Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.2 Brasília 2021 Epub 14-Jun-2021
http://dx.doi.org/10.1590/s1679-49742021000200014
Original Article
Health care in the first year of life of a prospective cohort of late-preterm and full-term infants, in Botucatu, state of São Paulo, Brazil, 2015-20171
1 Universidade Estadual Paulista ‘Júlio de Mesquita Filho’, Faculdade de Medicina de Botucatu, Botucatu, SP, Brazil
Objective:
To assess association between late-preterm birth and use of referral health services in the first year of life.
Methods:
This was a prospective cohort study, with data collected from infants at 1, 3, 6, 9 and 12 months old. Maternal and birth characteristics were compared between full-term and late preterm infants. The effect of late preterm birth on the use of specialized outpatient clinic, emergency room/emergency care center, hospitalizations and intensive care unit (ICU) admissions was evaluated by calculating adjusted odds ratios.
Results:
41 late preterm and 540 full-term infants differed as to frequency of low birth weight and in not staying in joint accommodation, both of which were higher in late-preterm infants, who were also more likely to be admitted to the neonatal ICU (OR=6.85 - 95%CI 2.56;18.34). Late preterm birth was not associated with the use of other referral health services.
Conclusion:
late preterm birth was not associated with greater use of referral health services after discharge from maternity hospital.
Keywords: Health Care; Premature Birth; Term Birth; Infant; Longitudinal Studies
Introduction
Preterm birth has been an important and growing public health problem worldwide. An estimated 15 million children were born before they were 37 weeks of gestational age, in 2018.1 Among various countries, the proportion of preterm births ranges from 5 to 18% of live births, and these differences are due to socioeconomic and demographic conditions, with higher values for the least developed countries.1
The prevalence of preterm birth in Brazil in 2011 and 2012 was 11.5%, with 74% of these preterm infants considered late, i.e., born in the period from 34 to 36 weeks and six days of gestational age.2 The high prevalence of late preterm birth was mainly attributed to the considerable proportions of elective caesarean deliveries, performed before the onset of labor, among women who use private health services for the procedure. Complications associated with teenage pregnancy, low maternal education and insufficient number of prenatal consultations - common facts among women belonging to socially disadvantaged groups - also contributed to the increase in cases of late preterm infants in the country.2
Late preterm infants have higher risk of perinatal and neonatal morbidity and mortality, infant and adult mortality, when compared to full-term infants.3,4 Late preterm infants may require referral health services more frequently for care of their clinical specificities.5
Among the recommended actions for health care of late preterm infants in the first years of life are more assiduous monitoring of growth and development, the individualized nutritional approach and breastfeeding promotion, ferrous sulfate dietary supplement and compliance with the vaccination schedule according to chronological age, based on the National Immunization Schedule.6,7 Three quarters of late preterm infant mortality would be preventable if they received appropriate interventions before and after birth.5
The researchers involved in this study identified only two published Brazilian studies dealing with health care for late preterm infants.8,9 In the face of the incipience of scientific production on the subject in Brazil, this study aimed to assess full-term and late preterm infants and investigate the presence of association between late preterm birth and use of referral health services in the first year of life.
Methods
This was a prospective cohort study, focusing on health care of late preterm infants. It is a subproject originated from the population-based research entitled ‘Child health in the first year of life: prospective cohort study in the interior region of São Paulo’ - which is a cohort of infants in Botucatu (CLaB).10
The CLaB study10 chose this medium-sized municipality in the interior region of the state of São Paulo, Brazil, which had a total of 21 Primary Health Centers in operation, providing primary care services for children, during the follow-up of this cohort study. They were comprised of: two School Based Health Centers, six Primary Health Centers and 12 Family Health Strategy centers, in addition to a municipal health service for neonatal care and screening. The municipality also had 37 private pediatric clinics.
At the time of data collection, the referral health services for pediatric care in Botucatu had a total of: four public specialized outpatient clinics for follow-up of newborns and infants with complex health problems; a private level I emergency care center; a public level II emergency room; two hospitalization units with their respective maternity hospitals, one being public and the other private; and two pediatric intensive care/intermediate care units, one public and the other private. The two maternity hospitals in the city provided joint accommodation, an inpatient unit (nursery) and a neonatal intensive care unit.
The recruitment process of mother-infant pairs to make up the cohort of the CLaB study was carried out in the municipal neonatal care and screening unit, chosen because it is a public service with high population coverage, among newborns in both public and private hospitals. Mandatory neonatal screening tests and the first newborn consultation are performed in this centralized unit; the consultation in the neonatal unit is scheduled when mother and newborn are still in the maternity hospital. This consultation should preferably take place in the first two weeks of the newborn’s life. It was at this place where, from June 29, 2015 to January 11, 2016, from Monday to Friday, trained interviewers assessed the eligibility of infants to participate in the CLaB study and conducted the first interview with their mothers.
The inclusion criteria in the original cohort were: infants born between June 2015 and January 2016, up to 1 month old at the time of recruitment, whose mothers lived in Botucatu, were their main caregiver and who were also capable of answering face-to-face and telephone interview questions. Children who had failed to attend the scheduled consultation at the neonatal care unit or who had attended it after turning 1 month old were not included in the CLaB study. The sample size of this study was defined based on the cohort size of the original study, which involved 656 infants in its baseline. For this study, the same inclusion criteria were adopted as in the original study, excluding infants who had not remained in the cohort study until 12 months of age and moderate or early preterm infants, given that the study aimed to compare late preterm infants and full-term infants.
Demographic, socioeconomic and obstetric variables of mothers and infants at birth were collected, regarding health care received by mothers during prenatal care, at the time of delivery and in the maternity hospital, and by the infants during the first year of life (Figure 1). The categories of these variables were defined based on risk and vulnerability criteria at birth established by the Brazilian Ministry of Health,6,7 according to the clinical recommendations for health care adequacy during prenatal care, childbirth, and for the age group studied.6,7,11
Late prematurity is defined as a ‘gestational age between 34 to 36 weeks and 6 days’, categorized as ‘full-term birth’ or ‘late preterm birth’.
Figure 1 Variables and sources of the data studied, Botucatu, Brazil, 2015-2017
| Variables/measurements | Data Source |
|---|---|
| Demographic, socioeconomic and obstetric characteristics of infants at birth | |
| Gestational age at birth (late preterm; full-term) | Maternity hospital records |
| Maternal age (in years: <20; ≥20) | Recruitment interview |
| Mother with a partner (no; yes) | Recruitment interview |
| Maternal skin race/color (non-white; white) | Recruitment interview |
| Years of maternal schooling (<8; ≥8) | Recruitment interview |
| Maternal work (unpaid; paid) | Recruitment interview |
| Household income per capita (minimum wages: <1; ≥1)a | Recruitment interview |
| Head of family employed (no; yes) | Recruitment interview |
| Mother or father alcohol or drug users (yes; no) | Recruitment interview |
| Well accepted pregnancy (no; yes) | Recruitment interview |
| High-risk pregnancy (yes; no) | Recruitment interview |
| Baby’s sex (male; female) | Recruitment interview |
| First child (yes; no) | Recruitment interview |
| Apgar score at the 5th minute of life (<7; ≥7) | Recruitment interview |
| Birth weight (<2,500g; ≥2,500g) | Maternity hospital records |
| Health care received by mothers during prenatal care, childbirth, and while in maternity hospital and by infants in the first year of life | |
| Prenatal follow-up (public; private) | Recruitment interview |
| Number of prenatal consultations (≥6; <6) | Pregnant women card |
| Prenatal education group (yes; no) | Recruitment interview |
| Childbirth service (public; private) | Recruitment interview |
| Type of childbirth (vaginal; C-section) | Maternity hospital records |
| Joint accommodation in maternity hospital (yes; no) | Maternity hospital records |
| Blood glucose control in maternity hospital (yes; no) | Maternity hospital records |
| Serum bilirubin control in maternity hospital (yes; no) | Maternity hospital records |
| Childcare service (public; private) | Interviews at 3, 6, 9 and 12 months old |
| Use of ferrous sulfate in the 1st year (yes; no) | Interviews at 3, 6, 9 and 12 months old |
| Number of appointments scheduled in the 1st year (≥6; < 6) | Interviews at 3, 6, 9 and 12 months old |
| Complete vaccination schedule in the 1st year (yes; no) | Children’s booklet |
| Monitoring of weight gain in the 1st year (yes; no) | Interviews at 3, 6, 9 and 12 months old |
| Monitoring of neuro psychomotor development in the 1st year (yes; no) | Recruitment interview |
| Use of referral health services | |
| Neonatal intensive care unit (yes; no) | Maternity hospital records |
| Specialized outpatient clinic in the 1st year (yes; no) | Interviews at 3, 6, 9 and 12 months old |
| Emergency room/emergency care center in the 1st year (yes; no) | Interviews at 3, 6, 9 and 12 months old |
| Hospitalization in the 1st year (yes; no) | Interviews at 3, 6, 9 and 12 months old |
| Intensive care unit/intermediate care unit up to 12 months (yes; no) | Interviews at 3, 6, 9 and 12 months old |
Household family income per capita was obtained by the sum of the individual income of each member of the infant’s family divided by the number of family members and expressed in minimum wages. Minimum wage in 2016 was BRL 880.00.
Late prematurity was considered as a dependent variable in the investigation of its association with maternal sociodemographic and obstetric characteristics and prenatal care, while later it was considered as an exposure variable in the investigation of its repercussions on the use of referral health services in the first year of life (Figure 1):
Hospitalization at a neonatal intensive care unit;
Use of specialized outpatient clinic;
Receiving care at an emergency room/emergency care center;
Hospitalization;
Hospitalization at an intensive care unit/intermediate care unit after discharge from maternity hospital and up to 12 months old.
Data were collected from mothers on seven different occasions - before the infant was 30 days old, at 3, 6, 9 and 12 months old - during face-to-face interviews at the recruitment site and at home; and by telephone calls, when the child was 2 and 4 months old. Mothers were asked about their children’s use of health care services on all those occasions. Pregnancy booklets, child health booklets and children’s medical records were used as other sources of data and measurement. (Figure 1).
The data collection instruments, designed by researchers who have experience in epidemiological study projects, were pretested in order for them to reach the version considered satisfactory by the researchers. Data collected in the pre-testing stage of the instruments were not included in the study.
Integrity of interviews was also verified by telephone, taking a random sample of 5% of the participants, when a second interview was conducted by a field supervision officer. The data were input twice to the databases, thus enabling inconsistencies in the questionnaires to be identified and duly eliminated or corrected.
Follow-up losses were minimized by recording other potentially useful phones/addresses, provided by children’s grandparents, mothers’ partners, relatives and friends, among others they suggested. All participating mothers received thank you letters or telephone calls from the researchers for their participation in the study, in addition to reminding them of the date of each new interview. The mothers had the possibility of making a collect call to inform the interviewers about any changes of address and/or scheduling/rescheduling of the interviews according to their convenience.
The differences between infants who remained in the study up to 12 months old and those configured as losses were evaluated by comparing maternal and infant characteristics: maternal age; years of maternal schooling; race/skin color; household income per capita; mother with a partner; birth weight; and Apgar score at 5 minutes after birth. In order to perform this assessment, Pearson’s nonparametric chi-square tests or Fisher’s exact test were used, adopting p<0.05 as critical level.
The cohort was analyzed descriptively, comparing the frequencies of late preterm infants with those of full-term infants, according to maternal socioeconomic and demographic variables and pre and postnatal health care variables, with significance assessed by Pearson’s nonparametric chi-square tests or Fisher’s exact test, considering the critical value of p<0.05.
Bivariate logistic regression analysis was then performed to estimate the crude odds ratio (OR) and respective 95% confidence intervals (95%CI). In this analysis, late prematurity was investigated as a dependent or outcome variable, and maternal demographic, socioeconomic and obstetric characteristics and infant’s birth characteristics as exposure variables.
At a later stage, late prematurity was investigated as a risk factor (explanatory or exposure variable) for the following outcomes: hospitalization at a neonatal intensive care unit; use of specialized outpatient clinic; receiving care at emergency room /emergency care center; hospitalization; and admission to the intensive care unit/intermediate care unit after discharge from the maternity hospital and up to 12 months old.
Crude and multiple logistic regression models were adjusted for each outcome separately, with the ‘full-term infant’ or ‘late preterm infant’ categories as the exposure variable. The selection of covariates that could possibly act as confounders of the associations investigated was performed through bivariate analyses, adopting p<0.20 as a critical level for their inclusion. In the adjusted models, the ‘late preterm infant’ exposure variable and covariates were included simultaneously and kept in the final model. Adjusted OR and respective 95% confidence intervals were calculated, and associations were considered significant if p<0.05.
The multiple logistic regression model was adopted for its adequacy to binary outcomes and with low frequency in the population,12 when there is interest in evaluating the presence of association and measuring the effect of an exposure variable adjusted by many potential confounders.13,14
The Hosmer & Lemeshow test was used to evaluate the fit of the final model. All analyses were performed using the Software Statistical Package for the Social Sciences (SPSS), version 21.
The study project was approved by the Human Research Ethics Committee of Botucatu Medical School (CEP/FMB/UNESP): Opinion No. 1,089,594, issued on October 17, 2013; Certificate of Submission for Ethical Appraisal (CAAE) No. 45017215.8.0000.5411. All infants’ mothers in the cohort we analyzed signed a Free and Informed Consent Form.
Results
At the recruitment site and during the original cohort study period, 923 newborns took part in the selection process, of whom 138 did not meet the inclusion criteria and were considered ineligible; 129 mothers refused to participate in the study (16.4% among eligible newborns), configuring a sample of 656 newborns in the original cohort study. Of these, 50 (7.6%) were born prematurely, with 45 late preterm infants and 5 moderate or early preterm infants. There were losses throughout the cohort study follow-up until the end of the first year of life: 51 (8.4%) full-term infants’ mothers and 3 (6.7%) late preterm infants’ mothers were not located, 16 (2.6%) full-term infants’ mothers refused to continue participating in the study and 1 (2.2%) late preterm infant died. Thus, the cohort analyzed in this study resulted in 581 infants: 540 full-term infants and 41 late preterm infants (Figure 2).
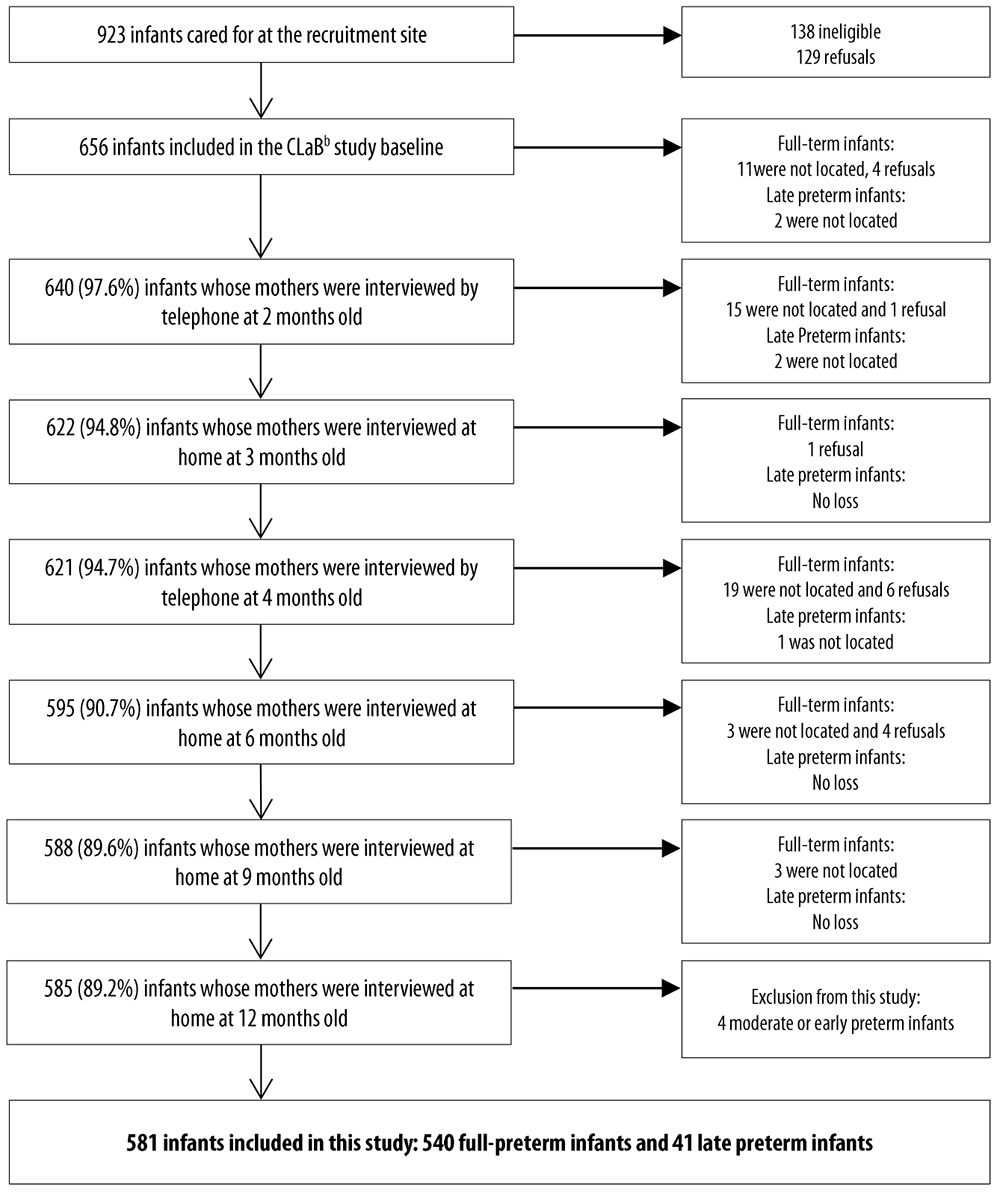
a) Denominator adopted to calculate the percentage of interviews conducted at each stage of data collection; b) CLaB: Botucatu infant cohort.
Figure 2 Cohort formation and follow-up of full-term infants and late preterm infants, Botucatu, Brazil, 2015-2017
Comparing the group of infants who completed the cohort follow-up (up to 12 months old) with the loss group, no significant differences were observed regarding the mothers’ demographic, socioeconomic and obstetric characteristics and the infants’ birth characteristics analyzed, with all p values >0.20; except the ‘mother with a partner’ variable, with p=0.141 (data not shown in table).
Late preterm infants did not differ from full-term infants regarding maternal demographic and socioeconomic characteristics, such as household income and employment situation of the head of the family. There was also no difference in the frequency of those born with Apgar <7 at the 5th minute of life. The main difference to consider was observed in birth weight: 39% of late preterm infants were low weight versus 2.2% of full-term infants (Table 1).
Table 1 Demographic, socioeconomic and obstetric characteristics of mothers and late preterm and full-term infants at birth (n=581), Botucatu, Brazil, 2015-2017
| Variables | Total | Late preterm infants | Full-term infants | ORc (95%ICd) | p-valuea | |||
|---|---|---|---|---|---|---|---|---|
| (n=581) | (n=41) | (n=540) | ||||||
| n | % | n | % | n | % | |||
| Maternal age (in years) | 0.947 | |||||||
| <20 | 83 | 14.3 | 6 | 14.6 | 77 | 14.3 | 1.03 (0.42;2.53) | |
| ≥20 | 498 | 85.7 | 35 | 85.4 | 463 | 85.7 | 1.00 | |
| Mother with a partner | 0.431 | |||||||
| No | 76 | 13.1 | 7 | 17.1 | 69 | 13.0 | 1.41 (0.59;3.29) | |
| Yes | 505 | 86.9 | 34 | 82.9 | 471 | 87.0 | 1.00 | |
| Maternal race/ skin color | 0.594 | |||||||
| Non-white | 221 | 38.0 | 14 | 34.2 | 207 | 38.3 | 0.83 (0.43;1.63) | |
| White | 360 | 62.0 | 27 | 65.8 | 333 | 61.7 | 1.00 | |
| Years of maternal schooling | 0.442b | |||||||
| <8 | 55 | 9.5 | 3 | 7.3 | 52 | 9.6 | 0.74 (0.22;2.48) | |
| ≥8 | 526 | 90.5 | 38 | 92.7 | 488 | 90.4 | 1.00 | |
| Mother’s work | 0.761 | |||||||
| Unpaid | 242 | 41.7 | 18 | 43.9 | 224 | 41.5 | 1.10 (0.58;2.09) | |
| Paid | 339 | 58.3 | 23 | 56.1 | 316 | 58.5 | 1.00 | |
| Household income per capita | 0.092 | |||||||
| <1 minimum wage | 457 | 78.7 | 28 | 68.3 | 429 | 79.4 | 0.56 (0.28;1.11) | |
| ≥1 minimum wage | 124 | 21.3 | 13 | 31.7 | 111 | 20.6 | 1.00 | |
| Head of family employed | 0.606b | |||||||
| No | 19 | 3.3 | 1 | 2.4 | 18 | 3.0 | 0.73 (0.09;5.57) | |
| Yes | 562 | 96.7 | 40 | 97.6 | 522 | 97.0 | 1.00 | |
| Mother or father alcohol or drug user | 0.066 | |||||||
| Yes | 53 | 9.1 | 7 | 17.1 | 46 | 8.5 | 2.21 (0.93;5.27) | |
| No | 528 | 90.9 | 34 | 82.9 | 494 | 91.5 | 1.00 | |
| Well accepted pregnancy | 0.411b | |||||||
| No | 46 | 7.9 | 4 | 9.7 | 42 | 7.8 | 1.28 (0.44;3.77) | |
| Yes | 535 | 92.1 | 37 | 90.3 | 498 | 92.2 | 1.00 | |
| High-risk pregnancy | 0.418 | |||||||
| Yes | 63 | 10.8 | 6 | 14.6 | 57 | 10.5 | 1.45 (0.57;3.60) | |
| No | 518 | 89.2 | 35 | 85.5 | 483 | 89.5 | 1.00 | |
| First child | 0.952 | |||||||
| Yes | 295 | 50.8 | 21 | 51.0 | 274 | 50.7 | 1.02(0.54;1.92) | |
| No | 286 | 49.2 | 20 | 49.0 | 266 | 49.3 | 1.00 | |
| Baby’s sex | 0.946 | |||||||
| Male | 323 | 55.6 | 23 | 56.0 | 300 | 55.6 | 1.02 (0.54;1.94) | |
| Female | 258 | 44.4 | 18 | 44.0 | 240 | 44.4 | 1.00 | |
| Apgar score at 5 minutes | 0.307b | |||||||
| <7 | 5 | 0.9 | 1 | 2.5 | 4 | 0.7 | 3.35 (0.37;30.68) | |
| ≥7 | 576 | 99.1 | 40 | 97.5 | 536 | 99.3 | 1.00 | |
| Birth weight | <0.001 | |||||||
| <2,500g | 28 | 4.8 | 16 | 39.0 | 12 | 2.2 | 28.16 (12.04;65.83) | |
| ≥2,500g | 553 | 95.2 | 25 | 61.0 | 528 | 97.8 | 1.00 | |
a) Pearson’s chi-square test; b) Fisher’s exact test; c) OR: odds ratio, obtained by bivariate logistic regression; d) 95%CI: 95% confidence interval.
The proportion of late preterm infants’ mothers who got prenatal follow-up in public services (OR=0.48 - 95% CI 0.26;0.92) and with 6 or more prenatal consultations (OR=0.17 - 95%CI 0.08;0.34) was lower. Regarding the type of delivery, 65.9% of late preterm infants were born by cesarean section versus 50.9% of full-term infants, a difference that did not reach the statistical significance stipulated (Table 2).
Table 2 Health care received by late preterm infants’ and full-term infants’ mothers during prenatal care, childbirth and while in the maternity hospital and health care received by infants from birth to 12 months old (n=581), Botucatu, Brazil, 2015-2017
| Variables | Total | Late preterm infants | Full-term infants | ORc (95%ICd) | p-valuea | |||
|---|---|---|---|---|---|---|---|---|
| (n=581) | (n=41) | (n=540) | ||||||
| n | % | n | % | n | % | |||
| Prenatal follow-up | 0.023 | |||||||
| Private | 202 | 34.8 | 20 | 48.8 | 182 | 33.7 | 0.48 (0.26;0.92) | |
| Public | 379 | 65.2 | 21 | 51.2 | 358 | 66.3 | 1.00 | |
| Number of prenatal consultationse | <0.001 | |||||||
| <6 | 42 | 8.3 | 9 | 24.3 | 33 | 7.0 | 4.27 (1.86;9.79) | |
| ≥6 | 466 | 91.7 | 28 | 75.7 | 438 | 93.0 | 1.00 | |
| Educational group during prenatal | 0.438b | |||||||
| No | 555 | 95.5 | 40 | 97.6 | 515 | 95.4 | 1.94 (0.26;14.70) | |
| Yes | 26 | 4.5 | 1 | 2.4 | 25 | 4.6 | 1.00 | |
| Childbirth service | 0.118 | |||||||
| Private | 191 | 32.9 | 18 | 43.9 | 173 | 32.0 | 0.60 (0.32;1.15) | |
| Public | 390 | 67.1 | 23 | 56.1 | 367 | 68.0 | 1.00 | |
| Type of childbirth | 0.065 | |||||||
| Caesarean Section | 302 | 52.0 | 27 | 65.9 | 275 | 50.9 | 1.86 (0.95;3.62) | |
| Vaginal delivery | 279 | 48.0 | 14 | 34.1 | 265 | 49.1 | 1.00 | |
| Joint accommodation in the maternity hospital | <0.001 | |||||||
| No | 57 | 9.8 | 14 | 34.2 | 43 | 8.0 | 5.99 (0.29;12.27) | |
| Yes | 524 | 90.2 | 27 | 65.8 | 497 | 92.0 | 1.00 | |
| Blood glucose control in the maternity hospital | <0.001 | |||||||
| No | 391 | 67.3 | 10 | 24.4 | 381 | 70.6 | 0.14 (0.06;0.28) | |
| Yes | 190 | 32.7 | 31 | 75.6 | 159 | 29.4 | 1.00 | |
| Serum bilirubin control in the maternity hospital | 0.844 | |||||||
| No | 178 | 30.6 | 12 | 29.3 | 166 | 30.7 | 0.93 (0.46;1.87) | |
| Yes | 403 | 694 | 29 | 70.5 | 374 | 69.3 | 1.00 | |
| Childcare service | 0.148 | |||||||
| Private | 156 | 26.9 | 15 | 36.6 | 141 | 26.1 | 0.61 (0.32;1.19) | |
| Public | 425 | 73.1 | 26 | 63.4 | 399 | 73.9 | 1.00 | |
| Number of consultations scheduled in the first year | 0.887 | |||||||
| <6 | 306 | 52.6 | 22 | 53.7 | 284 | 52.6 | 1.05 (0.55;1.98) | |
| ≥6 | 275 | 47.4 | 19 | 46.3 | 256 | 47.4 | 1.00 | |
| Blood glucose control in the first yeare | 0.983 | |||||||
| No | 389 | 67.7 | 27 | 67.5 | 362 | 67.7 | 1.01 (0.51;2.00) | |
| Yes | 186 | 32.3 | 13 | 32.5 | 173 | 32.3 | 0.10 | |
| Weight gain follow-up in the first year | 0.770 | |||||||
| No | 131 | 22.5 | 10 | 24.4 | 121 | 22.4 | 1.18 (0.53;12.34) | |
| Yes | 450 | 77.5 | 31 | 75.6 | 419 | 77.6 | 1.00 | |
| Monitoring of neuropsychomotor development in the first year | 0.635 | |||||||
| No | 193 | 33.2 | 15 | 36.6 | 178 | 33.0 | 1.17 (0.61;2.27) | |
| Yes | 388 | 66.8 | 26 | 63.4 | 362 | 67.0 | 1.00 | |
| Complete scheduling vaccination in the first year | 0.877 | |||||||
| No | 122 | 21.0 | 9 | 21.0 | 113 | 20.9 | 0.06 (0.49;2.29) | |
| Yes | 459 | 79.0 | 32 | 79.0 | 427 | 79.1 | 1.00 | |
| Ferrous sulfate use in the first year | 0.207b | |||||||
| No | 569 | 97.9 | 39 | 95.1 | 530 | 98.2 | 0.37 (0.08;1.74) | |
| Yes | 12 | 2.1 | 2 | 4.9 | 10 | 1.8 | 1.00 | |
a) Pearson’s chi-square test; b) Fisher’s exact test; c) OR: odds ratio obtained by bivariate logistic regression; d) 95%CI: 95% confidence interval.
Late preterm infants were less likely to stay in joint accommodation in the maternity hospital (OR=5.99 - 95% CI 0.29;12,27). For these infants, blood glucose control in the maternity hospital (75% versus 29%) and prescription of ferrous sulfate after discharge from the maternity hospital (4.9% versus 1.8%) were the most frequent health actions after birth, with statistical significance only for blood glucose control in the maternity hospital (Table 2).
According to the bivariate analysis, late preterm infants were more likely to be admitted to a neonatal intensive care unit (OR=4.62 - 95% CI 2.03;10.52) and were less likely to receive care in an emergency room/emergency care center (OR=0.50 - 95%CI 0.26;0.97), when compared to full-term infants. Despite the difference between late preterm infants and full-term infants regarding the frequency of hospitalization at an intensive care/intermediate care unit in the first year of life, this association did not reach statistical significance in the crude analysis (OR=6.76 - 95%CI 0.60;75.77). No associations were observed between preterm birth and use of specialized outpatient clinics, hospitalization or admission to an intensive care unit/intermediate care unit in the first year of life (Table 3).
Table 3 Odds ratio of use of referral health services according to late preterm birth (n=581), Botucatu, Brazil, 2015-2017
| Variáveis | Late preterm infants | Full-term infants | ORa (95%ICb) | p-valuec | ORa (95%ICb) | p-valuec | ||
|---|---|---|---|---|---|---|---|---|
| (n=41) | (n=540) | |||||||
| n | %d | n | %d | |||||
| Neonatal intensive care unit | <0.001 | <0.001 | <0,001 | |||||
| Yes | 9 | 22.0 | 31 | 5.7 | 4.62 (2.03;10.52) | 6.85e (2.56;18.34) | ||
| No | 32 | 78.0 | 509 | 94.3 | 1.00 | 1.00 | ||
| Specialized outpatient clinic in the first year | 0.948 | |||||||
| Yes | 5 | 12.2 | 64 | 11.8 | 1.03 (0.39;2.73) | |||
| No | 36 | 12.2 | 476 | 88.2 | 1.00 | |||
| Emergency room/ Emergency care center in the first year | 0.039 | 0,445 | ||||||
| Yes | 24 | 58.5 | 398 | 73.7 | 0.50 (0.26;0.97) | 0.73f (0.33;1.62) | ||
| No | 17 | 41.5 | 142 | 26.3 | 1.00 | 1.00 | ||
| Hospitalization in the first year | 0.519 | |||||||
| Yes | 6 | 14.6 | 58 | 10.7 | 14.3 (0.48;4.22) | |||
| No | 35 | 85.4 | 482 | 89.3 | 1.00 | |||
| Intensive care unit/intermediate care unit in the first year | 0.123 | 0,109 | ||||||
| Yes | 1 | 2.4 | 2 | 0.4 | 6.76 (0.60;75.77) | 9.00g (0.61;131.91) | ||
| No | 40 | 97.6 | 538 | 99.6 | 1.00 | 1.00 | ||
a) OR: odds ratio obtained by bivariate logistic regression; b) 95%CI: 95% confidence interval; c) Wald Test; d) The percentages were presented in the columns to facilitate the visualization of differences in the occurrence of outcomes in exposed and unexposed infants; e) OR adjusted for household income per capita, mother/father alcohol/drug user, prenatal follow-up, number of prenatal visits, childbirth service and type of childbirth; f) OR adjusted for household income per capita, mother/father alcohol/drug user, prenatal follow-up, number of prenatal visits, childbirth service, type of childbirth, stay in joint accommodation, blood glucose control in the maternity ward, childcare service and weight gain follow-up in the 1st year; g) OR adjusted for household income per capita, mother/father alcohol/drug user, prenatal follow-up, childbirth service and type of childbirth.
The adjusted analyses confirmed that late preterm infants were more likely to be admitted to a neonatal intensive care unit (OR=6.85 - 95% CI 2.56;18.34), regardless of household income per capita, parents being alcohol/drug users, the use of public or private services for prenatal check-up, number of prenatal visits and type of childbirth (Table 3). The fit of the model was considered adequate (p=0.471).
The association between late preterm birth and emergency room/emergency care center lost significance (OR=0.73 - 95% CI 0.33;1.62), after adjustments. The absence of association between late preterm birth and admission to an intensive care unit/intermediate care unit after discharge from the maternity hospital and up to 12 months old was confirmed by the adjusted analysis (OR=9.00 - 95%CI 0.61;131.91) (Table 3).
Discussion
Late preterm birth significantly increased the chances of admission to a neonatal intensive care unit - but not the chances of using referral health services after discharge from the maternity hospital. It is possible that the finding is due to the lack of statistical power of the study to identify associations with low frequency outcomes in the population and also to the original cohort characteristics. As one of the inclusion criteria was the infant being less than 30 days old, the cohort may have excluded newborns with health problems that implied prolonged hospitalization in the maternity hospital, which could cause a limitation for this study: the results are valid for late preterm infants who were discharged from the maternity hospital before turning one month old. Other limitations to be considered are: gestational age at birth, obtained from the medical records in the maternity hospitals where the infants were born, with possible differences in the methods of their determination; lack of information on the availability of support networks or other social resources that could influence the outcomes studied; and 12.6% missing information on the number of prenatal consultations.
The methodological design of the study, a prospective cohort, allowed us to obtain and analyze the variables of interest throughout the first year of life of late preterm infants and full-term infants, reducing the risk of information bias. Low percentage of loss to follow-up, completeness of information, and the absence of differences between the characteristics of the infants who completed the follow-up and the remainder, also reinforce the validity of the research.
The situation of health care during prenatal care and in maternity hospital was more negative for late preterm infants, compared to full-term infants, except for blood glucose control in the maternity hospital, an especially recommended action.7 Among late preterm infants, there was a lower demand for prenatal consultations by mothers, and a shorter stay in joint accommodation. These differences were statistically significant. However, both groups presented unsatisfactory results regarding the recommendation for mothers’ participation in educational groups during the prenatal period.15
The number of individual prenatal consultations recommended by the Ministry of Health, despite late preterm infants’ mothers having them less frequently, compared to full-term infants’ mothers, was an expected result, given that the former had had less time to meet this recommendation.11,16 The prenatal period is a period of time for physical and psychological preparation for childbirth and motherhood and, as such, a moment of fruitful and intense learning, both for pregnant women and for health professionals. For the latter, prenatal follow-up is an opportunity for being completely aware of the pregnancy process and for providing health education as a dimension of the care process. For pregnant woman, prenatal follow-up provides the possibility not only of receiving physical and educational care, but also for getting to know the whole action plan for the healthy birth of their child, asking questions and expressing their opinions,10 in addition to reducing and even dissipating anxiety and fear related to pregnancy and the postpartum period.15,17,18 Thus, frequency of individual prenatal consultations and participation in educational groups are fundamental to ensure the quality of prenatal care. Absences and omissions in both these aspects of prenatal health care have revealed, in other studies, risk factors for preterm birth.17,18
The greater chance of late preterm infants being born with low birth weight confirms the biological vulnerability inherent to them, such as developing neonatal complications, as well as not being able to stay together with their mothers in the same room, given their need for differentiated care in the maternity hospital.2,4 These adverse conditions contribute to the association detected between late preterm birth and admission to a neonatal intensive care unit, and the high magnitude of its effect, despite the wide confidence interval. In line with this result, a study conducted in Turkey, when comparing hospitalizations of 605 late preterm infants and 1,477 full-term infants at a neonatal intensive care unit in a large perinatal center, found a three-fold higher frequency of hospitalizations in late preterm infants.19
The absence of association between late preterm birth and outcomes related to the use of referral health services after discharge from the maternity hospital and up to the first 12 months contradicts the literature. A study in the United States identified, in late preterm infants, an increased risk of health complications, either during the period in the maternity hospital, or after discharge from the hospital, with increased hospitalizations and more health expenditure in the first year of life.20 The North American study had a sample of approximately 20 million infants, one quarter of them were late preterm infants while the others were full-term infants. The sample size of that study explains the statistically significant differences found, even though the proportions were close, for example, 14.2% of late preterm infants versus 11.8% of full-term infants hospitalized at least once after discharge from the maternity hospital.20 The frequency of hospitalizations in this cohort study, in Botucatu, was similar: 14.6% of late preterm infants versus 10.7% of full-term infants.
A systematic review, including 52 articles published between 1998 and 2016, on the use of health services by late preterm and full-term infants, from discharge from maternity ward to adulthood, concluded that late preterm infants are at higher risk of all-cause hospitalizations, during the neonatal period and beyond, until adolescence, in addition to the risk of greater frequency of use of other types of health services.5 The results of 4 studies, specifically on hospitalization after discharge from maternity hospital and up to 1 year old, were analyzed together: 2 studies conducted in the United States, 1 in Brazil and another in Australia. The frequencies of hospitalizations were 2 to 4 percentage points higher in late preterm infants, according to the results of both the North American and the Brazilian studies, similar to the frequencies found in Botucatu; only in the Australian study, the percentage difference was 9 points for late preterm infants.5
In addition to the small sample size of this study, a hypothesis for the absence of association between late preterm birth and use of referral health services in the first year of life would be better quality of services provided by Brazilian National Health System Primary Health Care services, given the differentiated care required for late preterm infants. However, this hypothesis does not find support in the results, when it is known that late preterm infants were not benefitted by important actions, such as monitoring child growth and development.6,7 A second hypothesis would be the fact that the late preterm infants studied and their families had support networks and/or social resources that protected them from postnatal health problems resulting from preterm birth.6,21 This possibility cannot be explored, however, as this data did not form part of the study.
In summary, this study identified characteristics and repercussions of late preterm birth, showing differences in view of full-term birth, with the potential to serve as a support for health care qualification in the face of this condition, in the context studied and in other similar ones. Late preterm infants differed from full-term infants by presenting higher frequency of low birth weight and lower frequency of prenatal care in public health services, compliance with the minimum recommended number of prenatal consultations and staying in joint accommodation at the maternity hospital, with a higher chance of hospitalization in a neonatal intensive care unit. After discharge from the maternity hospital and until they were 12 months old,
there was no difference in the use of referral health services by late preterm infants and full-term infants, a result contrary to what was expected after consulting the literature. The low statistical power of the sample and the possibility that the cohort study did not included newborns who had remained in prolonged hospitalization after birth may have contributed to these results.
Future studies with larger samples, including all late preterm infants, even those who remain hospitalized in the maternity hospital for a long period, are recommended, aiming to deepen knowledge about the effects of this health problem on the use of health services throughout the first year of life.
REFERENCES
1. World Health Organization. Pretern birth [Internet]. Geneva: WHO;2018 [citado 25 abr. 2020]. Disponível em: Disponível em: http://www.who.int/news-room/fact-sheets/detail/preterm-birth [ Links ]
2. Leal MC, Esteves-Pereira AP, Nakamura-Pereira M, Torres JÁ, Theme-Filha M, Domingues RMSM, et al. Prevalence and risk factors related to preterm birth in Brazil. Reprod Health. 2016;13(Suppl 3):127. doi: http://doi.org/10.1186/s12978-016-0230-0. [ Links ]
3. Machado-Júnior LC, Passini-Júnior R, Rosa IRM. Late prematurity: a systematic review. J Pediatr (Rio J). 2014;90(3):221-31. doi: http://doi.org/10.1016/j.jped.2013.08.012. [ Links ]
4. Morgan JC, Boyle EM. The late preterm infant. Paediatr Child Health. 2017;28(1):13-7. doi: https://doi.org/10.1016/j.paed.2017.10.003. [ Links ]
5. Isayama T, Lewis-Mikhael AM, O’Reilly D, Beyene J, McDonald SD. Health services use by late preterm and term infants from infancy to adulthood: a meta-analysis. Pediatrics. 2017;140(1):e20170266. doi: http://doi.org/10.1542/peds.2017-0266. [ Links ]
6. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Política nacional de atenção integral à saúde da criança: orientações para implementação. Brasília, DF: MS; 2018. [ Links ]
7. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas e Estratégicas. Atenção à saúde do recém-nascido: guia para os profissionais de saúde: cuidado como recém-nascido pré-termo. Brasília, DF: MS : 2011. [ Links ]
8. Santos IS, Matijasevich A, Silveira MF, Sclowitz IK, Barros AJ, Victora CG, et al. Associated factors and consequences of late preterm births: results from the 2004 Pelotas birth cohort. Paediatr Perinat Epidemiol. 2008;22(4):350-9. doi: https://doi.org/10.1111/j.1365-3016.2008.00934.x. [ Links ]
9. Leal MC, Esteves-Pereira AP, Nakamura-Pereira M, Torres JA, Domingues RMSM, Dias MAB, et al. Provider-initiated late preterm births in Brazil: differences between public and private health services. PLoS One. 2016;11(5):e0155511. doi: http://doi.org/10.1371/journal.pone.0155511. [ Links ]
10. Alves MS, Almeida MAM, Gomes CB, Ferrari AP, Parada CMGL, Carvalhaes MABL. Longer duration of exclusive breastfeeding reduces maternal weight retention: results from the CLaB study. Rev Bras Saude Matern Infant. 2020;20(1):273-84. doi: https://doi.org/10.1590/1806-93042020000100015. [ Links ]
11. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Atenção ao pré-natal de baixo risco. Brasília, DF: MS ; 2013. [ Links ]
12. Hirakata VN. Estudos transversais e longitudinais com desfechos binários: qual a melhor medida de efeito a ser utilizada? Clin Biomed Res. [Internet]. 2009 [citado 3 nov. 2020];29(2). Disponível em: Disponível em: https://seer.ufrgs.br/hcpa/article/view/9737 . [ Links ]
13. Karim F, Ali NB, Khan ANS, Hassan A, Hasan MM, Hoque DME, et al. Prevalence and factors associated with caesarean section in four Hard-to-Reach areas of Bangladesh: findings from a cross-sectional survey. PLoS One . 2020 Jun 9;15(6):e0234249. doi: https://doi.org/10.1371/journal.pone.0234249. eCollection 2020. [ Links ]
14. den Haan PJ, de Kroon MLA, van Dokkum NH, Kerstjens JM, Reijneveld SA, Bos AF. Risk factors for emotional and behavioral problems in moderately late preterms. PLoS One . 2019 May 2;14(5): e0216468. https://doi.org/10.1371/journal.pone.0216468.eCollection2019. [ Links ]
15. Henriques AHB, Gigliola MBL, Trigueiro JVS, Saraiva AM, Pontes MGAP, Cavalcanti JRD, et al. Grupo de gestantes: contribuições e potencialidades na complementaridade da assistência pré-natal. Rev Bras Promoc Saude. 2015;28(1):23-31. doi: http://doi.org/10.5020/18061230.2015.p23. [ Links ]
16. Feitosa PAM, Ávila AD, Isabela C, Correa CEH, Silva BP, Ramos AMM. Características maternas em gestações com risco de prematuridade tardia. Rev Bras Saude Matern Infant . 2013;13(2):161-6. doi: http://doi.org/10.1590/S1519-38292013000200009. [ Links ]
17. Leal MC, Esteves-Pereira AP, Viellas EF, Domingues RMSM, Gama SGN. Prenatal care in the Brazilian public health services. Rev Saude Publica. 2020;54:8. doi: https://doi.org/10.11606/s1518-8787.2020054001458. [ Links ]
18. Melo EC, Oliveira RR, Mathias TAF. Factors associated with the quality of prenatal care: an approach to premature birth. Rev Esc Enferm USP. 2015;49(4):0540-49. doi: http://dx.doi.org/10.1590/S0080-623420150000400002. [ Links ]
19. Celik IH, Demirel G, Canpolat FE, Dilmen U. A common problem for neonatal intensive care units: late preterm infants, a prospective study with term controls in a large perinatal center. J Matern Fetal Neonatal Med. 2013;26(5):459-62. doi: https://doi.org/10.3109/14767058.2012.735994. [ Links ]
20. Bird TM, Bronstein JM, Hall RW, Lowery CL, Nugent R, Mays GP. Late preterm infants: birth outcomes and health care utilization in the first year. Pediatrics . 2010; 126(2):e311-9. doi: https://doi.org/10.1542/peds.2009-2869. [ Links ]
21. Custódio ZAO, Crepaldi MA, Linhares MBM. Redes sociais de apoio no contexto da prematuridade: perspectiva do modelo bioecológico do desenvolvimento humano. Estud Psicol (Campinas). 2014;31(2):247-55. doi: http://doi.org/10.1590/0103-166X2014000200010. [ Links ]
1Article derived from the doctoral thesis entitled ‘Health care of a cohort of late-preterm infants in the first year of life’, submitted by Maria Cristina Heinzle da Silva Machado to the Postgraduate Program in Nursing of the Botucatu School of Medicine, ‘Júlio de Mesquita Filho’ Paulista State University (UNESP), in 2018. The study received financial support from the São Paulo State Research Support Foundation (FAPESP: Process No. 2015/03256-1); and from the Coordination for the Improvement of Higher Education Personnel/Ministry of Education (CAPES/MEC), through granting a doctorate social demand scholarship to Anna Paula Ferrari.
Received: September 04, 2020; Accepted: December 04, 2020











 texto en
texto en 


