Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.4 Brasília dez. 2021 Epub 19-Nov-2021
http://dx.doi.org/10.1590/s1679-49742021000400016
ORIGINAL ARTICLE
Regional and social inequalities in mammography and Papanicolaou tests in Brazilian state capitals in 2019: a cross-sectional study
1Universidade do Extremo Sul Catarinense, Programa de Pós-Graduação em Saúde Coletiva, Criciúma, SC, Brazil
2Universidade Federal do Pampa, Curso de Nutrição, Itaqui, RS, Brazil
Methods:
This was a cross-sectional study with data from the 2019 Chronic Disease Risk and Protective Factors Surveillance Telephone Survey (Vigitel). The outcome variables were mammography and cytopathology test. The exposure variables were race/skin color, schooling and region of residence in Brazil. Absolute inequality measurements were presented using the slope index of inequality (SII) and equiplots.
Results:
23,339 women were included in this study. Having a mammography was 5.2 percentage points higher in women with higher levels of education, while having a cytopathology test was 5.3 percentage points lower in women of Black race/skin color.
Having mammography and cytopathology tests was 3.9 and 11.2 percentage points higher, respectively, in the Southern region.
Conclusion:
Social and regional inequalities persist in Brazil and affect mainly women of Black race/skin color, with low education levels and living in the Northeast region of the country.
Keywords: Mammography; Papanicolaou Test; Gynecological Examination; Socioeconomic Factors; Cross-Sectional Studies; Health Surveys.
Introduction
In recent years, coverage of mammography and Papanicolaou tests has increased in Brazil.1,2 According to the Chronic Disease Risk and Protective Factors Surveillance Telephone Survey (Vigitel), the proportion of women aged 50 to 69 who reported having had mammography increased from 71% in 2007 to 77% in 2019. The proportion of women aged 25 to 64 who reported having had a Papanicolaou test was over 80% during that same 12-year period.1,2
Despite the high proportion of women reporting having had screening tests for cervical cancer and breast cancer, lower coverage can be seen among those whose social vulnerability is greater, especially in the poorer regions of the country.3-6 This problem appears to be related to difficulties in accessing these examinations,7-10 in addition to social determinants, such as low levels of schooling,4,5,11 being of Black and brown race/skin color11,12 and use of public health services.11
Regional and social inequalities in coverage of preventive examinations such as mammography and Papanicolaou tests are of even greater concern, in view of the fact that, in 2020, more than 80,000 women were affected by breast cancer or cervical cancer in Brazil, these being, respectively, the first and the third most frequent types of cancer among women in Brazil.13 In 2018, more than 107,000 Brazilian women died due to cancer, including 16% as a result of breast cancer and 6% as a result of cervical cancer.13
Early diagnosis and treatment increase the potential for curing these forms of cancer.14 In Brazil, the Ministry of Health recommends breast cancer screening using mammography every two years for women aged 50 to 69.15 As for the Papanicolaou test for cervical cancer screening, the Ministry of Health recommends that it be performed every three years in women 25 years of age or older, who are currently sexually active or have been previously, and who had two negative results in consecutive years.16
Inequalities in having mammography and Pap tests have a major influence on the progression and outcome of breast cancer and cervical cancer.17 Issues such as level of development and health services offered in the region of residence, as well as the time interval between diagnosis and treatment must be addressed in order to conclude the health-disease process.11,17,18
The need to expand mammography coverage and maintain Papanicolaou test coverage levels in Brazil1,2 makes analysis of inequalities in having these examinations even more relevant, with the aim of identifying groups with greater difficulty in accessing these services, monitoring and determining the continuity of the actions involved and/or proposing new interventions. The use of the slope index of inequality (SII), which allows absolute inequality to be calculated taking into account the sample size in each subgroup of the stratification variable, is still uncommon in research on the theme in Brazil. The objective of this study was to assess regional and social inequalities in mammography and Papanicolaou tests among women living in the Brazilian state capitals and Federal District.
Methods
Context
Since 2006, Vigitel has surveyed people aged 18 years or older, residing in the 26 state capitals and Federal District, with the purpose of identifying the epidemiological profile of the population, monitoring, by means of a telephone survey, the frequency and composition of the determinants of chronic non-communicable diseases in Brazil.2
Sampling process
The Vigitel sampling process occurred in two stages, with the first stage consisting of randomly selecting telephone lines in each city, using telephone companies’ electronic directories of household landlines: 197,600 telephone lines were selected. In the second stage, one adult living in each selected household was randomly selected. At the end of the process, the probabilistic sample totaled 52,443 adults (18 years or older) living in the 26 Brazilian state capitals and Federal District, with around 2,000 interviewees in each city.2
The present study included women aged 50 to 69 years, eligible for mammography; and women aged 25 to 64 years, eligible for Papanicolaou testing, according to the recommendations of the National Cancer Institute, an auxiliary body of the Ministry of Health19 (Figure 1).
To control for selection bias and to ensure that all individuals in the adult population of the participating cities had equal probability of being selected to participate in the study, given that the sample data arose from the each city’s landline telephone records, Vigitel assigned weighting to each participant. The weighting resulted from the multiplication of two factors: the inverse of the number of telephone lines in the household selected, which corrected for the possibility of more than one telephone line at the same household being selected; and the number of adults in the household, which corrected for the lesser likelihood of more than one person from the same household being selected.
Variables
The outcome variables were having had mammography and Papanicolaou tests at some point during lifetime, as self-reported by the participants in response to the questions: Have you ever had a breast x-ray? and Have you ever had a Papanicolau test, a test to prevent cervical cancer?
To which they could answer ‘yes’ or ‘no’.
The exposure variables studied were:
Age range for Papanicolaou test (in years: 25-39; 40-59; 60-64);
Age range for mammography (in years: 50-59; 60-69);
Race/skin color (white; brown; black);
Schooling (in years: none; 1-4; 5-8; 9-11; 12 or over);
Brazilian macro-region (Northeast; North; Midwest; Southeast; South); and
Health insurance (no; yes).
Statistical methods
The assignment of post-stratification weighting to each participant was calculated using the Rake method. This method aims to equalize, in each city, the estimated socio-demographic data of the population living in homes with telephone lines and the estimated socio-demographic data of the total population, using the distribution of simple frequencies of each variable, such as 'age group', 'sex' and 'schooling' of the population, for each state capital city. This method also allows different external sources to be used, in the period between censuses, to determine these weights.2
Associations between exposure variables and outcomes were analyzed using Pearson's chi-square test, adopting a 5% significance level and 95% confidence intervals (95%CI).
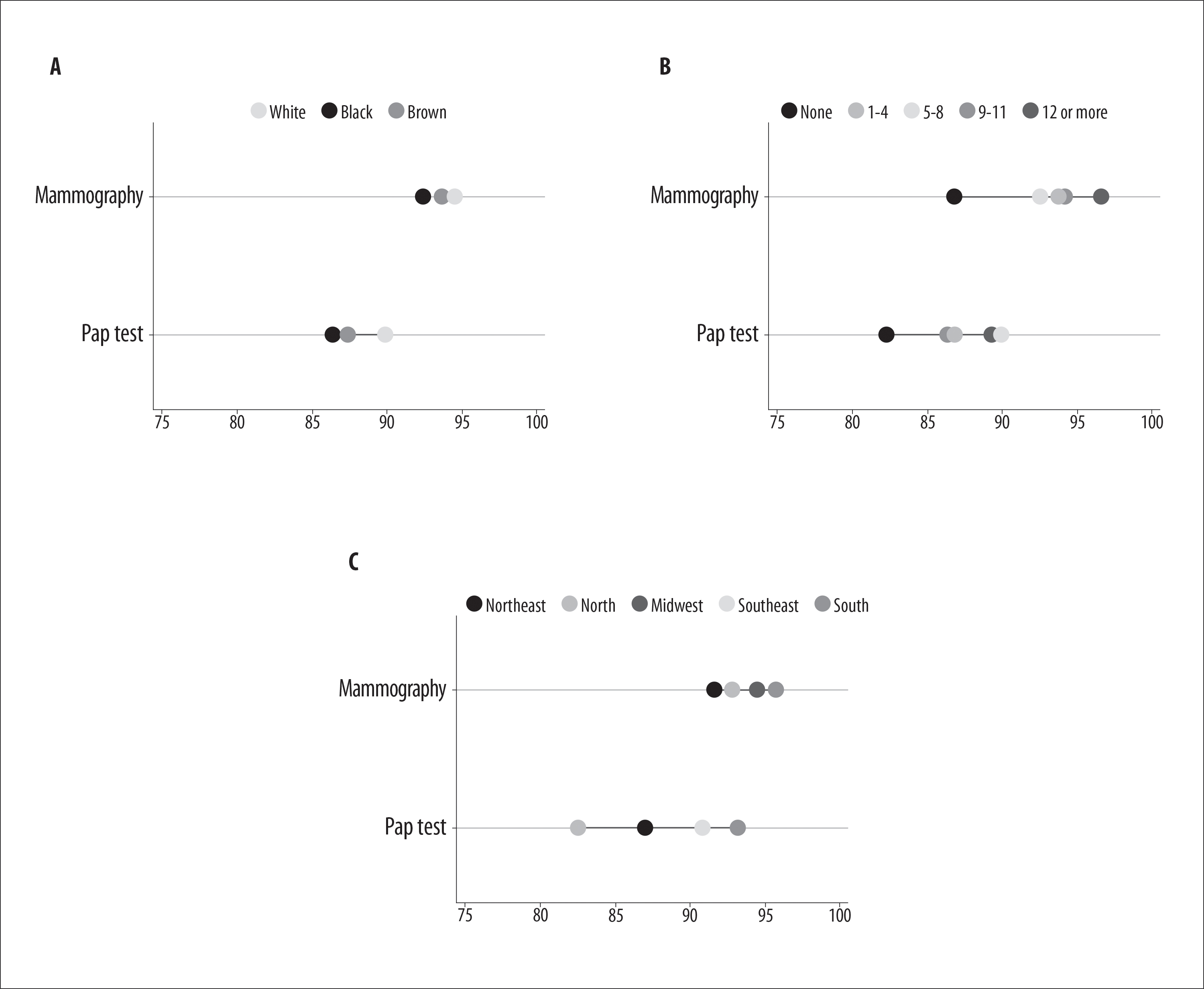
Racial, economic and regional inequalities with regard to having mammography and Papanicolaou tests were formally analyzed using SII. SII provides an absolute measurement of inequality, obtained based on the logistic regression of association between the dependent variable (having the examinations) and the independent variable included in the model; i.e. race/skin color, schooling and macro-region.20-22 SII allows to estimate the difference in prevalence of screening between the extreme groups of the independent variable (most privileged versus least privileged) to be calculated, taking into account the sample size in each subgroup of this variable. White race/skin color, no formal education, and living in the Northeast region were used as references in the analyses. Positive ISS values indicate greater prevalence of the outcome in the most privileged group, while negative values indicate greater prevalence of the outcome in the least privileged group. Equiplots were produced to illustrate the inequalities found.
The Stata statistical program, version 12.1, was used in all analyses, using the svy command because of Vigitel's complex sampling process.
Ethical aspects
The Vigitel 2019 survey project was approved by the Ministry of Health National Committee for Ethics in Human Research, as per Opinion No. 4324071, issued on June 6, 2017 (Certificate of Submission for Ethical Appraisal No. 65610017.1.0000.0008). All participants gave verbal informed consent at the time of the interview.2
Results
Of the 52,443 individuals surveyed in the 2019 edition of Vigitel, 34,089 were women. Of these, 10,750 were excluded from the analyses because they were outside the age group eligible for mammography or Papanicolaou test. Thus, 23,339 women were included in the analyses of the present study, with 20,361 eligible for Papanicolaou test (aged 25 to 64 years) and 13,423 eligible for mammography (aged 50 to 69 years) (Figure 1).
Among women aged 25 to 64 years eligible for the Papanicolaou test, 87.9% reported having already had this test at some point during their lifetime, while among women aged 50 to 69 years eligible for mammography, 93.8% reported having had this examination (Table 1). The percentage of women who had mammography was lowest in the Northeast (91.5%; p=0.052), among those who had completed less than one year of formal education (86.7%; p<0.001) and those who had no health insurance (91.3%; p<0.001). Lower percentages of Papanicolaou tests were found among women who lived in the Northern region of the country (82.5%; p<0.001), those who were younger (aged 25 to 39 years: 81.7%; p<0.001), those of brown race/skin color (86.3%; p=0.003), those who had completed less than one year of formal education (82.2%; p=0.027), and those who had no health insurance (84.7%; p<0.001).
Frequency of Papanicolaou testing was on average 5.3 percentage points lower among women of Black race/skin color compared to those of White race/skin color (95%CI -9.1;-1.5 - p=0.006) (Table 2 and Figure 2). Having mammography was, on average, 5.2 percentage points higher among women with higher levels of schooling when compared to those who had completed less than one year of formal education (95%CI 2.3;8.1 - p<0.001). Frequency of mammography (3.9 percentage points - 95%CI 1.6;6.3 - p=0.001) and Papanicolaou testing (11.2 percentage points - 95%CI 9.0;14.2 - p<0.001) among women living in the Southern region were higher when compared to those in the Northeastern region (Table 2 and Figure 2).
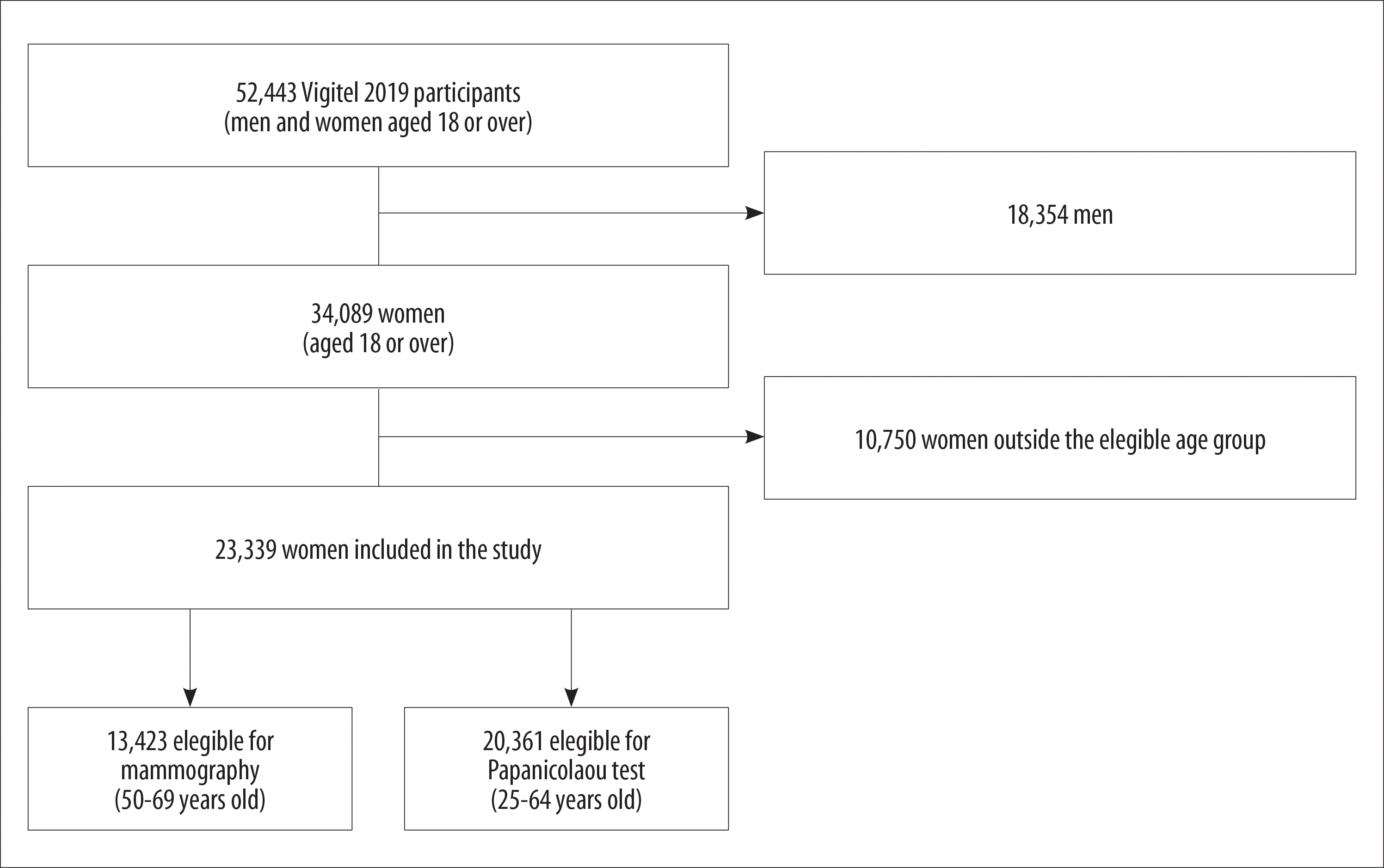
Figure 1 - Process of selection and inclusion of women participating in the study (n=23,339), Brazil, 2019
Table 1 - Mammography and Papanicolaou tests (n=23,339) performed according to sociodemographic variables of the women participating in the study, Brazil, 2019
| Variables | % | Mammography (n=13,423) | Pap test (n=20,361) | |||
|---|---|---|---|---|---|---|
| % (95%CI) | p-valuea | % (95%CI) | p-valuea | |||
| Age range for mammography (years) | 0.651 | |||||
| 50-59 | 58.9 | 94.0 (92.9;95.1) | ||||
| 60-69 | 41.1 | 93.6 (92.3;94.9) | ||||
| Age range for Papanicolaou test (years) | <0.001 | |||||
| 25-39 | 41.8 | 81.7 (79.8;83.7) | ||||
| 40-59 | 48.0 | 92.5 (91.6;93.4) | ||||
| 60-64 | 10.2 | 91.5 (89.6;93.4) | ||||
| Race/skin color | 0.392 | 0.003 | ||||
| White | 45.4 | 94.5 (93.3;95.7) | 89.9 (88.4;91.4) | |||
| Brown | 44.7 | 93.7 (92.4;95.1) | 86.3 (84.8;87.8) | |||
| Black | 9.9 | 92.4 (89.2;95.7) | 87.4 (84.3;90.5) | |||
| Schooling (years) | 0.001 | 0.027 | ||||
| None | 1.8 | 86.7 (78.4;94.5) | 82.2 (73.6;90.7) | |||
| 1-4 | 9.4 | 93.6 (91.5;95.7) | 86.7 (83.2;90.2) | |||
| 5-8 | 16.1 | 92.4 (90.3;94.6) | 89.7 (87.4;91.9) | |||
| 9-11 | 36.4 | 93.8 (92.5;95.0) | 86.4 (84.9;87.9) | |||
| ≥12 | 36.3 | 96.4 (95.2;97.6) | 89.2 (87.6;90.8) | |||
| Macro-region | 0.052 | <0.001 | ||||
| Northeast | 26.0 | 91.5 (89.6;93.4) | 87.0 (85.2;88.8) | |||
| North | 10.1 | 92.7 (91.6;93.9) | 82.5 (81.1;84.0) | |||
| Midwest | 11.7 | 94.3 (92.6;96.0) | 86.9 (84.4;89.4) | |||
| Southeast | 44.5 | 94.3 (92.8;95.8) | 90.7 (88.8;92.5) | |||
| South | 7.8 | 95.6 (93.8;97.3) | 93.0 (91.2;94.8) | |||
| Health insurance | <0.001 | <0.001 | ||||
| No | 54.9 | 91.3 (89.9;92.6) | 84.7 (83.3;86.2) | |||
| Yes | 45.1 | 96.8 (96.0;97.6) | 91.9 (90.8;93.1) | |||
| Total | 93.8 (93.0;94.7) | 87.9 (86.9;88.9) | ||||
a) Pearson’s chi-square test.
Table 2 - Absolute inequalities in having mammography and Papanicolaou tests (n=23,339) according to race/skin color, schooling and macro-region of the women participating in the study, Brazil, 2019
| Variables | Coefficientb | 95%CIa | p-valuec |
|---|---|---|---|
| Race/skin color | |||
| Mammography | -2.0 | -5.1;1.2 | 0.220 |
| Papanicolaou test | -5.3 | -9.1;-1.5 | 0.006 |
| Schooling | |||
| Mammography | 5.2 | 2.3;8.1 | <0.001 |
| Papanicolaou test | 3.0 | -0.9;6.9 | 0.132 |
| Macro-region | |||
| Mammography | 3.9 | 1.6;6.3 | 0.001 |
| Papanicolaou test | 11.2 | 9.0;14.2 | <0.001 |
a) 95%CI: 95% confidence interval; b) Unit of measurement: percentage points; c) Wald test.
Discussion
Frequency of Papanicolaou testing was lower among women of Black race/skin color, while frequency of mammography was greater among those with higher levels of schooling. Frequency of these examinations was lower in the Northeastern and Northern regions of the country.
The Vigitel sample only included individuals living in the capitals of the Brazilian states and the Federal District, in households with a landline telephone, which may reduce the representativeness of the sample, since the number of landline telephone in Brazilian households has been falling considerably in recent years. The North and Northeast had the lowest number of landline telephones per 100 households,23 these being precisely the regions that showed the lowest mammography and Papanicolaou test coverage, according to the results of the present study. The fact that low-income families have less access to landlines, precisely families whose access to these examinations is also lower, may indicate that regional inequality is even greater. The outcome we studied measures the prevalence of mammography and Papanicolaou tests performed at some point in life, without assessing the adequacy of the periodicity of these exams in keeping with Ministry of Health recommendations.15,16 This means that the results should be interpreted with caution, since the actual performance of the two female cancer prevention programs may be overestimated.
Standing out as a strength of the study was the formal inequality analysis using SII, which made it possible to calculate the difference in percentage points in the performance of each examination between the extreme groups of the stratification variable, taking into consideration the sample size in each subgroup of the independent variable.20-22
Confirmation of breast cancer diagnosis among women from the North, Northeast and Midwest macro-regions is more likely to occur later, since these regions have poorest coverage of general practitioners, radiologists, and mammography equipment, in contrast to the South and Southeast regions.7-9 A similar scenario is observed in relation to cervical cancer, since in the regions with the highest human development index, women were mostly diagnosed in stage I (tumor limited to the cervix), a situation opposite to that found in the Northeast.18
A cross-sectional study conducted with women aged 25 to 64 years, participating in the 2013 National Health Survey, found lower coverage of having a Papanicolaou test at least once in the last three years, in states in the Northeast region of the country, such as Maranhão (68%), Ceará (69%) and Sergipe (70%).6 The frequency of women who had never had an examination was also higher in states in the Northeast (Alagoas, 15%; Maranhão, 15%; Paraíba, 15%).6 The results of the cited study show the important regional differences in the frequency of mammography and Papanicolaou tests, and their heterogeneous representation in Brazil.4,6 The findings of the present study, in turn, show that the inequalities found in previous studies persist, despite progress with the coverage of tests observed in recent years, which may indicate difficulties in access to primary health care, since it is usually the way into the health system for these types of examinations.
One of the main problems associated with patient safety in primary health care is related to incorrect diagnosis of cancer, mainly caused by incorrect clinical evaluation or delay in ordering tests.24 Social and regional inequalities may have a direct relation with this situation, which goes beyond examination coverage, whereby timely diagnosis is needed, so as to ensure timely treatment.
Lower frequencies of mammography and Papanicolaou testing were found in women without health insurance when compared to those who reported using private health services. Despite the broad capillarity of primary health care services, with more than 43,000 Family Health Strategy teams, the barriers that make it difficult for users of the Brazilian National Health System (SUS) to have these examinations are many and varied, ranging from insufficient knowledge and lack of access to information, aspects linked to health services, to work-related situations.25
A cross-sectional survey of 345 women over 20 years of age, conducted in Maringá, Paraná, in 2015, also showed lower prevalence of having mammography among women without health insurance. The Papanicolaou test was not associated with health insurance.26 As for the public health sector, Family Health Strategy coverage is increasing in most of the country, although with a stationary trend in some states in the North, Northeast and Midwest.13
Considering the other variables used to assess racial and social inequality, greater levels of Papanicolaou testing were found in women of White race/skin color and who had higher levels of schooling, compared to those of Black race/skin color and no schooling. In addition, the percentage of having mammography examinations was higher among women with higher levels of schooling. A study using data from the 2008 National Household Sample Survey showed that level of schooling was associated with having mammography and clinical breast examination, whereby women without schooling had a higher risk of not having both tests.5 Similarly, another cross-sectional survey of 10,571 women aged 40 years and older showed higher rates of Papanicolaou test coverage in those with higher schooling (89%) and White race/skin color (83%).3
Level of schooling is one of the social determinants that impact the understanding of the health-disease process, access to information, health knowledge, and participation in treatment decisions. Low frequency of mammography and Papanicolaou testing among women with low schooling is related to some women's ability to understand, which reinforces the need to implement health education actions.27,28 In addition to offering these services, it is necessary to promote strategies that allow the health service user to understand the importance of participating in clinical decisions.
Racial inequalities and institutional racism make it difficult for Black women to access preventive health services,29 indicating, from a macro perspective, the need to expand access to the network of health services for Afro-Brazilian women, with emphasis on primary health care, improving health education processes, and even strengthening practices that combat institutional and structural racism.26
In conclusion, even with high frequencies of mammography and Papanicolaou examinations in Brazil, social and regional inequalities in having these exams persist, affecting mainly women of Black race/skin color, with low levels of schooling and who live in the Northeast region of the country.
Referências
1. Ministério da Saúde (BR). Vigitel Brasil 2007: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico. Brasília, DF: MS; 2008. (Série G. Estatística e Informação). [ Links ]
2. Ministério da Saúde (BR). Vigitel Brasil 2019: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2019. Brasília, DF: MS; 2020. [ Links ]
3. Barbosa YC, Oliveira AGC, Rabêlo PPC, Silva FS, Santos AM. Fatores associados à não realização de mamografia: pesquisa nacional de saúde, 2013. Rev Bras Epidemiol. 2019;22:e190069. doi: https://doi.org/10.1590/1980-549720190069. [ Links ]
4. Ramos ACV, Alves LS, Berra TZ, Popolin MP, Arcoverde MAM, Campoy LT, et al. Family Health Strategy, private health care, and inequalities in access to mammography in Brazil. Rev Panam Salud Publica. 2018 Nov 27;42:e166. doi: https://doi.org/10.26633/RPSP.2018.166. [ Links ]
5. Borges ZS, Wehrmeister FC, Gomes AP, Gonçalves H. Clinical breast examination and mammography: inequalities in Southern and Northeast Brazilian regions. Rev Bras Epidemiol. 2016;19(1):1-13. doi: https://doi.org/10.1590/1980-5497201600010001. [ Links ]
6. Barbosa IR. Regional and socioeconomic differences in the coverage of the papanicolau test in Brazil: data from the Brazilian health survey 2013. Rev Bras Ginecol Obstet. 2017;39(9):480-7. doi: https://doi.org/10.1055/s-0037-1604481. [ Links ]
7. Bezerra HS, Melo TFV, Barbosa JV, Feitosa EELC, Sousa LCM. Evaluation of access to mammographies in Brazil and socioeconomic indicators: a space study. Rev Gaucha Enferm. 2018 Oct 22;39:e20180014. doi: https://doi.org/10.1590/1983-1447.2018.20180014. [ Links ]
8. Nogueira MC, Fayer VA, Corrêa CSL, Guerra MR, De Stavola B, dos-Santos-Silva I, et al. Inequities in access to mammographic screening in Brazil. Cad Saude Publica. 2019 Jul 4;35(6):e00099817. doi: https://doi.org/10.1590/0102-311x00099817. [ Links ]
9. Rodrigues DCN, Freitas-Junior R, Rahal RMS, Corrêa RS, Gouveia PA, Peixoto JE, et al. Temporal changes in breast cancer screening coverage provided under the Brazilian National Health Service between 2008 and 2017. BMC Public Health. 2019 Jul 18;19(1):848. doi: https://doi.org/10.1186/s12889-019-7278-z. [ Links ]
10. Fernandes NFS, Galvão JR, Assis MMA, Almeida PF, Santos AM. Access to uterine cervical cytology in a health region: invisible women and vulnerable bodies. Cad Saude Publica. 2019 Oct 7;35(10):e00234618. doi: https://doi.org/10.1590/0102-311X00234618. [ Links ]
11. Cabral ALLV, Giatti L, Casale C, Cherchiglia ML. Social vulnerability and breast cancer: differentials in the interval between diagnosis and treatment of women with different sociodemographic profiles. Cien Saude Colet. 2019;24(2):613-22. doi: https://doi.org/10.1590/1413-81232018242.31672016. [ Links ]
12. Costa RFA, Longatto-Filho A, Vazquez FL, Pinheiro C, Zeferino LC, Fregnani JHTG. The quality of pap smears from the Brazilian cervical cancer screening program according to the human development index. Cancer Prev Res (Phila). 2020;13(3):299-308. doi: https://doi.org/10.5935/1676-2444.20160040. [ Links ]
13. Instituto Nacional de Câncer. Estatísticas de câncer [Internet]. Brasília, DF: INCA; 2021 [atualizado 4 mar. 2021; citado 21 mar. 2021]. Disponível em: Disponível em: https://www.inca.gov.br/numeros-de-cancer [ Links ]
14. World Health Organization. Guide to early cancer diagnosis. Geneva: WHO; 2017. [ Links ]
15. Migowski A, Silva GA, Dias MBK, Estevez Diz MDP, Sant’Ana DR, Nadanovsky P. Guidelines for early detection of breast cancer in Brazil. II: new national recommendations, main evidence, and controversies. Cad Saude Publica. 2018 Jun 21; 34(6):e00074817. doi: https://doi.org/10.1590/0102-311x00074817. [ Links ]
16. Instituto Nacional de Câncer José Alencar Gomes da Silva. Parâmetros técnicos para o rastreamento do câncer do colo do útero. Rio de Janeiro: INCA; 2019. [ Links ]
17. Oliveira NPD, Siqueira CAS, Lima KYN, Cancela MC, Souza DLB. Association of cervical and breast cancer mortality with socioeconomic indicators and availability of health services. Cancer Epidemiol. 2020;64:101660. doi: https://doi.org/10.1016/j.canep.2019.101660. [ Links ]
18. Vale DB, Sauvaget C, Muwonge R, Thuler LCS, Basu P, Zeferino LC, et al. Level of human development is associated with cervical cancer stage at diagnosis. J Obstet Gynaecol. 2019;39(1):86-90. doi: https://doi.org/10.1080/01443615.2018.1463976. [ Links ]
19. Ministério da Saúde (BR). Controle dos cânceres do colo do útero e da mama. 2a ed. Brasília, DF: MS; 2013. (Cadernos de atenção básica, n. 13). [ Links ]
20. Silva ICM, Restrepo-Mendez MC, Costa JC, Eweling F, Hellwig F, Ferreira LZ, et al. Mensuração de desigualdades sociais em saúde: conceitos e abordagens metodológicas no contexto brasileiro. Epidemiol Serv Saude. 2018;27(1):e000100017. doi: https://doi.org/10.5123/s1679-49742018000100017. [ Links ]
21. Barros AJD, Victora CG. Measuring coverage in MNCH: determining and interpreting inequalities in coverage of maternal, newborn, and child health interventions. PLoS Med. 2013;10(5):e1001390. doi: https://doi.org/10.1371/journal.pmed.1001390. [ Links ]
22. Schneider MC, Castillo-Salgado C, Bacallao J, Loyola E, Mujica OJ, Vidaurre M, et al. Métodos de mensuração das desigualdades em saúde. Rev Panam Salud Publica. 2002;12(6):398-414. doi: https://doi.org/10.1590/s1020-49892002001200006. [ Links ]
23. Agência Nacional de Telecomunicações. Painéis de dados: telefonia Fixa [Internet]. Brasília, DF: Anatel; 2021 [atualizado 4 mar. 2021; citado 21 mar. 2021]. Disponível em: Disponível em: https://informacoes.anatel.gov.br/paineis/ [ Links ]
24. Aaronson EL, Quinn GR, Wong CI, Murray AN, Petty CR, Einbinder J, et al. Missed diagnosis of cancer in primary care: insights from malpractice claims data. J Healthc Risk Manag. 2019;39(2):19-29. doi: https://doi.org/10.1002/jhrm.21385. [ Links ]
25. Aguilar RP, Soares DA. Barreiras à realização do exame papanicolau: perspectivas de usuárias e profissionais da estratégia de saúde da família da cidade de Vitória da Conquista-BA. Physis. 2015;25(2):359-79. doi: https://doi.org/10.1590/S0103-73312015000200003. [ Links ]
26. Lopes TCR, Gravena AAF, Agnolo CMD, Rocha-Brischiliari SC, Demitto MO, Carvalho MDB, et al. Prevalência e fatores associados à realização de mamografia e exame citopatológico. Rev Bras em Promo Saude. 2015;28(3):402-10. doi: https://doi.org/10.5020/18061230.2015.p402. [ Links ]
27. Maschka A, Paasche-Orlow MK, Kressin NR, Schonberg MA, Battaglia TC, Gunn CM. Discussions of potential mammography benefits and harms among patients with limited health literacy and providers: “Oh, there are harms?”. J Health Commun. 2020 Dec 1;25(12):951-61. doi: https://doi.org/10.1080/10810730.2020.1845256. [ Links ]
28. Bowser D, Marqusee H, El Koussa M, Atun R. Health system barriers and enablers to early access to breast cancer screening, detection, and diagnosis: a global analysis applied to the MENA region. Public Health. 2017;152:58-74. doi: https://doi.org/10.1016/j.puhe.2017.07.020. [ Links ]
29. Malta DC, Bernal RTI, Carvalho QH, Pell JP, Dundas R, Leyland A, et al. Women and evaluation of inequalities in the distribution of risk factors for Chronic non‑communicable diseases (NCD), Vigitel 2016-2017. Rev Bras Epidemiol. 2020 Jun 6;23:e200058. doi: https://doi.org/10.1590/1980-549720200058. [ Links ]
Received: March 26, 2021; Accepted: July 22, 2021











 texto em
texto em