Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.3 Brasília set. 2021 Epub 09-Jul-2021
http://dx.doi.org/10.1590/s1679-49742021000300012
ORIGINAL ARTICLE
Catastrophic costs and social sequels due to tuberculosis diagnosis and treatment in Brazil*
1Universidade Federal do Espírito Santo, Laboratório de Epidemiologia, Vitória, ES, Brazil
2Universidade Federal do Espírito Santo, Programa de Pós-Graduação em Saúde Coletiva, Vitória, ES, Brazil
3Universidade Federal de Mato Grosso do Sul, Programa de Pós-Graduação em Doenças Infecciosas e Parasitárias, Campo Grande, MS, Brazil
4Universidade Federal do Espírito Santo, Departamento de Ciências da Saúde, São Mateus, ES, Brazil
Objective:
To evaluate the impact of catastrophic costs on unfavorable tuberculosis treatment outcomes.
Methods:
This was a prospective cohort study, conducted in five Brazilian state capitals (Manaus, Recife, Vitória, Campo Grande and Porto Alegre) from June 2016 to July 2018. Logistic regression was used to calculate the odds ratio (OR) and 95% confidence intervals (95%CI).
Results:
Of the 350 participants, 310 were included, of whom 30 presented unfavorable outcomes. Catastrophic cost (OR=2.53 -95% CI 1.13;5.67) and divorce (OR=5.29 -95% CI 1.39;20.05) increased the chances of unfavorable outcomes.
Conclusion:
Financial difficulties during tuberculosis treatment may impair its outcome. Catastrophic cost and divorce were determining factors for treatment outcomes.
Keywords: Tuberculosis; Therapeutics; Costs and Cost Analysis; Cohort Studies; Socioeconomic Factors; Brazil
Introduction
Tuberculosis (TB) is an infectious disease with a strong social determinant, closely linked to poverty, with an important socioeconomic impact.1-6 In 2015, the World Health Organization (WHO) estimated about 10.4 million new cases and 1.4 million deaths due to TB worldwide. In 2016, there were 11.4 million new cases and 1.6 million deaths in developing countries.7 Spending on disease prevention, diagnosis and treatment reached $ 6.6 billion in 2015, exceeding the amount of $ 6.2 billion spent in 2014.8 Currently, estimates for financing TB control in the 129 low- and- middle-income countries monitored by the global plan to end TB have been increasing and, for the five-year period 2018-2022, $ 60 billion are expected, averaging $12 billion annually.9
Brazil ranks 30th in the list of countries with the highest TB burden.9 Approximately 80,000 cases are reported every year, in the country; in 2019, there were 73,864 incident cases.10 Among the factors that most contributed to this scenario were poverty and high population density in urban centers.11
WHO end TB strategy aims to end global TB epidemic by 2035.12 The new strategy has defined three high level indicators to facilitate progress focusing on controlling the disease to end TB. One of these goals ensure that no family is burdened with catastrophic costs due to TB.13.14
The Brazilian National Health System (SUS) provides universal and free treatment for TB,15 however, health seeking, diagnosis and follow-up during treatment represent expenses that may lead to losses and worsening of economic and financial situation, resulting in the impoverishment of many families.16
The total costs that people with TB have faced include direct payment (e.g. drugs, hospitalization and medical services, medical tests and transportation. Indirect costs include, mainly, loss of income because of incapacity for work due to illness. Direct and indirect costs may occur before and after TB diagnosis, and affect both sick individuals and other family members who provide care and support.13 In addition to direct and/or indirect costs, residents of TB-affected households may feel obliged to use their savings and/or borrow money.13
Studies concerning TB-affected household costs have already been conducted in other countries.1-3,16-18 In Brazil, there are few surveys on TB-related costs, usually focused on a city or a state.19-21
This study aimed to evaluate the economic impact on family level and social sequels observed, from TB diagnosis and treatment, in Brazil.
Methods
This was a prospective cohort study on data collected through face-to-face interviews and evaluation of case closure reported on the Notifiable Diseases Information System (Sinan).
The research was conducted in five Brazilian state capitals - Manaus, state of Amazonas (AM); Recife, state of Pernambuco (PE); Vitória, state of Espírito Santos (ES); Campo Grande, state of Mato Grosso do Sul (MS); and Porto Alegre, state of Rio Grande do Sul (RS). Data were collected in 14 health centers distributed among the five regions of the country, from June 2016 to July 2018. The selected health centers provide treatment for tuberculosis according to the guidelines established by the General Coordination for Surveillance of Chronic Conditions and Respiratory Transmitted Diseases (CGDR) of the Ministry of Health.
The sample analyzed was comprised of individuals diagnosed with tuberculosis, 18 years of age and older, undergoing treatment for at least one month with basic regimen (rifampicin, isoniazid, pyrazinamide and ethambutol for two months, and rifampicin and isoniazid for another four months). The first follow-up was conducted through interviews with individuals undergoing TB treatment at the selected health centers, on free demand, that is: those who agreed to be interviewed were included in the research as participants. In the second follow-up, the evaluation of the treatment outcome data described in the epigraph, made available by the municipal surveillance coordination offices, was performed as TB cases were closed.
The following variables were analyzed:
a) Sociodemographic
- Gender (male, female);
- Schooling (in years of study: 0-8; >8);
- Age (in years: 18-39; ≥40; not informed);
- Race/skin color (white; non-white [black; Asian; brown; indigenous; not informed]);
- Head of the family with TB (yes; no);
- Formal employment (yes; no);
- Job abandonment or school dropout (yes; no; not informed);
- Health insurance (yes; no).
b) Clinics
- Types of TB (pulmonary; extrapulmonary);
- Phases of treatment (intensive; follow-up);
- HIV (positive; negative; untested/unknown);
- Hospitalization (yes; no);
- Previous TB treatment (yes; no);
- Initial care (public; private; others);
- Comorbidities (yes; no).
c) Family changes during TB treatment
- Social sequel (yes; no);
- School dropout (yes; no);
- Job abandonment (yes; no);
- Divorce (yes; no);
- Disturbed sex life (yes; no);
- Child got sick (yes; no);
- Moved away from people (yes; no);
- Depression (yes; no);
- Experienced TB stigma (yes; no);
- Other social sequels (yes; no).
d) Economic conditions
- Household’s financial condition before TB (poor; not poor);
- Household’s financial condition after TB (poor; not poor);
- Income change after TB (yes; no).
e) Exposure
- Catastrophic cost exceeding a given threshold (e.g. 20%) of the household’s annual income before TB (yes; no).
f) Treatment outcome (favorable outcome [cure; treatment compliance]; unfavorable outcome [death; abandonment; treatment failure]).
'Catastrophic costs' were considered when household’s expenditures exceeded a given threshold (e.g. 20%) of the household’s annual income, according to World Health Organization.13,14 The WHO’s Tool to Estimate Patient's Costs was used as an instrument for data collection, in its Portuguese translation and Brazilian cultural adaptation.22.23 The catastrophic cost measurement started from the sum of total costs, divided by the value of the household’s annual income before the illness due to TB (household’s monthly income multiplied by 12).
To estimate medical and non-medical direct costs related to TB, the total medical direct costs during pre-diagnosis and diagnosis phases were used (the sum of total administrative costs, costs with diagnostic tests, radiological examination and medications); and non-medical direct costs such as, payment for transportation, food and accommodation - disregarding any reimbursement.
Micro-costing was used as the approach for valorization.24 The calculation of the total direct cost during treatment considered:
cost of visits to healthcare centers, necessary for treatment, directly observed per month (transportation and food costs for each weekly visit, taking into account four weeks in one month);
medication withdrawal costs (sum of transportation and food costs, administrative and accommodation costs, multiplied by the number of health care visits /month);
follow-up costs (sum of the total costs of a visit, such as payment for consultation fee, sputum culture test, radiological examination and medicines, among others, multiplied by the number of visits to the health center/month);
hospitalization costs (sum of payments for hospital administration fee, bed sheets/clothing, food, transportation, drugs, laboratory tests among others); and
monthly cost (payment for adequate food).
The approach for valorization of indirect costs used the human capital method. In this case, for the measurement of indirect costs related to TB, the total indirect costs of the infected individual were used, due to incapacity for work.24 The calculation of incapacity to work started from the individual monthly income before TB, multiplied by the total period of absence (in months) due to illness. The perspective addressed was that of the patient as payer.24
Extrapolation method was used to estimate the costs of the phases in which participants’ data were not collected (intensive and maintenance phases). For participating individuals who were interviewed during the intensive phase, the sum of the costs of pre-diagnosis and diagnosis plus direct costs (medical and non-medical) and indirect costs, multiplied by 2 and added to the average of the costs of maintenance phase, then multiplied by 4 or 6 (depending on the number of months established for the treatment) was used. Regarding the participating individuals who were interviewed during the maintenance phase the sum of the costs of pre-diagnosis and diagnosis plus direct costs (medical and non-medical) and indirect costs, multiplied by 4 or 6 (depending on the number of months established for the treatment), then multiplied by 2, was used. Therefore, for the total cost that was extrapolated, the monthly cost was used according to the phase in which the participant was interviewed, multiplied by the number of months established for the participant’s treatment during this phase plus the extrapolation value determined for the phase in which the participant was not interviewed.
For the calculation of impoverishment (decrease of participant's income during TB treatment), the monthly income was used before the illness divided by the number of household residents. To characterize poverty, the upper limit established by the World Bank of R$ 387.07 per month was used as a definition of a poor person.25 Thus, an income less than R$ 387.07/month per resident was considered a 'poor' condition, and an income higher than this, 'non- poor'.
During the approach of research participants, aiming to minimize possible recall bias of self-reported expenditures and thus help them answer the questionnaire, the researcher responsible for data collection used specific didactic approaches, such as: calendar help; mention of the latest visits to health centers; and the total amount spent on the last purchase, in the current month or week.
The size of the study was calculated using the Epidat® 4.0. The catastrophic cost was considered as an exposure factor, and an unfavorable outcome (death, abandonment or treatment failure) was considered as an outcome. Arbitrarily, the 15% risk among those exposed, and 7% risk among those unexposed, (ii) the ratio between unexposed and exposed of 5, (iii) 5% significance level and (iv) an 85% test power were considered. The minimum sizes were defined in 151 individuals without catastrophic costs and 75 with catastrophic costs. For possible losses, either during cost data collection or in the outcome, the sample was increased by 55%, obtaining a sample size of 350 participants, divided according to the incidence in each selected capital: Recife, state of Pernambuco (29.3%; 103 participants); Campo Grande, state of Mato Grosso do Sul (5.1%; 18 participants); Victoria, state of Espírito Santo (2.1%; 7 participants); Manaus, state of Amazonas (36%; 126 participants); and Porto Alegre, state of Rio Grande do Sul (27.3%; 96 participants).
In the variable description, absolute and relative frequencies were calculated. In the bivariate analysis, Pearson's chi-square test and Fisher's exact text were used.
The results of logistic regression analyses were expressed as odds ratio (OR) and 95% confidence intervals (95%CI). Logistic regression was used to investigate risk factors of TB treatment outcome. Hypothetical risk factors associated with p<0.2 outcomes were included in the multivariate analysis. For the multiple analysis, a theoretical model of classification of determinants at hierarchical levels was used: at the distal level, sociodemographic variables; at the intermediate level, clinical information regarding the current TB treatment and changes in family during TB episode; and at the proximal level, financial variables. P<0.05 values were considered statistically significant. For statistical analysis of data, Stata 14.0 software for statistics was used.
The study project was approved by the Human Research Ethics Committee of the Center for Health Sciences of the Federal University of Espírito Santo (CEP/CCS/UFES): Opinion No. 1,856,319, issued on December 7, 2016; Certificate of Submission for Ethical Appraisal (CAAE) No. 61080416.7.0000.5060. All participants were informed about the objectives of the research and signed the Free and Informed Consent Form, before granting an interview.
Results
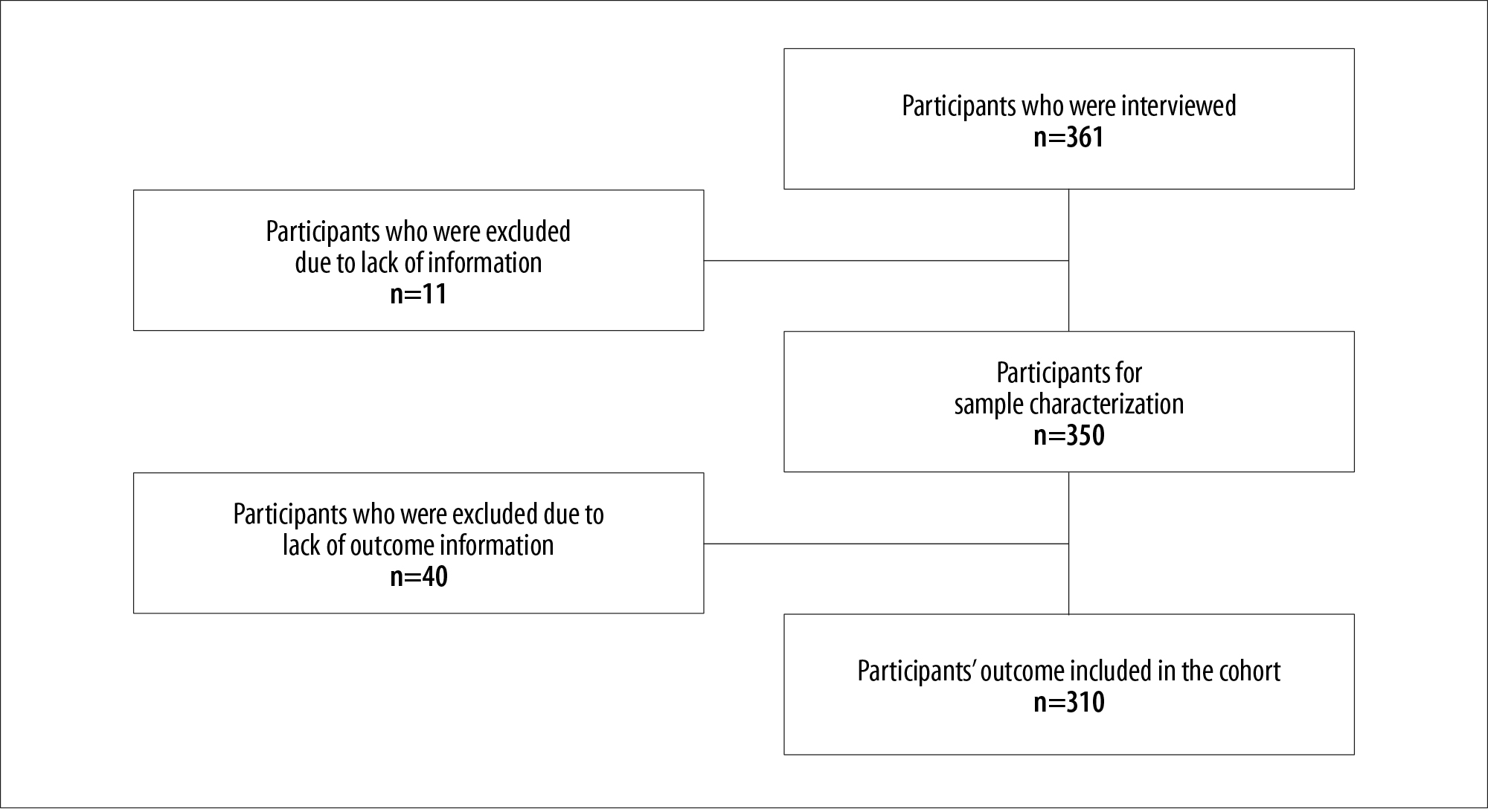
During the first follow-up of the study, 361 participants were eligible, of whom 11 did not report family income before illness due to TB, therefore it was not possible to calculate their catastrophic cost, while another 40 (11%) had no record of treatment outcome on Sinan. The final sample was comprised of 310 participants (Figure 1).
Regarding participating individuals undergoing TB treatment, 65% were male and 46% were head of the family. With regard to work, 60% of the interviewed participants were unemployed or were inserted in the informal labor market; 62% stopped working, studying or doing household chores due to illness. 83% of the interviewed participants were new TB cases, in relation to retreatment tuberculosis patients, 44% did not complete the previous treatment of tuberculosis. 71% of the households studied, were considered non-poor before one of its members became sick with TB disease; this percentage decreased to 61% after illness, showing a decreased income in 11% of the households studied (Table 1).
According to Table 2, 30 participants presented unfavorable outcome. In the adjusted analysis, divorce (OR=5.29 -95% CI 1.39;20.05) and catastrophic cost (OR=2.53 -95% CI 1.13;5.67) significantly increased the chances of an unfavorable treatment outcome.
Table 1 - Distribution of sociodemographic and clinic characteristics, changes in family during TB episode and economic status, according to catastrophic costs due to TB of participating individuals with TB from the five capitals (n=350), Brazil, June/2016-July/2018
| Variables | N (%) Total | N (%) Without catastrophic costs | N (%) With catastrophic costs |
|---|---|---|---|
| Sex | |||
| Male | 226 (65) | 132 (58) | 94 (42) |
| Female | 124 (35) | 73 (59) | 51 (41) |
| Schooling (years of study) | |||
| 0-8 | 173 (49) | 82 (47) | 91 (53) |
| >8 | 177 (51) | 123 (69) | 54 (31) |
| Age (years) | |||
| 18-39 | 165 (47) | 90 (55) | 75 (45) |
| ≥40 | 182 (52) | 113 (62) | 69 (38) |
| Not informed | 3 (1) | 2 (67) | 1 (33) |
| Race/skin color | |||
| White | 91 (26) | 59 (65) | 32 (35) |
| Non-white | 257 (73) | 145 (56) | 112 (44) |
| Not informed | 2 (1) | 1 (50) | 1 (50) |
| Head of the family with TB | |||
| Yes | 162 (46) | 86 (53) | 76 (47) |
| No | 188 (54) | 119 (63) | 69 (37) |
| Formal job | |||
| Yes | 139 (40) | 105 (76) | 34 (24) |
| No | 211 (60) | 100 (47) | 111 (53) |
| Absence from work or studies | |||
| Yes | 218 (62) | 104 (48) | 114 (52) |
| No | 126 (36) | 96 (76) | 30 (24) |
| Not informed | 6 (1) | 5 (83) | 1 (18) |
| Health insurance | |||
| Yes | 73 (21) | 62 (85) | 11 (15) |
| No | 277 (79) | 143 (52) | 134 (48) |
| Types of tuberculosis (TB) | |||
| Pulmonary | 263 (75) | 161 (61) | 102 (39) |
| Extrapulmonary | 87 (25) | 44 (51) | 43 (49) |
| Phases of treatment | |||
| Intensive | 98 (28) | 56 (57) | 42 (43) |
| Continuation | 252 (72) | 149 (59) | 103 (41) |
| HIVa | |||
| Positive | 60 (17) | 26 (43) | 34 (57) |
| Negative | 241 (69) | 149 (62) | 92 (38) |
| Untested/unknown | 49 (14) | 30 (61) | 19 (39) |
| Hospitalization | |||
| Yes | 140 (40) | 65 (46) | 75 (54) |
| No | 210 (60) | 140 (67) | 70 (33) |
| Previous TB treatment | |||
| Yes | 60 (17) | 30 (50) | 30 (50) |
| No | 290 (83) | 175 (60) | 115 (40) |
| Initial care | |||
| Public | 314 (90) | 180 (57) | 134 (43) |
| Private | 22 (6) | 18 (82) | 4 (18) |
| Others | 14 (4) | 7 (50) | 7 (50) |
| Comorbidities | |||
| Yes | 142 (41) | 76 (54) | 66 (46) |
| No | 208 (59) | 129 (62) | 79 (38) |
| Social sequel | |||
| Yes | 230 (66) | 123 (53) | 107 (47) |
| No | 120 (34) | 82 (68) | 38 (32) |
| School dropout | |||
| Yes | 5 (1) | 3 (60) | 2 (40) |
| No | 345 (99) | 202 (59) | 143 (41) |
| Job abandonment | |||
| Yes | 98 (28) | 40 (41) | 58 (59) |
| No | 252 (72) | 165 (65) | 87 (35) |
| Divorce | |||
| Yes | 17 (5) | 8 (47) | 9 (53) |
| No | 333 (95) | 197 (59) | 136 (41) |
| Disturbed sex life | |||
| Yes | 10 (3) | 7 (70) | 3 (30) |
| No | 340 (97) | 198 (58) | 142 (42) |
| Child got sick | |||
| Yes | 4 (1) | 3 (75) | 1 (25) |
| No | 346 (99) | 202 (58) | 144 (42) |
| Moved away from people | |||
| Yes | 95 (25) | - | 95 (100) |
| No | 255 (73) | 120 (47) | 135 (53) |
| Depression | |||
| Yes | 10 (3) | 7 (70) | 3 (30) |
| No | 340 (97) | 198 (58) | 142 (41) |
| Experience of prejudice due to tuberculosis | |||
| Yes | 17 (5) | 12 (71) | 5 (29) |
| No | 333 (95) | 193 (58) | 140 (42) |
| Other social sequels | |||
| Yes | 128 (37) | 78 (61) | 50 (39) |
| No | 222 (63) | 127 (57) | 95 (43) |
| Household’s financial condition before TB episode | |||
| Poor | 101 (29) | 33 (33) | 68 (67) |
| Non-poor | 249 (71) | 172 (69) | 77 (31) |
| Household’s financial condition after TB episode | |||
| Poor | 138 (39) | 54 (39) | 84 (61) |
| Non-poor | 212 (61) | 151 (71) | 61 (29) |
| Household income change after TB episode | |||
| Yes | 40 (11) | 22 (55) | 18 (45) |
| No | 310 (89) | 183 (59) | 127 (41) |
| Total | 350 (100) | 205 (59) | 145 (41) |
a) HIV: human immunodeficiency virus.
Table 2 - Tuberculosis (TB) treatment outcome and odds ratio of the unfavorable outcome, according to the characteristics of participating individuals with tuberculosis from the five capitals (n=310), Brazil, June/2016-July/2018
| Variables | Treatment outcome | Crude odds ratio (95%IC a ) | Adjusted odds ratio (95%IC a ) | |||
|---|---|---|---|---|---|---|
| Favorable (%) | Unfavorable (%) | p-valor | p-valueb | |||
| Distal level: sociodemographic variables | ||||||
| Sex | ||||||
| Male | 182 (91) | 18 (9) | 0.80 (0.35;1.92) | 0.586d | - | |
| Female | 98 (89) | 12 (11) | ||||
| Schooling (years of study) | ||||||
| 0-8 | 145 (91) | 14 (9) | 1.22 (0.53;2.82) | 0.594d | - | |
| >8 | 135 (89) | 16 (11) | ||||
| Age (years) | ||||||
| 18-39 | 135 (91) | 14 (9) | 1.06 (0.46;2.45) | 0.872d | - | |
| ≥40 | 145 (90) | 16 (10) | ||||
| Race/skin color | ||||||
| White | 70 (90) | 8 (10) | 0.92 (0.37;2.51) | 0.859d | - | |
| Non-white | 208 (90) | 22 (9%) | ||||
| Head of the family with tuberculosis | ||||||
| Yes | 122 (90) | 14 (10) | 1.13 (0.492.58) | 0.745d | - | |
| No | 158 (91) | 16 (9) | ||||
| Formal job | ||||||
| Yes | 112 (93) | 9 (7) | 1.55 (0.65;3.99) | 0.286d | - | |
| No | 168 (89) | 21 (11) | ||||
| Job abandonment or school dropout | ||||||
| Yes | 169 (88) | 22 (12) | 1.98 (0.78;5.69) | 0.121d | - | |
| No | 107 (94) | 7 (6) | ||||
| Health insurance | ||||||
| Yes | 61 (92) | 5 (8) | 0.71 (0.20;2.02) | 0.515d | - | |
| No | 219 (90) | 25 (10) | ||||
| Intermediate level: clinical information regarding the current TB treatment and changes in family during TB episode variables | ||||||
| Types of tuberculosis | ||||||
| Pulmonary | 208 (90) | 23 (10) | 1.13 (0.44;3.27) | 0.776d | - | |
| Extrapulmonary | 72 (91) | 7 (9) | ||||
| Phases of treatment | ||||||
| Intensive | 75 (88) | 10 (12) | 1.36 (0.54; 3.22) | 0.445d | - | |
| Continuation | 205 (91) | 20 (9) | ||||
| HIVc | ||||||
| Positive | 50 (93) | 4 (7) | 0.69 (0.16;2.16) | 0.616e | - | |
| Negative | 190 (90) | 22 (10) | ||||
| Hospitalization | ||||||
| Yes | 173 (91) | 17 (9) | 1.23 (0.52;2.82) | 0.584d | - | |
| No | 107 (89) | 13 (11) | ||||
| Previous TB treatment | ||||||
| Yes | 43 (81) | 10 (19) | 2.75 (1.07;6.66) | 0.013d | 2.34 (0.99;5.53) | 0.051 |
| No | 237 (92) | 20 (8) | 1.00 | |||
| Initial care | ||||||
| Public | 254 (91) | 25 (9) | 1.19 (0.12;5.52) | 0.686e | - | |
| Private | 17 (89) | 2 (11) | ||||
| Comorbidities | ||||||
| Yes | 119 (91) | 12 (9) | 0.9 (0.38;2.06) | 0.792d | - | |
| No | 161 (90) | 18 (10) | ||||
| Social sequel | ||||||
| Yes | 182 (90) | 21 (10) | 1.25 (0.52;3.23) | 0.584d | - | |
| No | 98 (92) | 9 (8) | ||||
| School dropout | ||||||
| Yes | 5 (100) | - | 0 (0.00;7.2) | 0.599e | - | |
| No | 275 (90) | 30 (10) | ||||
| Job abandonment | ||||||
| Yes | 80 (86) | 13 (14) | 1.91 (0.81;4.38) | 0.094d | - | |
| No | 200 (92) | 17 (8) | ||||
| Divorce | ||||||
| Yes | 8 (67) | 4 (33) | 5.23 (1.06;21.00) | 0.02e | 5.29 (1.39;20.05) | 0.014 |
| No | 272 (91) | 26 (9) | 1.00 | |||
| Disturbed sex life | ||||||
| Yes | 10 (100) | - | 0 (0.00;3.54) | 0.606e | - | |
| No | 270 (90) | 30 (10) | ||||
| Child got sick | ||||||
| Yes | 4 (100) | - | 0 (0.00;9.14) | 0.664e | - | |
| No | 276 (90) | 30 (10) | ||||
| Moved away from people | ||||||
| Yes | 72 (92) | 6 (8) | 0.72 (0.23;1.91) | 0.493d | - | |
| No | 208 (90) | 24 (10) | ||||
| Depression | ||||||
| Yes | 9 (100) | - | 0 (0.00;3.96) | 0.395e | - | |
| No | 271 (90) | 30 (10) | ||||
| Experience of prejudice due to tuberculosis | ||||||
| Yes | 15 (94) | 1 (6) | 0.60 (0.01;4.25) | 0.528e | - | |
| No | 265 (90) | 29 (10) | ||||
| Other social sequels | ||||||
| Yes | 102 (92) | 8 (7) | 0.63 (0.23;1.54) | 0.288d | - | |
| No | 178 (89) | 22 (11) | ||||
| Proximal level: financial variables | ||||||
| Catastrophic cost | ||||||
| Yes | 109 (85) | 19 (15) | 2.70 (1.16;6.54) | 0.010d | 2.53 (1.13;5,67) | 0,023 |
| No | 171 (94) | 11 (6) | 1,00 | |||
| Household financial condition before tuberculosis episode | ||||||
| Poor | 74 (85) | 13 (15) | 2.12 (0.90;4.89) | 0.050d | - | |
| Non-poor | 206 (92) | 17 (8) | ||||
| Household financial condition after tuberculosis episode | ||||||
| Poor | 104 (87) | 16 (13) | 1.93 (0.84;4.46) | 0.084d | - | |
| Non-poor | 176 (93) | 14 (7) | ||||
| Household income change after tuberculosis episode | ||||||
| Yes | 33 (92) | 3 (8) | 0.83 (0.15;2.94) | 0.529e | - | |
| No | 247 (90) | 27 (10) | ||||
| Total | 280 (90) | 30 (10) | ||||
a) 95%CI: 95% confidence interval; b) Wald test; (c) HIV: human immunodeficiency virus; d) Pearson’s chi-square test; e) Fisher's exact test.
Discussion
Financial difficulties faced by Brazilian families during TB diagnosis and treatment, and the social sequels of the disease, influence treatment outcome. Regarding the participants included and followed during TB treatment, the majority who presented unfavorable outcome also reported catastrophic cost. This was the first research conducted in Brazil with individuals undergoing TB treatment and devoted to the analysis of the association between catastrophic costs and treatment outcome experienced by TB patients and their households.
The analysis was based on self-reported expenditure, subject to underestimation or overestimation by the participants. Data were collected from men and women with TB assisted by diagnostic and treatment services for tuberculosis, therefore those who did not seek treatment were not included in the study. Data were collected from the second month of treatment and, thus, memory bias may have affected the findings. Adequate access to TB treatment, free of charge, in Brazil, however, prevented obtaining some hospital expenditure, limiting the comparison between data analysis and other scenarios. Participants working in the informal economy, self-employed and in agricultural activity, found it difficult to measure income and, therefore, the treatment outcomes of some of them were not obtained, given the limitation of the study in the use of secondary data. The cost stratification data were not showed for this article, although, it is possible that these limitations have not interfered in the results.
Approximately two-fifths of the participants reported catastrophic costs, a finding similar to studies conducted in Indonesia and Uganda, where the catastrophic cost was 36%4 and 53% respectively.3 The main contributor to total costs is participants’ income loss when they fall ill with TB. Long-term treatment and the severity of some cases, which can lead to greater or lesser incapacity to return to work, are relevant attributes to consider. Similar to other studies, the social impact of TB on patients and their households was alarming, a consequence of significant income loss and the cost generated by diagnosis and treatment.26.27 Participants from other surveys also stated that they were affected by income and job losses.16.26
With regard to participants with unfavorable outcome, the majority presented catastrophic cost. The chance of individuals who had tuberculosis presenting catastrophic cost and not succeeding in treatment was approximately 2.5 fold greater than those who did not present catastrophic cost. Despite the fact that the Brazilian National Health System (SUS) has universal coverage of health services that provides adequate access to TB diagnosis and treatment, free of charge, the disease implies other costs, as a result of the incapacity to work during the TB episode, and it is important to consider the need for government intervention aiming at minimizing the catastrophic costs due to TB, through specific public policy, in order to reduce income loss and thus improve the indicators of treatment outcome. This commonly suggested coping mechanism can mitigate the financial burden reported in other studies and optimize TB treatment and cure.1-4,16
Job and income losses after TB diagnosis are extremely important, as determining factors for household impoverishment, given that individuals are not able to maintain household financial stability after falling ill. The study observed that 11% of households underwent significant income change, before and after illness, leading to impoverishment. The findings of this study corroborate those of other studies conducted in Indonesia in 2018 and 2019, which found it would be relevant to provide travel assistance and nutritional support, and, moreover, social protection for TB patients, family members and the closest people, affected by the costs of tuberculosis disease in the context of their households.4.18
Important findings have described the disruption or breakup of a tuberculosis patient's home, a fact that has been neglected in important studies. Divorce or separation, disturbed sex life, social sequels among the participants of this research, are examples of these findings. The work on screen showed that experiencing divorce due to TB increased the chances of unfavorable treatment outcome by five times. In 2016, 344,526 divorces were recorded in Brazil - 2.38 divorces per 1 million inhabitants, a frequency lower than that observed in this study.28
The determinants of treatment outcomes showed in this study, highlight the magnitude of the problem of income loss and the need to address it adequately, in addition to the social difficulties faced due to TB. Households, both poor and non-poor, may experience poverty more deeply. This risk is more evident in participants from poor families.18 The findings of this study suggest that other measures, in addition to free medical services, are considered, especially when they are aimed at people living in poverty.
More than half of the participating individuals with TB who were interviewed have experienced some social sequels, approximately one quarter experienced job abandonment and a quarter mentioned that had moved away from people. It is necessary to consider socioeconomic and health system differences among different countries, also identified in other studies, in different proportions, taking into account their similarity experienced by TB patients, their respective specificities and determining factors of the evolution of TB in participating individuals and the impact on their households.1.3
In conclusion, Brazilian families run the risk of facing financial difficulties during TB episode, which may affect TB treatment outcome.
REFERENCES
1. Nhung NV, Hoa NB, Anh NT, Ngoc Anh LT, Siroka A, Lönnroth K, et al. Measuring catastrophic costs due to tuberculosis in Viet Nam. Int J Tuberc Lung Dis. 2018 Sep 1;22(9):983-90. doi: http://doi.org/10.5588/ijtld.17.0859. [ Links ]
2. Pedrazzoli D, Siroka A, Boccia D, Bonsu F, Nartey K, Houben R, et al. How affordable is TB care? Findings from a nationwide TB patient cost survey in Ghana. Trop Med Int Health. 2018;23(8):870-8. doi: https://doi.org/10.1111/tmi.13085. [ Links ]
3. Muttamba W, Tumwebaze R, Mugenyi L, Batte C, Sekibira R, Nkolo A, et al. Households experiencing catastrophic costs due to tuberculosis in Uganda: magnitude and cost drivers. BMC Public Health. 2020 Sep 16;20(1):1409. doi: https://doi.org/10.1186/s12889-020-09524-5. [ Links ]
4. Fuady A, Houweling TAJ, Mansyur M, Burhan E, Richardus JH. Effect of financial support on reducing the incidence of catastrophic costs among tuberculosis-affected households in Indonesia: eight simulated scenarios. Infect Dis Poverty. 2019 Feb 2;8(1):10. doi: https://doi.org/10.1186/s40249-019-0519-7. [ Links ]
5. Hargreaves JR, Boccia D, Evans CA, Adato M, Petticrew M, Porter JDH. Os determinantes sociais da tuberculose: das evidências à ação. Am J Public Health. 2011;101(4):654-62. doi: https://doi.org/10.2105/AJPH.2010.199505. [ Links ]
6. Oxlade O, Murray M. Tuberculosis and poverty: why are the poor at greater risk in India? PLoS One. 2012;7(11):e47533. doi: https://doi.org/10.1371/journal.pone.0047533. [ Links ]
7. World Health Organization. WHO Report 2016: global tuberculosis control. Geneva: WHO; 2017. [ Links ]
8. World Health Organization. WHO Report 2015: global tuberculosis control: surveillance, planning, financing. Geneva: WHO; 2015. [ Links ]
9. World Health Organization. WHO report 2019: global tuberculosis control: surveillance, planning, financing. Geneva: WHO ; 2019. [ Links ]
10. Ministério da Saúde (BR), Secretaria de Vigilância em Saúde. Doença pelo coronavírus: COVID-19. [Brasília, DF]: MS; 2020. (Boletim epidemiológico especial: n. 33). [ Links ]
11. Haling G, Castro MC. A spatial analysis of social and economic determinants of tuberculosis in Brazil. Health Place. 2014;25:56-67. doi: https://doi.org/10.1016/j.healthplace.2013.10.008. [ Links ]
12. World Health Organization. The end tuberculosis strategy. Geneva: WHO ; 2016. [ Links ]
13. World Health Organization. Tuberculosis patient cost surveys: a handbook. Geneva: WHO ; 2017. [ Links ]
14. World Health Organization. Protocol for survey to determine direct and indirect costs due to tuberculosis and to estimate proportion of tuberculosis-affected households experiencing catastrophic total costs due to tuberculosis. Geneva: WHO ; 2015. [ Links ]
15. Ministério da Saúde (BR), Secretaria de Vigilância em Saúde. Manual de recomendações para o controle da tuberculose no Brasil. Brasília, DF: MS; 2019. [ Links ]
16. Tanimura T, Jaramillo E, Well D, Raviglione M, Lonnroth K. Financial burden for tuberculosis patients in low- and middle-income countries: a systematic review. Eur Respir J. 2015;43(6):1763-75. doi: https://doi.org/10.1183/09031936.00193413. [ Links ]
17. Jackson S, Sleigh AC, Wang GJ, Liu XL. Poverty and the economic effects of tuberculosis in rural China. Int J Tuberc Lung Dis. 2006:10(10):1104-10. [ Links ]
18. Fuady A, Houweling TAJ, Mansyur M, Richardus JH. Catastrophic total costs in tuberculosis-affected households and their determinants since Indonesia's implementation of universal health coverage. Infect Dis Poverty. 2018 Jan. 12;7(1):3. doi: https://doi.org/10.1186/s40249-017-0382-3. [ Links ]
19. Steffen R, Menzies D, Oxlade O, Pinto M, Castro AZ, Monteiro P, et al. Patients' costs and cost-effectiveness of tuberculosis treatment in DOTS and non-DOTS facilities in Rio de Janeiro, Brazil. PLoS One. 2010 Nov 17;5(11):e14014. doi: https://doi.org/10.1186/s40249-017-0382-3.2018. [ Links ]
20. Costa JG, Santos AC, Rodrigues LC, Barreto ML, Roberts JA. Tuberculosis in Salvador, Brazil: costs to health system and families. Rev Saude Publica. 2005;39(1):122-8. doi: http://doi.org/10.1590/s0034-89102005000100016. Português [ Links ]
21. Prado TN, Wada N, Guidoni LM, Golub JE, Dietze R, Maciel ELN. Cost-effectiveness of community health worker versus home-based guardians for directly observed treatment of tuberculosis in Vitoria, Espírito Santo State, Brazil. Cad Saude Publica. 2011;27(5):944-52. doi: http://doi.org/10.1590/s0102-311x2011000500012. [ Links ]
22. KNCV Tuberculosis Foundation. Tool to estimate patients’ costs literature review. [The Hague, NL: KNCV]; 2008. [ Links ]
23. Nunes GF, Guidoni LM, Negri LSA, Zandonade E, Maciel ELN. Adaptação transcultural do instrumento “Tool to estimate patient’s costs” em municípios prioritários do Brasil no controle da tuberculose. Esc Anna Nery. 2018;22(4):e20180073. doi: http://doi.org/10.1590/2177-9465-ean-2018-0073. [ Links ]
24. Silva EM, Silva MT, Pereira MG. Identificação, mensuração e valoração de custos em saúde. Epidemiol Serv Saude. 2016;25(2):437-39. doi: http://dx.doi.org/10.5123/S1679-49742016000200023. [ Links ]
25. Instituto Brasileiro de Geografia e Estatística. Síntese de indicadores sociais: uma análise das condições de vida da população brasileira: Coordenação de População e Indicadores Sociais. Rio de Janeiro: IBGE; 2017. [ Links ]
26. Wingfield T, Tovar MA, Huff D, Boccia D, Montoya R, Ramos E, et al. The economic effects of supporting tuberculosis-affected households in Peru. Eur Respir J. 2016;48(5):1396-410. doi: http://dx.doi.org/10.1183/13993003.00066-2016. [ Links ]
27. Tomeny EM, Mendoza VL, Marcelo DB, Barrameda AJD, Langley I, Abong JM, et al. Patient-cost survey for tuberculosis in the context of patient-pathway modelling. Int J Tuberc Lung Dis. 2020:24(4):420-7. doi: http://doi.org/10.5588/ijtld.19.0206. [ Links ]
28. Instituto Brasileiro de Geografia e Estatística. Informativo das estatísticas do registro civil. Rio de Janeiro: IBGE ; 2016. 8 P. (vol. 43). [ Links ]
*Article derived from the doctoral thesis entitled 'Impact of catastrophic costs on the treatment of patients with tuberculosis in five regions of Brazil', submitted by Leticia Molino Guidoni to the Postgraduate Program in Collective Health of the Federal University of Espírito Santo, on August 10, 2020.
Erratum
In the article “Catastrophic costs and social sequels due to tuberculosis diagnosis and treatment in Brazil”, doi: 10.1590/S1679-49742021000300012, published on Epidemiology and Health Services, 30(3): 1-13, in the page 1:
Original text:
Márcia Regina de Oliveira Pedroso1 - orcid.org/0000-0002-2859-159X
Leticia Molino Guidoni1 - orcid.org/0000-0003-3737-5407
Eliana Zandonade2 - orcid.org/0000-0001-5160-3280
Geisa Fregona2 - orcid.org/0000-0001-5835-8222
Letícya dos Santos Almeida Negri1 - orcid.org/0000-0002-0056-4506
Sandra Maria do Valle Leone de Oliveira3 - orcid.org/0000-0002-8960-6716
Thiago Nascimento do Prado1 - orcid.org/0000-0001-8132-6288
Carolina Maia Martins Sales1 - orcid.org/0000-0002-2879-5621
Raisa da Silveira Coimbra1 - orcid.org/0000-0003-2528-6044
Heletícia Scabelo Galavote4 - orcid.org/0000-0003-4490-6763
Ethel Leonor Noia Maciel2 - orcid.org/0000-0003-4826-3355
Corrected text:
Leticia Molino Guidoni1 - orcid.org/0000-0003-3737-5407
Eliana Zandonade2 - orcid.org/0000-0001-5160-3280
Geisa Fregona2 - orcid.org/0000-0001-5835-8222
Letícya dos Santos Almeida Negri1 - orcid.org/0000-0002-0056-4506
Sandra Maria do Valle Leone de Oliveira3 - orcid.org/0000-0002-8960-6716
Thiago Nascimento do Prado1 - orcid.org/0000-0001-8132-6288
Carolina Maia Martins Sales1 - orcid.org/0000-0002-2879-5621
Raisa da Silveira Coimbra1 - orcid.org/0000-0003-2528-6044
Heletícia Scabelo Galavote4 - orcid.org/0000-0003-4490-6763
Ethel Leonor Noia Maciel2 - orcid.org/0000-0003-4826-3355
Received: September 27, 2020; Accepted: February 09, 2021











 texto em
texto em