Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.2 Brasília 2021 Epub 21-Mayo-2021
http://dx.doi.org/10.1590/s1679-49742021000200012
Original Article
Prevalence and factors associated with intimate partner violence during pregnancy in Caxias, state of Maranhão, Brazil, 2019-20201
1Universidade Federal do Piauí, Programa de Pós-Graduação em Saúde e Comunidade, Teresina, PI, Brazil
2 Universidade Estadual do Piauí, Centro de Ciências da Saúde, Teresina, PI, Brazil
Objective
To analyze prevalence and factors associated with intimate partner violence during pregnancy.
Methods
This was a cross-sectional study, with data obtained through interviews conducted with pregnant women aged 10 to 49 years during the third trimester of pregnancy, living in Caxias, state of Maranhão, Brazil (2019-2020). The instrument of the World Health Organization Violence Against Women Study was used to identify violence. A hierarchical analysis was performed using multiple logistic regression.
Results
233 pregnant women were interviewed. The prevalence of violence during pregnancy was 33.0%, with predominance of psychological violence (18.9%). In the final hierarchical model, women aged <20 years old (ORadj=2.09 - 95%CI 1.17;3.54) and illicit drug use by intimate partner (ORadj=8.78 - 95%CI 2.13;28.92) remained as factors associated with the outcome.
Conclusion
Prevalence of violence during pregnancy was high, with illegal drug use by young women and their partners being factors associated with its occurrence.
Keywords: Violence Against Women; Intimate Partner Violence; Pregnancy; Spouse Abuse; Cross-Sectional Studies
Introduction
Violence against women is an important cause of female morbidity and mortality. Due to its high magnitude and wide dissemination, this form of violence represents a challenge for Public Health around the world.1 Data from a survey conducted between 2010 and 2017, with women aged 15 to 49 years, living in 46 countries, showed that violence occurs mainly in the family environment and that intimate partners are the main aggressors. In addition, physical abuse or sexual violence at some point in life ranges from 3.5 to 46.0%.2 Intimate partner violence (IPV) is associated with post-traumatic stress, alcohol and illicit drug abuse, sexually transmitted infections (STIs), depression, suicidal ideation and death.3,4
Pregnant women are not exempt from IPV. Episodes of violence can even start or increase during the pregnancy-puerperal cycle. Although prevalence disparities are different in various regions of the world, intimate partner violence rates during pregnancy (IPVP) are higher in Africa and Latin America.5 In Brazil, a study conducted in the city of São Paulo and in the rural area of Pernambuco showed IPVP prevalence ranging from 8.0% to 12.0%, respectively, between 2000 and 2003.6 Another study, in the Northeast region in 2016, found that 20.1% of pregnant women suffered physical violence perpetrated by their partners.7 However, psychological violence is the most frequent form reported by women exposed to IPVP.8,9
IPVP affects women of all social classes.3,10 However, younger women, with low schooling and income, with a victimization history before pregnancy and who had witnessed their mothers being beaten by their intimate partners, have been pointed out as the most vulnerable to violence during pregnancy.11,12 Early initiation of sexual activity, having three or more children,13 reporting multiple sex partners,11 unplanned pregnancy,7 induced abortion or attempting to terminate pregnancy8 are also reported as factors associated with violence during pregnancy. In addition, alcohol and illicit drug use, low schooling, unfavorable socioeconomic conditions and intimate partner unemployment determine a higher risk of suffering IPVP.6,10,12,14
Negative IPVP outcomes for maternal and fetal health are well known, such as miscarriage, premature rupture of membranes, premature birth, increased labor complications, greater number of cesarean sections and hospitalizations, low birth weight, stillbirth and perinatal death.6,12,15 Limited or no access to prenatal consultations, reduction in breastfeeding duration, mental disorders, postpartum depression and women’s low quality of life are also strongly associated with IPV type, magnitude and persistence.6,7
Despite its relevance, data on IPVP magnitude are still scarce, and insufficient information may be an obstacle to evidence-based prevention, making it impossible to identify risk groups.1,2 It can be seen that these data vary frequently, depending on the sociocultural context in which women live. Thus, it is important to understand the panorama of IPVP in places without information on the subject, to support strategy planning to reduce cases at the local level, in addition to sensitizing professionals responsible for care for pregnant women about the relevance of this Public Health problem.
Thus, this study aimed to analyze prevalence and factors associated with intimate partner violence during pregnancy, in the municipality of Caxias, State of Maranhão, Brazil.
Methods
This was a cross-sectional study with pregnant women from Caxias, state of Maranhão, conducted between September 2019 and March 2020.
Caxias occupies an area of 5,196,769 km2 and is the third largest city in territorial extension in the State of Maranhão. Located in the eastern region of the state, 374km from the capital São Luís, and 70 km from Teresina, state capital of Piauí. The municipality’s population was estimated at 165,525 inhabitants in 2020, mostly female (51.6%) and without education or with only incomplete elementary school education (79.5%). The city has 36 primary health centers (PHC) that provide primary health care for 70.4% of its population.16
The study participants were pregnant women who were in the third trimester of pregnancy (from week 28), living in the municipality and with prenatal follow-up in the Brazilian National Health System (SUS) in the period analyzed. Women under 18 years old and whose guardians have not sign the Free and Informed Consent Form were excluded from the study, although they had agreed to participate, in addition to pregnant women who were not able to answer the interview questions.
Based on the total number of pregnant women in the third trimester of pregnancy (n=327), during the study period, 5% error, 95% confidence level, 80% power and 10% increase for losses, a minimum sample of 204 women was estimated. Convenience sampling was used, given the impossibility of obtaining a random sample representative of the population of pregnant women from Caxias. All pregnant women in the third trimester of pregnancy who had been registered were contacted.
Data collection was performed by a trained researcher and occurred, as a priority, at a PHC, in a reserved room, before or after prenatal consultations, without the presence of companions. For pregnant women who were not at a PHC, the interview was conducted at home, except when there were other people at the place or when it was not possible to conduct the interview in a reserved room. For the home interviews, after three unsuccessful visits, the pregnant woman was excluded from the study.
Data were collected during face-to-face interviews, using two structured forms with closed questions.
The first form was comprised of an IPV research instrument, known as the World Health Organization Violence Against Women Study (WHO VAW), validated in Brazil.17 The WHO VAW, used to assess the occurrence of violence during pregnancy, is comprised of 13 questions divided into 3 subscales, which assess the occurrence of physical, sexual and psychological violence, with 4 items to identify psychological violence, 6 items for physical violence and 3 items for sexual violence. The WHO VAW form considers that an affirmative answer is enough to indicate a case of violence.17 This study considered an IPVP case to be each account reported by the interviewees of some type of violence (physical or sexual or psychological) perpetrated by their intimate partner during pregnancy. Intimate partners were considered to be a boyfriend/ex-boyfriend, husband/ex-husband or any individual who, even without formal union, has established an affective relationship and has or has had a sexual relationship with the woman.18
The second form addressed the following variables:
-
Sociodemographic
- Age group (in years: 10-14; 15-19; 20-29; 30-39; 40-49);
- Race/skin color (white; black; brown; yellow; indigenous);
- Schooling (in completed years of study: 0-4; 5-8; 9-11; ≥12);
- Marital status (with a partner; without a partner);
- Own income source (yes; no);
- Occupational status (with occupation; without occupation);
- Housing status (home owner; rented house).
-
Obstetrics
- Number of pregnancies (≤2; >2);
- Number of births (≤2; >2);
- Previous miscarriage (yes; no);
- Number of prenatal consultations (<6; ≥6).
-
Health-related
- Alcohol consumption (yes; no) and illicit drug use (yes; no).
-
Victimization history
- Psychological violence before 15 years old (yes; no; does not apply) and after 15 years old (yes; no; does not apply);
- Physical violence before 15 years old (yes; no; does not apply) and after 15 years old (yes; no; does not apply);
- Sexual violence before 15 years old (yes; no; does not apply) and after 15 years old (yes; no; does not apply);
- Witnessed violence against their mothers (yes; no);
- Type of domestic violence that was witnessed (psychological; physical; sexual).
-
About the intimate partner
- Age group (in years: 10-14; 15-19; 20-29; 30-39; 40-49; ≥50);
- Race/skin color (white; black; brown; yellow; indigenous);
- Schooling (in years of study: 0-4; 5-8; 9-11; ≥12);
- Professional occupation (with occupation; without occupation);
- Alcohol consumption (yes; no) and illicit drug use (yes; no).
A pilot test was performed with ten pregnant women to enhance the form. After adjustments, the data collected in the pre-test were discarded. At the time of the interview, pregnant women identified as victims of violence were instructed to seek specialized care services for women in situations of violence in the municipality.
Data were analyzed using descriptive statistics, with absolute and relative frequencies, using the Statistical Package for the Social Sciences (SPSS) version 20. The prevalence of violence was calculated by identifying isolated occurrence, by type of violence, and simultaneous occurrence of two or more types of violence suffered by each participant, using a Venn diagram. For inferential analysis, all independent variables were dichotomized. Logistic regression was used to evaluate association between the independent variables (sociodemographic characteristics of pregnant women and their intimate partners; obstetric characteristics; health-related behaviors; history of violence against women) and the dependent variable (IPVP), expressed in values of crude odds ratios (ORcr) and adjusted odds ratios (ORadj), with a 95% confidence interval (95%CI). As a cutoff point for diagnosing multicollinearity, a variance inflation factor (VIF) below 10 was adopted.
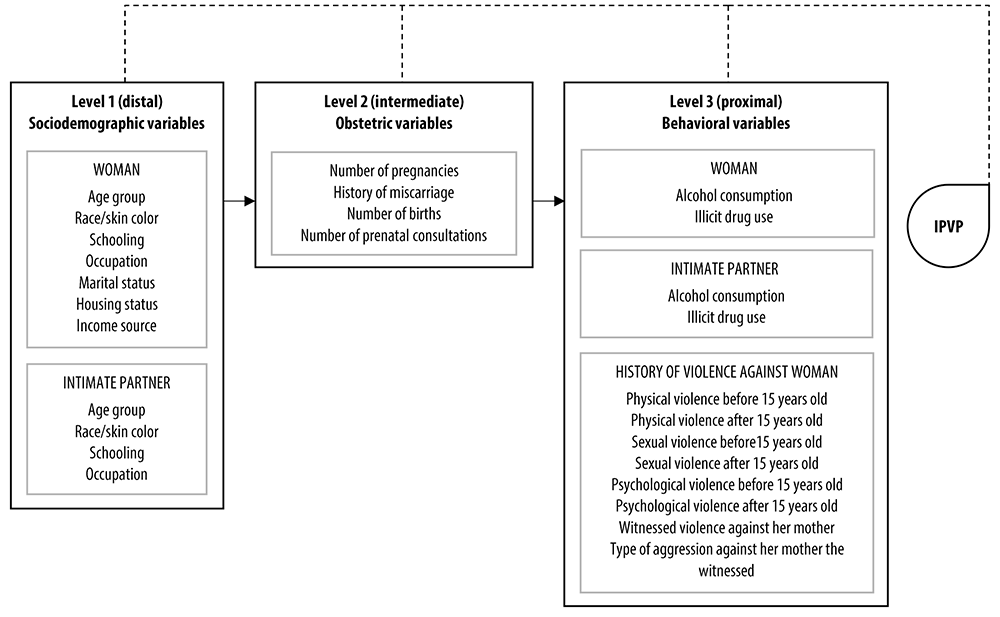
The independent variables were treated hierarchically (Figure 1), describing the relationships between IPVP risk factors, with three determinant levels: distal, intermediate and proximal. The hierarchization of the variables took previous studies as a reference.12,19 The distal level in relation to the outcome was comprised of sociodemographic variables of the women and their partners; while the intermediate level was comprised of obstetric characteristics; and the proximal level was comprised of behavioral aspects of the women and their partners, as well as characteristics regarding history of violence against women. The hierarchical model was analyzed according to the distal-proximal direction. Initially, only distal level variables were included in the model, whereby those with p≤0.10 were kept in the model. Then, the intermediate level variables were included, and those with p≤ 0.10 were kept on this level and adjusted for the previous level variables. At the proximal level, the variables were adjusted by all of the previous levels. In the final model, the variables that presented p<0.05 were considered to be associated with the outcome.
The study project was approved by the Human Research Ethics Committee of the Federal University of Piauí (CEP/UFPI): Certificate of Submission for Ethical Appraisal (CAAE) No. 16088619.9.0000.5214 Opinion No. 3.429.407, issued on July 1, 2019. All selected pregnant women signed the Free and Informed Consent Form as a condition for their participation in the study.
Results
A total of 233 pregnant women were interviewed and nine of them were excluded from the study. The prevalence of some type of violence during pregnancy was 33.0% (n=77), with isolated psychological violence being the most frequent (18.9%), followed by overlapping physical and psychological violence (5.2%) and isolated physical violence (4.3%) (Figure 2). Insults represented the most common type of psychological violence committed by partners (n=46; 19.7%), while slapping (n=18; 7.7%) and pushing (n=15; 6.4%) were the most common acts of physical violence. Physically forced sexual intercourse by the partner was the most reported (n=7; 3.0%) among types of sexual violence.
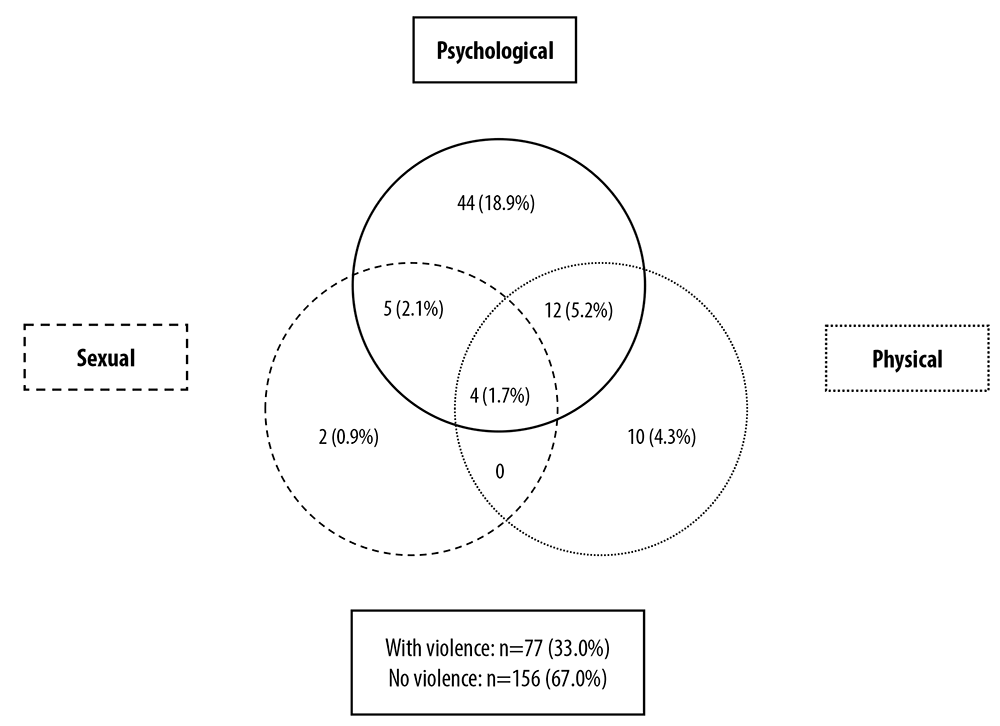
Figure 2 Prevalence of psychological, physical and sexual violence perpetrated by the intimate partner during pregnancy, Caxias, state of Maranhão, Brazil, 2019-2020
There was association between IPVP and age below 20 years (ORcr=2.59 - 95%CI 1.47;4.59). Pregnant women whose partners had no occupation (ORcr=3.32 - 95%CI 1.51;7.02) and used illicit drugs (ORcr= 11.33 - 95%CI 3.15;40.80) were more likely to be victims of violence during pregnancy (Table 1). There was also a higher chance of IPVP among those who suffered physical violence before (ORcr=2.63 - 95%CI 1.46;4.73) and after 15 years old (ORcr= 2.45 - 95%CI 1.22;4.93), sexual violence before 15 years old (OR=3.30 - 95%CI 1.13;9.67) and psychological violence before (ORcr=3.28 - 95%CI 1.84;5.89) and after 15 years old (ORcr=2.77 - 95%CI 1.59;4.94); and, also among pregnant women who witnessed physical and psychological violence against their mothers (ORcr= 2.90 - 95%CI 1.03;8.14) (Table 2).
Table 1 Association of sociodemographic and behavioral variables with the occurrence of intimate partner violence during pregnancy, Caxias, state of Maranhão, Brazil, 2019-2020
| Variables | All (n=233) | IPVPa (n=77) | ORcrb | 95%CIc | p-value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Age group (in years) | |||||||
| <20 | 78 | 33.5 | 37 | 48.0 | 2.59 | 1.47;4.59 | 0.001 |
| ≥20 | 155 | 66.5 | 40 | 52.0 | 1.00 | ||
| Race/skin colord | |||||||
| White | 11 | 4.7 | 2 | 2.6 | 1.00 | ||
| Black | 209 | 89.7 | 71 | 92.2 | 2.15 | 0.43;10.81 | 0.352 |
| Education (in years of study) | |||||||
| ≤8 | 89 | 38.2 | 34 | 44.1 | 1.00 | ||
| ≥9 | 144 | 61.8 | 43 | 55.9 | 0.68 | 0.39;1.20 | 0.189 |
| Marital status | |||||||
| With a partner | 189 | 81.1 | 59 | 76.6 | 1.00 | ||
| Without a partner | 44 | 18.9 | 18 | 23.4 | 1.52 | 0.78;2.99 | 0.220 |
| Own income source | |||||||
| Yes | 64 | 27.5 | 15 | 19.5 | 1.00 | ||
| No | 169 | 72.5 | 62 | 80.5 | 1.89 | 0.98;3.65 | 0.057 |
| Occupation | |||||||
| With occupation | 58 | 24.9 | 16 | 20.8 | 1.00 | ||
| No occupation | 175 | 75.1 | 61 | 79.2 | 1.40 | 0.73;2.70 | 0.309 |
| Housing status | |||||||
| Home owner | 168 | 72.1 | 53 | 68.8 | 1.00 | ||
| Rented house | 65 | 27.9 | 24 | 31.2 | 1.27 | 0.69;2.31 | 0.435 |
| Alcohol consumption by pregnant women | |||||||
| Yes | 62 | 26.6 | 23 | 29.9 | 1.27 | 0.69;2.35 | 0.429 |
| No | 171 | 73.4 | 54 | 70.1 | 1.00 | ||
| Illicit drug use by pregnant women | |||||||
| Yes | 6 | 2.6 | 3 | 3.9 | 2.06 | 0.41;10.49 | 0.381 |
| No | 227 | 97.4 | 74 | 96.1 | 1.00 | ||
| Partner age groupe | |||||||
| <20 | 32 | 13.7 | 11 | 14.3 | 0.96 | 0.47;2.28 | 0.923 |
| ≥20 | 197 | 84.6 | 66 | 85.7 | 1.00 | ||
| Partner race/skin colorf | |||||||
| White | 50 | 21.5 | 14 | 18.2 | 1.00 | ||
| Black | 167 | 71.7 | 56 | 72.7 | 1.17 | 0.53;2.63 | 0.696 |
| Partner’s education (in years of study)g | |||||||
| ≤8 | 85 | 36.5 | 32 | 41.5 | 1.00 | ||
| ≥9 | 127 | 54.5 | 39 | 50.6 | 0.73 | 0.41;1.31 | 0.295 |
| Partner occupancy | |||||||
| With occupation | 200 | 85.8 | 58 | 75.3 | 1.00 | ||
| No occupation | 33 | 14.2 | 19 | 24.7 | 3.32 | 1.51;7.02 | 0.002 |
| Alcohol consumption by the partner | |||||||
| Yes | 149 | 63.9 | 54 | 70.1 | 1.50 | 0.85;2.71 | 0.169 |
| No | 84 | 36.1 | 23 | 29.9 | 1.00 | ||
| Illicit drug use by the partner | |||||||
| Yes | 17 | 7.3 | 14 | 18.2 | 11.33 | 3.15;40.80 | <0.001 |
| No | 216 | 92.7 | 63 | 81.8 | 1.00 | ||
a) IPVP: intimate partner violence during pregnancy; b) ORcr: crude odds ratio; c) 95%CI: 95% confidence interval; d) Did not know/did not want to answer: 2 (0.9%); yellow, 10 (4.3%)/3 (1.3%) with IPVP; indigenous, 1 (0.4%)/1 (1.3%) with IPVP; e) Did not know/did not want to answer: 4 (1.7%); f) Yellow: 15 (6.4%)/3 (1.3%) with IPVP; indigenous, 1 (0.4%)/1 (1.3%) with IPVP; g) Did not know/did not want to answer: 21 (9.0%)/6 (7.8%) with IPVP.
Table 2 Association of obstetric variables and history of violence against woman with the occurrence of intimate partner violence during pregnancy, Caxias, state of Maranhão, Brazil, 2019-2020
| Variables | All (n=233) | IPVPa (n=77) | ORcrb | 95%CIc | p-value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Physical violence before 15 years old | |||||||
| Yes | 131 | 56.2 | 55 | 71.4 | 2.63 | 1.46;4.73 | 0.001 |
| No | 102 | 43.8 | 22 | 28.6 | 1.00 | ||
| Physical violence after 15 years oldd | |||||||
| Yes | 40 | 17.2 | 20 | 26.0 | 2.45 | 1.22;4.93 | 0.012 |
| No | 183 | 78.5 | 53 | 68.8 | 1.00 | ||
| Sexual violence before 15 years old | |||||||
| Yes | 15 | 6.4 | 9 | 11.7 | 3.30 | 1.13;9.67 | 0.029 |
| No | 218 | 93.6 | 68 | 88.3 | 1.00 | ||
| Sexual violence after 15 years oldd | |||||||
| Yes | 18 | 7.7 | 9 | 11.7 | 2.20 | 0.83;5.81 | 0.110 |
| No | 205 | 88.0 | 64 | 83.1 | 1.00 | ||
| Psychological violence before 15 years old | |||||||
| Yes | 119 | 51.1 | 54 | 70.1 | 3.28 | 1.84;5.89 | <0.001 |
| No | 114 | 48.9 | 23 | 29.9 | 1.00 | ||
| Psychological violence after 15 years olde | |||||||
| Yes | 100 | 42.9 | 45 | 58.4 | 2.77 | 1.59;4.94 | 0.001 |
| No | 123 | 52.8 | 28 | 36.4 | 1.00 | ||
| Witnessed violence against their mothers | |||||||
| Yes | 67 | 28.8 | 28 | 36.4 | 1.71 | 0.95;4.94 | 0.073 |
| No | 166 | 71.2 | 49 | 63.6 | 1.00 | ||
| Type of violence witnessede | |||||||
| Physical and psychological | 24 | 10.3 | 14 | 18.2 | 2.90 | 1.03;8.14 | 0.043 |
| Others | 43 | 18.5 | 14 | 18.2 | 1.00 | ||
| Number of pregnancies | |||||||
| ≤2 | 157 | 67.4 | 53 | 68.9 | 1.00 | ||
| >2 | 76 | 32.6 | 24 | 31.2 | 0.90 | 0.50;1.63 | 0.740 |
| Number of births | |||||||
| ≤2 | 203 | 87.1 | 69 | 89.6 | 1.00 | ||
| >2 | 30 | 12.9 | 8 | 10.4 | 0.70 | 0.29;1.67 | 0.426 |
| History of miscarriage | |||||||
| Yes | 51 | 21.9 | 18 | 23.4 | 1.00 | ||
| No | 182 | 78.1 | 59 | 76.6 | 0.87 | 0.46;.1.69 | 0.700 |
| Number of prenatal consultations | |||||||
| <6 | 114 | 48.9 | 40 | 51.9 | 1.00 | ||
| ≥6 | 119 | 51.1 | 37 | 48.1 | 0.83 | 0.48;1.44 | 0.517 |
a) IPVP: intimate partner violence during pregnancy; b) ORcr: crude odds ratio; c) 95%CI: 95% confidence interval; d) Does not apply: 10 (4.3%)/4 (5.2%) with IPVP; e) Does not apply: 166 (71.2%)/49 (63.6%) with IPVP.
Table 3 shows the data following hierarchical analysis. At level 1 (distal), the <20 year-old age group was associated with IPVP (ORadj=2.18 - 95%CI 1.15;4.18). None of the level 2 (intermediate) variables showed significance regarding the outcome in the crude analysis, therefore they were not included in the model. In the final model, women in the <20 year-old age group (ORadj=2.09 - 95%CI 1.17;3.54) and illicit drug use by intimate partners (ORadj=8.78 - 95%CI 2.13;28.92) remained associated with IPVP.
Table 3 Hierarchical analysis of factors associated with intimate partner violence during pregnancy, Caxias, state of Maranhão, Brazil, 2019-2020
| Variables | Model 1a | Model 2b | ||||
|---|---|---|---|---|---|---|
| ORadjc | 95%CId | p-value | ORadjc | 95%CId | p-value | |
| Age group (in years) | ||||||
| <20 | 2.18 | 1.15;4.18 | 0.023 | 2.09 | 1.17;3.54 | 0.031 |
| ≥20 | 1.00 | 1.00 | ||||
| Income source | ||||||
| Yes | 1.00 | 1.00 | ||||
| No | 1.08 | 0.86;2.56 | 0.211 | 1.06 | 0.84;2.45 | 0.465 |
| Partner has professional occupation | ||||||
| Yes | 1.00 | 1.00 | ||||
| No | 1.87 | 0.79;4.33 | 0.372 | 1.51 | 0.82;3.65 | 0.127 |
| Illicit drug use by the partner | ||||||
| Yes | 8.78 | 2.13;28.92 | 0.001 | |||
| No | 1.00 | |||||
| Physical violence before 15 years old | ||||||
| Yes | 1.55 | 0.93;4.55 | 0.134 | |||
| No | 1.00 | |||||
| Physical violence after 15 years old | ||||||
| Yes | 1.73 | 0.81;3.60 | 0.342 | |||
| No | 1.00 | |||||
| Sexual violence before 15 years old | ||||||
| Yes | 1.44 | 0.67;4.59 | 0.320 | |||
| No | 1.00 | |||||
| Psychological violence before 15 years old | ||||||
| Yes | 1.68 | 0.75;6.01 | 0.128 | |||
| No | 1.00 | |||||
| Psychological violence after 15 years old | ||||||
| Yes | 1.33 | 0.56;5.74 | 0.530 | |||
| No | 1.00 | |||||
| Witnessed aggression against their mothers | ||||||
| Yes | 1.23 | 0.82;2.96 | 0.125 | |||
| No | 1.00 | |||||
| Type of aggression against their mothers they witnessed | ||||||
| Physical and psychological | 1.94 | 0.74;6.04 | 0.076 | |||
| Others | 1.00 | |||||
a) Level 1 (distal) adjusted alone; b) Level 3 (proximal) adjusted by level 1 variables; c) ORadj: adjusted odds ratio; d) 95%CI: 95% confidence interval.
Discussion
This study was the first to estimate IPVI prevalence and associated factors in women living in Caxias. The data showed high prevalence of IPVP, and occurrence of isolated psychological violence was the most reported, followed by simultaneous occurrence of physical and psychological violence. A group of potential IPVP risk factor variables emerged from crude analysis. Young women, with a history of personal or family violence, with a partner who was unemployed and/or an illicit drug user, were more likely to be victims of violence during pregnancy. However, in the hierarchical analysis, only the use of illicit drugs by partners and the under 20 year-old age group remained associated with occurrence of IPVP.
The prevalence of IPVP observed in Caxias was higher than that found in most other studies.2,5,15 Data on IPVP prevalence in 19 countries, between 1998 and 2007, showed magnitude between 2.0 and 13.5%.3 A similar pattern was observed in a study conducted in the city of Rio de Janeiro, between 2006 and 2007, when IPVP prevalence was found in 5.1% of the interviewees.20 Higher prevalence, similar to that found in this study, was found in surveys conducted in the rural area of Pernambuco, between 2000 and 2003 (32%),6 and in São Luís, the state capital of Maranhão, in 2010 (49.6%).21 It is possible that the high prevalence of IPVP in the Northeast region is related to the social and structural contexts, with norms and values characteristic of a patriarchal culture that is considered responsible for violence against women.
Several factors may contribute to discrepancies in the prevalence of IPVP. First, it is worth considering that different instruments have been used to identify this phenomenon. One of the positive points of the use of WHO VAW would be the comparability between studies conducted in locations and regions with different sociocultural contexts.7,9,11,14,15 Second, the sample size and gestational period of the study participants may also influence the outcome. The inclusion of women in all gestational periods, as well as the retrospective evaluation of IPVP, performed in the postpartum period, may contribute to the difference in the prevalence found in the study.12,13 In addition, different definitions of IPVP were used in the surveys.13,20 However, it is possible that the indicators of IPVP occurrence do not reflect the true magnitude of the problem: many women do not report the violent acts of which they have been victims, either for fear of reporting such situations, or due to financial and emotional dependence on their partner.2,18
A higher frequency of psychological violence can be seen in this study, followed by concomitant psychological and physical violence, as observed in other studies.8,12,15,21 The predominance of psychological violence among most victims of IPV may be related to the embarrassment of reporting more severe types of marital violence and also to the fear of being the target of social judgements.13,15
Use of illicit drugs by intimate partners, verified by the hierarchical analysis of the cases investigated in Caxias, represented a risk factor for IPVP, as observed in other locations.8,12,22 Data from 1,379 women living in Campinas, state of São Paulo, showed that women were almost twice as likely to be victims of physical and sexual violence during pregnancy due to the use of illicit drugs by their partners.12 In Vitória, ES, the use of drugs by intimate partners also increased the probabilities of women being victims of psychological violence,23 making them more vulnerable to marital violence.
Use of illicit drugs by the aggressor, by the victim or both, is related to a wide range of episodes of domestic violence, which may culminate in physical trauma that endangers women’s lives.24,25 By reducing their ability to control their actions, use of illicit substances by partners makes women more vulnerable to conflict and often triggers a vicious cycle of violence.22 Arguments, victim blaming, minimizing aggression and promises of behavior change have been part of the usual IPVP script when there is illicit drug use by the partner.19,25,26
It is worth noting that, although drug use has played an important role in the occurrence of violent episodes, acting as a possible potentiator of aggression, its relationship with the occurrence of violence has not been fully elucidated.26 However, as intimate partner illicit drug use reduces, there is a decrease in cases of violence against women.24,26 Therefore, it is necessary to develop actions that articulate gender issues, in addition to those related to the use of licit and illicit drugs.23,24 Despite several studies having demonstrated use of alcohol by partners and that this can lead to the creation of conditions favorable to violence,12,14,19 this study did not find association between this variable and IPVP. Factors such as small sample size, varied violence typology and different ways of identifying alcohol consumption influence this association.19 It is also possible that the result of this study is related to the strength of the association observed with illicit drugs, thus masking the effect of alcohol.
A study conducted in ten countries, including Brazil, between 2000 and 2003, found that younger age was strongly associated with increased risk of IPV in all those countries,27 similarly to data from this study. Studies conducted in the city of Rio de Janeiro and in Recife, state capital of Pernambuco, also found higher prevalence of IPVP in women under the age of 20.7,20However, in São Luís,21 and in the city of São Paulo,13 IPVP was more prevalent in women aged 25 years or older, while in Turkey, the 45 to 49 year-old age group was identified as a risk factor for IPV among pregnant women.26 There is no consensus on young age of women on its own being a factor for the occurrence of IPV; this may be associated with other determining conditions, such as low schooling, unemployment, financial dependence on the intimate partner, and early and unplanned pregnancy.2,9,13 Thus, increasing age, education level and greater financial independence are protective characteristics associated with lower exposure and tolerance of women to partner violence.19,25
The sociodemographic and behavioral characteristics of women and intimate partners, as well as women’s exposure to violence in periods prior to pregnancy, have been identified as risk factors for IPVP.2,7,13,20,21,27,28 The findings of our study are aligned with the main findings in the literature. The hierarchical analysis showed that the absence of own income source and victimization history did not represent risk factors for the occurrence of IPVP. Similarly, intimate partners not having a professional occupation was also associated with violence during pregnancy.
Although intimate partner unemployment is known as a risk factor for IPV,2,19,22,28 it was not associated with IPVP, according to the results of the investigation in Caxias. In the municipality of Maringá, state of Paraná, on the contrary, intimate partner unemployment was significantly associated with IPVP,22 and also with physical violence against pregnant women in Recife.28 However, the reason why partner unemployment increases the chances of exposure to IPV, including in the gestational period, was not clarified. It is possible that there is an interrelationship between this type of violence and factors associated with unemployment, such as poverty and the inability of the partner to fulfill his breadwinner role, especially in a context of the family getting bigger due to pregnancy.2,19,29
Diverging from the findings frequently found in national and international studies,9,29,25 both exposure to physical and psychological violence before and after 15 years old, and the occurrence of sexual violence prior to this age, did not remain associated with the outcome in the hierarchical analysis of this study. According to data from a survey conducted in 2014, in the city of Florianópolis, state of Santa Catarina, women who had suffered partner violence within 12 months prior to pregnancy were 15.8 times more likely to be exposed to this type of violence.9 However, IPVP is not usually an isolated and one-off event: it is estimated that 60 to 96% of the victims of IPVP have been exposed before the gestational period, and that IPV episodes in pregnancy are just the continuity of previous events.29 It is also worth adding: having witnessed violence against their mothers proved to be a factor associated with IPVP: women who have seen their mothers suffer IPV are up to three times more likely to be victims of IPV,28 and there is still a risk of their testimony reinforcing a mistaken perception of this type of violence and its normalization as a fact inherent to conjugal relationships, and consequently, greater tolerance to IPV, albeit unacceptable.16,26
This study has limitations to be considered. First, the cross-sectional design of the study did not allow a relationship of temporality to be established between IPVP and the variables analyzed. Secondly, the approach did not include women in the first and second trimesters of pregnancy, although, in this initial period of pregnancy, pregnant women are not exempt from violent attitudes and actions perpetrated by an intimate partner. Moreover, the results of this study concern only women who got prenatal follow-up in public health services in Caxias, it has no information about the prevalence and factors associated with IPVP against pregnant women followed up in private services in the municipality. Thirdly and lastly, the participants were not selected by probabilistic sampling, and it is possible that the sample studied does not represent the universe investigated in a completely reliable manner.
Despite the limitations considered, this study deserves attention because it was the first to evaluate IPVP in Caxias, where there has been frequent occurrence of episodes of violence against pregnant women resulting in their insecurity and risk caused by violence during pregnancy. The results found can provide support for strategy planning and implementation of actions in response to violence against pregnant women, perpetrated by an intimate partner, in the municipality of Caxias. Primary health care services play a significant role in identifying aggression suffered by pregnant women. All health professionals involved in prenatal care should be aware of both signs of the presence of this form of violence and also opportunities for revealing it, and offer their support to these women not just when requested. Strategies such as active listening, avoiding judgment, providing moral comfort and information on legal rights are particularly important for a woman to make a decision in the face of her partner’s violence against her body and her conceptus.
REFERENCES
1. Kusuma YS, Babu BV. Elimination of violence against women and girls as a global action agenda. J Inj Violence Res [Internet]. 2017 Jul [cited 2020 Oct 10];9(2):117-21. Available from: https://doi.org/10.5249/jivr.v9i2.908 [ Links ]
2. Coll CVN, Ewerling F, García-Moreno C, Hellwig F, Barros AJD. Intimate partner violence in 46 low-income and middle-income countries: an appraisal of the most vulnerable groups of women using national health surveys. BMJ Global Health [Internet]. 2020 Jan [cited 2020 Oct 10];5(1):e002208. Available from: https://doi.org/0.1136/bmjgh-2019-002208 [ Links ]
3. Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet [Internet]. 2010 Jul [cited 2020 May 12];376(9734):41-8. Available from: https://doi.org/10.1016/S0140-6736(10)60548-X [ Links ]
4. Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, et al. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med [Internet]. 2013 May [cited 2020 Apr 17];10(5):e1001439. Available from: https://doi.org/10.1371/journal.pmed.1001439 [ Links ]
5. Devries KM, Kishor S, Johnson H, Stöckl H, Backus LJ, Garcia-Moreno C, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters [Internet]. 2010 Nov [cited 2020 Apr 17];18(36):158-70. Available from: https://doi.org/10.1016/S0968-8080(10)36533-5 [ Links ]
6. Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet [Internet]. 2006 Oct [cited 2020 Jun 22];368(9543):1260-9. Available from: https://doi.org/10.1016/S0140-6736(06)69523-8 [ Links ]
7. Carneiro JF, Valongueiro S, Ludermir AB, Araújo TVB. Violência física pelo parceiro íntimo e uso inadequado do pré-natal entre mulheres do Nordeste do Brasil. Rev Bras Epidemiol [Internet]. 2016 abr-jun [citado 2019 maio 3];19(2):243-55. Disponível em: https://doi.org/10.1590/1980-5497201600020003 [ Links ]
8. Viellas EF, Gama SGN, Carvalho ML, Pinto LW. Fatores associados à agressão física em gestantes e os desfechos negativos no recém-nascido. J Pediatr [Internet]. 2013 jan-fev [citado 2019 jul 25];89(1):83-90. Disponível em: https://doi.org/10.1016/j.jped.2013.02.013 [ Links ]
9. Pires MRM, Locatelli TZ, Rojas PFB, Lindner SR, Bolsoni CC, Coelho EBS. Prevalência e os fatores associados da violência psicológica contra gestantes em capital no Sul do Brasil. Saúde Transf Soc [Internet]. 2017 [citado 2020 jun 22];8(1):29-39. Disponível em: http://incubadora.periodicos.ufsc.br/index.php/saudeetransformacao/article/view/3797 [ Links ]
10. Chisholm CA, Bullock L, Ferguson II JE. Intimate partner violence and pregnancy: epidemiology and impact. Am J Obstet Gynecol [Internet]. 2017 Aug [cited 2020 Jan 2];217(2):141-4. Available from: https://doi.org/10.1016/j.ajog.2017.05.042 [ Links ]
11. Costa DCS, Ribeiro MRC, Batista RFL, Valente CM, Ribeiro JVF, Almeida LA, et al. Factors associated with physical violence against pregnant women from São Luís, Maranhão State, Brazil: an approach using structural equation modeling. Cad Saúde Pública [Internet]. 2017 Jan [cited 2020 Jan 2];33(1):e00078515. Available from: https://doi.org/10.1590/0102-311x00078515 [ Links ]
12. Audi CAF, Segall-Corrêa AM, Santiago SM, Andrade MGG, Pérez-Escamilla R. Violência doméstica na gravidez: prevalência e fatores associados. Rev Saúde Pública [Internet]. 2008 out [citado 2020 jun 22];42(5):877-85. Disponível em: https://doi.org/10.1590/S0034-89102008005000041 [ Links ]
13. Durand JG, Schraiber LB. Violência na gestação entre usuárias de serviços públicos de saúde da Grande São Paulo: prevalência e fatores associados. Rev Brasil Epidemiol [Internet]. 2007 set [citado 2019 jul 25];10(3):310-22. Disponível em: https://doi.org/10.1590/S1415-790X2007000300003 [ Links ]
14. Mahenge B, Stöckl H, Abubakari A, Mbwambo J, Jahn A. Physical, sexual, emotional and economic intimate partner violence and controlling behaviors during pregnancy and postpartum among women in Dar es Salaam, Tanzania. PLoS One [Internet]. 2016 Oct [cited 2020 Jun 22];11(10):e0164376. Available from: https://doi.org/10.1371/journal.pone.0164376 [ Links ]
15. Barros EN, Silva MA, Falbo-Neto GH, Lucena SG, Ponzo L, Pimentel AP. Prevalência e fatores associados à violência por parceiro íntimo em mulheres de uma comunidade em Recife/Pernambuco, Brasil. Ciênc Saúde Coletiva [Internet]. 2016 fev [citado 2019 abr 13];21(2):591-8. Disponível em: https://doi.org/10.1590/1413-81232015212.10672015 [ Links ]
16. Instituto Brasileiro de Geografia e Estatística -IBGE. Caxias. Panorama [Internet]. Rio de Janeiro: IBGE; 2020 [citado 2020 set 20]. Disponível em: https://cidades.ibge.gov.br/brasil/ma/caxias/panorama [ Links ]
17. Schraiber LB, Latorre MRD, França Jr I, Segri NJ, D’Oliveira AFPL. Validade do instrumento WHO VAW STUDY para estimar violência de gênero contra a mulher. Rev Saúde Pública [Internet]. 2010 ago [citado 2019 jul 25];44(4):658-66. Disponível em: https://doi.org/10.1590/S0034-89102010000400009 [ Links ]
18. World Health Organization - WHO. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence [Internet]. Geneva: WHO; 2013 [cited 2020 May 22]. Available from: https://www.who.int/reproductivehealth/publications/violence/9789241564625/en / [ Links ]
19. Silva EP, Valongueiro S, Araújo TVB, Ludermir AB. Incidência e fatores de risco para violência por parceiro íntimo no período pós-parto. Rev Saúde Pública [Internet]. 2015 ago [citado 2019 abr 13];49(5):46-55. Disponível em: https://doi.org/10.1590/S0034-8910.2015049005432 [ Links ]
20. Santos SA, Lovisi GM, Valente CDCB, Legay L, Abelha L. Violência doméstica durante a gestação: um estudo descritivo em uma unidade básica de saúde no Rio de Janeiro. Cad Saúde Coletiva [Internet]. 2010 out-dez [citado 2020 jan 2];18(4):483-93. Disponível em: http://www.cadernos.iesc.ufrj.br/cadernos/images/csc/2010_4/artigos/CSC_v18n4_483-493.pdf [ Links ]
21. Aguiar LC. Violência na gravidez: caracterização de casos em São Luís (MA) no ano de 2010 2014. [dissertação]. São Luís (MA): Universidade Federal do Maranhão; 2014. Disponível em: https://renasf.fiocruz.br/sites/renasf.fiocruz.br/files/disseracoes/2014_UFMA_Lia%20Cardoso%20de%20Aguiar.pdf [ Links ]
22. Sgobero JKGS, Monteschio LVC, Zurita RCM, Oliveira RR, Freitas-Mathias TA. Violência física por parceiro íntimo na gestação: prevalência e alguns fatores associados. Aquichan [Internet]. 2015 set [citado 2020 jul 12];15(3):339-50. Disponível em: https://doi.org/10.5294/aqui.2015.15.3.3 [ Links ]
23. Leite FMC, Luis MA, Amorim MHC, Maciel ELN, Gigante DP. Violência contra a mulher e sua associação com o perfil do parceiro íntimo: estudo com usuárias da atenção primária. Rev Brasil Epidemiol [Internet]. 2019 [citado 2020 maio 3];22: e190056. Disponível em: https://doi.org/10.1590/1980-549720190056 [ Links ]
24. Vieira LB, Cortes LF, Padoin SMM, Souza IEO, Paula CC, Terra MG. Abuso de álcool e drogas e violência contra as mulheres: denúncias de vividos. Rev Bras Enferm [Internet]. 2014 [citado 2020 maio 3];67(3):366-72. Disponível em: http://dx.doi.org/10.5935/0034-7167.20140048 [ Links ]
25. Zilberman ML, Blume SB. Violência doméstica, abuso de álcool e substâncias psicoativas. Rev Bras Psiquiatr [Internet]. 2005 [citado 2020 jun 12];27(supl 2):51-5. Disponível em: https://www.scielo.br/pdf/rbp/v27s2/pt_a04v27s2 [ Links ]
26. Yüksel-Kaptanoğlu İ, Adali T. Intimate partner violence during pregnancy in Turkey: determinants from nationwide surveys. J Interpers Violence [Internet]. 2019 Mar [cited 2020 May 22];1-30. Available from: https://doi.org/10.1177/0886260519837652 [ Links ]
27. Abramsky T, Watts CH, Garcia-Moreno C, Devries K, Kiss L, Ellsberg M, et al. What factors are associated with recent intimate partner violence? Findings from the WHO multi-country study on women’s health and domestic violence. BMC Public Health [Internet]. 2011 Feb [cited 2020 May 5];11(109):1-17. Available from: https://doi.org/10.1186/1471-2458-11-109 [ Links ]
28. Menezes TC, Amorim MMRD, Santos LC, Faúndes A. Violência física doméstica e gestação: resultados de um inquérito no puerpério. Rev Bras Ginecol Obstet [Internet]. 2003 jun [citado 2020 maio 5];25(5):309-16. Disponível em: https://doi.org/10.1590/S0100-72032003000500002 [ Links ]
29. Taillieu TL, Brownridge DA. Violence against pregnant women: prevalence, patterns, risk factors, theories, and directions for future research. Aggress Violent Behav [Internet]. 2010 Feb [cited 2020 Jul 12];15(1):14-35. Available from: https://doi.org/10.1016/j.avb.2009.07.013 [ Links ]
1Article derived from the master’s degree dissertation entitled ‘Intimate partner violence during pregnancy: prevalence and associated factors in Caxias, state of Maranhão’, submitted by Hayla Nunes da Conceição to the Health and Community Postgraduate Program of the Federal University of Piauí in 2020.
Received: September 21, 2020; Accepted: November 18, 2020











 texto en
texto en