Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.31 no.1 Brasília 2022 Epub 04-Abr-2022
http://dx.doi.org/10.1590/s1679-49742022000100009
Original Article
Profile of hospital admissions and deaths due to severe acute respiratory syndrome caused by COVID-19 in Piauí, Brazil: a descriptive study, 2020-2021
1 Universidade Federal do Piauí, Centro de Ciências da Saúde, Teresina, PI, Brazil
2 Universidade Estadual do Maranhão, São Luís, MA, Brazil
3 Universidade Nova de Lisboa, Instituto de Higiene e Medicina Tropical, Lisboa, Portugal
4 Universidade Federal do Piauí, Núcleo de Estudos em Saúde Pública, Teresina, PI, Brazil
5 Universidade Federal do Piauí, Curso de Engenharia Elétrica, Teresina, PI, Brazil
6 Fundação Instituto Oswaldo Cruz, Escritório Regional do Piauí, Teresina, PI, Brazil
7 Universidade Federal do Piauí, Centro de Inteligência de Agravos Tropicais Emergentes e Negligenciados, Teresina, PI, Brazil
Objective
To describe the profile and temporal variation of hospital admissions and deaths due to severe acute respiratory syndrome (SARS) caused by COVID-19 in Piauí, Brazil, according to place of hospitalization.
Methods
We performed a descriptive study using data from the Influenza Surveillance Information System between 2020 and 2021. Case fatality ratio among hospital records with outcome and respective 95% confidence intervals (95%CI) were calculated.
Results
We included 12,649 individuals who were mostly male (57.1%), Black (61.2%) and had one or two comorbidities (30.5%). Case fatality ratio among hospital records with outcome was higher in the state’s interior region than in its capital, with proportion of 44.1% (95%CI 42.0;46.3) for those who were hospitalized, 82.3% (95%CI 79.7;84.8) for those admitted to intensive care units and 96.6% (95%CI 94.9;97.8) for those undergoing invasive mechanical ventilation.
Conclusion
The study enabled characterization of the profile of SARS hospitalizations due to COVID-19 in Piauí and demonstrated high case fatality ratio, among hospital records with outcome, which remained high during the study period, especially in the interior of the state.
Keywords: COVID-19; Hospitalization; Respiration, Artificial; Critical Care Outcomes; Epidemiology, Descriptive
Study contributions
Main results
In Piauí, among hospital records with outcome, case fatality ratio was higth, especially in the interior of the state, pointing to regional differences in health care as factors that influence hospital outcomes.
Introduction
In-hospital deaths arising from hospitalizations of individuals with COVID-19 has varied depending on the place of hospitalization. For example, while the proportion of in-hospital deaths was 15% in the United States1 and 26% in the United Kingdom,2 the average proportion in Brazil was 38%, regardless of age group.3 Less developed Brazilian regions where social inequality is greater have even higher in-hospital proportion deaths, such as the Northeast region, 48%, and the Northern region, 50%.3
COVID-19 in-hospital mortality from may vary with age, race/skin color, difficulty in accessing immediate care and treatment resources, and other factors such as severity of the clinical picture and need for ventilatory support.1-3 In Brazil, in-hospital COVID-19 deaths have reached levels above 60% in individuals aged 80 years or older, reaching 80% in those undergoing invasive mechanical ventilation.3
The state of Piauí, located in Northeast Brazil, has health indicators of concern related to poverty and less access to health services, such as high maternal mortality rate,4 and is one of the Brazilian states with high risk of social inequalities impacting the COVID-19 pandemic. In Piauí, precarious sanitary conditions, low availability of hospital beds, lack of teams trained in intensive care, and lower availability of tests for diagnosing COVID-19 are considered risk factors for in-hospital COVID-19 deaths.5-7 The growth in the number of cases in the municipalities in the interior of the state has increased concern about the available capacity of health services and their ability to meet the demands of severe cases that require hospitalization. In the absence of these services in the interior, the search for high complexity care in the capital, Teresina, tends to increase even more.
With the increased demand for public health services due to COVID-19 and the absence of coordinated actions between the three levels of Brazilian government, the state governments strategically prepared their own plans of action to address the pandemic.
The objective of this study was to describe the profile and temporal variation of hospital admissions and deaths due to severe acute respiratory syndrome (SARS) caused by COVID-19 in Piauí, Brazil, according to place of hospitalization.
Methods
Design
This was a descriptive ecological study based on hospitalization records of individuals with COVID-19 held on the Influenza Epidemiological Surveillance Information System (SIVEP-Gripe), between epidemiological week (EW) 12/2020 (beginning March 15, 2020) and EW 12/2021 (ending March 27, 2021), in the state of Piauí, Brazil.
Background
Piauí had an estimated population of 3,289,820 inhabitants in 2021, distributed over 224 municipalities, divided into 11 health regions: Carnaubais; Cocais; Chapada das Mangabeiras; Entre Rios; Planície Litorânea; Serra da Capivara; Tabuleiros do Alto Parnaíba; Vale do Canindé; Vale dos Rios Piauí e Itaueiras; Vale do Rio Guaribas; and Vale do Sambito. The state capital, Teresina, had 868,075 (26.5%) inhabitants and is in the Entre Rios health region. Even after the increased supply of hospital beds in the interior of the state during the pandemic, in March 2021, 71% (302/428) of intensive care unit (ICU) beds were concentrated in the state capital. Three health regions in Piauí have no ICU beds: Tabuleiros do Alto Parnaíba, Vale do Sambito and Carnaubais.8
SIVEP-Gripe is Brazil’s information system for epidemiological surveillance of influenza, on which SARS cases requiring hospitalization are recorded. Data from hospitalized individuals are anonymized and aggregated based on the SARS notification forms, and these public access databases are made available on a platform provided by the Brazilian National Health System Information Technology Department (DATASUS).
Study participants
This study included all records of individuals hospitalized with diagnosis of severe acute respiratory syndrome (SARS) in the state of Piauí between EW 12/2020 and EW 12/2021. Those who did not have diagnosis of COVID-19 recorded as the cause of SARS were excluded. In this way we ensured that only individuals hospitalized with COVID-19 were included in the analyses.
The steps involving period selection, criteria for including and excluding participants and other analyses were performed using R software version 4.0.2, after downloading the databases from the DATASUS platform.
Variables
We analyzed the following variables retrieved from the SIVEP-Gripe database relating to COVID-19 cases hospitalized in the period covered by the study:
sex (male; female);
age group (in years: 0-59; 60 or over);
race/skin color [White; Black (Black and Brown); Yellow; Indigenous; Unknown];
schooling (no schooling; complete elementary education; complete high school education; higher education);
comorbidities (0; 1-2; 3 or more);
place of hospitalization (capital; interior);
place of hospitalization in ICU (capital; interior);
date of hospitalization (day, month and year);
hospitalized in ICU (yes; no);
ventilatory support (no; non-invasive; invasive); and
hospital outcome (cure; death).
Data source and measurement
The hospital data we analyzed, taken from the SIVEP-Gripe system and made available on the DATASUS platform, relate to 20209 and 2021,10 this being the study period corresponding to the first year of the pandemic in Piauí. Information about the number of ICU beds was obtained from the Piauí State Health Department website.8
COVID-19 case fatality ratio among hospital records with outcome was calculated by dividing the total number of subjects who died by the total number of records of subjects containing the hospital outcome (hospital discharge or death) at the time of data collection. ICU case fatality ratio among records with outcome was calculated by dividing the total number of ICU inpatients who died by the total number of ICU inpatients with a verified outcome. Case fatality ratio among records of individuals submitted to invasive mechanical ventilation was calculated by taking the number of individuals submitted to invasive mechanical ventilation who died, divided by the total number of inpatients with outcome submitted to invasive mechanical ventilation whose hospital outcome had been recorded.
Bias control
Due to information being missing for some variables on the SIVEP-Gripe database, these data were classified as ‘unknown’ and were excluded from the case fatality ratio calculation. Completeness of the variables used in the study was 84.5%; however, some variables, such as ‘schooling’ and ‘comorbidity’, had high ‘unknown’ percentages, equivalent to 59.1% and 63.3% respectively.
Statistical methods
We performed the analysis using R software, version 4.0.2. We undertook descriptive analysis of the data, calculating means and standard deviations (SD) for quantitative variables; and relative frequencies for categorical variables. ‘Unknown’ and blank variables were excluded from the descriptive analysis. COVID-19 case fatality ratio among records with outcome and its respective 95% confidence intervals (95%CI) were calculated using the Agresti & Coull method.11 When making the comparison between the state capital and the interior region of the state, we considered different the 95%CI that did not overlap. Regarding the temporal variation analysis, COVID-19 case fatality ratio among records with outcome was calculated for four-week periods and according to place of hospitalization, i.e. interior or capital of the state.
Results
Between epidemiological weeks 12/2020 and 12/2021, 18,014 cases of individuals hospitalized due to SARS were recorded in the state of Piauí, according to the SIGEP-Gripe system. Of these, 5,365 (29.8%) were excluded for not having confirmed diagnosis of COVID-19 (3,906 without etiologic diagnosis, 1,218 awaiting results or without etiologic diagnosis, 216 affected by other respiratory viruses, and 25 affected by other causes). Of the 12,649 hospitalized individuals who had COVID-19, 5,866 (46.4%) were discharged, 3,277 (25.9%) died, and 3,506 (27.7%) had no information on hospital outcome at the time of data collection (Figure 1).
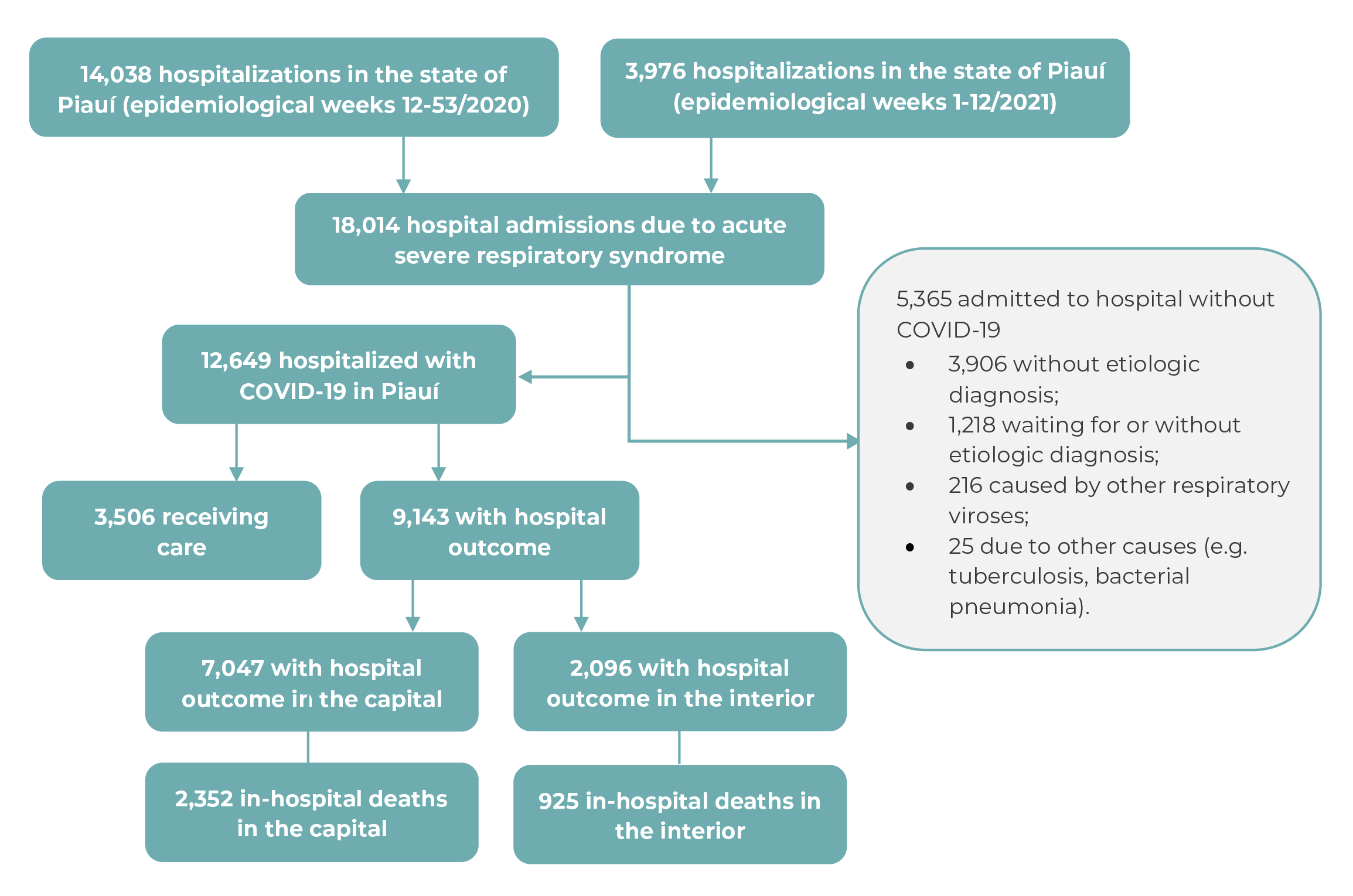
Figure 1 Process for selection of hospitalized individuals diagnosed as having COVID-19 in Piauí, Brazil, March/2020 to March/2021
The mean age of the hospitalized individuals was 60±19 years. A total of 5,761 (45.5%) individuals were up to 59 years old, and 6,888 (54.5%) were aged 60 or over. The majority were male (57.1%), of Black race/skin color (61.2%), and had one or two comorbidities (30.5%). Most of the individuals were hospitalized in the state capital, accounting for 79.5% of total admissions, and 76.6% of them occupied ICU beds (Table 1).
Table 1 Individuals hospitalized with COVID-19 (n=12,649) according to sociodemographic, health condition and hospitalization characteristics, and place of hospitalization, in Piauí, Brazil, March/2020 to March/2021
| Variables | n (%) |
|---|---|
| Sex | |
| Male | 7,222 (57.1) |
| Female | 5,427 (42.9) |
| Age group (years) | |
| 0-59 | 5,761 (45.5) |
| ≥60 | 6,888 (54.5) |
| Race/skin color | |
| White | 1,541 (12.2) |
| Black (Black and Brown) | 7,740 (61.2) |
| Yellow | 269 (2.1) |
| Indigenous | 17 (0.1) |
| Unknown | 3,082 (24.4) |
| Schooling | |
| No schooling | 681 (5.4) |
| Complete elementary education | 1,828 (14.4) |
| Complete high school education | 1,640 (13.0) |
| Higher education | 1,029 (8.1) |
| Unknown | 7,471 (59.1) |
| Comorbidities | |
| 0 | 459 (3.6) |
| 1-2 | 3,856 (30.5) |
| ≥3 | 333 (2.6) |
| Unknown | 8,001 (63.3) |
| Place of hospitalization | |
| Capital | 10,054 (79.5) |
| Interior | 2,595 (20.5) |
| Place of hospitalization = intensive care unit | |
| Capital | 3,097 (76.6) |
| Interior | 938 (23.4) |
| Total | 12,649 (100.0) |
Among the 9,143 individuals for whom hospital outcome (discharge or death) was recorded, case fatality ratio increased as the percentage of cases requiring intensive care and invasive procedures increased, approaching 100%, especially in the interior of the state (Table 2). Among the 2,096 individuals hospitalized with COVID-19 in the interior of the state and who had information on hospital outcome, 925 died, resulting in an case fatality ratio of 44.1% (95%CI 42.0;46.3). Among the 872 hospitalized in ICUs in the interior of the state who had information on hospital outcome, 718 died, corresponding to an case fatality ratio of 82.3% (95%CI 79.7;84.8), while among those undergoing invasive mechanical ventilation (n=679), 656 died, resulting in an case fatality ratio of 96.6% (95%CI 94.9;97.8) (Table 2).
Table 2 Case fatality ratio and 95% confidence intervals among individuals with COVID-19 and hospital outcome (n=9,143), according to sociodemographic, health condition and hospitalization characteristics, in the capital and interior region of Piauí, Brazil, March/2020 to March/2021
| Variables | Total | Capital | Interior | |||
|---|---|---|---|---|---|---|
| n | % (95%CIa) | n | % (95%CIa) | n | % (95%CIa) | |
| Sex | ||||||
| Female | 3,958 | 34.2 (32.7;35.7) | 3,006 | 31.6 (30.0;33.3) | 952 | 42.2 (39.1;45.4) |
| Male | 5,185 | 37.1 (35.8;38.5) | 4,041 | 34.7 (33.2;36.2) | 1,144 | 45.7 (42.9;48.6) |
| Race/skin color | ||||||
| Yellow | 182 | 26.9 (21.0;33.8) | 174 | 25.9 (19.9;32.9) | 8 | 50.0 (21.5;78.5) |
| Black | 5,748 | 38.6 (37.3;39.9) | 4,315 | 33.8 (32.4;35.2) | 1,433 | 53.1 (50.5;55.7) |
| White | 1,023 | 40.4 (37.4;43.4) | 909 | 36.6 (33.6;39.8) | 114 | 70.2 (61.2;77.8) |
| Schooling | ||||||
| No schooling | 583 | 48.9 (44.8;52.9) | 474 | 41.6 (37.2;46.0) | 109 | 80.7 (72.3;87.1) |
| Complete elementary education | 1,404 | 41.2 (38.6;43.8) | 1,192 | 34.6 (32.0;37.4) | 212 | 77.8 (71.7;82.9) |
| Complete high school education | 1,003 | 22.3 (19.9;25.0) | 923 | 20.5 (18.0;23.2) | 80 | 43.8 (33.4;54.7) |
| Higher education | 494 | 19.8 (16.6;23.6) | 463 | 18.4 (15.1;22.1) | 31 | 41.9 (26.4;59.3) |
| Comorbidities | ||||||
| 0 | 350 | 35.1 (30.3;40.3) | 308 | 30.5 (25.6;35.9) | 42 | 69.0 (53.9;81.0) |
| 1-2 | 2,945 | 43.6 (41.9;45.4) | 2,485 | 40.0 (38.1;41.9) | 460 | 63.5 (59.0;67.8) |
| ≥3 | 285 | 60.4 (54.6;65.9) | 241 | 55.2 (48.8;61.3) | 44 | 88.6 (75.6;95.5) |
| Intensive care unit | ||||||
| No | 5,080 | 14.7 (13.8;15.7) | 4,195 | 14.5 (13.4;15.6) | 885 | 16.0 (13.8;18.6) |
| Yes | 3,366 | 70.9 (69.3;72.4) | 2,494 | 66.8 (65.0;68.7) | 872 | 82.3 (79.7;84.8) |
| Respiratory support | ||||||
| No | 2,066 | 9.1 (7.9;10.4) | 1,859 | 9.5 (8.3;10.9) | 207 | 5.3 (2.9;9.4) |
| Non-invasive | 4,264 | 23.0 (21.7;24.3) | 3,273 | 23.6 (22.2;25.1) | 991 | 20.9 (18.5;23.5) |
| Invasive | 2,222 | 87.8 (86.4;89.1) | 1,543 | 84.0 (82.1;85.7) | 679 | 96.6 (94.9;97.8) |
| Total | 9,143 | 35.8 (34.9;36.8) | 7,047 | 33.4 (32.3;34.5) | 2,096 | 44.1 (42.0;46.3) |
a) 95%CI: 95% confidence interval.
In the state capital, the COVID-19 case fatality ratio among all hospitalized individuals whit outcome was 33.4% (95%CI 32.3;34.5), while it was 66.8% (95%CI 65.0;68.7) among those in ICUs and 84.0% (95%CI 82.1;85.7) among those undergoing invasive mechanical ventilation (Table 2).
Hospitalized individuals who were male, of Black race/skin color and had comorbidities had higher COVID-19 case fatality ratios (Table 2). A decrease in case fatality ratio was found as level of schooling increased, especially among hospitalized individuals living in the interior of the state, for whom COVID-19 case fatality ratio was 80.7% (95%CI 72.3; 87.1) among those with no schooling, 77.8% (95%CI 71.7;82.9) among those with complete elementary education, 43.8% (95%CI 33.4;54.7) among those with high school education, and 41.9% (95%CI 26.4;59.3) among those with higher education qualifications (Table 2).
COVID-19 case fatality ratio among records with outcome was higher in the elderly, especially among those hospitalized in the interior of the state. Among individuals aged 60 years or older, case fatality ratio was 45.0% (95%CI 43.4;46.5) in the state capital and 55.4% (95%CI 52.8;58.1) in the interior. Among individuals of the same age group who required and received intensive care, case fatality ratio was 73.9% (95%CI 71.8;76.0) in the state capital and 86.5% (95%CI 83.6%;88.9) in the interior. With regard to those who underwent invasive ventilation, case fatality ratio in individuals aged 60 years or older was 88.9% (95%CI 86.9;90.7) in the state capital and 98.3% (95%CI 96.7;99.1) in the interior (Figure 2).
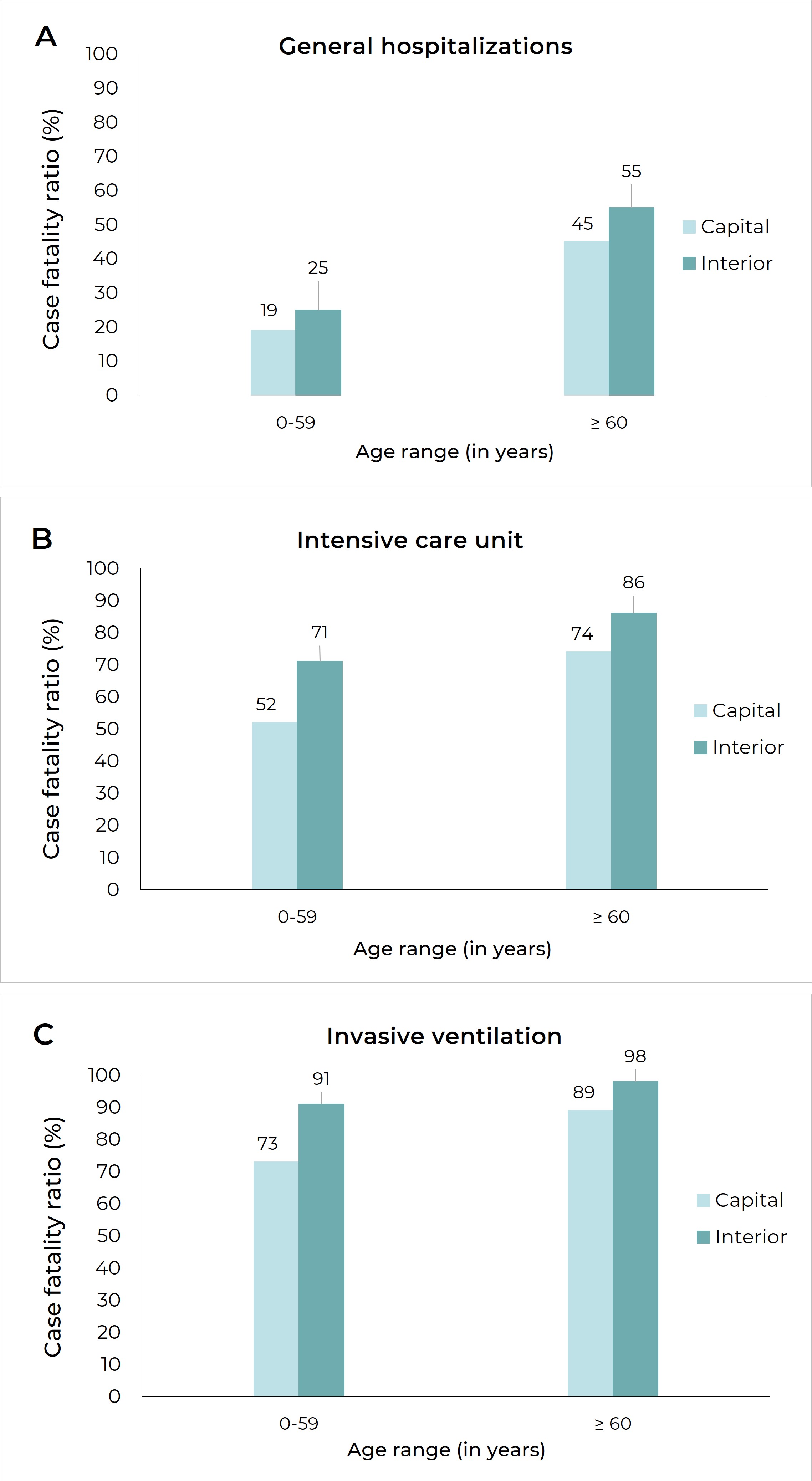
A) General case fatality ratio in the interior and the capital, by age group (in years); B) Intensive care unit (ICU) case fatality ratio, by place of hospitalization and age group (in years); C) Case fatality ratio among individuals who received invasive ventilation, by place of hospitalization and age group (in years).
Figure 2 Case fatality ratio among individuals with COVID-19 and hospital outcome (n=9,143), by age group (years) and hospitalization condition, in the capital and interior of Piauí, Brazil, March/2020 to March/2021
During the study period, differences were observed in the pattern of hospital admissions between the interior and capital of Piauí. In the capital, the peak in hospitalizations occurred between epidemiological weeks 24 and 27/2020, when 1,434 hospitalized individuals were recorded, whereas in the interior, the highest number of hospitalizations corresponded to epidemiological weeks 9 to 12/2021, when 351 hospitalizations were recorded (Figure 3A). In the capital, the peak in ICU admissions and in use of invasive respiratory support occurred between epidemiological weeks 24 and 27/2020, when 428 and 304 cases were recorded, respectively. In the interior of the state, the highest number of ICU hospitalizations and respiratory support use occurred between epidemiological weeks 9 and 12/2021, when 145 and 129 cases were recorded, respectively (Figures 3B and 3C).
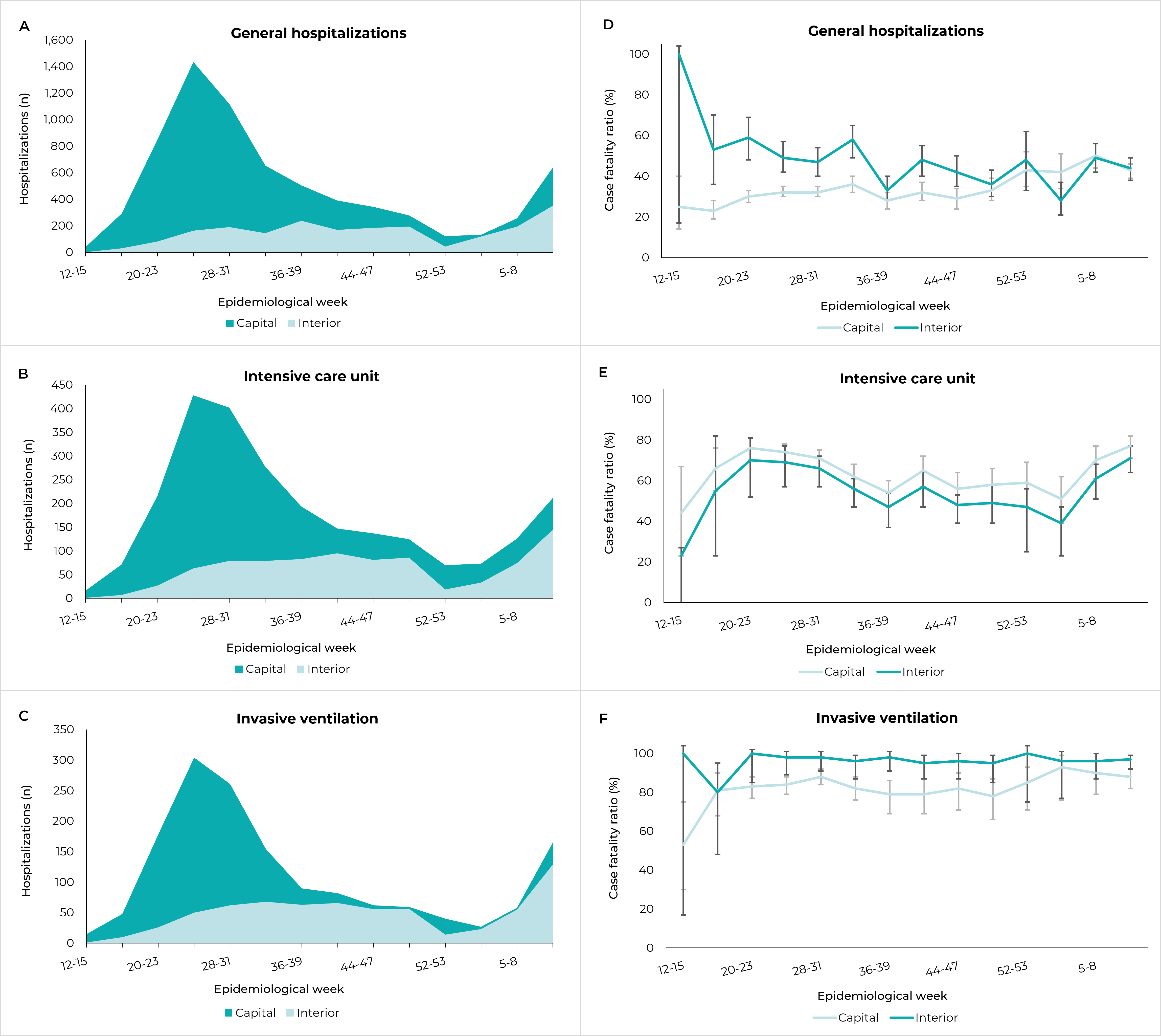
A) Temporal variation of the number of COVID-19 hospitalization in the capital and interior of the state; B) Temporal variation of the number of individuals with COVID-19 submitted to intensive care; C) Temporal variation of the number of individuals with COVID-19 who received invasive ventilation; D) Temporal variation of case fatality ratio in hospitalized individuals; E) Temporal variation of case fatality ratio in individuals admitted to an intensive care unit; F) Temporal variation of case fatality ratio in individuals submitted to invasive ventilation.
Figure 3 Temporal variation of number of hospitalizations and case fatality ratio among individuals with COVID-19 and hospital outcome (n=9,143), in the capital and interior of Piauí, Brazil, March/2020 to March/2021
During the years analyzed, regardless of the variation in the number of hospital admissions, COVID-19 case fatality ratio among records with outcome in the interior of the state remained higher than in the capital Teresina for most of this period, especially in ICUs and among those undergoing invasive ventilation. The case fatality ratio, the coefficient ranged from 25.0% (95%CI 14.0;40.4) to 49.6% (95%CI 43.5;55.7) in the state capital, while in the interior it reached 59.3% (95%CI 48.4;69.3) between epidemiological weeks 20 and 23/2020 (Figure 3D). In the case of individuals admitted to ICUs, case fatality ratio ranged from 43.7% (95%CI 23.1;66.8) to 76.9% (95%CI 70.1;82.1) in the state capital, while in the interior it remained above 70.0% with effect from epidemiological week 19/2020 (Figure 3E). And for those undergoing invasive mechanical ventilation in the state capital, case fatality ratio remained above 78.0% (95%CI 65.7;86.8) for most of the period, while in the interior of the state, it remained close to 100.0% throughout the period analyzed (Figure 3F).
Discussion
Our analysis of SARS hospitalizations due to COVID-19 in Piauí found high case fatality ratio among records with outcome, especially in the interior of the state and among individuals undergoing invasive mechanical ventilation. The study enabled characterization of the profile of hospitalized individuals in the state, finding a higher percentage of elderly people, males, those of Black race/skin color and those who had one or two comorbidities. Furthermore, our analysis identified temporal variation in the number of hospital admissions, in the capital and in the interior, revealing synchronization of the curves in the last epidemiological weeks analyzed. The case fatality ratio curves of individuals admitted to ICUs and submitted to mechanical ventilation with hospital outcome were higher in the interior of the state throughout the period studied.
It is important to emphasize that the study was based on secondary data and has limitations inherent to it, such as outdated information, lower reliability and problems related to record accuracy. The data source used was the SIVEP-Gripe, which is mandatory system for recording cases. It is the main repository of hospital data at national level, although it may be influenced by the flow of data between levels of government, in addition to weaknesses regarding data completeness. In the state of Piauí, the ‘schooling’ and ‘comorbidities’ variables had the lowest percentages of completeness, which may have influenced the analysis of the profile of cases found and analyzed.
Another limitation of this study is related to the scarcity of molecular tests in Brazil, which are primarily used for individuals with more severe conditions. Our analysis, which was restricted to those with hospital outcome and diagnosis confirmed by molecular testing and therefore with potentially more severe conditions, may have overestimated case fatality ratio. To reduce this bias, we included in the study all individuals diagnosed with COVID-19 registered on the SIVEP-Gripe system.
In Piauí, more than one-third of hospitalized individuals with outcome died, this being a result similar to that found in a retrospective study on hospitalization data recorded on the SIVEP-Gripe system for all of Brazil, which reported a 38% of deaths.3 On the other hand, the COVID-19 case fatality ratio for cases admitted to ICUs in the state of Piauí were higher than those previously reported, both for Brazil as a whole (59%) and for the Northeast region of Brazil (70%).3 This difference in case fatality ratio becomes even more pronounced when making a comparison between hospitalizations of individuals requiring intensive care and ventilatory support in the interior of the state and in the capital.
Among individuals submitted to invasive mechanical ventilation with hospital outcome, the case fatality ratio in the capital Teresina and in the cities of the interior of Piauí were higher than those found for Brazil as a whole (80%) and for the Northeast region (87%).3 Whereas case fatality ratio in regions with limited resources, such as the North and Northeast, is higher than in other regions of Brazil,12 the results found in this study also exceed the findings of studies conducted in various regions of the world. A meta-analysis that included 69 studies involving 57,420 individuals from various countries found a 45% case fatality ratio among individuals severely affected by COVID-19 and submitted to invasive ventilation.13 In Brazil, a cohort of 2,054 individuals admitted to 25 hospitals in 11 cities and three states, found a 59.5% of deaths among individuals who required invasive mechanical ventilation.14 Several factors must be considered in relation to that outcome, including lower access to health care and lower availability of supplies, equipment and health professionals trained to care for individuals with COVID-19 and its complications. In addition, specialized services in the interior of the country, in general, may have fewer physicians, intensivists and professionals specialized in care for COVID-19 cases - this being a fact that has also been associated with higher in-hospital mortality.15
Factors already reported in the literature, such as comorbidities, age, sex and schooling, have also been relevant for increased in-hospital deaths. In this study, despite the large amount of ‘unknown’ information, the most frequent comorbidities - cardiovascular diseases, followed by diabetes mellitus and obesity - corroborate the results of a systematic review involving 53 studies identified by means of a database search and conducted as at September 2020, which included 375,859 participants from 14 countries.16 The presence of comorbidities, especially in the elderly, can increase the need for ICU admission, mechanical ventilation and, consequently, risk of death.13,17,18 Regarding schooling, a clear decrease in in-hospital deaths was observed as the individuals’ level of education increased, regardless of where hospitalization took place, i.e. in the state capital or interior, corroborating similar results already reported, such as sociodemographic indicators associated with high in-hospital mortality in Brazil.19,20
The spread of COVID-19 cases to the interior of the state and the increased demand for care in all available health services in the state may influence mortality, due to the population’s demand for hospital beds, especially in the case of individuals most severely affected and in need of intensive care. As such, synchronization of the increase in the disease in the capital and in interior region cities is one of the factors aggravating and contributing to the collapse of the health system. The expansion and spread of COVID-19 in Piauí, confirmed by the hospitalization frequency curves, showed temporal variations like those in other Brazilian states, whereby the disease is seen to spread from the capital to smaller cities and to cities in the interior region of the state. Up until epidemiological week 53 of the period covered by the study, hospital admissions were higher in the state capital. This was followed by synchronization of COVID-19 hospitalization trend curves between the various points of care.
In general, community transmission of COVID-19, which started in the country’s state capitals, spreads to smaller municipalities due to the dynamics of human mobility; however, the most severe cases return to the capital in search of more specialized care.5 In Piauí, the object of this study, coronavirus cases spread from the capital to the interior, while the flow of care went from the interior to the capital, with most hospitalizations having occurred in Teresina. Average hospitalization due to COVID-19 for the Brazilian state capitals as a whole is 54%.3 Taking each of the Brazilian regions, on average their capital cities have the following COVID-19 hospitalization percentages: Midwest, 71%; Northeast, 70%; North, 61%; Southeast, 50%; and South, 32%.3 As such, centralization of health care in Piauí is higher than in most Brazilian regions and one of the highest in the country.
Also noteworthy is the increase in the number of clinical and ICU beds, throughout the period analyzed and in all the COVID-19 care regions in Piauí. Despite the increase in hospital care capacity, case fatality ratio remained high, revealing that the increased number of facilities, by itself, was not enough to reduce the high number of deaths.
The results of this study provide evidence of the high levels of case fatality ratio found in the interior of the state of Piauí, especially in individuals undergoing invasive mechanical ventilation. We hope that this evidence will contribute to the implementation of strategies aimed at reducing hospital deaths among COVID-19 cases and cases of other diseases, such as allocation of resources in a regionalized and equitable way, respecting health territories and enabling the strengthening of the entire health care network.21 In Brazil, health regions with a scarcity of high technology resources have had the highest average mortality rates.22
Our analysis of hospital admissions in Piauí enabled the profile of COVID-19 hospitalizations in the state to be described, as well as identifying high case fatality ratio among individuals treated in the interior of the state, especially those who underwent invasive mechanical ventilation. This evaluation points to weaknesses in health system organization in Piuaí, especially the most specialized services, and provides information for re-evaluating strategies for addressing the pandemic and potential public health emergencies.
Referências
1. Asch DA, Sheils NE, Islam MN, Chen Y, Werner RM, Buresh J, et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med. 2021;181(4):471-8. Doi: 10.1001/jamainternmed.2020.8193 [ Links ]
2. Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. Doi: 10.1136/bmj.m1985 [ Links ]
3. Ranzani OT, Bastos LSL, Gelli JGM, Marchesi JF, Baião F, Hamacher S, et al. Characterisation of the first 250 000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9(4):407-18. Doi: 10.1016/S2213-2600(20)30560-9 [ Links ]
4. Szwarcwald CL, Escalante JJC, Rabello Neto DL, Souza Junior PRB, Victora CG. Estimation of maternal mortality rates in Brazil, 2008-2010. Cad Saude Publica. 2014;30(Suppl 1):S1-12. doi: 10.1590/0102-311x00125313 [ Links ]
5. Castro MC, Kim S, Barberia L, Ribeiro AF, Gurzenda S, Ribeiro KB, et al. Spatiotemporal pattern of COVID-19 spread in Brazil. Science. 2021;372(6544):821-6. doi: 10.1126/science.abh1558 [ Links ]
6. Orellana JDY, Cunha GM, Marrero L, Horta BL, Leite IC. Explosão da mortalidade no epicentro amazônico da epidemia de COVID-19. Cad Saude Publica. 2020;36(7):e00120020. doi: 10.1590/0102-311x00120020 [ Links ]
7. Malta M, Strathdee SA, Garcia PJ. The brazilian tragedy: where patients living at the 'Earth's lungs' die of asphyxia, and the fallacy of herd immunity is killing people. EClinicalMedicine. 2021;32:100757. doi: 10.1016/j.eclinm.2021.100757 [ Links ]
8. Secretaria Estadual de Saúde (Piauí). Painel epidemiológico COVID-19 [Internet]. Piauí: Secretaria Estadual de Saúde; 2021 [citado 2021 Set 17]. Disponível em: https://datastudio.google.com/u/0/reporting/a6dc07e9-4161-4b5a-9f2a-6f9be486e8f9/page/2itOB [ Links ]
9. Ministério da Saúde (BR). Notificações de síndrome gripal [Internet]. Brasília: Ministério da Saúde; 2020 [citado 2021 Set 17]. Disponível em: https://opendatasus.saude.gov.br/dataset/bd-srag-2020 [ Links ]
10. Ministério da Saúde (BR). Notificações de síndrome gripal [Internet]. Brasília: Ministério da Saúde; 2021 [citado 2021 Set 17]. Disponível em: https://opendatasus.saude.gov.br/dataset/bd-srag-2021 [ Links ]
11. Agresti Alan, Coull Brent A. Approximate Is Better than "Exact" for Interval Estimation of Binomial Proportions. The American Statistician 1998;52(2). doi: 10.2307/2685469 [ Links ]
12. Madahar P, Wunsch H, Jha P, Slutsky AS, Brodie D. Trends in COVID-19-related in-hospital mortality: lessons learned from nationwide samples. Lancet Respir Med. 2021;9(4):322-4. doi: 10.1016/S2213-2600(21)00080-1 [ Links ]
13. Lim ZJ, Subramaniam A, Ponnapa Reddy M, Blecher G, Kadam U, Afroz A, et al. Case fatality rates for patients with COVID-19 requiring invasive mechanical ventilation: a meta-analysis. Am J Respir Crit Care Med. 2021;203(1):54-66. doi: 10.1164/rccm.202006-2405OC [ Links ]
14. Marcolino MS, Ziegelmann PK, Souza-Silva MVR, Nascimento IJB, Oliveira LM, Monteiro LS, et al. Clinical characteristics and outcomes of patients hospitalized with COVID-19 in Brazil: results from the Brazilian COVID-19 registry. Int J Infect Dis. 2021;107:300-10. doi: 10.1016/j.ijid.2021.01.019 [ Links ]
15. Portella TP, Mortara SR, Lopes R, Sánchez-Tapia A, Donalísio MR, Castro MC, et al. Temporal and geographical variation of COVID-19 in-hospital fatality rate in Brazil. medRxiv. 2021;2021.02.19.21251949. doi: 10.1101/2021.02.19.21251949 [ Links ]
16. Ng WH, Tipih T, Makoah NA, Vermeulen JG, Goedhals D, Sempa JB, et al. Comorbidities in SARS-CoV-2 patients: a systematic review and meta-analysis. mBio. 2021;12(1):e03647-20. doi: 10.1128/mBio.03647-20 [ Links ]
17. Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit. JAMA Netw Open. 2020;3(6):e2012270. doi: 10.1001/jamanetworkopen.2020.12270 [ Links ]
18. Nachtigall I, Lenga P, Józwiak K, Thürmann P, Meier-Hellmann A, Kuhlen R, et al. Clinical course and factors associated with outcomes among 1904 patients hospitalized with COVID-19 in Germany: an observational study. Clin Microbiol Infect. 2020;26(12):1663-9. doi: 10.1016/j.cmi.2020.08.011 [ Links ]
19. Peres IT, Bastos LSL, Gelli JGM, Marchesi JF, Dantas LF, Antunes BBP, et al. Sociodemographic factors associated with COVID-19 in-hospital mortality in Brazil. Public Health. 2021;192:15-20. doi: 10.1016/j.puhe.2021.01.005 [ Links ]
20. Passos VMA, Brant LCC, Pinheiro PC, Correa PRL, Machado IE, Santos MR, et al. Maior mortalidade durante a pandemia de COVID-19 em áreas socialmente vulneráveis em Belo Horizonte: implicações para a priorização da vacinação. Rev Bras Epidemiol. 2021;24:e210025. doi: 10.1590/1980-549720210025 [ Links ]
21. Palamim CVC, Marson FAL. COVID-19 - the availability of ICU beds in Brazil during the onset of pandemic. Ann Glob Health. 2020;86(1):100. doi: 10.5334/aogh.3025 [ Links ]
22. Moreira RS. COVID-19: unidades de terapia intensiva, ventiladores mecânicos e perfis latentes de mortalidade associados à letalidade no Brasil. Cad Saude Publica. 2020;36(5):e00080020. doi: 10.1590/0102-311x00080020 [ Links ]
Received: September 22, 2021; Accepted: November 29, 2021











 texto en
texto en 


