Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.31 no.1 Brasília 2022 Epub 25-Mar-2022
http://dx.doi.org/10.1590/s1679-49742022000100006
Original article
Multimorbidity and health care of community health workers in Vitória, Espírito Santo, Brazil, 2019: a cross-sectional study
1 Universidade Federal do Espírito Santo, Programa de Pós-Graduação em Saúde Coletiva, Vitória, ES, Brazil
2 Universidade Federal do Espírito Santo, Programa de Pós-Graduação em Nutrição e Saúde, Vitória, ES, Brazil
3 Universidad de las Américas Puebla, Ciencias de la Salud, San Andrés Cholula, PUE, Mexico
4 Universidade do Estado do Rio de Janeiro, Instituto de Medicina Social, Rio de Janeiro, RJ, Brazil
Objective
To assess health conditions, health care and lifestyle habits of community health workers (CHW) in Vitória, Espírito Santo, Brazil.
Methods
This was a cross-sectional study using baseline data from an intervention study. Biochemical, anthropometric and hemodynamic examinations and interviews were carried out between October 2018 and March 2019 in Vitória. Appropriate statistical tests, in accordance with the sample design, were performed using SPSS software version 21.0, adopting p<0.05.
Results
We assessed 262 CHWs with a mean age of 46.1±9.3 years. High prevalence of prediabetes (22.9%), diabetes mellitus (17.2%), hypertension (37.0%), obesity (39.8%), hypercholesterolemia (57.3%), hypertriglyceridemia (27.1%), multimorbidity (40.8%), physical inactivity (60.9%) and use of anxiolytics/antidepressants (22.5%) was found. Some 40% of the CHWs had three or more morbidities.
Conclusion
High percentages of chronic diseases, multimorbidity, sedentary lifestyle and use of anxiolytics/antidepressants were found in CHWs in Vitória.
Keywords: Community Health Workers; Multimorbidity; Nutritional Status; Chronic Disease; Lifestyle; Cross-Sectional Studies
Main results
Study contributions
We identify high prevalence of chronic diseases, sedentary lifestyle and use of antidepressants/anxiolytics among community health workers (CHW) in Vitória, ES. Some 40% had three or more morbidities.
Implications for services
Health professionals who work with health promotion and disease prevention are ill and need treatment and care. This condition impacts the quality of life of CHWs, as well as their work performance in health services.
Perspectives
Our findings reinforce the need to care for carers, especially those who are more socially and economically vulnerable, as is the case of CHWs. Improving the health status of CHWs is fundamental for strengthening the Brazilian National Health System.
Introduction
Community health workers (CHWs) are part of the teams of the Family Health Strategy of the Brazilian National Health System (SUS)1 and work on the front line of Primary Health Care, forming a link between the community and the health service. Standing out among the attributions of CHWs are the care of families who live in a given geographical area, health surveillance and the carrying out of educational activities among the population.1
Studies developed in the Southeast, South and Northeast regions of the country found that CHWs were mostly in the 24-45 age group, female, had complete high school education and monthly family income of two to four minimum wages.2,3 In the state of Rio Grande do Sul, 21.9% of the 564 CHWs studied reported being diagnosed as having hypertension and 5.5% as having diabetes mellitus.4 These results are similar to those found for CHWs in a municipality in the state of Rio Grande do Norte.5 Both in Rio Grande do Sul4 and in the capital of the state of Paraíba, João Pessoa (163 CHWs),6 a high percentage of overweight CHWs was found, 69.7% and 37.5% respectively, whereby the difference in these percentages may possibly be related to the fact that one of these studies used self-reported information,4 while the other used direct measurement.6
Simultaneous occurrence of two or more chronic non-communicable diseases in an individual, i.e. multimorbidity, increases risk of death, demand for health care and consequently costs imposed on the sector.7 Data from the 2013 National Health Survey indicate that 24.2% of Brazilian adults had two or more morbities.8 The relevance of the topic recommends investigation of occurrence of multimorbidity among healthcare workers.
The daily activities of CHWs in the community probably increase their exposure to situations of vulnerability while working, such as the demands of the population under their care and insecurity resulting from working in peripheral neighborhoods, which can affect the quality of life and health conditions of these workers.9 In this sense, studies with CHWs have been conducted in Brazil, mainly to identify the work processes involved in their jobs, their socio-demographic and economic reality and the impact of these aspects on their quality of life and mental health.2,10 Despite the limited number of these studies and their clearly restricted samples of CHWs, there is evidence that this is a group of workers with compromised physical and mental health, even though they live in the Primary Health Care context and undertake actions to promote health and prevent diseases and illnesses.4-6,10
To date, no research has been identified that investigates the health conditions of CHWs based on objective health information, only those using self-reported data from a limited number of chronic non-communicable disease. Information about the presence of multimorbidity in these health workers is scarce, for all the Brazilian Federative Units. Given this scenario, the present study aimed to assess health conditions, care of own health and lifestyle habits of CHWs in Vitória, state of Espírito Santo, Brazil.
Methods
Study design
This was a cross-sectional study using baseline data from an intervention study aimed at assessing the impact of a CHW training on nutrition education.11
Vitória, capital of the state of Espírito Santo, covers an area of 96.5 km2 and has around 362,000 inhabitants, of whom 245,516 were registered in the participating health centers during the study period. The municipality has 23 Family Health centers and two Primary Healthcare centers.
Participant sample and selection
All 375 CHWs who, according to the Vitória Municipal Government, were working at the time of participant recruitment in Family Health centers or Primary Healthcare centers in the municipality were eligible for the study. As this was a study that aimed to characterize health conditions and care, pregnant CHWs were excluded from the analysis due to metabolic changes resulting from pregnancy.
The CHWs were contacted by the researchers in order to present the study, invite them to take part and schedule data collection.
Data collection
Examinations and interviews took place at the Cardiovascular Research Clinic at the Universidade Federal do Espírito Santo University Hospital. Data collection took place from October 2018 to March 2019.
The interviews, clinical examinations and biochemical tests were performed by trained researchers on pre-scheduled days in the morning. The data collection and treatment methodology is detailed below.
a) Socioeconomic and lifestyle habit assessment
Demographic, socioeconomic and lifestyle habit data were obtained during the interviews by administering questionnaires with validated scales and questions developed by the researchers. The respondents’ age was categorized into two groups according to the median (<45 years; ≥45 years). Although there is no consensual definition as to being middle aged, we suggest an age group for CHWs between 40 and 59 years old,12 and this includes the sample median. Each participant was asked about the number of years they had worked as a CHW, as well as the their level of schooling by asking the question “Up to what grade did you study?”, whereby the variable was categorized into: complete elementary education; complete high school education; complete higher education.
Socioeconomic status was classified using the criteria of the Brazilian Association of Survey Companies (ABEP)13 i.e. socioeconomic classes: A and B; C; D and E. Reported race/skin color was categorized as white, black or brown; while marital status was classified as married, single or separated/widowed. Self-perceived health status was recorded as follows: very good; good; and regular/poor/very poor. Data on tobacco smoking and alcoholic beverage consumption were obtained by direct questions (no; yes).
Level of physical activity was estimated using the International Physical Activity Questionnaire (IPAQ) - long form, based on the ‘leisure time’ and ‘transportation’ activity domains.14 The pattern of the different domains of physical activity was reported in minutes per week, consisting of multiplying weekly frequency by the duration of each of the activities performed. Participants were considered active when they undertook ≥150 minutes per week of moderate/vigorous physical activity, insufficiently active when they did moderate/vigorous physical activity for <150 to >10 minutes per week, and sedentary when total physical activity was done for ≤10 minutes per week.15
Time spent sitting was assessed by using two questions from the IPAQ time spent sitting domain to identify how many hours per day, on weekdays and at the weekend, the individual remained sitting. The sum of the hours of time spent sitting during the week was divided by 7 and expressed as average hours per day. Screen time was obtained by asking questions about the use of screen devices at work or when studying and during leisure time (screen devices included smartphones, television, computers and video games), and was calculated by adding together screen time when working/studying and during leisure time, divided by 7, to express screen time in hours per day.
b) Biochemical tests, clinical examinations and care of own health
The biochemical tests were performed with blood samples collected by venipuncture following overnight fasting (10-14 hours). Blood glucose (mg/dL), insulin (mcUI/mL), total cholesterol and cholesterol fractions (mg/dL) and triglycerides (mg/dL) were measured. After blood collection, participants who stated they did not have diabetes mellitus and/or had not undergone bariatric surgery drank a solution containing 75g of flavored dextrose, for a new blood collection two hours after overload. All samples were sent to the accredited central laboratory (Laboratório Tommasi, Vitória, ES).
Still without having eaten anything and with their bladder empty, participants were submitted to anthropometric and hemodynamic tests, according to a standardized protocol. Height was measured by a wall stadiometer (Seca®, Hamburg, BRD) with a 0.1cm scale, with the individual in an upright position, barefoot and looking straight ahead. Height was measured during the inspiratory period of the breathing cycle. Weight and percentage body fat (PBF) were measured with the participant still barefoot, wearing light clothes, on Inbody® 230 - Body Composition Analyzer weighing scales. In the case of those with pacemakers and/or metallic prostheses in the upper and/or lower limbs, only body weight was measured, using electronic scales (Toledo®) with 200kg capacity and 50g precision.16
Taking the weight and height measurements, body mass index (BMI) was calculated by dividing weight (kg) by height (m) squared. We adopted the cut-off points recommended by the World Health Organization (WHO) for classification of nutritional status: low and normal weight (BMI <25.0 kg/m2); overweight (BMI ≥25.0 and <30.0 kg/m2); and obesity (BMI ≥30.0 kg/m2).17
Waist circumference was measured with the participant in an upright position, breathing normally, feet together, upper clothing raised and arms crossed in front of the chest. This measurement was taken with a non-stretch tape measure at the midpoint between the iliac crest and the lowest rib. When it was not possible to follow this protocol, the measurement was taken at the navel.16 Abdominal obesity was defined as being when waist circumference ≥88cm for females and ≥102cm for males.17
Blood pressure was measured after resting for five minutes, using a validated Omron® - HEM 705CPINT automatic device. To do so, the participant remained seated, without crossing their legs, with their feet flat on the floor, in a quiet, temperature-controlled environment (20-24ºC). Three measurements were taken on the left arm at one-minute intervals, and the average of the last two readings was considered to be casual blood pressure.18 The following were considered in order to classify hypertension: (i) use of antihypertensive medication and/or (ii) systolic blood pressure (SBP) ≥140 mmHg and/or (iii) diastolic blood pressure (DBP) ≥90 mmHg.19
Definition of diabetes mellitus cases was based on the presence of at least one of the following three criteria: (i) reported hypoglycemic medication use (insulin or oral hypoglycemic agent) and/or (ii) fasting blood glucose ≥126 mg/dL and/or (iii) blood glucose after 120 minutes of glucose solution ≥200 mg/dL.19 The Homeostasis Model Assessment (HOMA) index was calculated using the following formula:
Presence of prediabetes was defined when fasting blood glucose was ≥100 and <126 mg/dL.19 In order to calculate the number of associated morbidities and thus classify multimorbidity, the presence of the following clinical conditions was considered: diabetes mellitus, hypertension, BMI ≥30.0 kg/m2, abdominal obesity, hypercholesterolemia (total cholesterol ≥190 mg/dL)20 and hypertriglyceridemia (triglycerides ≥150 mg/dL).20
In order to calculate the number of associated morbidities and thus classify multimorbidity, the presence of the following clinical conditions was considered: diabetes mellitus, hypertension, BMI ≥30.0 kg/m², abdominal obesity, hypercholesterolemia (total cholesterol ≥190 mg/dL)20 and hypertriglyceridemia (triglycerides ≥150 mg/dL).20
Metabolic syndrome (SM) was defined by the presence of at least three of the following criteria21 abdominal obesity; High Density Lipoprotein (HDL) cholesterol <50 mg/dL for females and <40 mg/dL for males; triglycerides ≥150 mg/dL; SBP ≥130 mmHg and/or DBP ≥85 mmHg (or use of medication for hypertension); and fasting blood glucose ≥100 mg/dL (or use of medication for diabetes mellitus).
Medication use in the last two weeks prior to the interview was identified. Participants were encouraged to detail this information by providing the medication trade name and dosage. Thus, the criteria for assessing care of own health were: controlled hypertension (blood pressure <140/90 mmHg20 and use of antihypertensive medication); and controlled diabetes mellitus (fasting blood glucose <130 mg/dL19 and use of antidiabetic medication).
Statistical analysis
For the purposes of data analysis, descriptive statistics were applied using simple and percentage frequency, as well as measures of central tendency and dispersion. Data normality was verified by the Kolmogorov-Smirnov test. Pearson’s chi-square test and Fisher’s exact test were used to compare proportions, according to sex and age group. Continuous variables were presented as median (interquartile range) or mean (standard deviation). Comparison of independent sample means was done using Student’s t-test and the Mann-Whitney test, to assess association between biochemical and clinical parameters, according to sex and age group.
All analyses were conducted using the Statistical Package for the Social Sciences (SPSS) version 21.0. Statistical significance was set at a p-value of <0.05.
Ethical considerations
The study project was approved by the Human Research Ethics Committee of the Centro de Ciências da Saúde, Universidade Federal do Espírito Santo (Certificate of Submission for Ethical Appraisal No. 88008418.6.0000.5060; Opinion No. 2.669.734), after authorization had been given by the Vitória Municipal Health Department and the Espírito Santo State Health Department. The project was registered with the WHO (UTN - U1111-1232-4086) and with the Brazilian Clinical Trials Registry (REQ: RBR-4z26bv). CHWs who agreed to take part in the study signed a Free and Informed Consent form.
Results
Of the 375 CHWs eligible for the study, 263 (70.1%) showed up for the examinations and interviews, and had their data collected. After exclusion of one pregnant woman, data from 262 CHWs were included in the analysis. The sociodemographic characteristics of the participants, according to sex and age group, are shown in Table 1.
Table 1 Sociodemographic characteristics of community health workers by sex and age group, CACEA Study, Vitória, Espírito Santo, Brazil, 2018-2019
| Variables | Total | Sex | p-value | Age group (years) | p-value | ||
|---|---|---|---|---|---|---|---|
| Female | Male | <45 | ≥45 | ||||
| n (%) | n (%) | n (%) | n (%) | n (%) | |||
| 262 | 247 (94.3) | 15 (5.7) | 130 (49.6) | 132 (50.4) | |||
| Age (years)a | 46.1±9.3 | 46.4±9.2 | 40.6±8.6 | 0.023b | 38.2±3.8 | 53.8±5.9 | <0.001b |
| Race/skin color | 0.774d | 0.012c | |||||
| White | 49 (18.7) | 47 (19.0) | 2 (13.3) | 18 (13.8) | 31 (23.5) | ||
| Black | 82 (31.3) | 76 (30.8) | 6 (40.0) | 51 (39.2) | 31 (23.5) | ||
| Brown | 131 (50.0) | 124 (50.2) | 7 (46.7) | 61 (46.9) | 70 (53.0) | ||
| Schooling | 0.418d | 0.034d | |||||
| Complete elementary education | 11 (4.2) | 10 (4.0) | 1 (6.7) | 6 (4.6) | 5 (3.8) | ||
| Complete high school education | 213 (81.3) | 202 (81.8) | 11 (73.3) | 98 (75.4) | 115 (87.1) | ||
| Complete higher education | 38 (14.5) | 35 (14.2) | 3 (20.0) | 26 (20.0) | 12 (9.1) | ||
| Currently studying | 27 (10.3) | 23 (9.3) | 4 (26.7) | 0.055d | 22 (16.9) | 5 (3.8) | <0.001d |
| Socioeconomic class | 0.473d | 0.547d | |||||
| A and B | 103 (39.3) | 95 (38.5) | 8 (53.3) | 47 (36.2) | 56 (42.4) | ||
| C | 154 (58.8) | 147 (59.5) | 7 (46.7) | 81 (62.3) | 73 (55.3) | ||
| D and E | 5 (1.9) | 5 (2.0) | - | 2 (1.5) | 3 (2.3) | ||
| Marital status | 0.015d | <0.001c | |||||
| Single | 45 (17.2) | 38 (15.4) | 7 (46.7) | 32 (24.6) | 13 (9.8) | ||
| Married | 174 (66.4) | 167 (67.6) | 7 (46.7) | 87 (66.9) | 87 (65.9) | ||
| Separated or widowed | 43 (16.4) | 42 (17.0) | 1 (6.7) | 11 (8.5) | 32 (24.3) | ||
a) Data expressed in means ± standard deviation; b) Mann-Whitney test; c) Pearson’s chi-square test; d) Fisher’s exact test.
The sample was composed mostly of female participants (94.3%), of brown race/skin color (50.0%), with complete high school education (81.3%), belonging to socioeconomic class C (58.8%), married (66.4%) and whose mean age was 46.1±9.3 years (Table 1). Mean length of time working as a CHW was 16.2±4.8 years.
Significant differences were found for age and marital status in relation to the ‘sex’ variable (p-value=0.023 and p-value=0.015, respectively). All sociodemographic variables presented in Table 1 were statistically different in relation to age group, with the exception of socioeconomic class.
Taking the total sample, 60.9% were sedentary (Table 2). A higher percentage of current smokers was found among those aged ≥45 years (p-value<0.001). Male participants had a higher percentage of alcoholic beverage consumption and higher mean time spent sitting, when compared to females (p-value=0.050 and p-value=0.001, respectively). Younger individuals had higher mean screen time and time spent sitting (p=0.021 and 0.007, respectively), compared to those aged ≥45 years (Table 2).
Table 2 Lifestyle habits and health characteristics of community health workers by sex and age group, CACEA Study, Vitória, Espírito Santo, Brazil, 2018-2019
| Variables | Total | Sex | p-value | Age group (years) | p-value | ||
|---|---|---|---|---|---|---|---|
| Female | Male | <45 | ≥45 | ||||
| n (%) | n (%) | n (%) | n (%) | n (%) | |||
| 262 | 247 (94.3) | 15 (5.7) | 130 (49.6) | 132 (50.4) | |||
| Self-perceived health status | 0.210d | 0.736d | |||||
| Very good | 44 (16.8) | 39 (15.8) | 5 (33.3) | 24 (18.5) | 20 (15.2) | ||
| Good | 136 (51.9) | 129 (52.2) | 7 (46.7) | 65 (50.0) | 71 (53.8) | ||
| Regular, poor or very poor | 82 (31.3) | 79 (32.0) | 3 (20.0) | 41 (31.5) | 41 (31.0) | ||
| Tobacco smoking | 10 (3.8) | 8 (3.2) | 2 (13.3) | 0.100d | 1 (0.8) | 9 (6.8) | <0.001d |
| Alcoholic beverage consumption | 111 (42.4) | 101 (40.9) | 10 (66.7) | 0.050c | 58 (44.6) | 53 (40.2) | 0.465c |
| Physical activitya | 0.166d | 0.372c | |||||
| Active | 76 (29.1) | 69 (28.0) | 7 (46.7) | 43 (33.1) | 33 (25.2) | ||
| Insufficiently active | 26 (10.0) | 24 (9.8) | 2 (13.3) | 12 (9.2) | 14 (10.7) | ||
| Sedentary | 159 (60.9) | 153 (62.2) | 6 (40.0) | 75 (57.7) | 84 (64.1) | ||
| Physical activity (minutes/week)b | 107.6±174.1 | 103.2±169.9 | 179.3±228.3 | 0.099f | 123.9±187.5 | 91.4±158.8 | 0.195f |
| Screen time (hours/day)b | 3.6±2.2 | 3.6±2.2 | 3.8±1.8 | 0.473f | 3.9±2.2 | 3.3±2.2 | 0.021f |
| Time spent sitting (hours/day)b | 3.7±1.9 | 3.7±1.9 | 4.2±1.9 | 0.001e | 3.9±1.9 | 3.6±1.9 | 0.007e |
| Diabetes mellitus | 45 (17.2) | 42 (17.0) | 3 (20.0) | 0.727d | 14 (10.8) | 31 (23.5) | 0.006c |
| Hypertension | 97 (37.0) | 91 (36.8) | 6 (40.0) | 0.806c | 29 (22.3) | 68 (51.5) | <0.001c |
| Hypercholesterolemia (≥190 mg/dL) | 150 (57.3) | 145 (58.7) | 5 (33.3) | 0.063d | 60 (46.2) | 90 (68.2) | <0.001c |
| Hypertriglyceridemia (≥150 mg/dL) | 71 (27.1) | 68 (27.5) | 3 (20.0) | 0.766d | 27 (20.8) | 44 (33.3) | 0.022c |
| Nutritional statusa | 0.562d | 0.677c | |||||
| Normal and low weight | 68 (26.1) | 63 (25.6) | 5 (33.3) | 37 (28.4) | 31 (23.7) | ||
| Overweight | 89 (34.1) | 83 (33.7) | 6 (40.0) | 43 (33.1) | 46 (35.1) | ||
| Obesity | 104 (39.8) | 100 (40.7) | 4 (26.7) | 50 (38.5) | 54 (41.2) | ||
| Abdominal obesity | 132 (50.4) | 128 (51.8) | 4 (26.7) | 0.067d | 59 (45.4) | 73 (55.3) | 0.138c |
| Metabolic syndrome | 79 (30.2) | 75 (30.4) | 4 (26.7) | 1.000d | 26 (20.0) | 53 (40.2) | <0.001c |
a) Variable with missing data (n=261); b) Data expressed in means ± standard deviation; c) Pearson’s chi-square test; d) Fisher’s exact test; e) Student’s t-test; f) Mann-Whitney test.
Table 2 also shows the percentages of diabetes mellitus (17.2%), hypertension (37.0%), hypercholesterolemia (57.3%), hypertriglyceridemia (27.1%), obesity (39.8%), abdominal obesity (50.4%) and metabolic syndrome (30.2%). All of these, with the exception of obesity and abdominal obesity, were significantly higher among individuals aged ≥45 years. Sixty CHWs (22.9%) were identified as having prediabetes.
Figure 1 shows the most frequent percentages of multimorbidity. Of the CHWs studied, 40.8% had three or more morbidities, the most frequent being the combination of BMI ≥30kg/m2, abdominal obesity and hypercholesterolemia (22.0%). No statistically significant differences were observed between multimorbidity frequency and sex (p-value=0.061); however, 66.4% of individuals with three or more morbidities were aged ≥45 years (p-value<0.001).
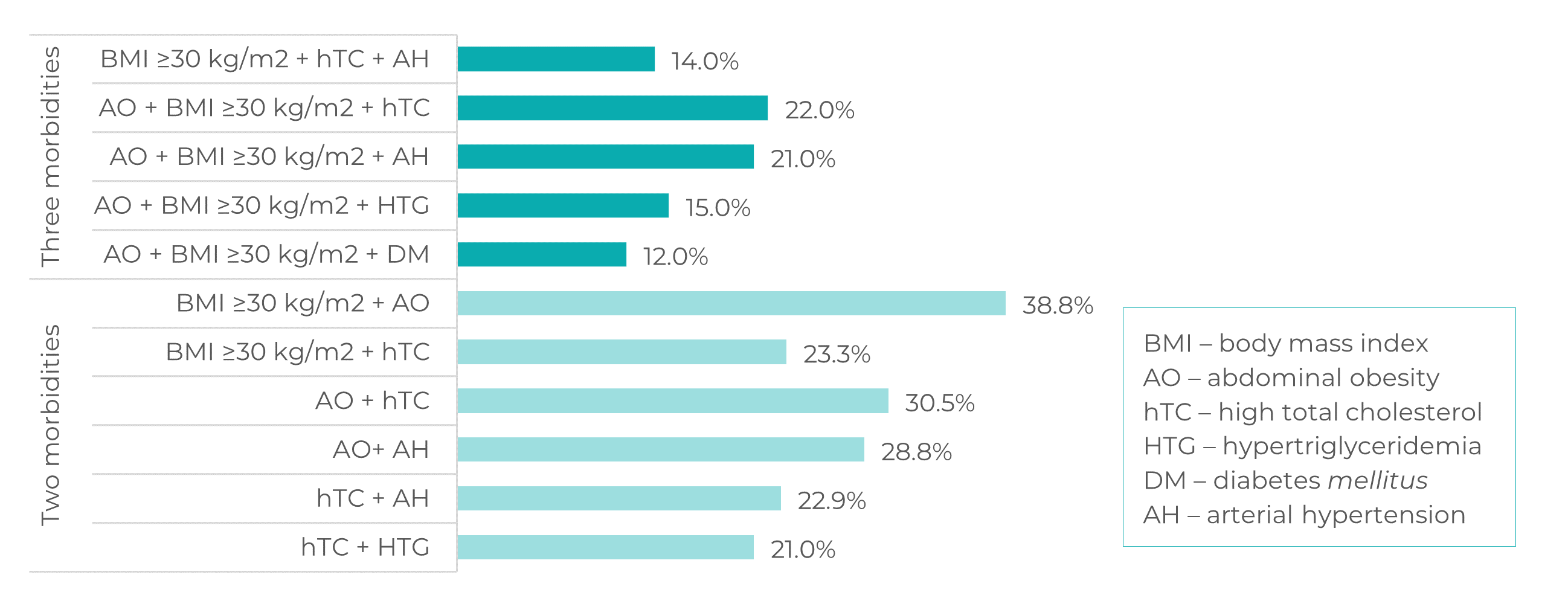
Figure 1 Most frequent percentages of two and three morbidities among community health workers, CACEA Study, Vitória, Espírito Santo, Brazil, 2018-2019
Table 3 shows the biochemical and clinical parameters, according to sex and age group. Female CHWs had higher values for total cholesterol (p-value=0.049), HDL-cholesterol (p-value=0.004) and PBF (p-value<0.001). Comparing biochemical and clinical parameters by age groups, total cholesterol (p-value<0.001), Lower Density Lipoprotein (LDL) cholesterol (p-value<0.001), triglycerides (p-value=0.008), PBF (p-value=0.047) and waist circumference (p-value=0.040) were higher in subjects aged ≥45 years.
Table 3 Biochemical and clinical parameters of community health workers by sex and age group, CACEA Study, Vitória, Espírito Santo, Brazil, 2018-2019
| Variables | Total | Sex | p-value | Age group (years) | p-value | ||
|---|---|---|---|---|---|---|---|
| Female | Male | <45 | ≥45 | ||||
| (n=262) | (n=247) | (n=15) | (n=130) | (n=132) | |||
| Colesterol total (mg/dL)a | 198.9±37.7 | 200.1±38.0 | 180.3±27.7 | 0.049c | 188.4±31.5 | 209.3±40.5 | <0.001c |
| HDL-colesterol (mg/dL)b | 48.5 (43.0;58.0) | 49.0 (43.0;58.0) | 42.0 (36.0;49.0) | 0.004d | 49.0 (42.7;59.2) | 48.0 (43.0;56.7) | 0.388d |
| LDL-colesterol (mg/dL)a | 121.7±35.0 | 122.4±35.5 | 110.8±23.0 | 0.209c | 111.6±28.0 | 131.6±38.2 | <000.1c |
| Triglicerídeos (mg/dL)b | 114.5 (85.7;154.2) | 115.0 (85.0;155.0) | 111.0 (93.0;144.0) | 0.911d | 103.5 (81.5;140.0) | 99.0 (92.0;110.0) | 0.008d |
| Glicemia em jejum (mg/dL) | 96.0 (88.0;105.0) | 96.0 (88.0;105.0) | 96.0 (92.0;104.0) | 0.606d | 92.0 (86.0;100.0) | 11.6 (7.6;18.3) | 0.606d |
| Insulina (mcUI/mL)b | 12.0 (8.1;18.3) | 12.1 (8.3;18.4) | 8.8 (5.4;17.1) | 0.256d | 12.6 (8.8;19.0) | 2.8 (1.7;4.6) | 0.851d |
| Índice HOMA-IRb | 2.9 (1.8;4.4) | 2.9 (1.8;4.4) | 1.0 (1.2;4.0) | 0.287d | 2.9 (1.8;4.3) | 122.0 (91.5;165.7) | 0.274d |
| Peso corporal (kg)a | 74.8±15.5 | 74.4±15.6 | 80.7±13.9 | 0.133c | 75.4±15.4 | 74.2±15.6 | 0.489c |
| IMC (kg/m2)a | 28.9±5.5 | 29.0±5.5 | 26.8±4.8 | 0.125c | 28.6±5.5 | 29.2±5.4 | 0.386c |
| PGC (%)a | 38.0±8.5 | 39.1±7.1 | 20.4±10.8 | <0.001c | 36.9±8.4 | 39.0±8.6 | 0.047c |
| CC (cm)a | 90.8±14.8 | 90.8±14.8 | 90.2±14.7 | 0.881c | 88.9±13.8 | 92.7±15.5 | 0.040c |
| PAS (mmHg)b | 113.5 (105.5;123.1) | 114.0 (105.5;123.0) | 113.0 (110.5;136.5) | 0.302d | 110.5 (104.5;118.0) | 117.2 (109.0;127.3) | 0.302d |
| PAD (mmHg)a | 74.6±9.4 | 74.5±9.0 | 76.9±14.7 | 0.346c | 74.6±9.5 | 74.7±9.4 | 0.907c |
Legend: HDL: High Density Lipoprotein; LDL: Lower Density Lipoprotein; HOMA-IR Index: Homeostases Model Assessment-Insulin Resistance; BMI: body mass index; PBF: percentage body fat; WC: waist circumference; SBP: systolic blood pressure; DBP: diastolic blood pressure. a) Means ± standard deviation for parametric variables; b) Medians (interquartile range) for non-parametric variables; c) Student’s t-test; d) Mann-Whitney test.
We classified 10 (22.2%) CHWs as having diabetes mellitus and 9 (9.3%) as having hypertension, but who reported that they had not been previously diagnosed as having these conditions and therefore did not use specific medication for them (Table 4). Of those who had prior diagnosis, 20% were not on medication for diabetes mellitus or hypertension. Moreover, about 23% had higher than normal blood glucose and 22.5% reported use of anxiolytic and/or antidepressant medication, with no significant difference between both age groups (p-value=0.206), although use of this medication was associated with poorer self-perceived health status (p-value<0.010).
Table 4 Knowledge and control of diseases and medication use among community health workers, CACEA Study, Vitória, Espírito Santo, Brazil, 2018-2019
| Variables | na | % |
|---|---|---|
| Diseases | ||
| Classified as having diabetes mellitus without prior diagnosis | 10 | 22.2 |
| Classified as having hypertension without prior diagnosis | 9 | 9.3 |
| Controlled diabetes mellitusb | 15 | 33.3 |
| Controlled hypertensionc | 71 | 73.2 |
| Medication use | ||
| Antidiabetics | 33 | 12.6 |
| Antihypertensives | 84 | 32.1 |
| Hypolipidemics | 20 | 7.6 |
| Anxiolytics and/or antidepressives | 59 | 22.5 |
| For gastric problems | 39 | 14.9 |
a) n=262; b) n=45; c) n=95.
Discussion
The CHWs we studied were mostly female, married, of brown skin color, with complete high school education and belonging to socioeconomic class C. They had high percentages of prediabetes, diabetes mellitus, hypertension, obesity, cholesterol, hypertriglyceridemia, metabolic syndrome and sedentarism. About 40% had three or more associated morbidities, and of those previously diagnosed with diabetes mellitus and/or hypertension, one-fifth were not taking medication for these conditions. Anxiolytic and/or antidepressant medication use was high, and was associated with poor self-perceived health status.
A study conducted in the Metropolitan Region of Vitória (which includes the municipalities of Cariacica, Vitória, Vila Velha and Serra), with 291 CHWs, found similar results regarding the sociodemographic characteristics and income of these professionals,2 as did studies conducted in the Northern6 and Southern regions of Brazil,3 with the exception of mean age, which in our study was higher than that found in those studies.2,3,6 Some 30% of the sample reported having worked as CHWs for a period ≥20 years (data not shown), which may explain their higher mean age in relation to peers from other locations in Brazil.
Younger individuals use screen devices more frequently and are more familiar with them;22 and mean time spent sitting is greater among those with higher levels of education.23 Both factors corroborate our findings on CWH screen time and time spent sitting. Although there is no consensus about recommended screen time for adults, the mean among the CHWs we studied was above 2 hours per day, which can be considered high. Therefore, sedentary behavior is a reality in the group studied, considering the high averages of screen time and time spent sitting, in addition to almost 61% reporting doing physical activities less than 10 minutes per week.
The relationship between adverse health conditions and age is already well established in the literature,24 which may justify our findings for older individuals. Moreover, in this study in Vitória, ES, we found a high percentage of chronic non-communicable diseases, higher than that found in a subsample of the 2013 National Health Survey from the same city.25 It should be emphasized that, although objective measurements were used in both of these studies, some of the diagnostic criteria were different, such as classification of diabetes mellitus and hypertension. In our study, we chose to increase diagnosis specificity, by using a greater number of criterias.
We found a considerable percentage of individuals who had diabetes mellitus and/or hypertension, and 13.4% of them were only classified as such during the study, i.e., they did not know their health condition until then. Even when they had prior diagnosis, a relevant percentage of CHWs did not use medication. This data is of concern, since they are professionals whose job includes raising community awareness about the need to control and adequately treat these diseases. We realize that underdiagnosis of diabetes mellitus and hypertension, which a priori are asymptomatic diseases, is still considerable, and may be reflected in lack of clinical follow-up and adequate treatment. Late diagnosis and management of chronic non-communicable diseases generates more costs for the health system and has considerable impact on terms of increasing morbidity and mortality.26
More participants in our study were classified as obese compared to CHWs assessed in other studies, such as those conducted in João Pessoa, PB,6 in the state of Rio Grande do Sul4 and in Vitória, ES.25
Female CHWs had higher total cholesterol and HDL-cholesterol values than male CHWs. This finding that may be related to their higher mean age, given the well-established relationship between age and serum lipid levels.27 Furthermore, there is evidence that sex hormones can influence HDL-cholesterol: endogenous estrogen production in premenopausal women is associated with higher levels of HDL-cholesterol.28 PBF was also higher in female CHWs, in line with the difference in the pattern of body fat distribution between the sexes.16
Age is an independent risk factor for a deteriorating lipid profile and development of cardiovascular disease.27 However, in our study, younger individuals also presented high biochemical and clinical parameters. Therefore, the sample studied, regardless of age group, presented unfavorable health conditions and multimorbidity, as well as a high percentage of anxiolytic and/or antidepressant medication use associated with poor self-perceived health status.
A study with CHWs from Pelotas, RS, Brazil, found high prevalence of stress and depression, which was measured by scales to identify symptoms and by saliva cortisol content.10 Among health professionals, these conditions are related to psychosocial and environmental risk factors to which they are exposed during their work routines.9 CHWs are members of the community in which they work and, therefore, are seen not just as neighbors, but also as facilitators of access to the local health service.9 This characteristic and other pressures inherent to the work of any health professional, are indicated as being factors that contribute to reduction in their quality of life and poorer mental health.9,10
Despite the high prevalence of chronic non-communicable diseases among Primary Health Care professionals,29 the situation of CHWs requires attention, since their socioeconomic status is generally low, which represents a risk factor for the occurrence of these diseases. The social determinants of health can hinder the incorporation of measures to prevent and control diseases and illnesses,30 given that these same professionals are responsible for raising the awareness of the community they assist.
Because it is a sample from a specific municipality, it is not possible to extrapolate its results to other locations, which we understand to be a limitation. However, the high adherence of the CHWs to our study makes it possible to consider that the sample is representative of the CHW population in Vitória. Moreover, some aspects assessed by our study were self-reported and, therefore, subject to memory bias, although it is worth highlighting the pioneer nature of this study in proposing a broad diagnosis of CHW health, through measurement and assessment of biochemical and clinical parameters, performed by a qualified team under supervision throughout the study period.
CHWs work in Primary Health Care, undertaking health promotion and disease prevention actions. We believe that assessing the health conditions of these workers can contribute to their self-care and, consequently, impact the performance of Family Health teams.
All participants received their test results with medical reports within ten days at the most, and those who presented any alteration were advised to seek treatment in the healthcare network. It is possible that their having undergone biochemical, clinical and imaging tests has encouraged them to seek treatment and change habits and lifestyles.
We conclude that the health conditions and lifestyle habits of CHW in Vitória, capital of the state of Espírito Santo, deserve attention, given the high percentage of chronic non-communicable diseases, multimorbidity and sedentary lifestyles found, in addition to early disease, considering the average age of the group. These health professionals will probably remain active indefinitely, for several years, on the labor market, pointing to the need for specific actions to prevent and treat the health problems we found.
Acknowledgements
We thank the community health workers of Vitória, ES, for their contribution to this research. We thank the Laboratório Tommasi for its analysis of the biochemical parameters.
REFERENCES
1. Ministério da Saúde (BR). Portaria nº 2.436, de 21 de setembro de 2017. Aprova a Política Nacional de Atenção Básica, estabelecendo a revisão de diretrizes para a organização da Atenção Básica, no âmbito do Sistema Único de Saúde. Diário Oficial da União, Brasília (DF), 2017 set 22, Seção 1: 68. [ Links ]
2. Garcia ACP, Lima RCD, Lima EFA, Galavote HS, Andrade MAC. The profile and work process of community health agentes. R Pesq Cuid Fundam [Internet]. 2019 [citado 2020 mar 13];11(esp 2):339-44. doi: 10.9789/2175-5361.2019.v11i2.339-344 [ Links ]
3. Carneiro VPP, Gumy MP, Otenio JK, Bortoloti DS, Castro TE, Lourenço ELB, et al. Perfil dos Agentes comunitários de saúde de um município do estado do Paraná e sua relação com plantas medicinais. Braz J of Dev [Internet]. 2020 [citado 2020 jun 23];6(1):2902-18. doi: 10.34117/bjdv6n1-209 [ Links ]
4. Silveira FDC, Fernandes CG, Almeida MDD, Aldrighi LB, Jardim VMR. Prevalência de sobrepeso e obesidade em agentes comunitários de saúde na região sul do Rio Grande do Sul, 2017. Epidemiol Serv Saúde [Internet]. 2020 [citado 2020 set 03];29:e2019447. doi: 10.5123/S1679-49742020000400013 [ Links ]
5. Dantas AAG, Oliveira NPD, Santos Silva MDF, Sousa Dantas D. Condições de saúde e estado nutricional de agentes comunitários de Saúde no interior do nordeste brasileiro. Revista Ciência Plural [Internet]. 2020 [citado 2020 mar 13];6(1):32-43. doi: 10.21680/2446-7286.2020v6n1ID17157 [ Links ]
6. Barbosa AM, Lacerda DAL. Associação entre consumo alimentar e estado nutricional em agentes comunitários de saúde. Rev Bras Ciênc Saúde [Internet]. 2017 [citado 2020 mar 13];21(3):189-96. doi: 10.22478/ufpb.2317-6032.2017v21n3.25321 [ Links ]
7. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet [Internet]. 2012 [cited 2021 jun 23];380(9836):37-43. doi: 10.1016/S0140-6736(12)60240-2 [ Links ]
8. Rzewuska M, Azevedo-Marques JM, Coxon D, Zanetti ML, Zanetti ACG, Franco LJ, et al. Epidemiology of multimorbidity within the Brazilian adult general population: evidence from the 2013 National Health Survey (PNS 2013). PloS One [Internet]. 2017 [cited 2021 jun 23];12(2):e0171813. doi: 10.1371/journal.pone.0171813 [ Links ]
9. Galavote HS, Prado TN, Maciel ELN, Lima RCD. Desvendando os processos de trabalho do agente comunitário de saúde nos cenários revelados na Estratégia Saúde da Família no município de Vitória (ES, Brasil). Cienc Saude Coletiva [Internet]. 2011[citado 2021 out 21];16(1):231-40. doi: 10.1590/s1413-81232011000100026 [ Links ]
10. Knuth BS, Cocco RA, Radtke VA, Medeiros JRC, Oses JP, Wiener CD et al. Stress, depression, quality of life and salivary cortisol levels in community health agents. Acta Neuropsychiatr [Internet]. 2016 [cited 2020 sept 10]; 28(3):165-72. doi: 10.1017/neu.2015.58 [ Links ]
11. Molina MCB, Martins HX, Siqueira JH, Oliveira AMA, Jesus HC, Pereira TSS. Impacto da capacitação de agentes comunitários de saúde em educação alimentar: aspectos metodológicos e potencialidades. R Pesq Cuid Fundam [Internet]. 2021;13:1526-35. doi: 10.9789/2175-5361.rpcfo.v13.102 [ Links ]
12. Toothman EL, Barrett AE. Mapping midlife: an examination of social factors shaping conceptions of the timing of middle age. Adv Life Course Res. 2011;16(3):99-111. doi:10.1016/j.alcr.2011.08.003 [ Links ]
13. Associação Brasileira de Empresas de Pesquisas. Critério Brasil 2018 e atualização da distribuição de classes para 2018 [Internet]. São Paulo, 2018 [citado 2020 mar 13]. Disponível em: http://www.abep.org/criterioBr/01_cceb_2018.pdf [ Links ]
14. Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, et al. Questionário Internacional de Atividade Física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde [Internet]. 2012 [citado 2020 mar 25];6(2):5-18. doi: 10.12820/rbafs.v.6n2p5-18 [ Links ]
15. World Health Organization. Global strategy on diet, physical activity and health [Internet]. Geneva: World Health Organization, 2016 [cited 2020 mar 11]. Available from: https://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf [ Links ]
16. Lohman TG, Roche AF, Martorell R, editors. Anthropometric standardization reference manual. Champaign: Human Kinetics Publications; 1988. [ Links ]
17. World Health Organization. Obesity: preventing and managing the global epidemic [Internet]. Geneva: World Health Organization, 2000 [cited 2020 mar 11]. Available from: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ [ Links ]
18. National Institutes of Health; National Heart, Lung, and Blood Institute. Atherosclerosis risk in communities study. Sitting blood pressure and postural changes in blood pressure and heart rate. Chapel Hill: Aric Coordination Center, 1997 [Internet]. (Aric Study Protocols and Manuals of Operation, 11) [cited 2020 mar 13]. Available from: https://sites.cscc.unc.edu/aric/Cohort_Manuals/Sitting_Blood_Pressure_and_Postural_Changes_in_Blood_Pressure_and_Heart_Rate_11.PDF [ Links ]
19. Sociedade Brasileira de Diabetes. Diretrizes da Sociedade Brasileira de Diabetes 2017-2018 [Internet]. São Paulo: Editora Clannad, 2017 [citado 2020 mar 11]. Disponível em: https://www.diabetes.org.br/profissionais/images/2017/diretrizes/diretrizes-sbd-2017-2018.pdf [ Links ]
20. Sociedade Brasileira de Cardiologia. VII diretriz brasileira de hipertensão arterial. brasil, grandes regiões e unidades da federação. Arq. Bras. Cardiol. [Internet]. 2016 [citado 2020 mar 11];107(3 Supl 3):1-83. Disponível em: http://publicacoes.cardiol.br/2014/diretrizes/2016/05_HIPERTENSAO_ARTERIAL.pdf [ Links ]
21. Carvalho MHC (ed). I Diretriz brasileira de diagnóstico e tratamento da síndrome metabólica. Arq Bras Cardiol [Internet]. 2005 [citado 2020 mar 11];84(Supl 1):3-28. doi: 10.1590/S0066-782X2005000700001 [ Links ]
22. Christensen MA, Bettencourt L, Kaye L, Moturu ST, Nguyen KT, Olgin JE, et al. Direct measurements of smartphone screen-time: relationships with demographics and sleep. PLoS One [Internet]. 2016 [cited 2020 oct 14];11(11):e0165331. doi: 10.1371/journal.pone.0165331 [ Links ]
23. Martins HX, Camargo HXAA, Siqueira JH, Enriquez-Martínez OG, Aprelini CMO, Pereira TSS, et al. Actividad física, comportamiento sedentario y factores asociados en adultos brasileños. Av Enferm. [Internet]. 2020 [citado 2021 oct 25];38(3):347-57. doi: 10.15446/av.enferm.v38n3.85874 [ Links ]
24. Van den Akker M, Buntinx F, Metsemakers JFM, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol [Internet]. 1998 [cited 2020 oct 17];51:367-75. doi: 10.1016/s0895-4356(97)00306-5 [ Links ]
25. Borgo MV, Pimentel EB, Baldo MP, Souza JB, Malta DC, Mill JG. Prevalência de fatores de risco cardiovascular na população de Vitória segundo dados do VIGITEL e da Pesquisa Nacional de Saúde de 2013. Rev Bras Epidemiol [Internet]. 2019 [citado 2020 set 13];22:e190015. doi: 10.1590/1980-549720190015 [ Links ]
26. World Health Organization. A comprehensive global monitoring framework including indicators and a set of voluntary global targets for the prevention and control of noncommunicable [Internet]. Geneva: World Health Organization, 2012:1-23 [cited 2020 mar 11]. Available from: https://www.who.int/nmh/events/2012/discussion_paper2_20120322.pdf [ Links ]
27. Abbott RD, Garrison RJ, Wilson PW, Epstein FH, Castelli WP, Feinleib M, et al. Joint distribution of lipoprotein cholesterol classes. The Framingham study. Arteriosclerosis. 1983;3(3):260-72. doi: 10.1161/01.atv.3.3.260 [ Links ]
28. Knopp RH, Paramsothy P, Retzlaff BM, Fish B, Walden C, Dowdy A, et al. Sex differences in lipoprotein metabolism and dietary response: basis in hormonal differences and implications for cardiovascular disease. Curr Cardiol Rep [Internet]. 2006 [cited 2020 sept 20];8(6):452-9. doi: 10.1007/s11886-006-0104-0 [ Links ]
29. García-Rodríguez A, Gutiérrez-Bedmar M, Bellón-Saameño JÁ, Munoz-Bravo C, Navajas JFC. Psychosocial stress environment and health workers in public health: Differences between primary and hospital care. Aten Primaria [Internet]. 2015 [cited 2020 sept 03];47(6):359-66. doi: 10.1016/j.aprim.2014.09.003 [ Links ]
30. Buss PM, Pellegrini Filho A. A saúde e seus determinantes sociais. Physis: Rev. Saúde Coletiva [Internet]. 2007 [citado 2020 out 19];17(1):77-93. doi: 10.1590/S0103-73312007000100006 [ Links ]
Associated academic work Article derived from the academic master’s degree dissertation entitled ‘Health conditions of community health workers in the municipality of Vitória, ES’, defended by Haysla Xavier Martins at the Programa de Pós-Graduação em Saúde Coletiva, Universidade Federal do Espírito Santo, in 2021.
Financial Maria del Carmen Bisi Molina received a Research Productivity grant from the National Council for Scientific and Technological Development/Ministry of Science, Technology and Innovation (CNPQ/MCTI), File No. 309095/2017-4; Haysla Xavier Martins received a study grant from the Coordination for the Improvement of Higher Education Personnel/Ministry of Education (CAPES/MEC).
Received: June 29, 2021; Accepted: November 12, 2021











 texto em
texto em 
 Curriculum ScienTI
Curriculum ScienTI

