Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.4 Brasília dic. 2021 Epub 08-Oct-2021
http://dx.doi.org/10.1590/s1679-49742021000400006
ORIGINAL ARTICLE
Trend in cases of gestational and congenital syphilis in Minas Gerais, Brazil, 2009-2019: an ecological study
1NOVA Faculdade, Curso de Enfermagem, Contagem, MG, Brazil
2Universidade Federal de Minas Gerais, Departamento de Enfermagem Materno-Infantil e Saúde Pública, Belo Horizonte, MG, Brazil
3Universidade Federal de Minas Gerais, Programa de Pós-Graduação em Ciências da Saúde, Belo Horizonte, MG, Brazil
Objective:
To analyze the trend of notifications of gestational and congenital syphilis in Minas Gerais, Brazil, from 2009 to 2019.
Methods:
This was an ecological time series study which took the state of Minas Gerais as its unit of analysis, based on data reported on the Notifiable Health Conditions Information System (SINAN). The Prais-Winsten autoregressive model was used to verify trends.
Results:
20,348 cases of gestational syphilis and 11,173 cases of congenital syphilis were reported. Average percentage annual increase was 36.7% (95%CI 32.5;41.0), for gestational syphilis incidence rates, and 32.8% (95%CI 28.0;37.8) for congenital syphilis incidence rates (p<0.001).
Conclusion:
The temporal trend analysis showed that gestational and congenital syphilis incidence rates had significant increasing trends, which may be related to inadequate treatment or failure to treat syphilis during pregnancy.
Keywords: Syphilis; Congenital Syphilis; Pregnant Women; Epidemiological Monitoring; Sexually Transmitted Diseases; Time Series Studies.
Introduction
Sexually transmitted infections are a serious global public health problem which generates economic, social and health impacts.1) Global estimates show that approximately 2 million gestational syphilis cases occur worldwide annually,2 and if infected women are not treated, or inadequately treated, there is a 50% likelihood of their transmitting it to their child during pregnancy.3),(4
In 2016, the estimated global prevalence of gestational syphilis was 0.7%, while for the region of the Americas it was 0.9%. High prevalence of gestational syphilis resulted in a congenital syphilis incidence rate of 473 cases per 100,000 live births worldwide.2
In 2020, in Brazil, 61,127 gestational syphilis cases were reported on the Notifiable Health Conditions Information System (SINAN), with a detection rate of 20.8 cases per 1,000 live births.5 The congenital syphilis incidence rate was 8.2 per 1,000 live births, while the congenital syphilis mortality rate was 5.9 deaths per 1,000 live births in Brazil as a whole.5 It is noteworthy that the congenital syphilis incidence rate in the state of Minas Gerais was higher than the national rate (8.7 cases per 1,000 live births).5
Prevention of vertical transmission of syphilis is relatively simple, by means of rapid screening tests and serological tests during prenatal care and immediate treatment with injected benzathine penicillin. The newborn child of a syphilis-infected and adequately treated pregnant woman is not, in principle, considered to be a suspected case of congenital syphilis.6 Congenital syphilis is a disease with high prevention potential; however, for prevention to be effective, infected pregnant women and their sex partners need to be diagnosed and treated during prenatal care.7
When vertical transmission of syphilis occurs during pregnancy, infection can lead to serious fetal outcomes during gestation,8 such as miscarriage, early fetal death, stillbirth, neonatal death, premature birth, low birth weight, and congenital syphilis.8 When syphilis affects pregnant women, prevalence of congenital syphilis is alarming, especially in low- and middle-income countries.8 In this context, Primary Health Care is an essential and strategic point of care in the fight against gestational and congenital syphilis, since it is the health service’s first level of care for pregnant women.9 Through the longitudinal care it offers, Primary Health Care enables bonds to be formed between the health service and pregnant women, besides making it possible to change the epidemiological picture of gestational syphilis and congenital syphilis.9
Given this scenario, there is a need for a better understanding of the epidemiological profile of gestational syphilis and congenital syphilis in Minas Gerais, since studies based on data for that state are still incipient in the literature10),(11 and often only focus on specific cities,3),(11) such as its capital Belo Horizonte.3 In addition, analyzing trends of gestational syphilis and congenital syphilis cases in Minas Gerais can contribute to better knowledge of the problem, with the aim of improving prevention of vertical transmission. Trend analysis can support the development of strategies for achieving the goal set by the World Health Organization (WHO) to reduce occurrence of congenital syphilis to less than 50 cases per 100,000 live births by 2030 in 80% of member countries.12
The objective of this study was to analyze the trend of notifications of gestational and congenital syphilis in the state of Minas Gerais, Brazil, from 2009 to 2019.
Methods
This was an ecological time series study of gestational syphilis e congenital syphilis cases notified on the SINAN system between 2009 and 2019, taking the state of Minas Gerais as the unit of analysis.
Minas Gerais is comprised of 853 municipalities spread over 586,528 km2. In 2019 it had population of 21,168,791 inhabitants and is Brazil’s second most populous state.13),(14 The Minas Gerais Health Regionalization Master Plan divides the state into 14 health macro-regions, with the objective of organizing and planning health care in their respective areas of coverage.15
The data on gestational syphilis and congenital syphilis cases were obtained via the Information Technology Department of the Brazilian National Health System (DATASUS) and tabulated using TABNET, a public domain Ministry of Health tabulator, which allows data to be tabulated and cross-checked in a fast and safe way.16
The data obtained from DATASUS were retrieved from the website http://indicadoressifilis.aids.gov.br/,17 applying a filter for state-level data and using the subcategory ‘state of Minas Gerais’. The data were exported from DATASUS, via TABNET, on October 14th 2020.
The indicators analyzed were the Minas Gerais gestational syphilis and congenital syphilis incidence rates. However, it should be noted that gestational syphilis and congenital syphilis incidence rates for 2019 were not included as they were not yet available at the website where this information is held, i.e. http://indicadoressifilis.aids.gov.br/.17 The method used by the SINAN system to calculate incidence rates is described below:
a) To calculate the gestational syphilis incidence rate, the number of cases notified or confirmed in pregnant women in Minas Gerais is divided by the number of live births in the state and then multiplied by 1,000.
b) To calculate the congenital syphilis incidence rate, SINAN takes the number of new cases of congenital syphilis in Minas Gerais per year, divided by the number of live births in the state in the same year and then multiplied by 1,000.
We also analyzed the variables related to the information provided on the gestational syphilis and congenital syphilis notification forms, by means of absolute and relative frequencies of case notifications in Minas Gerais, according to their characteristics and categories. It should be noted that the ‘missing’ category was included in the ‘unknown’ category of each variable. The following variables were analyzed:
a) Sociodemographic characteristics
- Maternal age range (in years: 10-14; 15-19; 20-29; 30-39; 40 or over);
- Child’s age (less than 7 days; 7-27 days; 28-364 days; 1 year; 2-4 years; 5-12 years);
- Maternal schooling (illiterate; 1st to 4th grade incomplete; 4th grade complete; 5th to 8th grade incomplete; complete elementary education; incomplete high school education; complete high school education; incomplete higher education; complete higher education; unknown); and
- Maternal race/skin color (white; black; yellow; brown; indigenous; unknown).
b) Clinical characteristics
- Clinical classification of gestational syphilis (primary syphilis; secondary syphilis; tertiary syphilis; latent syphilis; unknown);
- Gestational age at diagnosis (1st trimester; 2nd trimester; 3rd trimester; unknown);
- Time at which maternal syphilis diagnosed (during prenatal period; at childbirth/curettage; after childbirth; not performed; unknown);
- Maternal treatment regimen (adequate; inadequate; not performed; unknown);
- Sex partner treated (yes; no; unknown).
The Stata Statistical Software package, version 16.0, was used to analyze the data. The variables regarding gestational and congenital syphilis were presented in terms of absolute and relative frequencies (percentages).
Trends were analyzed using autoregressive Prais-Winsten models, in which the dependent variables were the incidence rates and the proportions of the sociodemographic and clinical characteristics of gestational syphilis and congenital syphilis. The independent variables were the years covered by the study (2009-2019). We used the Prais-Winsten regression model because it is indicated for correcting serial autocorrelation arising from time series.18
To perform the Prais-Winsten regression, the incidence rates and proportions of gestational and congenital syphilis were expressed on the logarithmic scale. This process is performed to reduce the heterogeneity of the variance of the residuals arising from time series regression analysis.18
We also calculated average annual percent change (APC) for each dependent variable analyzed. The following formula was used to calculate APC: APC = (-1+10[b1]*100%), where b1 refers to the angular coefficient (beta) of the Prais-Winsten regression.18
We also calculated the 95% confidence intervals (95%CI) for the APC measurements by using the following formula: minimum 95%CI (-1+10 [b1-t*e]*100%) and maximum 95%CI (-1+10 [b1+t*e]*100%). The values of the angular coefficients (b1) of the Prais-Winsten regression and standard errors were generated by the statistical analysis software. The letter t in the formula refers to Student’s t test, which corresponded to 9 degrees of freedom (t=2.262 for the ten-year period) and 10 degrees of freedom for the remaining proportions of gestational and congenital syphilis (t=2.228 for the eleven-year period), both with a 95% confidence interval.
The regression results were interpreted as follows: rising trend, when the p-value was less than 0.05 and the regression coefficient was positive; falling trend, when the p-value was less than 0.05 and the regression coefficient was negative; or stationary trend, when the p-value was greater than 0.05.18
As we used non-nominal public data provided by DATASUS, the study project did not require approval by a Research Ethics Committee.
Results
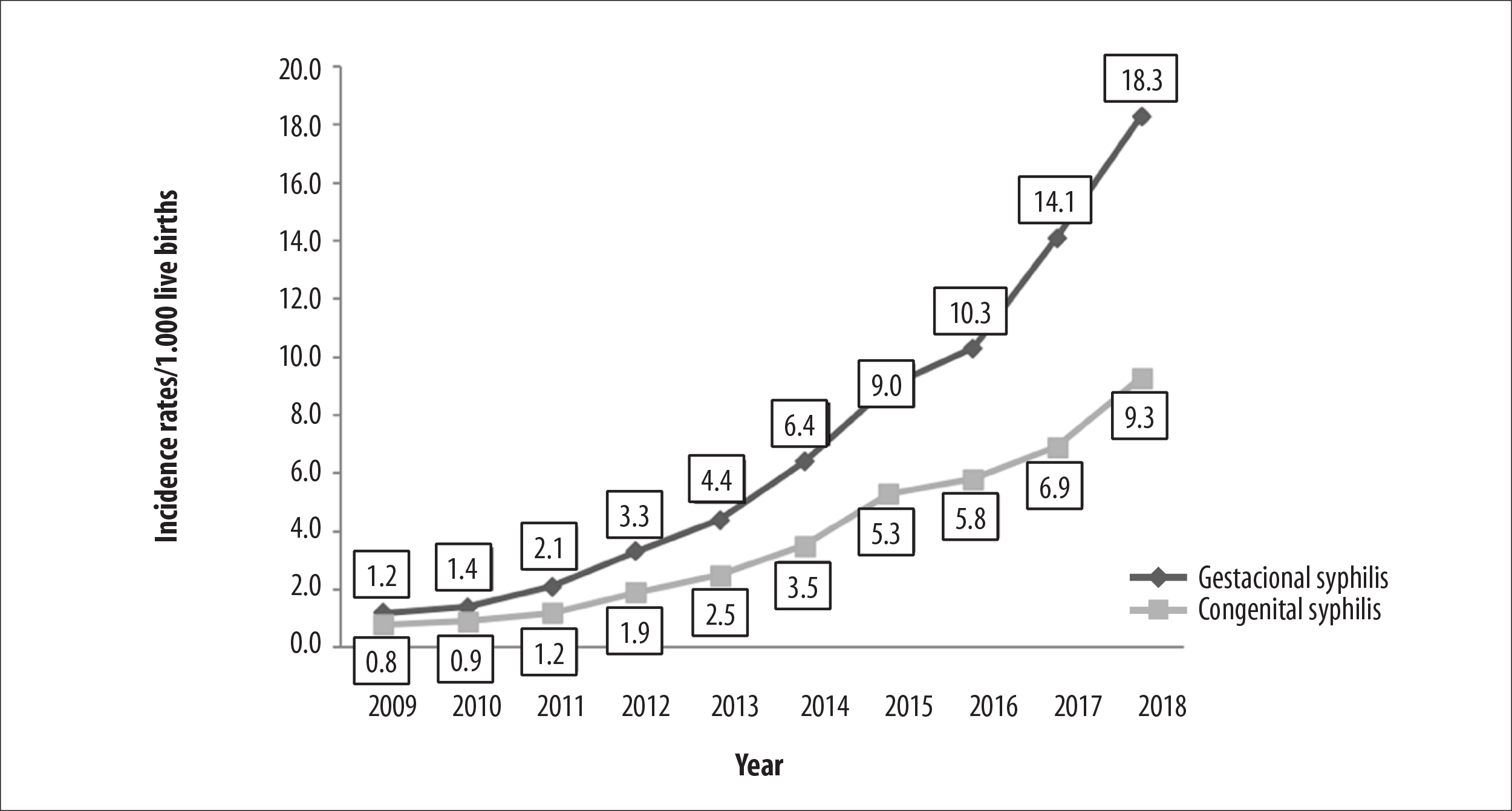
Between 2009 and 2019, 20,348 gestational syphilis cases 11,173 congenital syphilis cases were identified in Minas Gerais. Between 2009 and 2018 there was a statistically significant increase in gestational syphilis incidence rates (APC=36.7 - 95%CI 32.5;41.0) and congenital syphilis incidence rates (APC=32.8 - 95%CI 28.0;37.8) in the state (Figure 1).
It can be seen in Table 1 that 52.9% (n=10,754) of the reported cases of gestational syphilis were women aged 20 to 29 years. With regard to educational level, 16.7% (n=3,404) of the pregnant women had incomplete 5th to 8th grade education, while level of schooling was unknown for 38.6% (n=7,855). Regarding race/skin color, 48.0% (n=9,760) self-reported having brown skin color.
Among the notified congenital syphilis cases, 95.9% (n=10,718) were babies under seven days old, 52.2% (n=5,834) were born to mothers aged between 20 and 29 years, and 16.3% (n=1,816) of mothers had incomplete 5th to 8th grade education. Similarly to gestational syphilis, level of schooling was unknown for the mothers of 41.2% (n=4,599) of congenital syphilis cases (Table 1).
Regarding the clinical characteristics of gestational syphilis and congenital syphilis infections, we found that 33.8% (n=6,869) of gestational syphilis cases were primary syphilis; however, information for 35.3% (n=7,178) of cases was missing. 39.4% (n=8,020) of the women were diagnosed as having gestational syphilis during the 3rd trimester of pregnancy. The clinical characteristics of congenital syphilis showed that 62.8% (n=7,015) of maternal diagnosis occurred during the prenatal period and that 59.6% (n=6,664) of the mothers had inadequate syphilis treatment; in 61.0% (n=6,820) of cases, the sex partners of the mothers of the newborn babies were not treated (Table 2).
Table 3 shows the proportions of gestational syphilis and congenital syphilis according to sociodemographic and clinical variables, by year of notification. It can be seen that both for gestational syphilis and congenital syphilis, 2018 was the year in which Minas Gerais had the highest number of notified cases. According to the sociodemographic characteristics, pregnant women in the 20-29 age group had the highest proportion of cases, compared to the other age groups, in all the years studied. Regarding clinical characteristics, gestational syphilis cases diagnosed in the 3rd trimester showed the highest proportions for all the years studied. Regarding clinical classification at the time gestational syphilis was diagnosed, up until 2016 the unknown category accounted for the highest proportions; in the years that followed, the highest proportions were found for gestational syphilis cases clinically classified as primary syphilis. With regard to congenital syphilis cases, over the ten years of the study the highest proportions related to mothers who had follow-up during prenatal period and those for whom maternal treatment was considered to be inadequate (Table 3).
Table 1 - Absolute and percentage distribution of the sociodemographic characteristics of gestational and congenital syphilis cases, Minas Gerais, Brazil, 2009-2019
| Sociodemographic characteristics | n | % | |
|---|---|---|---|
| Gestational syphilis | |||
| Maternal age (years) (n=20,347) | |||
| 10-14 | 229 | 1.1 | |
| 15-19 | 5,197 | 25.5 | |
| 20-29 | 10,754 | 52.9 | |
| 30-39 | 3,779 | 18.6 | |
| ≥40 | 388 | 1.9 | |
| Schooling (n=20,347) | |||
| Illiterate | 68 | 0.3 | |
| 1st to 4th grade incomplete | 593 | 2.9 | |
| 4th grade complete | 551 | 2.7 | |
| 5th to 8th grade incomplete | 3,404 | 16.7 | |
| Complete elementary education | 1,965 | 9.7 | |
| Incomplete high school education | 2,527 | 12.4 | |
| Complete high school education | 3,027 | 14.9 | |
| Incomplete higher education | 196 | 1.0 | |
| Complete higher education | 161 | 0.8 | |
| Unknowna | 7,855 | 38.6 | |
| Race/skin color (n=20,348) | |||
| White | 4,820 | 23.7 | |
| Black | 3,229 | 15.9 | |
| Yellow | 224 | 1.1 | |
| Brown | 9,760 | 48.0 | |
| Indigenous | 25 | 0.1 | |
| Unknowna | 2,290 | 11.2 | |
| Congenital syphilis | |||
| Child’s age (n=11,173) | |||
| Less than 7 days | 10,718 | 95.9 | |
| 7-27 days | 192 | 1.7 | |
| 28-364 days | 210 | 1.9 | |
| 1 year | 27 | 0.2 | |
| 2-4 years | 15 | 0.1 | |
| 5-12 years | 11 | 0.1 | |
| Maternal age (years) (n=11,173) | |||
| 10-14 | 90 | 0.8 | |
| 15-19 | 2,635 | 23.6 | |
| 20-29 | 5,834 | 52.2 | |
| 30-39 | 2,196 | 19.7 | |
| ≥4 | 223 | 2.0 | |
| Unknowna | 195 | 1.7 | |
| Maternal schooling (n=11,173) | |||
| Illiterate | 60 | 0.5 | |
| 1st to 4th grade incomplete | 340 | 3.0 | |
| 4th grade complete | 238 | 2.1 | |
| 5th to 8th grade incomplete | 1,816 | 16.3 | |
| Complete elementary education | 1,174 | 10.5 | |
| Incomplete high school education | 1,169 | 10.5 | |
| Complete high school education | 1,525 | 13.6 | |
| Incomplete higher education | 88 | 0.8 | |
| Complete higher education | 78 | 0.7 | |
| Not applicable | 86 | 0.8 | |
| Unknowna | 4,599 | 41.2 | |
| Maternal race/skin color (n=11,173) | |||
| White | 2,042 | 18.3 | |
| Black | 1,511 | 13.5 | |
| Yellow | 68 | 0.6 | |
| Brown | 5,933 | 53.1 | |
| Indigenous | 16 | 0.1 | |
| Unknowna | 1,603 | 14.3 | |
a) The ‘missing’ category was included in the ‘unknown’ category of each variable.
Table 2 - Absolute and percentage distribution of the clinical detection characteristics of gestational and congenital syphilis, Minas Gerais, Brazil, 2009-2019
| Clinical characteristics | n | % | |
|---|---|---|---|
| Gestational syphilis (n=20,348) | |||
| Clinical classification | |||
| Primary syphilis | 6,869 | 33.8 | |
| Secondary syphilis | 1,441 | 7.1 | |
| Tertiary syphilis | 1,184 | 5.8 | |
| Latent syphilis | 3,676 | 18.1 | |
| Unknowna | 7,178 | 35.3 | |
| Gestational age | |||
| 1st trimester | 5,628 | 27.7 | |
| 2nd trimester | 5,146 | 25.3 | |
| 3rd trimester | 8,020 | 39.4 | |
| Unknowna | 1,554 | 7.6 | |
| Congenital syphilis (n=11,173) | |||
| Time at which maternal syphilis diagnosed | |||
| During prenatal period | 7,015 | 62.8 | |
| Congenital syphilis (n=11,173) | |||
| Time at which maternal syphilis diagnosed | |||
| At childbirth/curettage | 2,893 | 25.9 | |
| After childbirth | 840 | 7.5 | |
| Not performed | 75 | 0.7 | |
| Unknowna | 350 | 3.1 | |
| Maternal treatment regimen | |||
| Adequate | 601 | 5.4 | |
| Inadequate | 6,664 | 59.6 | |
| Not performed | 2,721 | 24.4 | |
| Unknowna | 1,187 | 10.6 | |
| Sex partner treated | |||
| Yes | 2,030 | 18.2 | |
| No | 6,820 | 61.0 | |
| Unknowna | 2,323 | 20.8 | |
a) The ‘missing’ category was included in the ‘unknown’ category of each variable.
Table 3 - Proportion of gestational and congenital syphilis according to sociodemographic and clinical variables by year of notification, Minas Gerais, Brazil, 2009-2019
| Year | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic and clinical variables | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
| Gestational syphilis cases | n=306 | n=362 | n=550 | n=871 | n=1,138 | n=1,698 | n=2,410 | n=2,605 | n=3,667 | n=4,851 | n=1,890 | |
| Gestational syphilis cases according to period in which syphilis was diagnosed | ||||||||||||
| 1st trimester | 15.7 | 16.6 | 20.2 | 22.2 | 23.2 | 22.0 | 22.2 | 25.2 | 31.3 | 33.0 | 33.9 | |
| 2nd trimester | 28.4 | 31.5 | 31.1 | 28.1 | 26.8 | 24.7 | 25.0 | 25.9 | 25.1 | 22.9 | 26.0 | |
| 3rd trimester | 46.7 | 45.8 | 39.6 | 41.8 | 40.9 | 43.1 | 43.5 | 40.9 | 37.3 | 37.0 | 34.9 | |
| Unknowna | 9.2 | 6.1 | 9.1 | 7.9 | 9.1 | 10.2 | 9.3 | 8.0 | 6.3 | 7.1 | 5.2 | |
| Gestational syphilis cases by pregnant women’s age range (years) at the time syphilis was diagnosed | ||||||||||||
| 10-14 | 0.3 | 1.1 | 1.8 | 1.0 | 1.5 | 1.6 | 1.2 | 1.3 | 0.9 | 1.0 | 1.0 | |
| 15-19 | 21.9 | 19.6 | 23.3 | 23.1 | 26.3 | 28.6 | 26.2 | 25.2 | 27.3 | 25.0 | 23.3 | |
| 20-29 | 55.6 | 56.1 | 49.1 | 46.4 | 51.9 | 49.1 | 51.7 | 53.9 | 52.8 | 54.4 | 56.2 | |
| 30-39 | 18.6 | 21.3 | 21.5 | 27.3 | 18.8 | 18.8 | 19.1 | 18.2 | 17.0 | 17.8 | 17.5 | |
| ≥40 | 3.6 | 1.9 | 4.3 | 2.2 | 1.5 | 1.9 | 1.8 | 1.5 | 2.0 | 1.8 | 2.0 | |
| Gestational syphilis cases according to clinical classification of gestational syphilis at the time syphilis was diagnosed | ||||||||||||
| Primary syphilis | 36.8 | 33.4 | 34.2 | 29.6 | 32.3 | 37.3 | 34.1 | 31.9 | 35.3 | 33.9 | 31.4 | |
| Secondary syphilis | 8.3 | 6.9 | 9.3 | 8.5 | 6.9 | 6.5 | 7.8 | 9.2 | 7.2 | 5.7 | 5.6 | |
| Tertiary syphilis | 3.5 | 3.6 | 4.4 | 4.9 | 5.5 | 6.1 | 5.5 | 5.4 | 6.0 | 6.4 | 6.6 | |
| Latent syphilis | 8.0 | 11.9 | 10.9 | 8.8 | 7.0 | 9.0 | 10.7 | 14.6 | 20.8 | 25.7 | 31.1 | |
| Unknowna | 43.3 | 44.2 | 41.2 | 48.2 | 48.3 | 41.1 | 41.9 | 38.9 | 30.7 | 28.3 | 25.3 | |
| Congenital syphilis cases | n=197 | n=230 | n=312 | n=508 | n=642 | n=947 | n=1,422 | n=1,473 | n=1,813 | n=2,443 | n=1,186 | |
| Congenital syphilis cases according to prenatal follow-up information on the mother | ||||||||||||
| Yes | 84.8 | 83.9 | 76.9 | 75.0 | 78.4 | 83.3 | 84.3 | 86.2 | 88.1 | 89.4 | 88.4 | |
| No | 13.2 | 12.6 | 17.0 | 19.3 | 16.0 | 13.7 | 10.3 | 9.5 | 9.7 | 8.8 | 8.9 | |
| Unknowna | 2.0 | 3.5 | 6.1 | 5.7 | 5.6 | 3.0 | 5.4 | 4.3 | 2.2 | 1.8 | 2.7 | |
| Congenital syphilis cases according to maternal treatment regimen | ||||||||||||
| Adequate | 4.6 | 5.7 | 4.8 | 4.1 | 4.7 | 3.7 | 5.0 | 4.1 | 7.1 | 5.8 | 6.4 | |
| Inadequate | 47.2 | 50.4 | 43.9 | 51.0 | 52.6 | 62.9 | 60.1 | 62.1 | 61.1 | 63.3 | 59.3 | |
| Not performed | 32.0 | 28.7 | 29.2 | 26.0 | 27.1 | 22.0 | 24.0 | 25.1 | 25.3 | 22.6 | 22.2 | |
| Unknowna | 16.2 | 15.2 | 22.1 | 18.9 | 15.6 | 11.4 | 10.9 | 8.7 | 6.5 | 8.3 | 12.1 | |
a) The ‘missing’ category was included in the ‘unknown’ category of each variable.
Table 4 - Trend and average annual percent change of the gestational and congenital syphilis incidence rates and of the proportions of gestational and congenital syphilis cases according to sociodemographic and clinical variables of notified cases, Minas Gerais, Brazil, 2009-2019
| Demographic and clinical variables | % average annual percent change (95%CI)a | p-valueb | Trendc |
|---|---|---|---|
| Gestational syphilis incidence rate (2009-2018) | 36.7 (32.5;41.0) | <0.001 | Rising |
| Congenital syphilis incidence rate (2009-2018) | 32.8 (28.0;37.8) | <0.001 | Rising |
| Gestational syphilis cases by gestational age at diagnosis of syphilis | |||
| 1st trimester | 7.8 (5.5;10.1) | <0.001 | Rising |
| 2nd trimester | -2.3 (-3.6;-1.0) | 0.004 | Falling |
| 3rd trimester | -2.4(-3.8;-1.0) | 0.005 | Falling |
| Gestational age unknownd | -3.2 (-7.8;1.5) | 0.161 | Stationary |
| Gestational syphilis cases by pregnant women’s age range (years) at the time syphilis was diagnosed | |||
| 10-14 | 4.2 (-6.8;16.6) | 0.433 | Stationary |
| 15-19 | 1.4 (-1.3;4.2) | 0.285 | Stationary |
| 20-29 | 0.3 (-1.4;2.1) | 0.673 | Stationary |
| 30-39 | -2.3 (-4.6;0.1) | 0.058 | Stationary |
| ≥40 | -5.4 (-10.0;-0.5) | 0.037 | Falling |
| Gestational syphilis cases according to clinical classification of gestational syphilis at the time syphilis was diagnosed | |||
| Primary syphilis | -0.5 (-2.0;1.1) | 0.519 | Stationary |
| Secondary syphilis | -3.1 (-6.6;0.5) | 0.087 | Stationary |
| Tertiary syphilis | 6.1 (3.3;9.0) | 0.001 | Rising |
| Latent syphilis | 13.8 (3.2;25.5) | 0.016 | Rising |
| Diagnosis unknownd | -4.0 (-7.6;-0.2) | 0.042 | Falling |
| Congenital syphilis cases according to prenatal follow-up information on the mother | |||
| Yes | 0.7 (-0.8;2.3) | 0.304 | Stationary |
| No | -5.0 (-10.3;0.7) | 0.083 | Stationary |
| Unknownd | -2.7 (-13.6;9.6) | 0.622 | Stationary |
| Congenital syphilis cases according to maternal treatment regimen | |||
| Adequate | 2.7 (-1.3;6.9) | 0.168 | Stationary |
| Inadequate | 3.2 (1.5;5.0) | 0.003 | Rising |
| Not performed | -3.0 (-4.4;-1.7) | 0.001 | Falling |
| Unknownd | -6.2(-13.3;1.4) | 0.101 | Stationary |
a) 95%CI: 95% confidence interval; b) Statistical significance established using the Prais-Winsten regression T-test; c) Rising trend, when the p-value was less than 0.05 and the regression coefficient was positive; falling trend, when the p-value was less than 0.05 and the regression coefficient was negative; or stationary trend, when the p-value was greater than 0.05;
d) The ‘missing’ category was included in the ‘unknown’ category of each variable
Table 4 shows the trend analysis and average annual percent change for the gestational syphilis and congenital syphilis incidence rates, as well as for the proportions of gestational syphilis and gestational syphilis cases according to reported sociodemographic and clinical variables. Regarding the proportions of gestational syphilis and congenital syphilis cases, according to sociodemographic and clinical variables, a rising trend was observed in the proportions of gestational syphilis cases diagnosed in the 1st trimester (APC=7.8% - 95%CI 5.5%; 10.1%). An increasing trend was also found in the proportions of gestational syphilis cases clinically classified at the time of diagnosis as tertiary syphilis (APC=6.1% - 95%CI 3.3%; 9.0%) and as latent syphilis (APC=13.8% - 95%CI 3.2%;25.5%). There was also a significant rising trend in the proportion of cases of congenital syphilis with an inadequate maternal treatment regimen (APC=3.2% - 95%CI 1.5%;5.0%) (Table 4).
A falling trend was observed in the proportions of gestational syphilis cases according to gestational age at the time syphilis was diagnosed in the 2nd trimester (APC=-2.3% - 95%CI -3.6%;-1.0%) and in the 3rd trimester (APC=-2.4% - 95%CI -3.8%;-1.0%). A falling trend was also found in the proportions of gestational syphilis cases according to the age group of the pregnant woman at the time syphilis was diagnosed in women over 40 years old (APC=-5.4% - 95%CI -10.0%; -0.5%), in the proportions of gestational syphilis cases with unknown clinical classification at the time syphilis was diagnosed (APC=-4.0 - 95%CI -7.6%;-0.2%), and in the proportions of congenital syphilis cases for which there had been no maternal treatment regimen (APC=-3.0 - 95%CI -4.4%;-1.7%) (Table 4).
Discussion
The results found in this study show that there were significant rising trends in the gestational syphilis and congenital syphilis incidence rates. There was a significant rising trend in the proportions of gestational syphilis cases according to gestational period at diagnosis and clinical classification at diagnosis. Additionally, there was a significant rising trend in the proportion of congenital syphilis cases according to inadequate maternal treatment regimen.
Despite the discovery of penicillin in 1928, this being an effective drug for treating and curing syphilis, studies show a worldwide resurgence of this infection, especially among pregnant women, placing the disease as one of the most difficult challenges of the century for public health.19),(20 The increase in gestational syphilis and congenital syphilis incidence rates may be a reflection of the lack of supply of penicillin in the state of Minas Gerais. It is noteworthy that Brazil experienced a period of difficulty regarding distribution of this drug, between 2014 and 2016, due to lack of availability of raw materials to produce it and, consequently, lack of penicillin supplies throughout Brazil21 and worldwide.22
Previous studies have shown an increase in the cases of gestational syphilis and congenital syphilis in Minas Gerais, demonstrating that even today it continues to be a public health problem to be addressed in the state.3),(10),(11 This issue reinforces the need for health services, especially Primary Health Care services, to begin care for pregnant women early, as well as providing timely syphilis screening tests, enabling pregnant women to receive information and guidance for syphilis prevention and treatment in a timely manner.3)
Regarding the time at which gestational syphilis was diagnosed, a significant rising trend was observed in the proportions of gestational syphilis cases in the 1st trimester, and a significant falling trend in the 2nd and 3rd trimesters of gestation. These results suggest improvement in prenatal care coverage in Minas Gerais, since starting prenatal care late (after gestational age greater than 12 weeks) is the main factor hindering disease control during the gestational period.23 The federal government launched the Stork Network (Rede Cegonha) strategy in Brazil in 2011. In addition to being an important initiative for prenatal care, labor and birth, the Stork Network enables greater capacity to detect gestational syphilis through decentralization of syphilis screening tests to Primary Health Care.24 A nationwide study conducted in 2014 showed prenatal care coverage higher than 90.0%, regardless of the country's regions or the mothers’ characteristics.8) A significant rising trend was observed in the proportions of gestational syphilis cases with tertiary and latent syphilis. Latent syphilis is the asymptomatic phase of infection, and may be further classified as recent latent syphilis (infection for less than two years) or late latent syphilis (infection for more than two years).5 During the period of latency, the screening test is the most effective measure, since there are no signs or symptoms of infection.25 One of the hypotheses for this finding is the improvement in the coverage of prenatal care in Minas Gerais, in addition to provision of screening tests for pregnant women who benefit from this care. A previous study conducted in 2014 showed that Brazilian municipalities with reduced rates of vertical transmission of syphilis used a strategy which offered rapid testing and antibiotics (benzathine penicillin) to pregnant women in Primary Health Care.26 However, even though Brazilian municipalities have expanded access to prenatal care and actions to diagnose syphilis, high rates of congenital syphilis continue to be observed, and this is also a reality in Minas Gerais.26 The progress made by the Brazilian National Health Service is notorious. However, some events, such as congenital syphilis, are considered to be sentinel events with regard to access and especially for the quality of Primary Health Care, being closely related to weaknesses in prenatal care.27
As for the rising trend of congenital syphilis cases with an inadequate maternal treatment regimen, it must be highlighted that one of the major problems hindering the decrease of congenital syphilis is adherence to treatment.23 Currently, most women are diagnosed with syphilis during pregnancy; however, the high rates of congenital syphilis may reflect inadequate treatment.20 In order for treatment of gestational syphilis to be adequate, part of the cases need frequent visits to health services, leading to more traveling, increased costs and time off work.26 In addition, higher gestational syphilis and congenital syphilis incidence rates are found among women who are more vulnerable, such as those of brown and black skin color, those with less than eight years of schooling, and those in the 20-29 age group.3),(28
The quality of care offered to pregnant women during prenatal visits, delivery and birth is a key point for reducing the rates of vertical transmission of syphilis.25 For control of the disease to be effect, prevention must be based on three elements: serological screening, adequate treatment of pregnant women and adequate treatment of their sex partners.1) It should be emphasized that treating partners is no longer considered to be a criterion for assessing the adequacy of gestational syphilis treatment.7 However, the need should be stressed for cases of partners to be notified and treated with a view to their being cared for and, consequently, their pregnant partners not being infected again.29
This study has limitations inherent to the origin of the data, since it is based on passive notification of syphilis cases in the state of Minas Gerais. It is noteworthy that the data are updated periodically, which may alter the results, depending on the dates on which the data are accessed. It should also be remembered that congenital syphilis became a compulsorily notifiable disease in 1986, while gestational syphilis only became so in 2005. However, it is important to mention that over time the notification criteria have changed, and this directly impacts the variation in the number of reported cases.7 We highlight the possibility of the occurrence of gestational syphilis being underreported and also the incompleteness of the gestational syphilis and congenital syphilis notification forms identified by this study, as well as errors with regard to typing and filling in some of the fields.
The time trend analysis showed rising incidence of gestational and congenital syphilis, which can be related to higher detection of syphilis cases during pregnancy. However, there is a rising trend in the proportion of congenital syphilis cases with an inadequate maternal treatment regimen. Although this sexually transmitted infection is easily preventable and its treatment is effective, many challenges remain in related to controlling it. Continuing education of health professionals is suggested in order to improve gestational syphilis and congenital syphilis surveillance, as well as reinforcement of health actions, so that the problem can be mitigated, especially regarding strategies for women's health care and prenatal care.30
Therefore, this study highlights the need to strengthen actions aimed at the adequate treatment of gestational syphilis and the reduction of the epidemiological picture experienced by the state of Minas Gerais.
Referências
1. Magalhães DMS, Kawaguchi IAL, Dias A, Calderon IMP. Sífilis materna e congênita: ainda um desafio. Cad. Saúde Pública. 2013;29(6):1109-20. doi. https://doi.org/10.1590/S0102-311X2013000600008. [ Links ]
2. Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiané SG, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes: estimates for 2016 and progress since 2012. PLoS One. 2019 Feb 27;14(2):e0211720. doi: http://dx.doi.org/10.1371/journal.pone.0211720. [ Links ]
3. Nonato SM, Melo APS, Guimarães MDC. Sífilis na gestação e fatores associados à sífilis congênita em Belo Horizonte-MG, 2010-2013. Epidemiol Serv Saude. 2015;24(4):681-94. doi: http://dx.doi.org/10.5123/S1679-49742015000400010. [ Links ]
4. Macêdo VC, Lira PIC, Frias PG, Romaguera LMD, Caires SFF, Ximenes RAA. Fatores de risco para sífilis em mulheres: estudo caso-controle. Rev Saude Publica. 2017;51:78. doi: http://dx.doi.org/10.11606/s1518-8787.2017051007066. [ Links ]
5. Secretaria de Vigilância em Saúde (BR). Sífilis: 2020. Boletim epidemiológico [Internet]. out. 2020 [acesso 23 jul. 2021];(n. especial):1-42. Disponível em: Disponível em: http://www.aids.gov.br/pt-br/pub/2020/boletim-sifilis-2020 [ Links ]
6. Ministério da Saúde (BR). Protocolo clínico e diretrizes terapêuticas para atenção integral às pessoas com infecções sexualmente transmissíveis. Brasília, DF: MS; 2019. [ Links ]
7. Domingues RMSM, Szwarcwald CL, Souza-Junior PRB, Leal MC. Prevalência de sífilis na gestação e testagem pré-natal: estudo nascer no Brasil. Rev Saude Publica. 2014;48(5):766-74. doi: http://dx.doi.org/10.1590/S0034-8910.2014048005114. [ Links ]
8. Gomez GB, Kamb ML, Newman LM, Mark J, Broutet N, Hawkes SJ. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ. 2013 Mar 1;91(3):217-26. doi: http://dx.doi.org/10.2471/BLT.12.107623. [ Links ]
9. Cavalcante PAM, Pereira RBL, Castro JGD. Sífilis gestacional e congênita em Palmas, Tocantins, 2007-2014. Epidemiol Serv Saude. 2017;26(2):255-64. doi: https://doi.org/10.5123/s1679-49742017000200003. [ Links ]
10. Alves PIC, Scatena LM, Haas VJ, Castro SS. Evolução temporal e caracterização dos casos de sífilis congênita em Minas Gerais, Brasil, 2007-2015. Cienc Saude Colet. 2020;25(8):2949-60. doi: http://dx.doi.org/10.1590/1413-81232020258.20982018. [ Links ]
11. Magalhães EA, Silva GJ, Soares HSF, Guarienti M, Melo-Neto OP, Almeida KC, et al. Perfil epidemilógico de sífilis congênita no município de Patos de Minas-MG. Braz J Health Rev. 2020;3(2):2710-22. doi: http://dx.doi.org/10.34119/bjhrv3n2-117. [ Links ]
12. World Health Organization. Global health sector strategy on sexually transmitted infections, 2016-2021. Geneva: WHO; 2016 [acesso 23 jul. 2021]. Disponível em: Disponível em: https://www.who.int/reproductivehealth/publications/rtis/ghss-stis/en/ [ Links ]
13. Ministério da Saúde (BR). Indicadores e dados básicos da sífilis nos municípios brasileiros [Internet]. [Brasília, DF]: MS; [c2008; acesso 23 jul. 2021]. Disponível em: Disponível em: http://indicadoressifilis.aids.gov.br/ [ Links ]
14. Instituto Brasileiro de Geografia e Estatística. Área territorial oficial:consulta por unidade da federação com data de referência 2018 [Internet]. [Brasília, DF]: IBGE; [2019? acesso 20 mar. 2020]. Disponível em: Disponível em: https://www.ibge.gov.br/geociencias/organizacao-do378territorio/estrutura-territorial/15761-areas-dos-municipios.html?t=acesso-ao379produto&c=31 [ Links ]
15. Instituto Brasileiro de Geografia e Estatística. Estimativas da população residente no Brasil e unidades da federação com data de referência em 1. de julho de 2019 [Internet]. [Brasília, DF]: IBGE; [2020?; acesso 20 mar. 2020]. Disponível em: Disponível em: https://agenciadenoticias.ibge.gov.br/media/com_mediaibge/arquivos/7d410669a4ae85faf4 384 e8c3a0a0c649c7 [ Links ]
16. Secretaria de Estado de Saúde de Minas Gerais, Subsecretaria de Gestão Regional. Ajuste do plano diretor de regionalização de saúde de Minas Gerais (PDR/MG). Belo Horizonte: SES-MG; 2020 [acesso 23 jul. 2021]. Disponível em: Disponível em: www.saude.mg.gov.br . [ Links ]
17. Ministério da Saúde (BR). DATASUS [Internet]. Brasília, DF: MS ; c2008 [acesso 30 mar. 2021], Disponível em: Disponível em: http://www.datasus.gov.br [ Links ]
18. Antunes JLF, Cardoso MRA. Uso da análise de séries temporais em estudos epidemiológicos. Epidemiol Serv Saude. 2015;24(3):565-76. doi: http://dx.doi.org/10.5123/S1679-49742015000300024. [ Links ]
19. De Lorenzi DRS, Madi JM. Sífilis congênita como indicador de assistência Pré-natal. Rev Bras Ginecol Obstet. 2001;23(10):647-52. doi: http://dx.doi.org/10.1590/S0100-72032001001000006. [ Links ]
20. Cardoso ARP, Araújo MAL, Cavalcante MS, Frota MA, Melo SP. Análise dos casos de sífilis gestacional e congênita nos anos de 2008 a 2010 em Fortaleza, Ceará, Brasil. Cienc Saude Colet. 2018;23(2):563-74. doi: http://dx.doi.org/10.1590/1413-81232018232.01772016. [ Links ]
21. Ministério da Saúde (BR), Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Nota informativa conjunta GAB/SVS/MS n. 109/2015. Orienta a respeito da priorização da penicilina G benzatina para sífilis em gestantes e penicilina cristalina para sífilis congênita no país e alternativas para o tratamento da sífilis [Internet]. Brasília, DF: MS; 2015 [acesso 4 maio 2021]. Disponível em: Disponível em: http://www.aids.gov.br/ sites/default/files/legislacao/2015/-notas_informativas/ nota_informativa_109_assinada_pdf_20349.pdf [ Links ]
22. Nurse-Findlay S, Taylor MM, Savage M, Mello MB, Saliyou S, Lavayen M, et al. Shortages of benzathine penicillin for prevention of mother-tochild transmission of syphilis: an evaluation from multi-country surveys and stakeholder interviews. PLoS Med. 2017 27;14(12):e1002473. doi: https://doi. org/10.1371/journal.pmed.1002473. [ Links ]
23. World Health Organization, Department of Reproductive Health and Research. Investment case for eliminating mother-to-child transmission of syphilis: promoting better maternal and child health and stronger health systems. Geneva: WHO; 2012 [acesso 25 jul. 2021]. Disponível em: Disponível em: https://www.who.int/reproductivehealth/publications/rtis/9789241504348/en/ [ Links ]
24. Ministério da Saúde (BR). Portaria MS/GM n. 1.459, de 24 de junho de 2011. Institui, no âmbito do sistema único de saúde - SUS a rede cegonha [Internet]. Brasília, DF.: MS; 2011 jun 27 [acesso 4 maio 2021] Disponível em: Disponível em: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt1459_24_06_2011 [ Links ]
25. Viana-Filho LP, Silva AF, Rosa ACRG, Batista ALF, Chaves BC, FerreiRA JPT, et al. Dificuldades na abordagem e manejo da sífilis na gestação. Braz J Health Rev. 2020;3(4):11163-79. doi: https://doi.org/10.34119/bjhrv3n4-366. [ Links ]
26. Figueiredo DCMM, Figueiredo AM, Souza TKB, Tavares G, Vianna RPT. Relação entre oferta de diagnóstico e tratamento da sífilis na atenção básica sobre a incidência de sífilis gestacional e congênita. Cad Saude Publica. 2020; 36(3): e00074519. doi: https://doi.org/10.1590/0102-311x00074519. [ Links ]
27. Domingues RMSM, Saracen V, Hartz ZMA, Leal MC. Sífilis congênita: evento sentinela da qualidade da assistência pré-natal. Rev Saude Publica. 2013;47(1):147-57. doi: https://doi.org/10.1590/S0034-89102013000100019. [ Links ]
28. Lafetá KRG, Martelli-Júnior H, Silveira MF, Paranaíba LMR. Sífilis materna e congênita, subnotificação e difícil controle. Rev Bras Epidemiol. 2016;19(1):63-74. doi: https://doi.org/10.1590/1980-5497201600010006. [ Links ]
29. Plotzker RE, Murphy RD, Stoltey JE. Congenital syphilis prevention: strategies, evidence, and future directions. Sex Transm Dis. 2018;45(9S Suppl 1):S29-S37. doi: https://doi.org/10.1097/OLQ.0000000000000846. [ Links ]
30. Heringer ALDS, Kawa H, Fonseca SC, Brignol SMS, Zarpellon LA, Reis AC. Desigualdades na tendência da sífilis congênita no município de Niterói, Brasil, 2007 a 2016. Rev Panam Salud Publica. 2020;44:e3. doi: https://doi.org/10.26633/RPSP.2020.8. [ Links ]
Received: March 10, 2021; Accepted: May 24, 2021











 texto en
texto en