Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.1 Brasília 2021 Epub 29-Mar-2021
http://dx.doi.org/10.1590/s1679-49742021000100030
Experience Report
List of priority congenital anomalies for surveillance under the Brazilian Live Birth Information System
1Ministério da Saúde, Secretaria de Vigilância em Saúde, Brasília, DF, Brazil
2Hospital de Clínicas de Porto Alegre, Serviço de Genética Médica, Porto Alegre, RS, Brazil
3Pontifícia Universidade Católica do Rio Grande do Sul, Escola de Medicina, Porto Alegre, RS, Brazil
4Universidade Federal do Rio Grande, Faculdade de Medicina, Rio Grande, RS, Brazil
5Ministério da Saúde, Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Brasília, DF, Brazil
Objective
To define the list of priority congenital anomalies for improving their recording on the Brazilian Live Birth Information System (Sinasc).
Methods
Based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), international protocols and meetings with specialists, the list of priority anomalies was built considering two main criteria: being diagnosable at birth and having intervention available at different levels. The list was submitted for consideration by the Brazilian Medical Genetics and Genomics Society.
Results
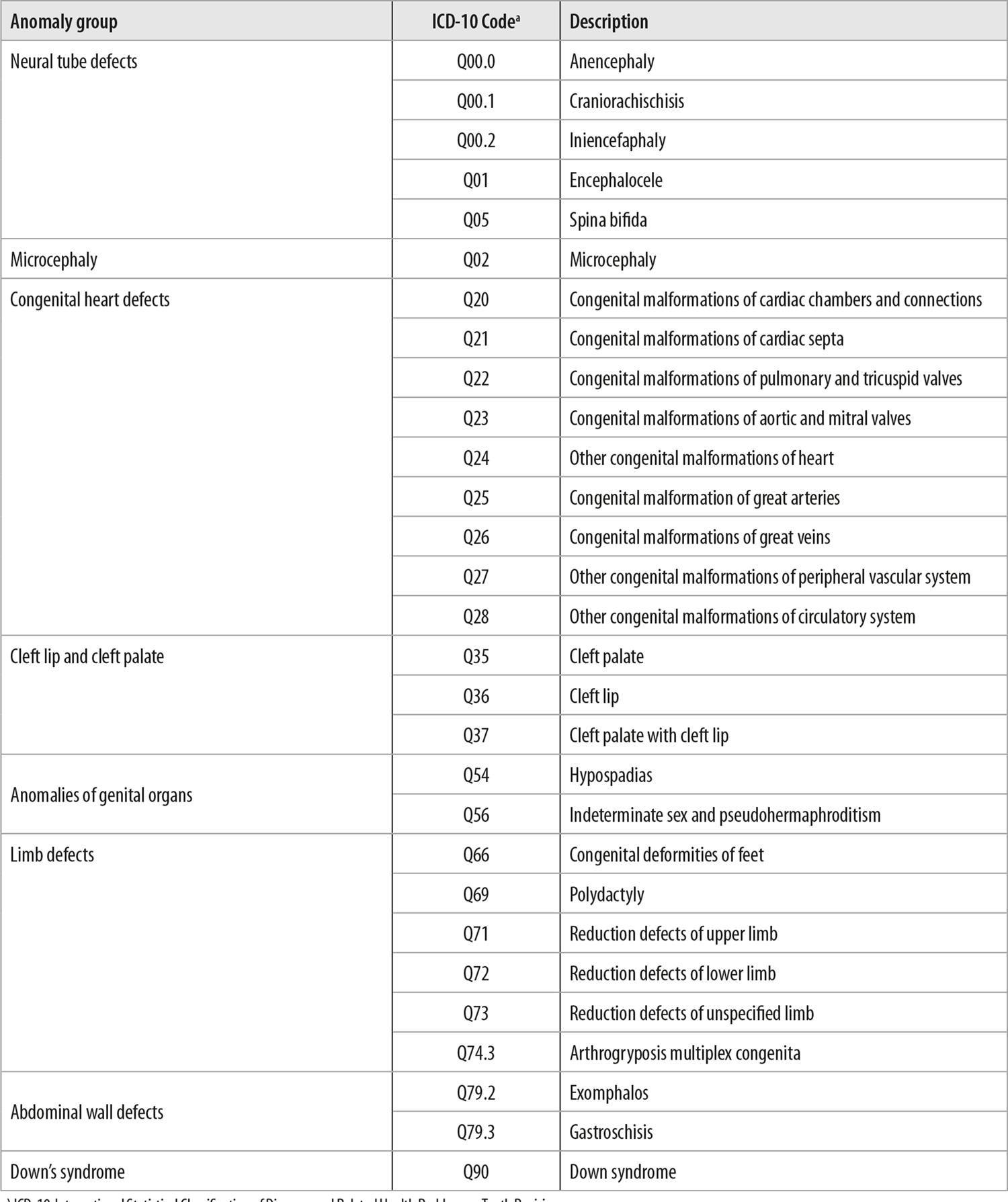
The list comprised eight groups of congenital anomalies distributed according to the type of related anomaly, as well as the affected part of the body and its corresponding code in ICD-10 Chapter XVII.
Conclusion
The list of priority congenital anomalies for notification provides a basis for improving case recording on Sinasc.
Key words: Congenital Abnormalities; Health Services; Information Systems; Epidemiological Monitoring; Directory
Introduction
Congenital anomalies comprise a wide range of structural or functional changes before birth.1Worldwide, 303,000 newborn babies are estimated to die every year in the first four weeks of life as a result of congenital anomalies, accounting for the leading cause of infant mortality in high-income countries.1 In Brazil, congenital anomalies accounted for the second leading cause of death in children under 5 years old in 2017.3 The Live Birth Information System (Sinasc) is the official system for recording congenital structural anomalies visible at childbirth for all newborn babies nationwide.5
Every year some 25,000 live births are recorded on Sinasc with some kind of congenital anomaly.4 There is, however, notorious spatial and temporal heterogeneity in notification of anomalies throughout the country. In the majority of cases, this variability is attributed to under-recording or incorrect recording of certain types of anomalies, thus hindering reliable epidemiological analysis using Sinasc system data.4 With the aim of enhancing the quality of anomaly recording on Sinasc, in discussions with specialists, the need was identified to create a list of priority anomalies to be recorded at birth. This is because some anomalies are not visible at childbirth and others, although they are diagnosable at birth, require specific technical instruments or knowledge which are not always available in all public health services or supplementary health care services.6
In the case of collection of data to be used in Public Health surveillance, quality is just as important as quantity. Furthermore, high quality data about the frequency of certain selected anomalies can be more useful than low quality data on all anomalies.2 As such, the priority list should be comprised of anomalies that are diagnosable at birth, so as to produce more reliable epidemiological indicators of this issue in Brazil and, from the Public Health point of view, offer any possible interventions.
The objective of this paper was to report on the process of building the list of priority congenital anomalies for surveillance within the scope of the Sinasc system.
Methods
This is documentary research based on the Tenth Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), international protocols9 and meetings with specialists, with the aim of establishing a list of priority congenital anomalies for notification via Sinasc. The main protocols used were the ‘Birth Defects Surveillance: A Manual for Programme Managers’ and the ‘Atlas of Selected Congenital Anomalies’, both from the collection entitled ‘Birth Defects Surveillance’, built in partnership between the World Health Organization (WHO), the United States Centers for Disease Control and Prevention (CDC/USA) and the International Clearinghouse for Birth Defects Surveillance and Research (ICBDSR) – an international network the objective of which is to promote congenital anomaly surveillance and research based on various records held around the world.9
Sinasc has collected data on births from all over Brazil since 1990. The data are registered on Live Birth Certificates (Declaração de Nascido Vivo - DNV). Since 1999 the system also captures information about congenital structural anomalies.5 In addition to information about anomalies, the DNV provides anthropometric and sociodemographic data on mother and child, data on pregnancy, date and place where childbirth occurred, mother’s place of residence, among other data.
The Law No. 12662, dated June 5th 2012, transformed the DNV into a temporary identity document valid nationwide. In turn, Law No. 13685, dated June 25th 2018, established that information about anomalies identified at birth must be recorded on the DNV. As a result, use of data contained on the DNV, as a primary source of information about congenital anomalies, is supported by law and provides coverage of practically all live births in Brazil.11
The recording of anomalies on Sinasc derives from the filling in of the DNV, using as a reference the codes contained in ICD-10 Chapter XVII – Congenital malformations, deformations and chromosomal abnormalities.5 The selection of anomalies to be considered as priority for notification via Sinasc was based on Chapter XVII, which has 619 codes associated with congenital anomalies.12 Any anomalies found which were not listed in Chapter XVII or which were not associated with a specific ICD-10 code were excluded from the selection.
Three face-to-face meetings were held between Health Ministry technical staff and specialists on the subject between 2019 and 2020. The group of specialists was comprised of professionals integrating the Latin American Congenital Malformations Study and health research and care institutions from the Brazilian state of Rio Grande do Sul.
During these meetings, in the light of international protocols for congenital anomalies surveillance,9 a preliminary list of anomalies to be considered priority for notification was compiled, using two main criteria for selecting congenital anomalies: being diagnosable at birth; and having preventive intervention at different levels. Both criteria are detailed below.
a) Diagnosable at birth
Congenital anomalies diagnosable at birth are, for the most part, those referred to as ‘major’, which are the focus of the majority of surveillance programs around the world. They are defined as structural changes that imply major medical, social or cosmetic consequences for affected individuals and, usually, require medical care. It is not unusual for a major anomaly to be accompanied by minor anomalies, i.e. other changes that do not interfere significantly with the person’s health, and the social or esthetic consequences of which are limited.2
Besides being potentially detectable at birth, it is important for anomalies to be easily diagnosable at this time, i.e. they can be detected by a wide range of health professionals and not just by specialists in dysmorphology; and that this does not require complex structures in order to be performed. The list of priority anomalies was prepared taking these limitations into consideration, given that epidemiological information arising from national surveillance can be directly influenced by issues relating to diagnosis of changes.
That proposal was based on limitations existing in the health care network for early diagnosis of some anomalies, as information recorded on Sinasc is based only on data collected in health service delivery rooms. Notwithstanding, we recognized the existence of health conditions – when identified through imaging diagnosis during pregnancy – being the object of greater attention of the medical team during birth, so as to achieve better diagnosis and then record it on the DNV.
b) Preventive intervention at different levels
Several types of anomalies can be avoided by taking simple and relatively harmless measures, such as nutritional supplementation with folic acid and iodine during pregnancy, maternal vaccination and control of maternal health problems such as diabetes mellitus; or adoption of healthy habits like abstaining from consuming alcohol and tobacco (primary prevention).1
Secondary prevention is restricted by law in Brazil. Prenatal diagnosis of anomalies followed by termination of pregnancy is not allowed other than in cases of anencephaly. Even though the impact of secondary prevention measures is slight, prenatal diagnosis continues to be important. It enables early interventions that save lives, as in the case of congenital heart defects, besides opening possibilities for referring pregnant mothers to reference centers.13
Finally, examples of tertiary prevention include pediatric surgery to correct lip and palate clefts and heart defects. When performed at the right time, these surgical interventions can drastically reduce morbidity or even related mortality. Likewise, earlier stimulation and rehabilitation methods can also be considered as examples of preventive tertiary intervention aimed at improving the quality of life of individuals with anomalies.
Revision of the list
The preliminary list was submitted to the Brazilian Medical Genetics and Genomics Society. Its opinions were analyzed and incorporated in the final list. Figure 1 provides a summarized flowchart of the process, from the first stages of the work to the final result.

a) Sinasc: Live Birth Information System.
b) ICD-10: International Statistical Classification of Diseases and Related Health Problems – Tenth Revision.
Figure 1 – Process flowchart, highlighting the main stages of building the priority list of congenital anomalies for strengthening notification on Sinasca
Results
As a starting point, it is appropriate to recall that ICD-10 contains 898 health conditions that fall into the concept of congenital anomalies, 619 of which are listed in ICD-10 Chapter XVII.12
After applying the above mentioned criteria, the preliminary list was comprised of seven groups of congenital anomalies, in the same hierarchical distribution as that of ICD-10. Initially we considered the type of related anomaly and the affected part of the body, namely: neural tube defects (Q00.0, Q00.1, Q00.2, Q01 and Q05); microcephaly (Q02); congenital heart defects (Q20-Q28); cleft lip and cleft palate (Q35-Q37); anomalies of genital organs (Q54 and Q56); limb defects (Q71, Q72 and Q73); and abdominal wall defects (Q79.2 and Q79.3). Revision by the Brazilian Medical Genetics and Genomics Society resulted in the suggestion to include congenital deformities of feet (Q66), polydactyly (Q69) and arthrogryposis multiplex congenita (Q74.3) in the ‘limb defects’ group, as well as the creation of a new group for Down’s syndrome (Q90).
All the anomalies comprising the list met both the criteria established, except congenital heart defects, for which the criterion of being easily diagnosable at birth cannot always be applied. The complete list of priority anomalies for notification on Sinasc is shown in Figure 2.
Discussion
The list of eight groups of priority congenital anomalies, as defined in this report, provides a basis for enhancing their recording on Sinasc. Given the complexities involved in diagnosing and notifying anomalies based on Sinasc, in the context of a socially and demographically diverse, populous and territorially huge country like Brazil, having a list of priority anomalies, selected based on aspects relevant for their recognition and management, revealed itself to be fundamentally important for the system.
Certain limitations were found during the process of building the list of priorities, such as using ICD-10 instead of the new version of the international classification (ICD-11), which has added a new chapter dedicated to congenital anomalies, namely Chapter XX, Developmental Anomalies, which includes new codes.12 However, we opted to use ICD-10 given that this is the version used by official health information systems in Brazil (in particular the Sinasc system), for recording diseases and health problems.14 Another possibility limitation might be the absence of documentation of the voting process to reach consensus, enabling cataloguing and calculations so as to minimize subjectivities. However, the decisions taken occurred in face-to-face meetings with specialists, following consensus and final approval by all those involved. Moreover, the list can be revised and updated: new diagnosis or preventive intervention methods can make anomalies eligible that have not been included on the list, because they did not meet the criteria established in this publication.
The anomalies selected are in agreement with the main surveillance models of these health conditions used throughout the world.16 The ‘Birth Defects Surveillance Manual for Programme Managers’, produced by ICBDSR in partnership with WHO and CDC, recommends that anomalies to be included in a new surveillance program be limited initially to structural anomalies, readily identifiable and easily recognizable during physical examination at birth.9 The list presented here includes all the anomalies suggested (neural tube defects; cleft lip and cleft palate; congenital malformations of genital organs; microcephaly (Q02); congenital heart defects; limb reduction defects and talipes; omphalocele and gastroschisis), plus three further categories considered relevant for our health system: microcephaly, congenital heart defects and Down’s syndrome.
Microcephaly (Q02), i.e. head circumference smaller than average for the same gestational age and weight, is a sentinel anomaly for congenital infections, especially for infection by Zika virus and cytomegalovirus. The severe form of microcephaly comprises a head circumference measurement three standard deviations below the average for age and sex. Microcephaly prevalence at birth in Brazil, as recorded on Sinasc, varied between 0.53/10,000 and 0.63/10,000 live births (LB) between 2010 and 2014, reaching 5.83/10,000 LB in 2015 and peaking at 7.96/10,000 LB in 2016. Also in 2016, taking only the Northeast region of Brazil, microcephaly prevalence at birth reached 13.42/10,000 LB.4 This variation can be explained, for the most part, by the epidemic of congenital syndrome associated with Zika virus infection, especially between 2015 and 2016, having its epicenter in Northeast Brazil.17 Prevention of this condition can occur on the primary level, avoiding contact with the mosquito that transmits the virus, and also on the tertiary level by means of early stimulation, rehabilitation and other measures.
Congenital heart defects are a partial exception to the criterion of easy diagnosis at birth. They are however an important cause of postnatal mortality. They are also part of the National Plan for Care for Children with Congenital Heart Defects (which recommended maternity hospitals to perform pulse oximetry on babies) and they can often be detected before birth by morphology ultrasound and fetal echocardiography.18 As such, we consider them to be an important indicator for surveillance, even though under-recording can be expected.
Down’s syndrome (Q90) was included on the list because, although diagnosis in the delivery room is not always possible, it is a more common genetic syndrome with an incidence rate of approximately 1/600 live births.19 Down’s syndrome epidemiology can therefore be considered to be a good indicator of the quality of records made at birth; moreover, its early diagnosis enables referral for family support therapy and genetic counseling.
The list presented here has a considerably specific focus on surveillance at birth, for recording on Sinasc, and it was built with the aim of increasing diagnosis and availability of preventive care, as well as rehabilitation procedures for affected children.9 However, it is important to point out that the health professionals involved in recognizing and coding anomalies need to be encouraged to continue diagnosing and recording all the anomalies contained in ICD-10 Chapter XVII, including those not listed as a priority. Once again it must be remembered that the list can be revised whenever necessary and be complemented with other conditions, taking into consideration the criteria expounded here. This initiative should encourage health professionals and health services to be better at identifying and offering due care to newborn babies with anomalies.
Articulated action between health surveillance and health care can contribute to the formulation of new public health policies.4 Health services are surveillance sentinel units, and the work done by health surveillance helps to understand health problems and to improve policies and the services they provide for, with the aim of strengthening the health care network and the various care strategies implemented by the Brazilian National Health Service (SUS). Finally, the focus on which this list has been built, with the inclusion of a specific number of anomalies, also takes on strategic relevance, to the extent that it will inform the publication, by the Ministry of Health, of norms essential to the structuring of a national congenital anomaly surveillance project, in addition to assisting the production of clear and objective instructions, directed towards health professionals who notify congenital anomalies on Sinasc.
REFERENCES
1. World Health Organization. Congenital anomalies [Internet]. [Geneva: WHO]; 2016 [acesso 28 jan. 2020]. Disponível em: https://www.who.int/news-room/fact-sheets/detail/congenital-anomalies [ Links ]
2. Centers Disease Control and Prevention. External major congenital anomalies for monitoring [Page last reviewed: October 30, 2019]. In: Birth defects surveillance toolkit [Internet]. [Washington, DC]: CDC; 2019 [acesso 12 jul 2020]. Available from: https://www.cdc.gov/ncbddd/birthdefects/surveillancemanual/facilitators-guide/module-4/mod4-1.html [ Links ]
3. Instituto de Pesquisa Econômica Aplicada. ODS 3: Assegurar uma vida saudável e promover o bem-estar para todas e todos, em todas as idades. In: Objetivos de Desenvolvimento Sustentável [Internet]. Brasília, -DF; 2019 [acesso 10 jul. 2020]. Disponível em: http://www.ipea.gov.br/portal/publicacoes [ Links ]
4. Ministério da Saúde (BR), . Secretaria de Vigilância em Saúde. Anomalias congênitas no Brasil, 2010 a 2018: análise dos dados de sistemas de informação para o fortalecimento da vigilância e atenção em saúde. Brasília, DF: MS; 2020 [acesso 10 jul. 2020]. Boletim Epidemiológico. p. 19–36. Disponível em: https://www.saude.gov.br/images/pdf/2020/marco/27/Boletim-epidemiologico-SVS-13.pdf [ Links ]
5. Ministério da Saúde (BR), Secretaria de Vigilância em Saúde. Sistema de informações sobre nascidos vivos (SINASC) [Internet]. Brasília, DF: SVS; [data desconhecida, acesso 6 jan. 2021. Disponível em: http://svs.aids.gov.br/dantps/cgiae/sinasc/ [ Links ]
6. Luquetti DV. Avaliação da qualidade das informações sobre anomalias congênitas do sistema de informações sobre nascidos vivos. Rio de Janeiro: Fundação Oswaldo Cruz; 2009. [ Links ]
7. Ministério da Saúde (BR). Como nascem os brasileiros: captação e prevalência das anomalias congênitas. In: Saúde Brasil 2018: uma análise da situação de saúde e das doenças e agravos crônicos: desafios e perspectivas. Brasília, DF: MS; 2019. p. 15–32. [ Links ]
8. Laurenti R, Siqueira AAF, Jorge MHPM, Gotlieb SLD, Pimentel EC. The importance of congenital malformations at birth. J Hum Growth Dev. 2014;24(3):328-38. [ Links ]
9. World Health Organization. Birth defects surveillance: a manual for programme managers. Geneva: WHO; 2014. [ Links ]
10. World Health Organization. Birth defects surveillance: atlas of selected congenital anomalies. Geneva: WHO; 2014. [ Links ]
11. Pedraza DF. Qualidade do sistema de informações sobre nascidos vivos (Sinasc): análise crítica da literatura. Cienc Saude Colet. 2012;17(10): 2729-37. doi: https://doi.org/10.1590/S1413-81232012001000021. [ Links ]
12. Bremm JM, Cardoso-dos-Santos AC, Magalhães VS, Medeiros-de-Souza AC, Alves RFS, Araujo VEM, et al. Anomalias congênitas na perspectiva da vigilância em saúde: compilação de uma lista com base na CID-10. Epidemiol Serv Saude. 2020;29(5):e2020164. Epub 4 dez. 2020. doi: https://doi.org/10.1590/s1679-49742020000500015. [ Links ]
13. Christianson A, Howson CP, Modell B. March of Dimes: global report on birth defects. New York: MD; 2006. [ Links ]
14. Datasus (BR), Coordenação Geral de Informações e Análise Epidemiológica. Consolidação do Sistema de informações sobre nascidos vivos: 2011 [Internet]. Brasília, DF; 2011 [acesso 10 jul. 2020]. Disponível em: http://tabnet.datasus.gov.br/cgi/sinasc/Consolida_Sinasc_2011.pdf [ Links ]
15. Coordenação-Geral de Informações e Análises Epidemiológicas (BR). Instruções para preenchimento da DN versão Jan 2011 [Internet]. [Brasília, DF: CGIAE; 2011 [acesso 19 feb. 2020]. Disponível em: http://svs.aids.gov.br/dantps/cgiae/sinasc/documentacao/ [ Links ]
16. Cardoso-dos-Santos AC, Magalhães VS, Medeiros-de-Souza AC, Bremm JM, Alves RFS, Araujo VEM, et al. International collaboration networks for the surveillance of congenital anomalies: a narrative review. Epidemiol Serv Saude2020;29(4):e2020093. doi: https://doi.org/10.5123/s1679-49742020000400003. [ Links ]
17. França GVA, Pedi VD, Garcia MHO, Carmo GMI, Leal MB, Garcia LP. Síndrome congênita associada à infecção pelo vírus Zika em nascidos vivos no Brasil: descrição da distribuição dos casos notificados e confirmados em 2015-2016. Epidemiol Serv Saude. 2018;27(2):e2017473. doi: https://doi.org/10.5123/s1679-49742018000200014. [ Links ]
18. Ministério da Saúde(BR). Portaria n. 1.727, de 11 de julho de 2017. Aprova o plano nacional de assistência à criança com cardiopatia congênita. Brasília, DF: Diário Oficial da União 12 jul. 2017 [acesso 20 jul. 2020]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2017/prt1727_12_07_2017. [ Links ]
19. Barros ALO, Barros AO, Barros GL M, Santos MTBR. Sobrecarga dos cuidadores de crianças e adolescentes com síndrome de down. Cienc Saude Colet. 2017];22(11):3625-34. doi: https://doi.org/10.1590/1413-812320172211.31102016. [ Links ]
20. Ministério da Saúde (BR), Secretaria de Vigilância em Saúde - Síndrome congênita associada à infecção pelo vírus Zika. Brasília, DF; 2019. 31 p. Boletim Epidemiológico. [ Links ]
Received: October 05, 2020; Accepted: February 11, 2021











 texto en
texto en 
 Curriculum ScienTI
Curriculum ScienTI