Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.30 no.4 Brasília dez. 2021 Epub 05-Nov-2021
http://dx.doi.org/10.1590/s1679-49742021000400015
RESEARCH NOTE
National congenital anomaly registers in the world: historical and operational aspects
1Ministério da Saúde, Secretaria de Vigilância em Saúde, Brasília, DF, Brazil
Objective:
To identify registers of congenital anomalies with national coverage currently available around the world, highlighting their main historical and operational characteristics.
Methods:
This was a documentary study by means of a Medline database search (via PubMed) and searches involving reports, official documents and websites. Studies reporting at least one national registry were included.
Results:
40 registers of national congenital anomalies were identified in 39 different countries. All registers included in the study were concentrated in upper-middle or high-income countries located in Europe. Most of the registers were population-based, compulsory notification and with a time limit for notification of up to 1 year of age. The Brazilian register showed the highest annual coverage.
Conclusion:
The registers analyzed showed different characteristics, related to the reality of each country. The results presented provide support for the theme of congenital anomalies surveillance, especially in places where such activity is intended to be implemented.
Keywords: Congenital anomalies; Birth Declaration; Epidemiological Surveillance; Review; International Cooperation; Health Services; Disease Records.
Introduction
Congenital anomalies are structural or functional changes that occur during intrauterine life.1 In addition to being important causes of perinatal and neonatal deaths, they can contribute to long-term disability, which may have significant impacts on individuals, their families, healthcare systems, and societies.1,2 According to the World Health Organization, about 295,000 babies die within the first four weeks of birth due to congenital anomalies every year.1
Systematic and continuous collection of information on cases of congenital anomalies in a well-defined population characterizes a register.3 In the world, different registers of congenital anomalies were developed in the second half of the twentieth century, after the episode known as "the thalidomide tragedy", when more than 10 thousand children in 46 countries were born with severe congenital anomalies due to the use of this drug during pregnancy.4 Registers of congenital anomalies are useful for monitoring temporal or geographic differences in the frequencies of these disorders and assisting in the identification of risk factors. They can also contribute in delineating vulnerable populations, plan and evaluate health care offers, among others.3,5
Understanding the epidemiological profile of congenital anomalies, by means of information systems and monitoring with national coverage, provides countries with an opportunity to perceive their impact on the population and health systems. This knowledge also produces useful information that can promote prevention measures and adequate health care aimed at the specific scenario of each location.6-8
Registers of congenital anomalies can cover entire countries or a representative sample of the national population (national registers), or specific locations in a country (local or subnational registers). In addition, they can cover all births of a given geographical area (population-based) or cover only births in a single hospital or selected hospitals (hospital-based).9,10 However, there are no data in the scientific literature on the global and updated perspective of national registers of congenital anomalies and their peculiarities.
The objective of this study was to identify registers of congenital anomalies with national coverage currently available around the world, highlighting their main historical and operational characteristics.
Methods
This was a documentary study, which its methodological strategy was detailed in a narrative review on international congenital anomaly surveillance collaboration networks, previously published.6 In general, to map and document the registers of congenital anomalies with national coverage currently available around the world, we searched for bibliographic references indexed in Medical Literature Analysis and Retrieval System Online (Medline)/PubMed database (made available by the National Library of Medicine of the United States) on January 10, 2020, through the search key specified in Figure 1. In addition to this search, relevant information related to this research theme was obtained from reports, official documents and websites made available by networks, records and institutions that work with the surveillance of congenital anomalies.
The main methodological steps, as well as the information extracted from each of the studies or documents that were found, are detailed in Figure 1. The information extracted was analyzed by two reviewers (Cardoso-dos-Santos AC and Alves SRM), in an independent manner. Information on the gross national income per capita of each participating country was obtained from the World Economic Situation and Prospects report, produced by the United Nations.7
Results
A total of 40 registers of congenital anomalies with national coverage were identified in 39 countries. Their main characteristics are presented in Box 1. With the exception of Africa, all continents have submitted at least one national register of congenital anomalies. Most of these countries were located on the European continent, all of them were in the upper-middle (12) and high income (28) categories as shown in Figure 2. There were 26 population-based and 12 hospital-based registers; no registers were found for Chile and Panama.
The Hungarian Congenital Abnormality Registry was the oldest registry. It was established in 1962, while the most recent was the Scottish, implemented in 2018. The majority of the national registries (29/40) were included in at least one international congenital anomaly surveillance collaboration network. The Brazilian registry was the one with the highest number of births annually - around 3 million - and covered 100% of births in the country. In total, 19 registers had more than 98% coverage. Almost all of them were population-based: two of them, Cuba and the Dominican Republic, in Central America, were hospital-based registries.
Fourteen national registers were compulsory, of these, 12 were population-based notifications; and of the 11 voluntary registers, only five were population-based notifications. The chronological age limit to notify an individual with congenital anomaly was also very different among the registers, ranging from hospital discharge (6) to one month (5) or greater than or equal to 1 year of age (23).
A total of 16 national registers reported only major congenital anomalies, and 14 reported major and minor congenital anomalies. The International Statistical Classification of Diseases and Related Health Problems (ICD, 9th and 10th revisions) was the main coding system used (32); however, ten national registers modified the ICD (especially the British Pediatric Association Classification of Diseases).
Regarding gestational outcomes, 33 information systems reported notifications of live births and stillbirths, and of these, 20 included termination of pregnancy in their scope. Brazilian and Thai registers were the only ones to include only live births. Among the registers searched, at least 19 also performed the surveillance of congenital anomalies in their coverage area.

Legend: CA: congenital anomalies; ICD: International Statistical Classification of Diseases and Related Health Problems; PubMed/Medline: Medical Literature Analysis and Retrieval System Online (Medline)/PubMed, is the U.S National Library of Medicine’s premier bibliographical database.
Figure 1 - Flowchart of the main methodological steps for the identification and selection of registers of congenital anomalies with national coverage currently available around the world
Box 1 - Main characteristics of registers of congenital anomalies with national coverage around the world, January 10, 2020
| Country | Income | Registry | Year created | Type of registry | Network | Number of births (thousands) annually (% of coverage) | Compulsory | Time limit | Type of congenital anomaly | Coding | Pregnancy outcomes | Surveillance | Information source |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Saudi Arabia | High | Medical Service Department- Birth Defect Registry (MSD-BDR) | 2010 | Hospital-based | ICBDSR | - | Yes | 2 years | Major | ICD-BPA | - | - | https://bit.ly/2XHWSNm |
| Argentina | Upper-middle | National Registry of Congenital Anomalies of Argentina (RENAC) | 2009 | Hospital-basesd | ICBDSR, ReLAMC | 300 (40%) | No | Hospital discharge | Major | ICD-BPA | Live birth and Stillborn | Yes | https://bit.ly/3bCBph4 http://dx.doi.org/10.5546/aap.2013 |
| Australia | High | Australian Congenital Anomalies Monitoring System (ACAMS) | 1981 | Population-based | - | - | Hybrid | Vary among different collections | Major | ICD-BPA and AM | Live birth and Stillborn | Yes | https://bit.ly/2LqbnTQ https://bit.ly/2Ke5JmZ |
| Brazil | Upper-middle | Sistema de Informações sobre Nascidos Vivos (Sinasc) | 1999 | Population-based | ReLAMC | 3.000 (100%) | Yes | Hospital discharge | Major | ICD | Live birth | No | https://bit.ly/3nId7VA |
| Canada | High | Canadian Congenital Anomalies Surveillance System (CCASS) | 1966 | Population-based | ICBDSR | 330 (98%) | - | 1 month | Major | ICD-CA | Live birth and Stillborn | Yes | https://bit.ly/3bEVm6U https://bit.ly/2LMLUDV |
| Chile | High | Registro Nacional de Anomalías Congénitas de Chile (RENACH) | 2016 | - | ReLAMC | 220 | - | - | - | - | - | - | https://bit.ly/38Gs1Hq https://bit.ly/3qyZ7iq |
| China | Upper-middle | Birth Defects Surveillance System for the Collaborative Project-China (BDSS-China) | 1992 | Population-based | - | 260 | - | 42 days | Major | ICD | Live birth and Stillborn | Yes | https://doi.org/10.1002/ajmg.c.31690 https://doi.org/10.1007/s12519-011-0326-0 |
| China | Upper-middle | Chinese Birth Defects Monitoring Network (CBDMN) | 1988 | Hospital-based | - | 1.380 (8.51%) | No | 7 days | Major | ICD | Live birth, Stillborn and Termination of pregnancy | Yes | https://doi.org/10.1007/s12519-011-0326-0 https://doi.org/10.1046/j.1365-3016.2003.00478.x |
| Colombia | Upper-middle | Vigilancia de los Defectos Congénitos | 2010 | Population-based | ReLAMC | 661 (100%) | - | 1 year | Major | ICD | - | - | https://doi.org/10.26633 /RPSP.2019.44 |
| Costa Rica | Upper-middle | Costa Rican Birth Defects Register Centre (CREC) | 1985 | Population-based | ICBDSR, ReLAMC | 70 (100%) | Yes | 1 year | Major and minor | ICD-BPA | Live Birth and Stillborn | Yes | https://bit.ly/3bPXdWL https://doi.org/10.26633 /RPSP.2019.44 https://doi.org/10.1007/s10995-014-1542-8 |
| Cuba | Upper-middle | Cuban Register of Congenital Malformation (RECUMAC) | 1985 | Hospital-based | ICBDSR, ReLAMC | 120 (100%) | No | Hospital discharge | Major and minor | ICD-BPA | Live birth, Stillborn and Termination of pregnancy | - | https://doi.org/10.26633 /RPSP.2019.44 http://doi.org/10.26633/RPSP.2017.174 |
| Denmark | High | Danish Medical Birth Registry | 1973 | Population-based | - | - | - | 1 year | - | ICD | Live birth, Stillborn and Termination of pregnancy | - | https://bit.ly/3quYJ4D https://doi.org/10.1080/ 14034940210134194 https://doi.org/10.3402/ ijch.v68i5.17376 |
| The United Arab Emirates | High | National Congenital Anomalies Register | 1999 | Population-based | - | 63 (100%) | - | 1 year | Major | ICD with modification | Live Birth and Stillborn | Yes | https://bit.ly/39LKphk |
| Scotland | Highb | The Scottish Linked Routine Data Congenital Anomaly Register | 2018 | Population-based | EUROCAT | 50-55 (100%) | Hybrid | 1 year | Major | ICD | Live birth, Stillborn and Termination of pregnancy | - | https://bit.ly/3oUI0Y1 https://bit.ly/39FYiO5 |
| Slovakia | High | Teratologic Information Centre, Slovak Medical University | 1964 | Population-based | ICBDSR | 55 (100%) | Yes | Hospital-based | - | - | Live birth, Stillborn and Termination of pregnancy | - | https://bit.ly/2XHWSNm http://dx.doi.org/10.1136/bmjopen-2018-028139 |
| Spain | High | Spanish Collaborative Study of Congenital Malformations (ECEMC) | 1976 | Hospital-based | ICBDSR, EUROCAT | 90 (20%) | No | 3 days | Major and minor | ICD | Live birth and Stillborn (Termination of pregnancy in some hospitals) | Yes | https://bit.ly/3imtzto, https://doi.org/10.2165/00002018-200831060-00008 https://doi.org/10.1016/j.jpedsurg.2008.07.002 |
| The United States | High | National Birth Defects Prevention Network (NBDPN) | 1997 | Population-based | - | - | No | - | Major | ICD e CDC/BPA | Live birth, Stillborn and Termination of pregnancy | Yes | https://bit.ly/3sxskMG https://doi.org/10.1002/ bdr2.1607 https://doi.org/ 10.1155/2014/212874 |
| Finland | Alta | Register of Congenital Malformations | 1963 | Population-based | ICBDSR, EUROCAT | 60 (100%) | Yes | 1 year | Major | ICD | Live birth, Stillborn and Termination of pregnancy | Yes | https://bit.ly/3nUTRUH https://bit.ly/2XHWSNm https://doi.org/10.3402/ijch.v68i5.17376 https://doi.org/10.1093/ije/11.3.239 |
| Guatemala | Upper-middle | Protocolo de Vigilancia de Anomalías Congénitas | 2017 | Hospital-based | - | 155 (40%) | - | 1 month | Major | ICD | - | Yes | https://doi.org/10.26633 /RPSP.2019.44 |
| Hungary | High | Hungarian Congenital Abnormality Registry (HCAR) | 1962 | Population-based | ICBDSR, EUROCAT | 100 (100%) | Yes | 1 year | Major and minor | ICD with modification | Live birth, Stillborn and Termination of Pregnancy | - | https://bit.ly/2XHWSNm https://doi.org/10.1111/cga.12025 |
| England | Highb | National Congenital Anomaly and Rare Disease Registration Service (NCARDRS) | 2015 | Population-based | BINOCAR, ICBDSR | 610 (100%) | No | - | Major and minor | ICD | Live birth, Stillborn and Termination of pregnancy | - | https://bit.ly/38UlJEb http://dx.doi.org/ 10.1136/archdischild- 2017-312833 |
| Iceland | High | Icelandic Register of Births | - | Base populacional | - | - | - | - | - | ICD | Live birth and Stillborn | - | https://doi.org/10.3402/ijch.v68i5.17376 |
| Italy | High | Italian Multicenter Register for Congenital Malformations (IPIMC) | 1977 | Hospital-based | - | 116 (20%) | No | 5 days | Major | - | Live birth and Stillborn | Yes | http://doi.wiley.com/10.1002/ajmg.1320460425 https://doi.org/10.1007/BF00162315 |
| Japan | High | Japan Association of Obstetricians and Gynaecologists (JAOG) | 1972 | Hospital-based | ICBDSR | 100 (9%) | - | 7 days | - | - | Live birth and Stillborn | - | https://bit.ly/2XTwSyV https://bit.ly/2XHWSNm |
| Latvia | High | Register of Patients Suffering from Certain Diseases | 1987 | Population-based | EUROCAT | 19.2 (100%) | Yes | 18 years | - | - | Live birth, Stillborn and Termination of pregnancy | - | https://bit.ly/3oUI0Y1 https://doi.org/10.1186/s13023-014-0147-z |
| Malta | High | Malta Congenital Anomalies Register (MCAR) | 1985 | Population-based | ICBDSR, EUROCAT | 4 (100%) | No | 1 year | Major and minor | ICD | Live birth and Stillborn | - | https://bit.ly/2XHWSNm https://bit.ly/3oUI0Y1 |
| Mexico | Upper-middle | Registro y Vigilancia Epidemiológica de Malformaciones Congénitas (RYVEMCE) | 1978 | Hospital-based | ICBDSR | 62 (3.5%) | No | Hospital discharge | Major and minor | - | Live birth and Stillborn | Yes | https://doi.org/10.26633/RPSP.2019.44 https://bit.ly/2XHWSNm https://doi.org/10.1016/j.bmhimx.2017.02.003 https://bit.ly/3qqzz76 |
| Norway | High | Medical Birth Registry of Norway (MBRN) | 1967 | Population-based | ICBDSR, EUROCAT | 60 (100%) | Yes | 1 year | - | ICD-BPA | Live birth, Stillborn and Termination of pregnancy | Yes | https://bit.ly/35OTZyM http://doi.wiley.com/ 10.1034/j.1600-0412. 2000.079006435.x https://doi.org/ 10.1111/dmcn.13552 |
| New Zealand | High | New Zealand Birth Defects Registry (NZBDR) | 1975 | Population-based | ICBDSR | 58 (100%)c | Yes | No time limit | Major and minor | - | Live birth, Stillborn and Termination of pregnancy | - | https://bit.ly/2XRvhK4 https://bit.ly/2XHWSNm |
| Wales | Highb | Congenital Anomaly Register & Information Service for Wales (CARIS) | 1998 | Population-based | BINOCAR, ICBDSR, EUROCAT | 35 (100%) | No | 1 year | Major and minor | ICD | Live birth, Stillborn and Termination of pregnancy | - | https://bit.ly/3nUENXh https://bit.ly/2XHWSNm http://doi.wiley.com/10.1002/bdra.23336 |
| Panama | High | Programa Nacional de Malformaciones Congénitas de Panama (PNMC) | - | - | ReLAMC | - | - | - | - | - | - | - | https://bit.ly/3qyZ7iq |
| Paraguay | Upper-middle | Programa Nacional de Prevención de Defectos Congénitos del Ministerio de Salud Pública del Paraguay (PNPDC) | 2016 | Hospital-based | ReLAMC | Yes | 1 year | Major and minor | ICD | - | - | https://bit.ly/3qwW9LG https://bit.ly/3qyZ7iq | |
| Poland | High | Polish Registry of Congenital Malformations (PRCM) | 1997 | Population- based | EUROCAT | 300 (85%) | Yes | 2 years | Major and minor | ICD | Live birth, Stillborn and Termination of pregnancy | Yes | https://bit.ly/3oVZp2G https://bit.ly/3oUI0Y1 https://bit.ly/3oWRSAL |
| Portugal | High | Portuguese national registry of congenital anomalies (RENAC) | 1995 | Population-based | EUROCAT | - | No | At the end of the neonatal period | Major | ICD | Live birth, Stillborn and Termination of pregnancy | Yes | https://bit.ly/2NgJ7DC http://doi.wiley.com/10.1002/bdra.23530 |
| Czech Republic | High | National Registry of Congenital Anomalies (NRCA) of the Czech Republic | 1964 | Population-based | ICBDSR, EUROCAT | 110 (100%) | Yes | 15 years | - | ICD | Live birth, Stillborn and Termination of pregnancy | Yes | https://bit.ly/35QVI6U https://bit.ly/2XHWSNm https://doi.org/10.21101/cejph.a4201 |
| Dominican Republic | Upper-middle | Sistema Nacional de Vigilancia Epidemiológica | 2016 | Hospital-based | - | 193 (100%) | - | Hospital discharge | Major and minor | ICD | - | - | https://doi.org/10.26633/RPSP.2019.44 |
| Singapore | High | National Birth Defects Registry | 1992 | Population-based | - | - | - | 18 years | Major and minor | ICD | Live birth, Stillborn and Termination of pregnancy | - | http://doi.org/10.3389/fped.2014.00060 https://bit.ly/38S57Nk |
| Sweden | High | Swedish Medical Birth Registry (MBR) | 1964 | Population-based | ICBDSR, EUROCAT | 100-120 (100%) | Yes | 1 year | - | ICD | Live birth, Stillborn and Termination of pregnancy | Yes | http://doi.wiley.com/10.1080/ 00016340902934696 http://doi.wiley.com/10.1111/ j.1651-2227.1989.tb11122.x |
| Thailand | Upper-middle | Thailand Birth Defects Registry | 2014 | Hospital- based | SEAR-NBBD | 67 (8.3%) | - | 1 year | 5 priority typesd | ICD | Live birth | - | https://bit.ly/2NgKfqQ https://doi.org/10.1002/ajmg.c.31690 |
| Uruguay | High | Registro Nacional de Defectos Congénitos y Enfermedades Raras de Uruguay (RNDCER) | 2011 | Population-based | ReLAMC | 28 (58%) | Yes | 6 years | Major and minor | ICD | Live birth, Stillborn and Termination of pregnancy | Yes | https://bit.ly/2KumQRM https://doi.org/10.26633/RPSP.2019.44 https://bit.ly/3qyZ7iq |
a) NBDPN is a volunteer-based organization in the United States; (b) the information is related to the United Kingdom; (c) covers all live births delivered or treated at a public hospital in New Zealand; d) Down syndrome, neural tube defects, cleft lip and palate, limb abnormalities and Duchenne muscular dystrophy.
Legend: BINOCAR: British and Irish Network of Congenital Anomaly Researchers; BPA: British Pediatric Association Classification of Diseases; CDC: Centers for Disease Control and Prevention of the United States; ICD: International Classification of Diseases and Related Health Problems; EUROCAT: European surveillance of congenital anomalies; ICBDSR: International Clearinghouse for Birth Defects, Surveillance and Research; ReLAMC: Red Latinoamericana de Malformaciones Congénitas; SEAR-NBBD: South-East Asia Region New-born and Birth Defects.
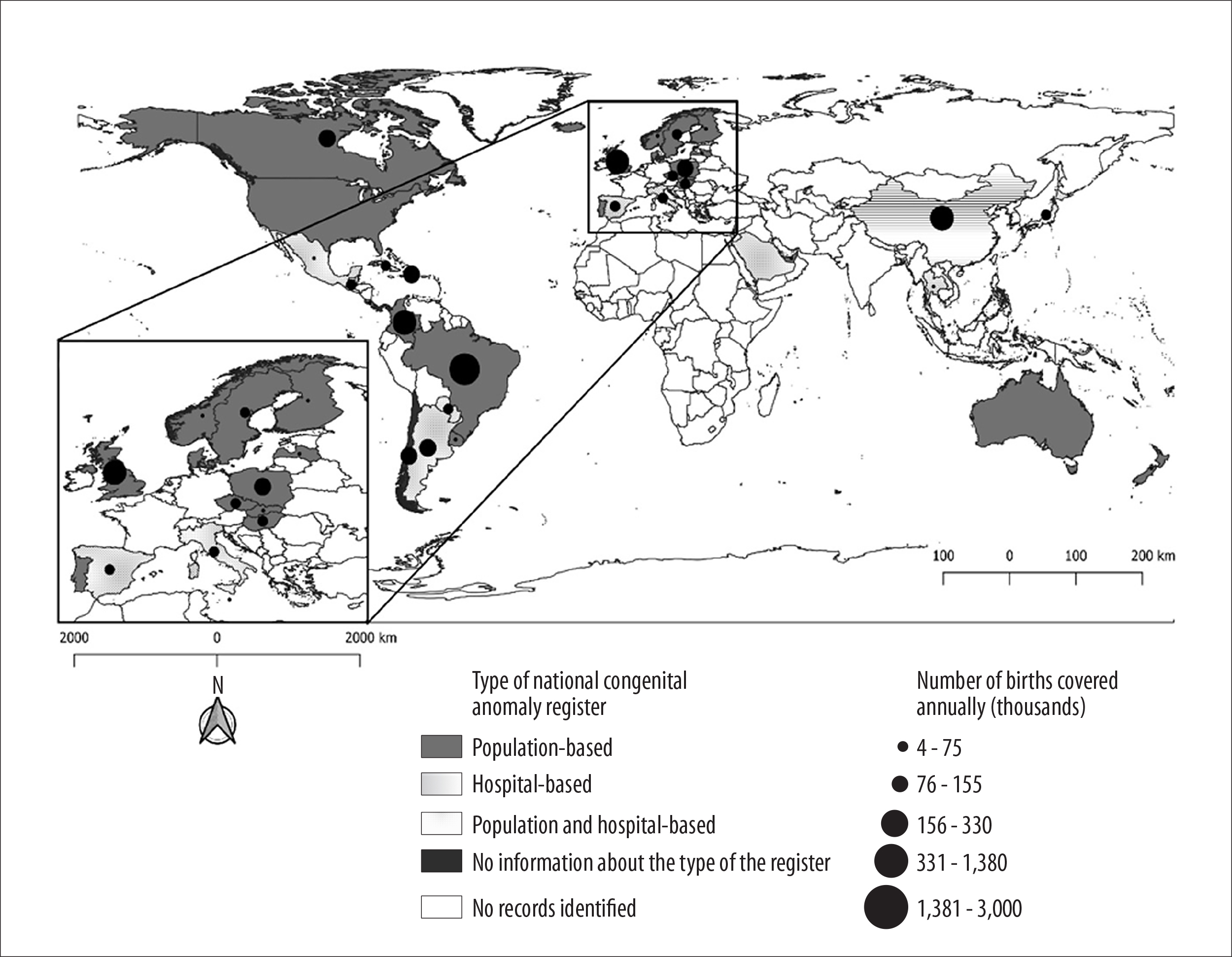
Note: England, Scotland and Wales registries were jointly represented by the United Kingdom, and the annual coverage was represented by the sum of births in the three registries of congenital anomalies. Filled polygons represent countries that have at least one national registry of congenital anomalies of population-based, hospital-based or both. The size of the circle is proportional to the number (thousands) of births covered annually, in each registry.
Figure 2 - Worldwide distribution and annual coverage of the registers included in this study (A), highlighting the European continent (B), January 10, 2020
Discussion
Only 40 registers of congenital anomalies with national coverage were found in 39 different countries worldwide. The registers identified were concentrated exclusively in upper-middle and high-income countries, most of them located in Europe. Thus, the global estimates of congenital anomalies tend to overrepresent these places, to the detriment of others. However, the production of a series of technical and scientific papers for guidance of the different stages of surveillance of congenital anomalies is an important contribution of the registers present in these countries.
The absence of representativeness in low and lower-middle-income countries is important because, in these contexts, the impact of anomalies on health may be greater, due to the low supply of adequate health services for the care of affected children.8 In addition, in these countries, other causes of infant mortality, such as malnutrition, poor sanitation conditions and susceptibility to infections, difficulty accessing health care services, among others, are still common, which can help "mask" the real magnitude of congenital anomalies, in epidemiological aspects.8,11
Major events involving teratogenic effects, such as the thalidomide tragedy,4,12 the Chernobyl disaster13 and the congenital syndrome associated with Zika virus infection,14 have been mobilizing nations and their territories for the surveillance of congenital anomalies. Despite the Hungarian register being the oldest found in this study (1962), the Czech Republic National Registry began its activities in 1961 but regular monitoring started in 1964.15
The registers with national coverage presented different characteristics among themselves. Most of them were population-based, which makes the prevalence obtained from such systems less susceptible to biases, compared to those obtained from hospital records.5,16 Hospital-based programs may be an interesting choice, especially in countries with incipient records and/or limited financial resources; in addition, there is a possibility of these same programs expanding into population-based programs in the future.5,17 It is also important to mention that some registers have complemented their information through active search, such as review of hospital discharge reports (for example some States of the United States),18 perinatal audit (Australia and New Zealand)19 and linkage between databases (Scotland).20
What, when and how to notify congenital anomalies were also revised questions. Most registers showed compulsory notifications, especially related to major anomalies according to ICD, among live births, stillbirths and children aged equal to or less than 1 year.
Although the study investigated only registers with national coverage, the proportion of births covered annually varied widely. The Brazilian register - Live Birth Information System (Sinasc) - presented the highest absolute number of births covered annually. Sinasc uses the Declaration of Live Birth, a nationally standardized document, in which data on the presence and type of congenital anomaly have been recorded since 1999.21,22
Although hospital surveillance has been carried out in a few hospitals in Brazil through the Latin American Collaborative Study of Congenital Malformations (ECLAMC), the surveillance of congenital anomalies has not been performed systematically yet, throughout the national territory. However, a national surveillance model has been structured within the Health Surveillance Secretariat of the Brazilian Ministry of Health, in articulation with other secretariats of the agency, members of the academic community and medical societies.23-25
This study presented some limitations, that is, some registers with national coverage may not have been retrieved through the methodological approach used, due to the lack of material published online. In addition, registers are dynamic and some characteristics, such as ‘coverage’ can change over time.
In conclusion, this study reviewed the main registers of congenital anomalies with national coverage around the world. A total of 40 registers were analyzed and presented different characteristics, constituting consultation material for professionals interested in the theme and, above all, providing subsidies for reflections on surveillance activities and characteristics that are desirable or possible to be implemented, taking into consideration the reality of each nation.
REFERENCES
1. World Health Organization. Congenital anomalies [Internet]. Geneva: WHO; 2020 [acesso 28 May 2020]. Disponível em: Disponível em: https://www.who.int/health-topics/congenital-anomalies#tab=tab_1 [ Links ]
2. Thong M-K. Birth defects registries in the genomics era: challenges and opportunities for developing countries. Front Pediatr. 2014 Jun 16;2:60. doi: https://doi.org/10.3389/fped.2014.00060. [ Links ]
3. Lechat MF, Dolk H. Registries of congenital anomalies: EUROCAT. Environ Health Perspect. 1993;101 (Suppl 2):153-7. doi: http://dx.doi.org/10.1289/ehp.93101s2153. [ Links ]
4. Moro A, Invernizzi N. A tragédia da talidomida: a luta pelos direitos das vítimas e por melhor regulação de medicamentos. Hist Cienc SaudeManguinhos. 2017 Jul;24(3):603-22. doi: http://dx.doi.org/10.1590/S0104-59702017000300004. [ Links ]
5. World Health Organization. Birth defects surveillance: a manual for programme managers. Geneva: HOW; 2014. [ Links ]
6. Cardoso-dos-Santos AC, Magalhães VS, Medeiros-de-Souza AC, Bremm JM, Alves RFS, Araujo V, EM, et al. International collaboration networks for the surveillance of congenital anomalies: a narrative review. Epidemiol Serv Saude. 2020;29(4):e2020093.. doi: https://doi.org/10.5123/S1679-49742020000400003. [ Links ]
7. United Nations. World Economic situation and prospects. New York; UN; 2020 [acesso 21 Jul 2020]. Disponível em: Disponível em: https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/WESP2020_Annex.pdf [ Links ]
8. Penchaszadeh VB. Preventing congenital anomalies in developing countries. Community Genet. 2002;5(1):61-9. doi: https://doi.org/10.1159/000064632. [ Links ]
9. Miller JR, Lowry RB. Birth defects registries and surveillance. In: Wilson JG, Fraser FC, editors. Comparative, maternal, and epidemiologic aspects. Boston, MA: Springer; 1977 [acesso 22 lul. 2020].. doi: http://doi.org/10.1007/978-1-4615-8936-5_8. [ Links ]
10. Centers for Disease Control and Prevention. Birth defects surveillance course overview: Atlanta: CDC; 2019 [acesso 23 Jul 23]. Disponível em: Disponível em: https://www.cdc.gov/ncbddd/birthdefects/surveillancemanual/facilitators-guide/course-overview.html [ Links ]
11. Victora CG, Aquino EM, Leal MC, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet. 2011 May 28;377(9780):1863-76. doi: http://doi.org/10.1016/S0140-6736(11)60138-4. [ Links ]
12. Weatherall JAC, Haskey JC. Surveillance of malformations. Br Med Bull. 1976;32(1):39-44. doi: https://doi.org/10.1186/s12884-019-2542-x. [ Links ]
13. Wertelecki W. Birth defects surveillance in Ukraine: a process. J Appl Genet. 2006;47(2):143-9. doi: http://doi.org/10.1007/BF03194614. [ Links ]
14. Ministério da Saúde (BR) BSíndrome congênita associada à infecção pelo vírus Zika. Bol Epidemiol. 2020;51(47):1-31. [ Links ]
15. Kucêra MJ. Congenital malformation surveillance systems. Int J Epidemiol. 1986;15(3):430. doi: https://doi.org/10.1093/ije/15.3.430. [ Links ]
16. Dai L, Zhu J, Liang J, Wang Y-P, Wang H, Mao M. Birth defects surveillance in China. World J Pediatr. 2011;7(4):302-10. doi: doi: https://doi.org/10.1007/s12519-011-0326-0. [ Links ]
17. Durán P, Liascovich R, Barbero P, Bidondo MP, Groisman B, Serruya S, et al. Sistemas de vigilancia de anomalías congénitas en América Latina y el Caribe: presente y futuro. Rev Panam Salud Publica. 2019;43:e44. doi: http://doi.org/10.26633/rpsp.2019.44. [ Links ]
18. Centers for Disease Controle and Prevention. State-based birth defects tracking systems [Internet]. Atlanta: CDC; 2020 [acesso 28 maio 2021]. Disponível em: Disponível em: https://www.cdc.gov/ncbddd/birthdefects/states/index.html [ Links ]
19. Australian & New Zealand Neonatal Network (ANZNN). [Internet]. Sydney: NPESU; 2013 [acesso 28 maio 2021]. Disponível em: Disponível em: https://npesu.unsw.edu.au/data-collection/australian-new-zealand-neonatal-network-anznn [ Links ]
20. European Commission. Scottish linked routine data congenital anomaly register [Internet]. 2020 [acesso 23 jul. 2020]. Disponível em: Disponível em: https://eu-rd-platform.jrc.ec.europa.eu/eurocat/eurocat-members/registries/scottish_en [ Links ]
21. Brasil. Lei n. 13.693/18 de 10 de julho de 2018, . Institui o dia nacional de doenças raras [Internet]. Brasília, DF: Diário Oficial da União [acesso 19 fev. 2020]. Disponível em: Disponível em: https://presrepublica.jusbrasil.com.br/legislacao/599358970/lei-13693-18 [ Links ]
22. Luquetti DV, Koifman RJ. Surveillance of birth defects: Brazil and the US. Cien Saude Colet. 2011;16(suppl 1):777-85. doi: https://doi.org/10.1590/S1413-81232011000700008. [ Links ]
23. Ministério da Saúde (BR). Anomalias congênitas no Brasil, 2010 a 2018: análise dos dados de sistemas de informação para o fortalecimento da vigilância e atenção em saúde. Bol Epidemil. 2021 [acesso 10 jul. 2020];52(6):1-22. Disponível em: Disponível em: https://bit.ly/32S8f8h [ Links ]
24. Cardoso-dos-Santos AC, Medeiros-de-Souza AC, Bremm JM, Alves RFS, Araújo VEM, Leite JCL, et al. List of priority congenital anomalies for surveillance under the Brazilian Information system on live births. Epidemiol Serv Saude. 2021;30(1):e2020835. doi: http://dx.doi.org/10.1590/s1679-49742021000100030. [ Links ]
25. Ministério da Saúde (BR). Saúde Brasil 2018: uma análise da situação de saúde e das doenças e agravos crônicos: desafios e perspectivas [Internet]. Brasília, DF: MS; 2019 [acesso 10 jul. 2020]. Disponível em: Disponível em: https://bvsms.saude.gov.br/bvs/publicacoes/saude_brasil_2018_analise_situacao_saude_doencas_agravos_cronicos_desafios_perspectivas.pdf [ Links ]
Associate Editor: Bárbara Reis-Santos - orcid.org/0000-0001-6952-0352
Received: February 04, 2021; Accepted: May 24, 2021











 texto em
texto em 


