Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.2 Brasília 2021 Epub 21-Abr-2021
http://dx.doi.org/10.1590/s1679-49742021000200020
Research note
Frequency and factors associated with recording deaths due to unspecified external causes in Brazil: a cross-sectional study, 2017
1Universidade de Brasília, Faculdade de Ciências da Saúde, Brasília, DF, Brazil.
Objective
To analyze the frequency and factors associated with recording deaths due to unspecified external causes in Brazil.
Methods
This was a cross-sectional study of Mortality Information System data for the year 2017. Univariate logistic regression was used to obtain odds ratios (OR) and 95% confidence intervals (95%CI) of nonspecific recording according to the explanatory variables - (hospital deaths and deaths certified by coroners).
Results
Brazil registered 159,720 deaths from external causes; 38.9% occurred in hospital, 83.4% were certified by coroners and 21.7% were from unspecified causes. Factors associated with the recording of unspecified external causes were hospital death (OR=2.00 - 95%CI 1.96;2.05) and the coroner’s certification (OR=1.08 - 95%CI 1.04;1.11).
Conclusion
The frequency of recording unspecified external causes is greater for hospital deaths than for coroner’s certification.
Keywords: Forensic Medicine; Cause of Death; External Causes; Data Accuracy; Information Systems; Cross-Sectional Studies
Introduction
Reliable cause-of-death statistics provide valid evidence for informing policy development.1 External causes represented a higher percentage of deaths in Brazil (12.3%), compared to other countries in the Americas (9.5%), Asia (8.5%), Africa (7.5%) and Europe (5.6%) in 2017.2
Death certificates often do not specify the circumstance of death due to external causes and are therefore of little use to Public Health.3,4 This type of unspecific recording, known as garbage codes, is a quality indicator of the underlying cause of death.1 Low accuracy in recording causes of death forces health sectors to spend resources on field investigations. In 2016, after checking and retrieving information, 15% of the 160,000 deaths from external causes remained without a specific record in Brazil.5
Brazilian regulatory standards make it mandatory for forensic medicine services to provide a death certificate for unnatural deaths.6 In locations without this service, the death certificate must be issued by a physician. In Brazil, the medico-legal death investigation system combines medical and scientific investigation with police investigation in an open coroner’s court, known as the legal medicine system.7 Although this system does not determine civil or criminal liability, its objective is to establish facts that will be used as the basis for defining the legal cause of death.8
The Institutes of Forensic Medicine are part of the Brazilian National Public Security System.9 The authority of the medico-legal death investigation system is therefore recognized within law enforcement. Municipal Health Authorities are, however, responsible for performing the local procedures necessary for inputting records on the Ministry of Health Mortality Information System (SIM), which are then shared with the National Health Authority for the compilation of death statistics.6
In addition to seeking, in the normative structure of the medico-legal death investigation system, elements for understanding why less accurate information is produced, the objective of this research was to analyze the frequency and factors associated with recording of deaths due to unspecified external causes in Brazil.
Methods
This was a cross-sectional study using secondary data from the SIM database.
Deaths with original underlying cause - a cause prior to investigation by the death surveillance service - are considered to be external causes, i.e. those provided for in codes V01 to Y98 of the 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10). Certification of this type of cause is assigned to a coroner or another person to whom this role has been given by a judicial or police authority.6
External causes were the outcome variable of this study, subgrouped into unspecified and defined causes. In this study, unspecified causes corresponded to records containing unspecified circumstances of death on death certificates, according to the Global Burden of Disease (GBD) Study list, 2015.5,10
Based on the literature,3,5,11,12 two explanatory variables were created from fields contained on the death certificate, and they were organized into binary categories:
Place of occurrence of death - hospital (hospital; health centers); and non-hospital (residence; public highway; other);
Certifying physician - record certified by a forensic institute (coroner); and not certified by a forensic institute (treating physician; substitute doctor; death verification service; other).
Initially, the outcome variables and explanatory variables were represented in a flow diagram of the frequency of unspecified records; existence of a possible multicollinearity was tested by linear regression, using tolerance and variance inflation factors (VIF). Finally, univariate binary logistic regression was applied to test how much the unspecified external cause was modified by the occurrence of hospital deaths and then by the record certified by a forensic institute. The measurement of this change was obtained by odds ratios (OR), their respective 95% confidence intervals (95% CI) and p-value <0.05. R software (version 4.0.2) was used for all the analyses.
This study was based on non-nominal secondary data in accordance with National Health Council Resolution No. 466, dated December 12, 2012, which standardizes research involving human beings.
Results
In 2017, Brazil recorded 159,720 deaths from external causes, of which 38.9% were in hospitals, 83.4% were certified by forensic medicine and 21.7% were attributed to unspecified causes. Coroner’s certification 74.9% of hospital deaths and 93.0% of events in residences/public highways (Figure 1).
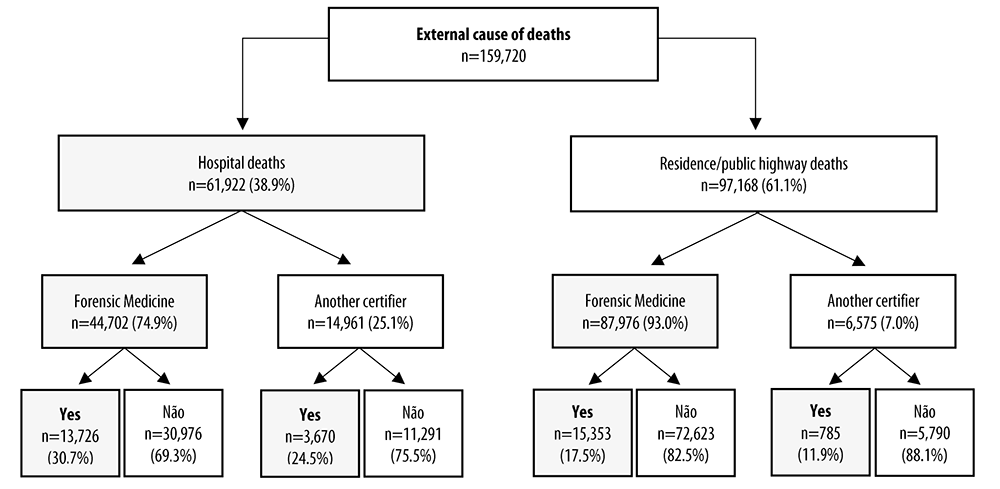
Source: Mortality Information System, Ministry of Health.
Note: Unreported data were excluded: 0.4% (n=630) of occurrences at the place of death; and 3.1% (n=4,898) by coroners.
Figure 1 Schematic representation of the frequency of recording deaths due to unspecified external causes, according to place of occurrence and coroner, Brazil, 2017
Occurrence of hospital deaths (n=61,922) certified by coroners (n=44,702) presented 30.7% (13,726) nonspecific codes, while those issued by other death verification services had 24.5% nonspecific codes (n=3,670). In turn, occurrence of home/public highway deaths (n=87,976) certified by coroners had 17.5% (n=15,353) unspecified causes, and those issued by other death verification services had 11.9% (n=785) unspecified causes (Figure 1).
The odds ratio (OR) for hospital deaths being recorded with a nonspecific code was 2.00 (95%CI 1.96;2.05), compared to those that occurred at home/public highway, with an effect similar on the interaction of independent variables. However, when the independent variable was only death certified by a coroner, the odds ratio was lower: OR=1.08 - 95%CI 1.04;1.11 (Table 1). The independent variables did not present multilinearity: tolerance >0.7 and VIF <1.5.
Table 1 Frequency of mortality from unspecified external causes, odds ratio (OR) and respective 95% confidence intervals, according to place of occurrence and coroner, Brazil, 2017
| Variables | Total (n) | Unspecified | Odds ratio | 95% confidence intervals | p-valuea | |
|---|---|---|---|---|---|---|
| (n) | (%) | |||||
| Place of occurence | ||||||
| Residence/public highway | 97,168 | 16,518 | 17.0 | 1.00 | - | - |
| Hospital deaths | 61,922 | 18,022 | 29.1 | 2.00 | 1.96; 2.05 | <0.001 |
| Certifying physician | ||||||
| Another certifying physician | 21,573 | 4,460 | 20.7 | 1.00 | - | - |
| Coroner | 133,249 | 29,173 | 21.9 | 1.08 | 1.04; 1.11 | <0.001 |
| Interaction | ||||||
| Residence/public highway and coroner | 87,976 | 15,353 | 17.5 | 1.00 | - | - |
| Hospital death and coroner | 44,702 | 13,726 | 30.7 | 2.01 | 1.96; 2.06 | <0.001 |
a) p-value of the odds ratio, calculated by the Wald test.
Discussion
Deaths occurring in hospitals and certified by forensic institutes were associated with recording of death due to unspecified external causes. This type of garbage coding was, however, more likely to be modified by the hospital event and by its interaction with the record issued by coroners.
Previous findings indicated deaths occurring in hospitals and records certified by coroners as being predictors of unspecified recording. Hospital deaths were associated with unspecified causes,11,12 while records issued by coroners, while strongly associated with ill-defined causes, proved to be a protective factor for unspecified causes.11
The occurrence of garbage codes in records issued by forensic medicine may involve different reasons related to the filling in of the death certificate. Sometimes certain data are not properly used or they are available only after the death certificate is issued.3 There are other situations, however, in which the coroner does not make the most of the information available, which may be disregarded because they do not have police reports as a source, for example.13
The correct recording of the external cause of death depends on the results of police investigations and examinations, which are not always performed or completed, and which are affected by poor quality investigations at crime scenes.8 This technical-legal nature of diagnosis of cause of death in the medico-legal death investigation system, under police operational management, produces information that depends on validation procedures standardized by Public Security and Justice agencies.8,9
In the medico-legal death investigation system, it is not the coroner’s prerogative to determine the legal cause of death from unnatural causes, but to contribute to its clarification. This is based on the fact that the physician does not have legal competence to certify definite cause of death, even when the probability of the event being attributed to a certain circumstance of external cause is high.8 Thus, it is not uncommon for the coroner to be led to use a garbage death code, to avoid probable inaccuracies in his professional work.5,13,14 As a result, it is possible that information from hospital records is not used when it is not confirmed by police reports.5,13 In deaths from natural causes, differently, the entire sequence of events is the sole responsibility of the physician, and it is acceptable to certify a highly probable cause based on the clinical history of the individual. In these cases, for the health sector, the epidemiological outcome of the event prevails.1,4,15
Although the legal structure of medico-legal death investigation systems varies widely worldwide, experiences in Brazil and other countries exemplify possible ways to deal with the issues and challenges of recording deaths from external causes, briefly discussed in this article as preliminary notes of an ongoing investigation.13,16,17 In certain countries, the death certificate is a two-part form, with (i) a section for personal information for use at registry offices and burial and (ii) another section for recording the cause of death. This document format allows the coroner to consider results of examinations and criminal reports a posteriori.18
Although the findings help to envisage how hospital deaths due to external causes can increase the recording of unspecified causes certified by coroners in Brazil, this article points to ways for building a classic association model, adjusting potential confounding variables, such as a complete model with greater predictive capacity. Furthermore, qualitative research is needed, together with the collection of epidemiological data, to achieve a more accurate understanding of the phenomenon.
The possibility of predicting unspecified external causes, based on the variables ‘hospital death’ and ‘certified by a coroner’, can support actions to improve the recording of violent causes of death on the SIM database. As medical-legal research information is shared by different social spheres, the promotion of an interinstitutional justice-health dialogue, based on evidence, may mean a further incentive for building intersections between national policies to improve the quality of records and the meaning of deaths due to external causes, in addition to supporting the identification of collaborative best practices of forensic medicine with health surveillance services.
Referências
1. Mikkelson L, Richards N, Lopez AD. Redefining 'garbage codes' for public health policy: report on the expert group meeting, 27-28 February 2017 [Internet]. Melbourne, Australia: Bloomberg Philanthropies Data for Health Initiative, Civil Registration and Vital Statistics Improvement, University of Melbourne; 2018 [cited 2020 Jun 15]. Available from: https://crvsgateway.info/file/14581/276 [ Links ]
2. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet [Internet]. 2018 Nov [cited 2020 Jun 15];392(10159):1736-88. Available from: https://doi.org/10.1016/S0140-6736(18)32203-7 [ Links ]
3. Soares Filho AM, Cortez-Escalante JJ, França E. Review of deaths correction methods and quality dimensions of the underlying cause for accidents and violence in Brazil. Ciênc Saúde Coletiva [Internet]. 2016 Dec [cited 2020 Jun 15];21(12):3803-18. Available from: http://dx.doi.org/10.1590/1413-812320152112.13682015 [ Links ]
4. Rao C, Lopez AD, Yang G, Begg S, Ma J. Evaluating national cause-of-death statistics: principles and application to the case of China. Bull World Health Organ [Internet]. 2005 Aug [cited 2020 Jun 15];83(8):618-25. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2626325/pdf/16184281.pdf [ Links ]
5. Soares Filho AM, Vasconcelos CH, Nóbrega AA, Pinto IV, Merchan-Hamann E, Ishitani LH, et al. Improvement of the unspecified external causes classification based on the investigation of death in Brazil in 2017. Rev Bras Epidemiol [Internet]. 2019 Nov [cited 2020 Jun 15]; 22 Suppl 3:e190011.supl.3. Available from: https://doi.org/10.1590/1980-549720190011.supl.3 [ Links ]
6. Brasil. Ministério da Saúde. Portaria n° 116, de 11 de fevereiro de 2009. Regulamenta a coleta de dados, fluxo e periodicidade de envio das informações sobre óbitos [Internet]. Diário Oficial da União, Brasília (DF), 2009 fev 12 [citado 2020 jun 15]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/svs/2009/prt0116_11_02_2009.html [ Links ]
7. Kalougivaki JJVP. Medico-legal death investigation systems in the pacific and creating a stronger pacific disaster victim identification network. J Forensic Res [Internet]. 2015 [cited 2020 Jun 15];6:1. Available from: https://doi.org/10.4172/2157-7145.1000255 [ Links ]
8. Ministério da Justiça (BR). Secretaria Nacional de Segurança Pública. Investigação criminal de homicídios [Internet]. Brasília: Ministério da Justiça; 2014 [citado 2020 jun 15]. 124 p. Disponível em: https://www.justica.gov.br/central-de-conteudo/seguranca-publica/livros/ctr_homicidios_final-com-isbn.pdf [ Links ]
9. Brasil. Presidência da República. Lei no 13.675, de 11 de junho de 2018. Disciplina a organização e o funcionamento dos órgãos responsáveis pela segurança pública; cria a Política Nacional de Segurança Pública; institui o Sistema Único de Segurança Pública [Internet]. Diário Oficial da União, Brasília (DF), 2018 jun 12 [citado 2020 jun 15]. Disponível em: http://www.planalto.gov.br/ccivil_03/_Ato2015-2018/2018/Lei/L13675.htm [ Links ]
10. GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 198-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet [Internet]. 2016 Oct [cited 2020 Jun 15];388(10053):1459-544. Available from: https://doi.org/10.1016/S0140-6736(16)31012-1 [ Links ]
11. Balieiro PCS, Silva LCF, Sampaio VS, Monte EX, Pereira EMS, Queiroz LAF, et al. Fatores associados à mortalidade por causas inespecíficas e mal definidas no estado do Amazonas, Brasil, de 2006 a 2012. Ciênc Saúde Coletiva [Internet]. 2020 jan [citado 2020 mar 27];25(1):339-52. Disponível em: http://dx.doi.org/10.1590/1413-81232020251.27182017 [ Links ]
12. Kanso S, Romero DE, Leite IC, Moraes EN. Diferenciais geográficos, socioeconômicos e demográficos da qualidade da informação da causa básica de morte dos idosos no Brasil. Cad Saúde Pública [Internet]. 2011 jul [citado 2020 Jul 15];27(7):1323-39. Disponível em: http://dx.doi.org/10.1590/S0102-311X2011000700008 [ Links ]
13. Lopes AS, Passos VMA, Souza MFM, Cascão AM. Improvement of data quality on the underlying cause of death from external causes using Health, Public Security and Press sector database linkage in the State of Rio de Janeiro, Brazil, 2014. Epidemiol Serv Saúde [Internet]. 2018 [cited 2020 Jun 15];27(4):e2018058. Available from: https://doi.org/10.5123/s1679-49742018000400011 [ Links ]
14. Lu TH, Walker S, Anderson RN, McKenzie K, Bjorkenstam C, Hou WH. Proportion of injury deaths with unspecified external cause codes: a comparison of Australia, Sweden, Taiwan and the US. Inj Prev [Internet]. 2007 [cited 2020 Jun 15];13(4):276-81. Available from: http://dx.doi.org/10.1136/ip.2006.012930 [ Links ]
15. Loreto Núñez FM, Gloria Icaza NM. Calidad de las estadísticas de mortalidad en Chile, 1997-2003. Rev Med Chile [Internet]. 2006 [cited 2020 Jun 15];134(9):1191-6. Available from: http://dx.doi.org/10.4067/S0034-98872006000900016 [ Links ]
16. Miki J, Rampatige R, Richards N, Adair T, Cortez-Escalante J, Vargas-Herrera J. Saving lives through certifying deaths: assessing the impact of two interventions to improve cause of death data in Perú. BMC Public Health [Internet]. 2018 [cited 2020 Jun 15];18(1):1329. Available from: http://dx.doi.org/10.1186/s12889-018-6264-1 [ Links ]
17. Jackson D, Wenz K, Muniz M, Abouzahr C, Schmider A, Braschi MW, et al. Civil registration and vital statistics in health systems. Bull World Health Organ [Internet]. 2018 [cited 2020 Jun 15];96(12):861-3. Available from: http://dx.doi.org/10.2471/BLT.18.213090 [ Links ]
18. Books EG, Reed KD. Principles and pitfalls: a guide to death certification. Clin Med Res [Internet]. 2015 Jun [cited 2020 Jun 15];13(2):74-82. Available from: http://dx.doi.org/10.3121/cmr.2015.1276 [ Links ]
Received: July 02, 2020; Accepted: November 22, 2020











 texto en
texto en 


