Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.3 Brasília set. 2021 Epub 04-Ago-2021
http://dx.doi.org/10.1590/s1679-49742021000300002
ORIGINAL ARTICLE
Health-related habits among community health workers in Montes Claros, Minas Gerais, Brazil: a cross-sectional study, 2018
1Centro Universitário FIPMoc, Departamento de Medicina, Montes Claros, MG, Brazil
2Faculdade de Saúde Ibituruna, Departamento de Nutrição, Montes Claros, MG, Brazil
3Universidade Estadual de Montes Claros, Programa de Pós-Graduação em Cuidado Primário em Saúde, Montes Claros, MG, Brazil
Methods:
This was a cross-sectional study conducted in Montes Claros, Minas Gerais, Brazil, 2018. Anthropometric, sociodemographic, labor and lifestyle characteristics were evaluated. Poisson regression was applied to calculate the prevalence ratio (PR) and 95% confidence interval (95%CI) of unhealthy habits according to independent variables.
Results:
675 CHW participated. Regarding their health profile, 60.8% were overweight, 83.0% reported low fruit consumption and 58.1% reported low greens and vegetable consumption. Physical inactivity was reported by 26.2%. 7.1% stated they were smokers were 37.6% drank alcoholic beverages. Inadequate health habits were higher among males (PR=1.24 - 95%CI 1.05;1.45), younger workers (PR=1.19 - 95%CI 1.01;1.40) and workers without a religion (PR=1.23 - 95%CI 1.04;1.45).
Conclusion:
There was relevant prevalence of inadequate health habits among community health workers, associated with sociodemographic factors.
Keywords: Occupational Health; Risk Factors; Chronic Disease; Community Health Workers; Cross-Sectional Studies.
Introduction
Community health workers (CHW) are professionals responsible for providing counseling for prevention and health promotion, guidance about health services, and strengthening the link between families and teams of health professionals. CHWs provide guidance on healthy living habits, including healthy eating, physical activity, and body weight control,1 and thus potentially contribute to chronic disease management in primary health care.2
Chronic non-communicable diseases (NCDs) have multifactorial causes and are influenced by the presence of four main risk factors: alcohol abuse, inadequate diet, sedentary lifestyle, and tobacco consumption. Removal and/or reduction of exposure to these factors is determinant in reducing mortality, morbidity, and future complications of these diseases.3
It is known that the long working hours, stress and anxiety experienced by health care workers can directly affect their quality of life.4 Demands and challenges found in the CHW work process can have a negative impact on the health of these professionals,5 who work on the front line of adequate habit promotion. Adoption of unhealthy practices in their own lives can influence their competence as health workers. CHWs embody the closest and most immediate contact of the population with the Brazilian National Health System (SUS), and when they adopt healthy habits, they contribute to the dissemination of these practices in the community they serve. Precisely through this they will gain the trust of the population in both preventive counseling and their broader work, motivating individuals to avoid risky health behaviors.4),(6),(7
As potential multipliers of this information in society, CHWs can and should strive for a better understanding of factors related to well-being and improved quality of life among the general population.8 There is evidence that if a health professional is committed to adopting a proper diet, he or she is more likely to be effective in counseling the population on the benefits of physical activity and healthy eating.4)
The objective of this study was to analyze the health-related habits of community health workers in Montes Claros, Minas Gerais, Brazil.
Methods
This was a cross-sectional study conducted in Montes Claros/MG, in 2018. As the sixth largest municipality in the state of Minas Gerais, with a resident population of 413,487 inhabitants, Montes Claros has a Gini index of 0.53 and 100% Family Health Strategy coverage.
The target population of this study consisted of all 797 CHWs existing in Montes Claros, working as part of the 135 the municipal Family Health Strategy teams at the time of data collection. All CHW professionals in Montes Claros were invited to participate in the study. The inclusion criterion was that they had to be effectively exercising their function as CWHs. The exclusion criteria, therefore, were not effectively exercising their function and being pregnant at the time of the study. The estimated participation of the CHW population did not require sample calculation; the statistical power of the contingent of CHW participants (β error) was tested a posteriori (post hoc test), for comparison between the groups related to the variables analyzed.
Data collection, carried out by health professionals and scientific initiation students, took place at the Montes Claros Regional Occupational Health Reference Center, on weekdays, in the morning, between August and October 2018. Administration of the questionnaire was entrusted to research collaborators and addressed sociodemographic, work, and lifestyle characteristics:
a) Sociodemographic characteristics
- Sex (female; male);
- Age group (in years: ≤40; >40);
- Schooling (elementary education/high school education; incomplete higher education; complete higher education);
- Family income (in minimum wages: BRL 954 in 2018, later categorized into <2, 2-3 and >3 minimum wages);
- Number of people in the family (up to 3; 4 or more);
- Marital status (has a partner; does not have a partner);
- Race/skin color (white; non-white);
- Academic qualifications in the area of health (yes; no);
- Religion (yes; no).
b) Labor characteristics
- Employment relationship with the institution (public sector employee; hired; consolidated labor laws; service provider);
- Has a second job (yes; no);
- Length of service in the area of Health (years of service: <1; 1-5; >5);
- Length of service as a community health worker (years of service: <1; 1-5; >5);
- Weekly workload in the Family Health Strategy (in hours: ≤40; >40).
c) Lifestyle characteristics
- Daily fruit consumption (yes; no);
- Daily greens and vegetable consumption (yes; no);
- Excess salt in food (yes; no);
- Overweight/obesity (yes; no);
- Alcohol consumption (does not consume alcoholic beverage; consumes alcoholic beverage);
- Physical inactivity (inactive or insufficiently active; active);
- Tobacco smoking: (does not smoke; smokes).
Anthropometric data on weight (kg) and height (cm) were measured individually, using BALMAK 111® mechanical portable scales with 100g precision and a SECA 206® portable stadiometer with 0.1cm precision affixed to a smooth wall. During measurement, participants were barefoot, wearing light clothing and were placed in a standing position according to the Frankfurt plane. Taking the values obtained for height and weight, body mass index (BMI) was assessed in order to identify overweight and obese cases by dividing weight (in kg) by height (in meters) squared. Based on the results found, the interviewees were classified according to the reference values established by the World Health Organization(WHO) and according to the Brazilian Obesity Guidelines: a person was considered to be underweight when their BMI was less than 18.5; normal or eutrophic, BMI between 18.5 and 24.9; overweight or pre-obese, between 25.0 and 29.9; grade 1 obesity, between 30.0 and 34.9; grade 2 obesity, between 35.0 and 39.9; and BMI greater than or equal to 40.0 characterized the CHW as having severe or grade 3 obesity.9
Food consumption was assessed using questions taken from the questionnaire used by the Chronic Disease Risk and Protective Factors Surveillance Telephone Survey (Vigitel),10 regarding the weekly frequency of consumption of fruit, raw greens/salads, and cooked vegetables (reply options: never/almost never; 1 to 2 times/week; 3 to 4 times/week; 5 to 6 times/week; every day of the week) and regarding adding extra salt to meals that had already been salted during preparation (excess salt in food: yes; no). Participants were also asked about cigarette smoking (does not smoke; smokes) and alcoholic beverage consumption (no alcoholic beverage consumption; alcoholic beverage consumption).
In order to assess physical activity practice, we used a global instrument, namely the International Physical Activity Questionnaire (IPAQ), as proposed by the WHO and validated in Brazil,11 with the objective of estimating the prevalence of physical activity/inactivity in adults. Level of physical activity was classified taking into account the duration, intensity, and frequency of these activities during the week prior to the interview, distributing participants between two categories: inactive or insufficiently active (<150 minutes per week); and active (≥150 minutes per week).
The following recommendations were considered with regard to healthy health-related habits: BMI<24.9kg/m2; not smoking; not drinking alcoholic beverages; consuming fruit daily; consuming vegetables daily; practicing physical activity regularly; and not adding more salt to meals already salted during preparation. Non-adherence to three or more of these factors defined the extent of the variable called 'inadequate health habits'.
For data analysis, we applied descriptive statistics, using simple frequencies and percentages, the results of which are presented in tables. We performed Pearson’s chi-square test to check for association between the ‘inadequate health habits’ variable and the following independent variables: sex; age; schooling; family income; number of people in the family; marital status; race/skin color; academic qualifications in the area of health; religion; employment relationship with the institution; second job; length of service in the area of Health; length of service as a CHW; and workload in the Family Health Strategy.
Variables with p-values <0.20 were selected for multiple analysis. The Poisson model with robust variance was used to estimate the magnitude of association according to the crude and adjusted prevalence ratios (PR) taking a 5% significance level. The deviance test was used to assess the quality of the model fit. All analyses were performed using SPSS version 20.0.
The study project was approved by the Research Ethics Committee of the State University of Montes Claros: Opinion No. 2,425,756, issued on December 8, 2017. An Informed Consent Form was signed by the CHWs as a precondition for data collection.
Results
Of the 797 CHWs in the municipality, 122 (15.3%) were excluded from the study due to the following: not working as a CHW; being pregnant; working for less than a year; being on maternity leave; being on sick leave (Figure 1). We interviewed 675 community health agents from Montes Claros.
Most of these professionals were female (83.9%) and their average age was calculated as 36.7 years: minimum of 19 and maximum of 68 years. 56.7% reported having complete high school education, 49.3% had family income of two to three minimum wages, 59.7% had a partner, 87.1% were of non-white race/skin color and 84.3% were religious. With regard to occupational characteristics, the majority had length of service in the area of Health (46.1%) and length of service as a CHW (43.5%) greater than 5 years, and Family Health Strategy workload above 40 hours a week (54.7%). There was a predominance of respondents who had no academic qualifications in the area of health (64.3%), those who had a hired/consolidated labor laws/service provider employment relationship with the institution (74.2%), and those who did not have a second job (90.2%) (Table 1).
Fifty-three percent of the CHW had inadequate health habits. The prevalence of each factor assessed is shown in Table 2: the most frequent factor in the population studied was low fruit consumption (83.0%), while tobacco smoking was the least common (7.1%). Alcohol consumption was reported by 37.6% of the respondents, while 26.2% reported physical inactivity. The majority had BMI outside the recommended range (60.8%). The habit of adding salt to food that had already been salted during preparation was high among these professionals (81.2% prevalence). Figure 2 shows the distribution of the participants according to the number of inappropriate behaviors they reported.
Bivariate association analysis, between inadequate health habits and independent variables, identified statistical significance up to 20% for the following variables: 'sex' (PR=1.30 - 95%CI 1.11;1.52), 'age' (PR=1.22 - 95%CI 1.04;1.43), 'incomplete higher education' (PR=1.09 - 95%CI 0.92; 1.30), 'complete higher education' (PR=0.90 - 95%CI 0.75;1.08), 'marital status' (PR=1.12 - 95%CI 0.97;1.29), 'academic qualifications in the area of health' (PR=1.19 - 1.02;1.39) and 'religion' (PR=1.26 - 1.07;1.49) (Table 3).
In the multiple model, 'sex' (PR=1.24 - 95%CI 1.05;1.45), 'age' (PR=1.19 - 95%CI 1.01;1.40) and 'religion' (PR=1.23 - 95%CI 1.04;1.45) remained associated with CHW inadequate health habits. Males had higher prevalence of inadequate health habits, as well as CHW up to 40 years old and those who reported not being religious (Table 3).
The estimates for a posteriori calculated association analysis indicated that the power of the study was 83.4%, considering 53% prevalence of inadequate health habits, with the 675 individuals assessed and a 95% confidence level.
Figure 1 - Process of selection participant community health workers, Montes Claros, Minas Gerais, Brazil, 2018
Table 1 - Main community health worker characteristics (n=675), Montes Claros, Minas Gerais, Brazil, 2018
| Characteristics | n | % | |||||
|---|---|---|---|---|---|---|---|
| Sex | |||||||
| Female | 566 | 83.9 | |||||
| Male | 109 | 16.1 | |||||
| Age group (in years) | |||||||
| ≤40 | 444 | 65.8 | |||||
| >40 | 231 | 34.2 | |||||
| Schooling | |||||||
| Elementary education/high school education | 383 | 56.7 | |||||
| Incomplete higher education | 126 | 18.7 | |||||
| Complete higher education | 166 | 24.6 | |||||
| Family income (in minimum wages)a | |||||||
| <2 | 205 | 30.4 | |||||
| 2-3 | 333 | 49.3 | |||||
| >3 | 137 | 20.3 | |||||
| Number of people in the family | |||||||
| Up to 3 | 331 | 49.0 | |||||
| 4 or more | 344 | 51.0 | |||||
| Marital status | |||||||
| Has a partner | 403 | 59.7 | |||||
| Does not have a partner | 272 | 40.3 | |||||
| Race/skin color | |||||||
| White | 87 | 12.9 | |||||
| Non-white | 588 | 87.1 | |||||
| Academic qualifications in the area of health | |||||||
| Yes | 241 | 35.7 | |||||
| No | 434 | 64.3 | |||||
| Religion | |||||||
| Yes | 568 | 84.3 | |||||
| No | 106 | 15.7 | |||||
| Employment relationship with the institution | |||||||
| Public sector employee | 174 | 25.8 | |||||
| Hired/consolidated labor laws/service provider | 501 | 74.2 | |||||
| Second job | |||||||
| No | 609 | 90.2 | |||||
| Yes | 66 | 9.8 | |||||
| Length of service in the area of Health (in years) | |||||||
| <1 | 167 | 24.7 | |||||
| 1-5 | 197 | 29.2 | |||||
| >5 | 311 | 46.1 | |||||
| Length of service as a CHWb (in years) | |||||||
| <1 | 180 | 26.7 | |||||
| 1-5 | 201 | 29.8 | |||||
| >5 | 294 | 43.5 | |||||
| Workload (hours per week) in the FHSc | |||||||
| Up to 40h | 306 | 45.3 | |||||
| Over 40h | 369 | 54.7 | |||||
a) The minimum wage was BRL 954 in 2018; b) CHW: community health worker; c) FHS: Family Health Strategy.
Table 2 - Frequency of community health worker inadequate health habits (n=675), Montes Claros, Minas Gerais, Brazil, 2018
| Inadequate health habit components | n | % |
|---|---|---|
| Low fruit consumption | 560 | 83.0 |
| Excess salt in food | 548 | 81.2 |
| Overweight/obesity | 409 | 60.8 |
| Low consumption of greens and vegetables | 392 | 58.1 |
| Alcohol consumption | 254 | 37.6 |
| Physical inactivity | 177 | 26.2 |
| Tobacco smoking | 48 | 7.1 |
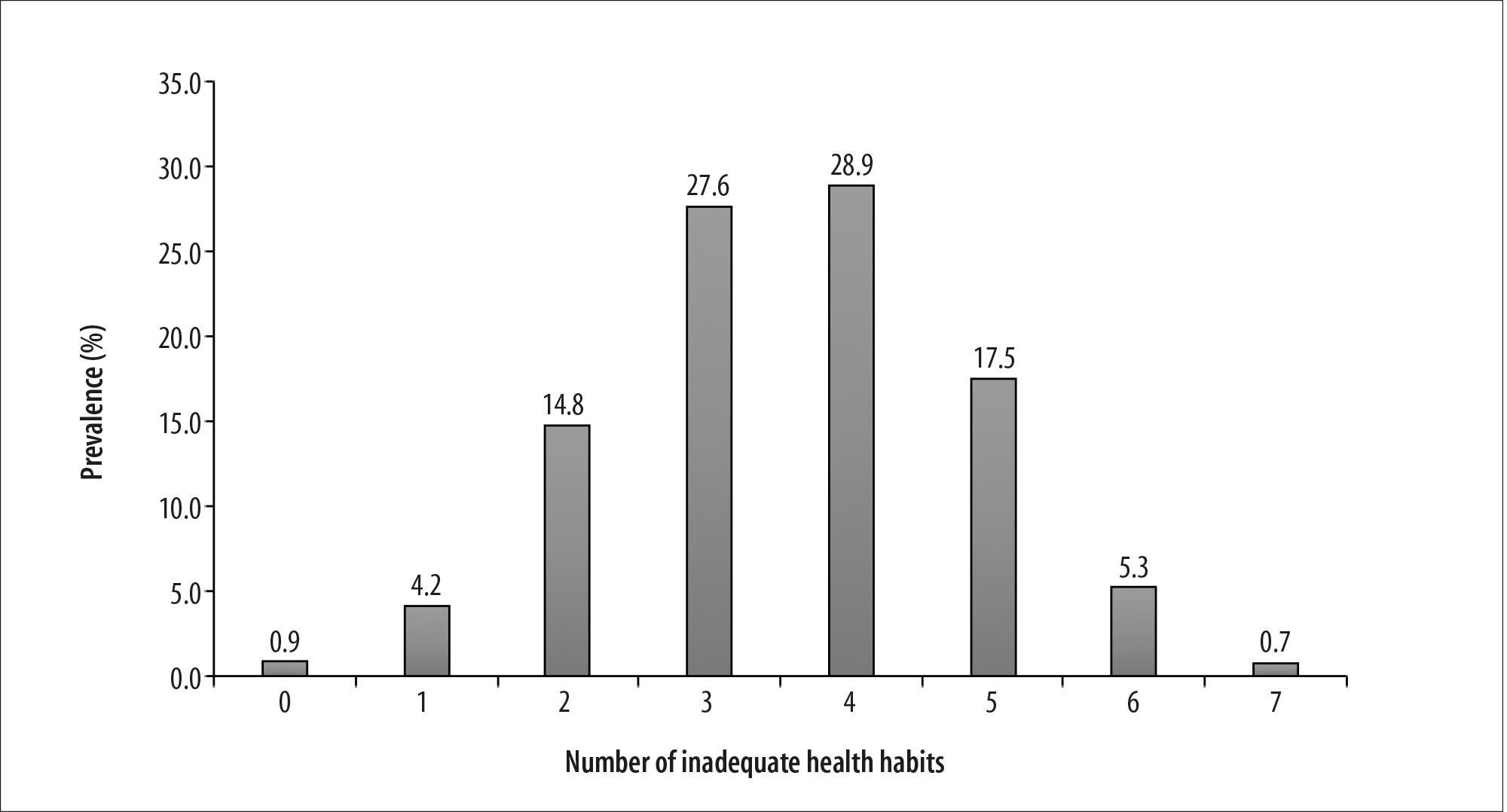
Figure 2 - Distribution of community health workers (n=675) according to number of inadequate health habit components, Montes Claros, Minas Gerais, Brazil, 2018
Table 3 - Crude and adjusted prevalence ratios of inadequate health habits according to community health worker (n=675) sociodemographic, labor and lifestyle variables, Montes Claros, Minas Gerais, Brazil, 2018
| Variables | Prevalence (%) | Crude prevalence ratio | Adjusted prevalence ratio | ||||
|---|---|---|---|---|---|---|---|
| (95%CI)a | p-valueb | (95%CI)a | p-valuec | ||||
| Sex | |||||||
| Female | 50.5 | 1.00 | 1.00 | ||||
| Male | 65.7 | 1.30 (1.11;1.52) | 0.001 | 1.24 (1.05;1.45) | 0.011 | ||
| Age (in years) | |||||||
| >40 | 46.3 | 1.00 | 1.00 | ||||
| ≤40 | 56.5 | 1.22 (1.04;1.43) | 0.016 | 1.19 (1.01;1.40) | 0.038 | ||
| Schooling | |||||||
| Fundamental/high school education | 53.4 | 1.00 | 1.00 | ||||
| Incomplete higher education | 58.4 | 1.09 (0.92;1.30) | 1.02 (0.83;1.20) | ||||
| Complete higher education | 47.9 | 0.90 (0.75;1.08) | 0.199 | 0.87 (0.72;1.05) | 0.307 | ||
| Family income (in minimum wages)d | |||||||
| <2 | 57.4 | 1.00 | - | ||||
| 2-3 | 52.0 | 0.91 (0.77;1.06) | |||||
| >3 | 48.9 | 0.85 (0.69;1.05) | 0.272 | ||||
| Number of people in the family | |||||||
| Up to 3 | 52.0 | 1.00 | - | ||||
| 4 or more | 54.0 | 1.04(0.90;1.20) | 0.610 | ||||
| Marital status | |||||||
| Has a partner(a) | 50.5 | 1.00 | 1.00 | ||||
| Does not have a partner(a) | 56.7 | 1.12 (0.97;1.29) | 0.113 | 1.07 (0.93; 1.25) | 0.309 | ||
| Race/skin color | |||||||
| White | 52.9 | 1.00 | - | ||||
| Non-white | 53.0 | 1.00 (0.81;1.24) | 0.981 | ||||
| Academic qualifications in the area of health | |||||||
| Yes | 47.3 | 1.00 | - | ||||
| No | 56.2 | 1.19 (1.02;1.39) | 0.032 | ||||
| Religion | |||||||
| Yes | 50.8 | 1.00 | 1.00 | ||||
| No | 64.2 | 1.26 (1.07;1.49) | 0.005 | 1.23 (1.04;1.45) | 0.017 | ||
| Employment relationship with the institution | |||||||
| Public sector employee | 56.0 | 1.00 | - | ||||
| Hired/consolidated labor laws/service provider | 51.7 | 0.91 (0.78;1.07) | 0.252 | ||||
| Second job | |||||||
| No | 52.8 | 1.00 | - | ||||
| Yes | 54.5 | 1.03 (0.82;1.30) | 0.787 | ||||
| Length of service in the area of Health (in years) | |||||||
| <1 | 50.0 | 1.00 | - | ||||
| 1-5 | 53.9 | 1.08 (0.88;1.32) | |||||
| >5 | 54.0 | 1.08 (0.90;1.30) | 0.672 | ||||
| Length of service as a CHWe (in years) | |||||||
| <1 | 49.2 | 1.00 | - | ||||
| 1-5 | 53.3 | 1.01 (0.89;1.32) | |||||
| >5 | 55.1 | 1.12 (0.94;1.35) | 0.449 | ||||
| Workload (hours per week) in the FHSf | |||||||
| Up to 40h | 51.5 | 1.00 | - | ||||
| Over 40h | 54.2 | 1.05 (0.91;1.22) | 0.484 | ||||
a) 95%CI: 95% confidence interval; b) p-value: probability of significance - Pearson’s chi-square test; c) p-value: probability of significance -final multiple analysis model (backward method), adjusted by the following variables: ‘sex’, ‘age’, ‘schooling’, ‘marital status’, ‘academic qualifications in the area of health’ and ‘religion’ (deviance test [p-value = 0.665]); d) The minimum wage was BRL 954 in 2018. e) CHW: community health worker; f) FHS: Family Health Strategy.
Discussion
Among the CHW professionals studied, approximately half presented inadequate health habits. Most of those surveyed had inadequate BMI, reported low fruit, vegetable, and greens consumption, and had the habit of adding salt to food that had already been salted during preparation. Approximately one third of the CHWs consumed alcohol and about one quarter were physically inactive. Smoking was reported by a minority of respondents. Presence of inadequate health habits was associated with being male, being under 40 years old, and not being religious. Such habits can interfere negatively in the quality of life of these health professionals.12
A limitation of this study is the use questionnaires answered based on CHW self-assessment. Since these are individuals working in the health area, it is questionable whether, at some point, there may have been omission of habits recognized by Public Health as harmful to health. Self-reported CHW answers may underestimate the real prevalence of inadequate health habits and, therefore, represent a source of bias in the interpretation of the study results.
Inadequate CWH health habits in this study are in line with previous research on the Brazilian scenario, where CHWs did not adequately follow health promotion guidelines in their own behaviors.8),(13 It is essential that health professionals adopt healthy behaviors in order to convince their patients about the risk of NCDs, reduce that risk, and promote well-being among them.13 Health service managers, in turn, can also contribute to the adoption of these practices, by providing moments of reflection and knowledge about self-care and healthy lifestyle habits, such as physical activity and encouraging healthy eating in the work environment of their administrative unit or body.
In this study, prevalence of inadequate BMI corresponded to more than half of the CHWs. A similar result was found in a previous study conducted in 2011 with CHWs from all over the country: 48.5% of these professionals were overweight and 14.2% were obese.4 According to data collected by the Vigitel survey10 in 2016, 53.8% of adults in the 27 capitals of the Brazilian Federative Units were overweight.
The frequency of smokers among those surveyed - 9.3% - was below the national average identified by Vigitel in 2018, although it was similar to that seen in a nationwide survey which found that 7.4% of CHW were smokers.13 This finding is important, since tobacco smoking is the main determinant of lung cancer, among other diseases and health conditions,14 and Brazil is a world reference when it comes to policies to combat this practice.15
Use of alcoholic beverages was reported by more than a third of the CHWs surveyed. Worldwide, there are currently estimated to be 2.3 billion alcohol consumers.16 Although alcoholic beverages are legalized and accepted in society, there is a great potential for psychological and physical dependence on this substance, which is the cause of great personal and social harm. Its harmful use is a factor that contributes to several diseases and lesions, strongly associated with mental and behavioral disorders, in addition to NCDs.16
Daily fruit consumption was low among CHW. A similar result was found by a study conducted in Primary Healthcare Centers (PHC) in Brazil in 2011: of 798 PHC health professionals surveyed, 269 of whom were CHW, only 26.2% consumed five or more servings of fruit and/or vegetables per week;13 the study also found low daily consumption of vegetables in more than half of the participants. The WHO recommends consumption of five or more servings of fruits and vegetables daily, implying a greater supply of micronutrients and fiber.17
The habit of adding salt to food already salted during preparation was reported by most CHWs. The WHO recommendation, again, is intake of up to 5g/day of salt; therefore, adding salt to the previously salted food increases the chances that, by exceeding the maximum amount indicated for salt, it becomes a risk factor for noncommunicable chronic diseases.17 A national survey found that the population consumes salt in excessive amounts. Considering the risks of high salt consumption for hypertension and impaired kidney function, it is necessary to adopt wide-reaching public policies to reduce the intake of this ingredient.18)
Around a quarter of the CHWs were physically inactive, while those who reported moderate physical activity were predominant. Research conducted in the Brazil in 2011,4 found that 64.9% of CHW practiced regular physical activity. This data may be related to the fact that some of the CHWs' work activities, dependent on physical displacement essential for home visits over the extension of their work territory, are considered physical activity practices, as per the International Physical Activity Questionnaire (IPAQ) that served as reference for this study.11
Inadequate health habits were associated with the male sex. According to a survey conducted between May and July 2012, when assessing the profile of SUS health professionals in the city of Pelotas/RS, the conclusion was reached that females show better results regarding taking care of their own health.8 In this sense, a study conducted in Southern Brazil from January to July 2013, exclusively with men in the 40-50 year age group, found high prevalence of some health risk behaviors among them.19 One of the stereotypes related to masculinity defines the male sex as 'stronger and invulnerable' compared to females, which can make it difficult for men to adopt self-care measures and seek health services.
Being up to 40 years old was associated with the outcome variable. Similarly, a previous study with data from the 2013 National Health Survey on the multidimensional profiles of lifestyle-related risk factors in adult individuals found association between lifestyle-related factors and national sociodemographic characteristics. Practicing healthy behaviors varies according to 'age group', and is higher among older people.20
It has been found that the most affected population identifies with categories usually associated with poor self-care, despite the fact that the media and other means of communication have recently emphasized health care as a trend in general society.21 The challenge of changing behaviors is universal, and it is important to emphasize, especially for health professionals, their role as role models and examples to be followed, sharing responsibilities with the people they assist and guide.
Inadequate health habits were more prevalent among CHW who stated that they were not religious. A study conducted in Israel22 and published in 2016 concluded that individuals with higher spirituality/religion had lower disease prevalence due to greater health care. A survey of users of Primary Healthcare Centers in Ribeirão Preto/SP, published in 2019, detected low levels of alcohol intake among religious individuals and/or practitioners of a religion.23 Notwithstanding recent studies addressing the influence of religion and spirituality on healthcare, the topic still lacks further investigation.
In this study, the presence of unhealthy habits among CHWs indicates the need to value these professionals from a holistic perspective. One of the measures in this sense would be the implementation of actions to promote and protect their health, contributing to lower incidence of diseases and absence from their work context. Consequently, the service provided to the community is improved, because with adequate health indices, it is possible to act more effectively and earlier in the identification of problems, supporting the monitoring of chronic diseases and reducing the use of acute and secondary care services by the community. This also impacts on the reduction of unnecessary workload for the health team.
Another way to address the issue is to recognize the role of CHWs in the health team, highlighting the relevance of their activities with the community and creating opportunities for improvement and professional growth. The incentive to train CHWs, focusing on the principles of the SUS, is important for them to perform their work according to SUS guidelines and to collaborate with their consolidation,24) restructuring current models found in health services and strengthening of Primary Health Care as the coordinating core of the health care network.25
Finally, it is worth highlighting the exemplary role of CHWs as facilitators of communication between health services, individuals and the community. As bearers of a community identity, their tasks are not restricted to the limits of the health service as an institution, but extend to the living and working territory of the citizens they are intended to assist. This is the strength and richness of the presence of these social actors in a Family Health team.26
Inadequate health habits were common among community health workers in Montes Claros, being more prevalent among males, younger people and among non-religious people. Therefore, it is necessary to emphasize the importance of measures that aim to promote changes in lifestyle, especially among these groups, in order to reduce the incidence of non-communicable diseases and complications arising from them.
REFERENCES
1. Ministério da Saúde (BR). Portaria nº 2.436, de 21 de setembro de 2017. Aprova a Política Nacional de Atenção Básica, estabelecendo a revisão de diretrizes para a organização da Atenção Básica, no âmbito do Sistema Único de Saúde. Brasília, DF: Diário Oficial da União; 22 set. 2017; 68: (Seção 1). [ Links ]
2. Hayhoe B, Cowling TE, Pillutla V, Garg P, Majeed A, Harris M. Integrating a nationally scaled workforce of community health workers in primary care: a modelling study. JR Soc Med. 2018;111(12): 453-61. doi: http://doi.org/10.1177/0141076818803443. [ Links ]
3. Malta DC, Oliveira TP, Santos MAS, Andrade SSCA, Silva MMA. Avanços do Plano de Ações Estratégicas para o Enfrentamento das Doenças Crônicas não Transmissíveis no Brasil, 2011-2015. Epidemiol Serv Saude. 2016;25(2):373-90. https://doi.org/10.5123/s1679-49742016000200016. [ Links ]
4. Florindo AA, Brownson RC, Mielke GI, Gomes GA, Parra DC, Siqueira FV, et al. Association of knowledge, preventive counseling and personal health behaviors on physical activity and consumption of fruits or vegetables in community health workers Health behavior, health promotion and society. BMC Public Health. 2015 Apr 9;15:344. doi: http://doi.org/10.1186/s12889-015-1643-3. [ Links ]
5. Alonso CMC, Béguin PD, Duarte FJCM. Work of community health agents in the Family Health Strategy: meta-synthesis. Rev Saude Publica. 2018;52:14. doi: http://dx.doi.org/10.11606/s1518-8787.2018052000395. [ Links ]
6. Siqueira FV, Reis DS, Souza RAL, Pinho S, Pinho L. Excesso de peso e fatores associados entre profissionais de saúde da Estratégia Saúde da Família. Cad Saude Colet. 2019;27(2):138-45. doi: http://dx.doi.org/10.1590/1414-462x201900020167. [ Links ]
7. Frank E, Dresner Y, Shani M, Vinker S. The association between physicians' and patients' preventive health practices. CMAJ. 2013 May 14;185(8):649-53. doi: http://dx.doi.org/10.1503/cmaj.121028. [ Links ]
8. Pretto ADB, Pastore CA, Assunção MCF. Comportamentos relacionados à saúde entre profissionais de ambulatórios do Sistema Único de Saúde no município de Pelotas-RS. Epidemiol Serv Saude. 2014;23(4):635-44. doi: https://doi.org/10.5123/S1679-49742014000400005. [ Links ]
9. Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica Diretrizes brasileiras de obesidade. 4.ed. São Paulo: ABESO, 2016. [ Links ]
10. Ministério da Saúde (BR). Vigitel Brasil 2016: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2016. Brasília, DF: MS; 2017. [ Links ]
11. Matsudo SM, Araújo T, Matsudo VR, Andrade D, Andrade E, Oliveira LC, et al. Questionário Internacional de Atividade Física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fis Saude. 2001;6(2):5-18. doi: https://doi.org/10.12820/rbafs.v.6n2p5-18. [ Links ]
12. Teles MAB, Barbosa MR, Vargas AMD, Gomes VE, Ferreira EF, Martins AMEBL, et al. Psychosocial work conditions and quality of life among primary health care employees: a cross sectional study. Health Qual Life Outcomes. 2014 May 15;12:72. doi: https://doi.org/10.1186/1477-7525-12-72. [ Links ]
13. Hidalgo KD, Mielke GI, Parra DC, Lobelo F, Simões EJ, Gomes GO, et al. Health promoting practices and personal lifestyle behaviors of Brazilian health professionals. BMC Public Health. 2016 Oct 24;16(1):1114. doi:https://doi.org/10.1186/s12889-016-3778-2. [ Links ]
14. Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the National Institutes of Health-AARP diet and health study. JAMA Intern Med. 2017 Jan 1;177(1):87-95. doi: http://doi.org10.1001/jamainternmed.2016.7511. [ Links ]
15. Franceschini JP, Santoro IL. Estadiamento do câncer de pulmão: uma visão epidemiológica brasileira. J Bras Pneumol. 2020;46(1):e20190412. doi: http://doi.org/10.1590/1806-3713/e20190412. [ Links ]
16. Organização Pan-Americana da Saúde. Álcool [Internet]. Folha Informativa. Brasília, DF: OPAS; 2019 [citado 2 mar 2020]. Disponível em Disponível em https://www.paho.org/bra/index.php?option=com_content&view=article&id=5649:folha-informativa-alcool&Itemid=1093 [ Links ]
17. World Health Organization. Regional Office for the Eastern Mediterranean. Healthy diet. Genebra: WHO; 2019. [ Links ]
18. Mill JG, Malta DC, Machado IE, Pate A, Pereira CA, Jaime PC, et al. Estimativa do consumo de sal pela população brasileira: resultado da Pesquisa Nacional de Saúde 2013. Rev Bras Epidemiol. 2019;22(Supp2 l ):e190009.SUPL.2. doi: http://dx.doi.org/10.1590/1980-549720190009.supl.2. [ Links ]
19. Arruda GO, Marcon SS. Comportamentos de riscos à saúde de homens da região sul do Brasil. Texto Contexto Enferm. 2018;27(2):e2640014. doi: http://dx.doi.org/10.590/0104-07072018002640014. [ Links ]
20. Pereira IFS, Gonzaga MR, Lyra CO. Indicador multidimensional de fatores de risco relacionados ao estilo de vida: aplicação do método grade of membership. Cad Saude Publica. 2019;35(6):e00124718. doi: http://dx.doi.org/10.590/0102-311x00124718. [ Links ]
21. Profis M, Simon-Tuval T. The influence of healthcare workers' occupation on Health Promoting Lifestyle Profile. Ind Health. 2016;54(5):439-447. doi:10.2486/indhealth.2015-0187. [ Links ]
22. Lucchetti G, Lucchetti ALG, Avezum Jr A. Religiosidade, Espiritualidade e Doenças Cardiovasculares. Rev Bras Cardiol. 2011;24(1):55-7. [ Links ]
23. Martinez EZ, Silva AS, Giglio FM, Terada NAY, Zucoloto ML. Religiosity and patterns of alcohol consumption among users of primary healthcare facilities in Brazil. Cad Saude Colet. 2019;27(2):146-57. doi: http://doi.org/10.1590/1414-462x201900020234. [ Links ]
24. Gomes KO, Cotta RMM, Cherchiglia ML, Mitre SM, Batista RS. A práxis do agente comunitário de saúde no contexto do programa saúde da família: reflexões estratégicas. Saude Soc. 2009;18(4):744-55. doi: http://doi.org/10.1590/S0104-12902009000400017. [ Links ]
25. Baralhas M, Pereira MAO. Prática diária dos agentes comunitários de saúde: dificuldades e limitações da assistência. Rev Bras Enferm. 2013;66(3):358-65. doi: http://doi.org/10.1590/S0034-71672013000300009. [ Links ]
26. Nunes MO, Trad LB, Almeida BA, Homem CR, Melo MCIC. O agente comunitário de saúde: construção da identidade desse personagem híbrido e polifônico. Cad Saude Publica. 2002;18(6):1639-46. doi: http://doi.org/10.1590/S0102-311X2002000600018. [ Links ]
Received: November 11, 2020; Accepted: January 15, 2021











 texto em
texto em 


