base populacional. Cad Saúde Pública [Internet]. 2012 jan [citado 2020 set 3];28(1):104-14. Disponível em: https://doi.org/10.1590/S0102-311X2012000100011 [ Links ]
11. Boing AC, Bertoldi AD, Boing AF, Bastos JL, Peres KG. Acesso a medicamentos no setor público: análise de usuários do Sistema Único de Saúde no Brasil. Cad Saúde Pública [Internet]. 2013 abr [citado 2020 set 3];29(4):691-701. Disponível em: https://doi.org/10.1590/S0102-311X2013000400007 [ Links ]
12. Gonçalves H, Tomasi E, Tovo-Rodrigues L, Bielemann RM, Machado AKF, Ruivo ACO, et al. Population-based study in a rural area. Rev Saúde Pública [Internet]. 2018 [cited 2020 Sep 3];52(Suppl 1):3s. Available from: https://doi.org/10.11606/s1518-8787.2018052000270 [ Links ]
13. Arruda NM, Maia AG, Alves LC. Desigualdade no acesso à saúde entre as áreas urbanas e rurais do Brasil: uma decomposição de fatores entre 1998 a 2008. Cad Saúde Pública [Internet]. 2018 [citado 2020 set 3];34(6):e00213816. Disponível em: https://doi.org/10.1590/0102-311x00213816 [ Links ]
14. Instituto Brasileiro de Geografia e Estatística - IBGE. Censo 2010 [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2010 [citado 2020 set 3]. Disponível em: www.censo2010.ibge.gov.br [ Links ]
15. Dias-Damé JL, Cesar JA, Silva SM. Tendência temporal de tabagismo em população urbana: um estudo de base populacional no Sul do Brasil. Cad Saúde Pública [Internet]. 2011 nov [citado 2020 set 3];27(11):2166-74. Disponível em: https://doi.org/10.1590/S0102-311X2011001100010 [ Links ]
16. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform [Internet]. 2009 Apr [cited 2020 Sep 3];42(2):377-81. Available from: https://dx.doi.org/10.1016%2Fj.jbi.2008.08.010 [ Links ]
17. World Health Organization - WHO. ATC/DDD index 2019 [Internet]. Geneva: World Health Organization; 2019 [cited 2020 Sep 3]. Available from: https://www.whocc.no/atc_ddd_index [ Links ]
18. Associação Brasileira de Empresas de Pesquisa - ABEP. Critério de classificação econômica Brasil [Internet]. São Paulo: ABEP; 2016 [citado 2020 set 3]. 6 p. Disponível em: https://www.abep.org [ Links ]
19. Bertoldi AD, Barros AJD, Hallal PC, Lima RC. Utilização de medicamentos em adultos: prevalência e determinantes individuais. Rev Saúde Pública [Internet]. 2004 abr [citado 2020 set 3];38(2):228-38. Disponível em: https://doi.org/10.1590/S0034-89102004000200012 [ Links ]
20. Gomes VP, Silva MT, Galvão TF. Prevalência do consumo de medicamentos em adultos brasileiros: uma revisão sistemática. Ciênc Saúde Coletiva [Internet]. 2017 ago [citado 2020 set 3];22(8):2615-26. Disponível em: https://doi.org/10.1590/1413-81232017228.29412016 [ Links ]
21. Moura ML, Boszczowski I, Mortari N, Barrozo LV, Chiaravalloti Neto F, Lobo RD, et al. The impact of restricting over-the-counter sales of antimicrobial drugs: preliminary analysis of national data. Medicine [Internet]. 2015 Sep [cited 2020 Sep 3];94(38):e1605. Available from: https://doi.org/10.1097/md.0000000000001605 [ Links ]
22. Garnelo L, Lima JG, Rocha ESC, Herkrath FJ. Acesso e cobertura da Atenção Primária à Saúde para populações rurais e urbanas na região Norte do Brasil. Saúde Debate [Internet]. 2018 set [citado 2020 set 3];42(spe1):81-99. Disponível em: https://doi.org/10.1590/0103-11042018s106 [ Links ]
23. Martins RC, Silva ICM, Hallal PC. Physical activity in the rural population of Pelotas, Brazil. Rev Saúde Pública [Internet]. 2018 [cited 2020 Sep 3];52(Suppl 1):9s. Available from: https://doi.org/10.11606/s1518-8787.2018052000265 [ Links ]
24. Jaeger GP, Mola CL, Silveira MF. Alcohol-related disorders and associated factors in a rural area in Brazil. Rev Saúde Pública [Internet]. 2018 [cited 2020 Sep 3];52(Suppl 1):8s. Available from: https://doi.org/10.11606/s1518-8787.2018052000262 [ Links ]
25. Matta SR, Bertoldi AD, Emmerick ICM, Fontanella AT, Costa KS, Luiza VL. Fontes de obtenção de medicamentos por pacientes diagnosticados com doenças crônicas, usuários do Sistema Único de Saúde. Cad Saúde Pública [Internet]. 2018 mar [citado 2020 set 3];34(3):e00073817. Disponível em: http://dx.doi.org/10.1590/0102-311X00073817 [ Links ]
26. Medronho RA. Epidemiologia. 2. ed. São Paulo: Editora Atheneu; 2009. 246 p. [ Links ]
27. Levorato CD, Mello LM, Silva AS, Nunes AA. Fatores associados à procura por serviços de saúde numa perspectiva relacional de gênero. Ciênc Saúde Coletiva [Internet]. 2014 abr [citado 2020 set 3];19(4):1263-74. Disponível em: https://doi.org/10.1590/1413-81232014194.01242013 [ Links ]
28. Malta DC, Bernal RTI, Lima MG, Araújo SSC, Silva MMA, Freitas MIF, et al. Noncommunicable diseases and the use of health services: analysis of the National Health Survey in Brazil. Rev Saúde Pública [Internet]. 2017 [cited 2020 Sep 3];51(Suppl 1):4s. Available from: https://doi.org/10.1590/s1518-8787.2017051000090 [ Links ]
29. Costa KS, Francisco PMSB, Barros MBA. Utilização e fontes de obtenção de medicamentos: um estudo de base populacional no Município de Campinas, São Paulo, Brasil. Cad Saúde Pública [Internet]. 2016 [citado 2020 set 3];32(1): e00067814. Disponível em: https://doi.org/10.1590/0102-311X00067814 [ Links ]
30. Paniz VMV, Fassa AG, Facchini LA, Bertoldi AD, Piccini RX, Tomasi E, et al. Acesso a medicamentos de uso contínuo em adultos e idosos nas regiões Sul e Nordeste do Brasil. Cad Saúde Pública [Internet]. 2008 fev [citado 2020 set 3];24(2):267-80. Disponível em: https://doi.org/10.1590/S0102-311X2008000200005 [ Links ]
Received: May 07, 2020; Accepted: August 04, 2020











 texto em
texto em 


