Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Epidemiologia e Serviços de Saúde
versão impressa ISSN 1679-4974versão On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.31 no.1 Brasília 2022 Epub 01-Abr-2022
http://dx.doi.org/10.1590/s1679-49742022000100012
ORIGINAL ARTICLE
Costs of hospital admission authorizations due to falls among older people in the Brazilian National Health System, Brazil, 2000-2020: a descriptive study
1Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil
2Instituto Federal de Educação, Ciência e Tecnologia do Rio Grande do Sul, Porto Alegre, RS, Brazil
3Universidade Federal do Rio Grande do Sul, Programa de Pós-Graduação em Enfermagem, Porto Alegre, RS, Brazil
Objective:
To describe the costs of hospital admission authorizations (AIHs) due to falls among older people within the Brazilian National Health System (SUS).
Methods:
This was a descriptive cost analysis study, based on data from the SUS’s Hospital Information System, related to AIH due to falls among older people (60 years and older), between 2000 to 2020. A descriptive analysis was performed and cost measurement was based on a macro-costing method.
Results:
1,746,097 AIHs due to falls among older people were recorded, and the total cost was found to be BRL 2,315,395,702.75. The proportion of hospitalization costs was higher among those aged 80 years and older (36.9%), female (60.4%) and the Southeast region of the country (57.3%). The average length of stay in hospital ranged from 5.2 to 7.5 days.
Conclusion:
The high costs identified showed the need for investments in more effective measures in order to prevent and mitigate the damage caused by falls among older people.
Keywords: Accidents due to Falls; Hospital Costs; Hospitalization; Older people; Descriptive Epidemiology; Costs and Cost Analysis.
Study contributions
Main results
1,746,097 hospital admission authorizations due to falls among older people were recorded. The average length of stay in hospital ranged from 5.2 to 7.5 days. The total cost of hospitalizations was R$ 2,315,395,702.75, and it was higher among those ≥80 years old, female and the Southeast region.
Implications for services
The findings make it possible to measure the financial impact of falls on older people, promoting public policies and priority actions aimed at this population.
Perspectives
Investment in community-based services is the main focus of the implementation of prevention strategies, as well as the quality of the records as a way to elucidate indirect costs and identify other social investment actions.
INTRODUCTION
Aging is a natural process in which there is a general decline in physical capacities of an individual.1 The presence of chronic degenerative diseases, cognitive decline, visual alterations and change in physical mobility, in addition to polypharmacy, make older people more fragile and vulnerable to events such as falls.2 Strategies to prevent these falls could substantially reduce health costs.3
Falls are the most frequent domestic accident among older people. It is estimated that among this population, about 60% to 70% of falls occur inside the homes or their surroundings, and 30% of people aged 65 years and older, and 50% of those aged 80 years and older experience at least one fall within a year. In Brazil, falls accounted for 22.5% of deaths among older people in the period between 1996 and 2005.2,4,5 Older people consider their homes a safe place, given their familiarity and knowledge about the place, and perhaps for this reason, it becomes a hazardous environment due to self-confidence when moving around and performing daily activities, and inadequacies of the environment and furniture, such as the presence of unfixed carpets, physical obstacles and absence of grab bars in bathrooms. In addition to these factors, it is worth mentioning the physiological changes resulting from the aging process.4,6
Falls can cause serious injury, skin lesions, dislocations and fractures, impair physical mobility, worsen prior clinical conditions, progressively reduce the functional capacity, cause dependence and generate psychological consequences, such as anxiety, insecurity, loss of confidence due to fear of falling again, social isolation, loss of autonomy and independence to perform basic activities of daily living.1,2,4
The economic costs of fall-related injuries are substantial. In Australia, the average cost of health care for older people aged 65 and older is $ 1,049 per hospital-treated fall injuries, while in Finland, it is $ 3,611.3 These costs are related to the diagnosis, treatment, recovery from the disease and rehabilitation after it. A study conducted in the United States sought to estimate the average direct costs of fatal and non-fatal injuries in hospitals, emergency rooms and outpatient settings among older people, and identified the occurrence of 24,190 fatal injuries and 3.2 million medically treated non-fatal fall related injuries among older adults from that country, in 2012. The direct medical costs related to this treatment totaled $ 616.5 million for fatal and $ 30.3 billion for non-fatal injuries,7 evidencing the need for multimodal strategies that can promote health practices that enable the mitigation of damages, both in the community and long-term hospitals.
Falls are a global public health problem and an adverse event that affects 4% to 16% of hospitalized individuals in developed countries. In Brazil, falls are the third most commonly reported adverse event to the Agência Nacional de Vigilância Sanitária (Anvisa), representing high risk for hospitalized older adults and prevalence of 28% to 32% outside healthcare institutions.8-10
As such, studies are needed to contribute to a reflection about the impact of falls on older people and also health care economy, in addition to the implementation of measures to prevent this occurrence.
The objective of this study was to describe the costs of hospitalizations due to falls among older people within the Brazilian National Health System (SUS).
METHODS
Study design
This was a descriptive cost analysis study of hospital admission authorizations (AIHs) due to falls among older people, within the SUS. The costs were observed in the period between 2000 and 2020. ‘Methodological Guidelines: Economic Evaluation Guideline’ were adopted in order to conduct the study.11
Data from the Hospital Information System (SIH/SUS) were used, made available by the Brazilian National Health System Information Technology Department (DATASUS), for public consultation. All AIHs funded by the SUS are recorded on the SIH/SUS for reimbursement purposes.12
The measurement of hospitalization costs was performed based on a macro-costing method,12 from data provided by DATASUS. National guidelines were used in order to deal with the methodological uncertainties of the study, such as the choice of the cost-based valuation method.13
Context
The growth of the population aged 60 years and older in Brazil has accelerated in recent decades. According to data from the Instituto Brasileiro de Geografia e Estatística (IBGE),14 in Brazil, the number of older adults increased from 15.5 million, 8.6% of the country’s population, in 2000 to 29.9 million in 2020, representing 14% of Brazilians.
The accelerated growth of older population has increased the concern about falls, the most frequent event among this population, including at home. Falls can cause serious physical injuries and result in hospitalizations, presenting a significant burden to health care systems in order to treat them.6
Each hospitalization generates an AIH, which is an instrument used by all SUS managers and service providers to enable hospitalizations and generation of payment amounts. Data from hospital institutions, identification of individuals, primary and secondary diagnosis, according to the International Statistical Classification of Diseases and Related Health Problems 10th revision (ICD-10), the procedures performed and the amount paid are recorded in the AIH. The payment is made based on predetermined values for medical procedures, which include the materials to be used, procedures performed, health professionals involved and hospital hotel service. Therefore, the costs paid for hospitalizations depend on the proper completion of AIH.15
Participants
Among the hospitalizations recorded by hospital institutions providing care via the SUS,14 we included hospitalizations of older people aged 60 years and older, due to external causes, classified using ICD-10 W00-W19 codes, related to falls.
Variables
The following variables were analyzed:
sex (female; male);
age group (in years: 60 to 69; 70 to 79; 80 and older);
region of the country (North; Northeast; Midwest; Southeast; South);
average length of stay in hospital (in days);
cn-hospital case fatality ratio (ratio of total deaths due to falls and total hospitalization due to falls, multiplied by 100);
total amount paid for hospital admissions [In Brazilian Reais (BRL) million].
The in-hospital case fatality ratio due fall were calculated, considering that fall is a preventable event and its occurrence can cause serious injuries or even lead to death. Moreover, the calculation of rates offers an overall panorama of the severity of accidents due to falls among these individuals profiles, and their costs to the public health system.
Data source and measurement
DATASUS provides information, both from the period between ‘1998 to 2007’ and from’ 2008’ onwards. The path taken on the website in order to obtain data was: Access to information > Health Information (TABNET) > Epidemiological and Morbidity > Hospital Morbidity in the SUS > External causes, by place of hospitalization from 1998 to 2007, or External causes, by place of hospitalization from 2008 onwards > Geographic scope: Brazil by region and federative unit > Content: Hospitalizations, Total Value, Average Length of Stay in Hospital and Mortality Rate > Available Periods: Jan./2000 to Dec./2007; and Jan./2008 to Dec./2020 > Group of Causes: W00-W19 Falls > Age Group 1: 60 to 69 years, 70 to 79 years and 80 years and older.12 The data were retrieved in May 2021.
Data analysis
Statistical analysis was performed using Microsoft Excel 365 and SPSS (Statistical Package for Social Sciences), version 18.0 for Windows.
Frequency tables (simple and cross tabulation) and line charts were elaborated. The total number of hospitalizations, the average length of stay in hospital, the in-hospital case fatality ratio and the total amount spent by the SUS in the periods from 1998-2007 and 2008-2020 were calculated. Cost calculation was performed by dividing the aggregate cost of hospitalizations (in BRL), for the period, by the number of AIHs.16 Descriptive statistics were generated (frequency tables, line charts, calculation of the mean and standard deviation). The mean number of hospitalizations and the average total cost, per region of Brazil, were calculated by dividing the sum of the values obtained from the SIH/SUS by the number of years of the study period (21 years: 2000 to 2020).
In addition, the total cost was presented, adjusted according to the National Consumer Price Index - Extended (IPCA) for the study period.
The time frame of the study enabled us to verify the evolution of occurrence of falls among this specific population, recorded on SIH/SUS; and include the year 2013, when the National Patient Safety Program (PNSP) was established, in order to prevent and reduce the incidence of adverse events related to health care, and encourage health institutions to develop and implement protocols that ensure safer healthcare for health users.17
Ethical aspects
The study project met the determinations described in the National Health Council (CNS), Resolution No. 466 of December 12, 2012.18 The project was not submitted to a Research Ethics Committee, because it used data available in the public domain, which does not allow the identification of the subjects.
RESULTS
1,746,097 AIHs due to falls among older people in Brazil were recorded on the Hospital Information System (SHI/SUS), between 2000 and 2020, which corresponded to a cost of BRL 2,315,395,702.75 for the health care system, as shown in Table 1.
Table 1 - Absolute (N) and relative (%) frequencies, average length of stay in hospital, mortality and cost rates, according to age group and sex, of the hospital admission authorizations due to falls among the older population, Brazil, 2000-2007 and 2008-2020
| Characteristics | Period | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2000-2007 | 2008-2020 | |||||||||||||
| Age group (years) | Sex | N (%) | Average length of stay in a hospital (days) | In-hospital case fatality ratio (%) | Cost (BRL) (%) | Cost-a (BRL)a | N (%) | Average length of stay in a hospital (days) | In-hospital case fatality ratio (%) | Cost (BRL) (%) | Cost-a (BRL)a | N total (%) | Total cost (BRL) (%) | Cost-a (BRL)a |
| 60-69 | Male | 88,775 (13.5) | 6.2 | 3.9 | 71,210,621.44 (10.1) | 181,606,293.06 | 238,306 (36.2) | 6.1 | 3.7 | 310,603,500.11 (44.2) | 407,228,826.39 | 327,081 (49.7) | 381,814,121.55 (54.3) | 588,835,119.45 |
| Female | 88,693 (13.5) | 5.2 | 1.6 | 65,665,838.23 (9.4) | 167,795,454.52 | 242,484 (36.8) | 5.2 | 1.4 | 254,747,242.75 (36.3) | 334,294,757.11 | 331,177 (50.3) | 320,413,080.9 (45.7) | 502,090,211.63 | |
| Total | 177,468 (27.0) | - | - | 136,876,459.67 (19.5) | 349,401,747.58 | 480,790 (73.0) | - | - | 565,350,742.86 (80.5) | 741,523,583.50 | 658,258 (37.7) | 702,227,208.53 (30.3) | 1,090,925,331.08 | |
| 70-79 | Male | 59,219 (10.6) | 7.0 | 6.0 | 57,751,976.69 (7.6) | 141,841,581.90 | 150,666 (26.8) | 7.5 | 11.4 | 243,040,470.22 (32.1) | 320,571,075.71 | 209,885 (37.4) | 300,792,446.91 (39.7) | 462,412,657.61 |
| Female | 97,916 (17.4) | 6.4 | 2.8 | 95,064,156.09 (12.5) | 233,955,428.37 | 254,139 (45.2) | 7.4 | 7.2 | 362,382,945.39 (47.8) | 478,453,069.54 | 352,055 (62.6) | 457,447,101.48 (60.3) | 712,408,497.91 | |
| Total | 157,135 (28.0) | - | - | 152,816,132.78 (20.1) | 375,797,010.27 | 404,805 (72.0) | - | - | 605,423,415.61 (79.9) | 799,024,145.25 | 561,940 (32.2) | 758,239,548.39 (32.8) | 1,174,821,155.52 | |
| 80-89 | Male | 39,442 (7.5) | 7.3 | 9.1 | 44,789,748.16 (5.2) | 109,631,518.89 | 114,915 (21.9) | 7.5 | 11.4 | 213,932,613.33 (25.0) | 279,822,337.95 | 154,357 (29.4) | 258,722,361.49 (30.2) | 389,453,856.84 |
| Female | 92,798 (17.6) | 7.3 | 5.6 | 107,464,653.41 (12.6) | 263,326,248.13 | 278,744 (53.0) | 7.4 | 7.2 | 488,741,930.93 (57.2) | 639,717,858.52 | 371,542 (70.6) | 596,206,584.34 (69.8) | 923,044,106.65 | |
| Total | 132,240 (25.1) | - | - | 152,254,401.57 (17.8) | 372,957,767.02 | 393,659 (74.9) | - | - | 702,674,544.26 (82.2) | 919,540,196.47 | 525,899 (30.1) | 854,928,945.83 (36.9) | 1,292,497,963.49 | |
| Total | 466,843 (26.7) | - | - | 441,946,994.02 (19.1) | 1,098,156,524.85 | 1,279,254 (73.3) | - | - | 1,873,448,702.73 (80.9) | 2,460,087,925.23 | 1,746,097 (100.0) | 2,315,395,702.75 (100.0) | 3,558,244,450.08 | |
a) Cost adjusted (cost-a) for inflation, according to National Consumer Price Index-Extended (IPCA).
In the age group 60 to 69 years, it could be seen the highest proportional participatory hospitalizations due to falls among older people (37.7%), which corresponded to 30.3% of the total cost of these hospitalizations; a 5.5% lower value (32.2%) was observed in the number of hospitalizations among those aged 70 to 79 years, although the costs corresponding to this age group were higher, 32.8% of the total value of these hospitalizations; and finally, the cost of these hospitalizations among those aged 80 years and older represented 36.9% of the total cost of hospitalizations of older people due to falls (Table 1).
There was a higher proportion of hospitalizations due to falls among older female: 60.4% of all hospitalizations, 50.3% in the age group 60 to 69 years, 62.6% for those aged 70 to 79 years, and 70.6% among those aged 80 years or older (Table 1).
The cost of hospitalizations due to falls among the population aged 60 to 69 years was BRL 702,227,208.53, and 54.3% of which was allocated to male hospitalizations. For the same age group, the average length of stay in hospital was 6.2 days for male and 5.2 days for female; in addition, the in-hospital case fatality ratio among male in this age group was more than double that of female: 3.9% versus 1.6% between 2000 and 2007; and 3.7% versus 1.4% between 2008 and 2020 (Table 1).
In the age groups 70 to 79 and 80 years and older, in-hospital case fatality ratio among male was also higher. Among older adults aged 70 to 79 years, in the periods 2000-2007 and 2008-2020, the in-hospital case fatality ratio among male was 6.0% and 11.4%, respectively, versus 2.8% and 7.2% among female. In the age group 80 years and older, for the same periods, the in-hospital case fatality ratio was 9.1% and 11.4% for male versus 5.6% and 7.2% for female. However, the majority of hospitalizations due to falls among the general older population, during both periods, occurred among female sex (Table 1).
In the period 2000 to 2019, there was an increase of 162.2% in the number of hospitalizations due to falls among older adults, followed by a decrease of 12.6% between 2019 and 2020, according to data and trend lines showed in Figure 1.
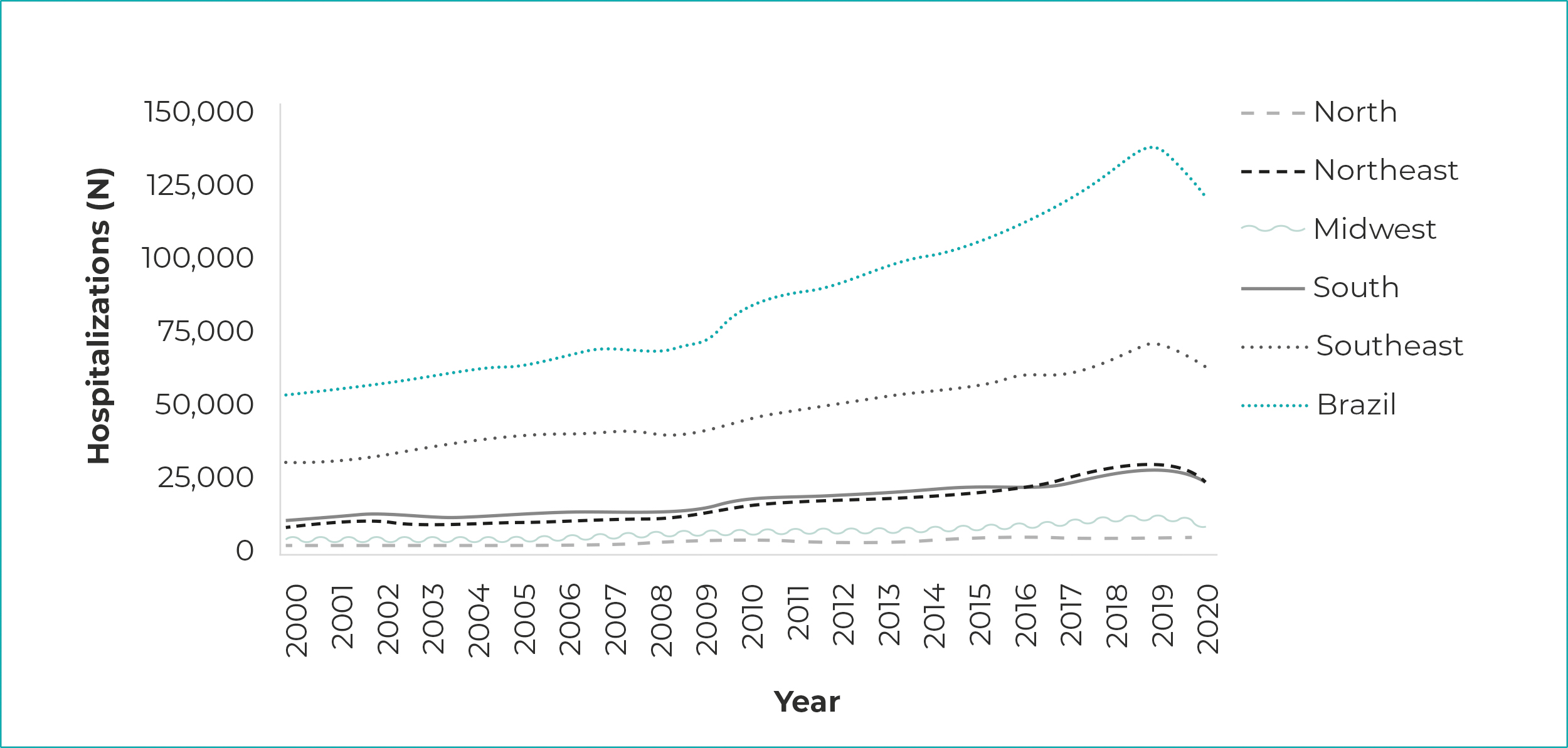
Figure 1 - Number of hospital admission authorizations due to falls among the older population, by regions, Brazil, 2000-2020
Regarding the total amount paid for hospitalizations, Figure 2 shows a trend of rising costs between 2000 and 2019, and therefore a reduction in the total cost of hospitalizations in 2020, compared to the previous year.
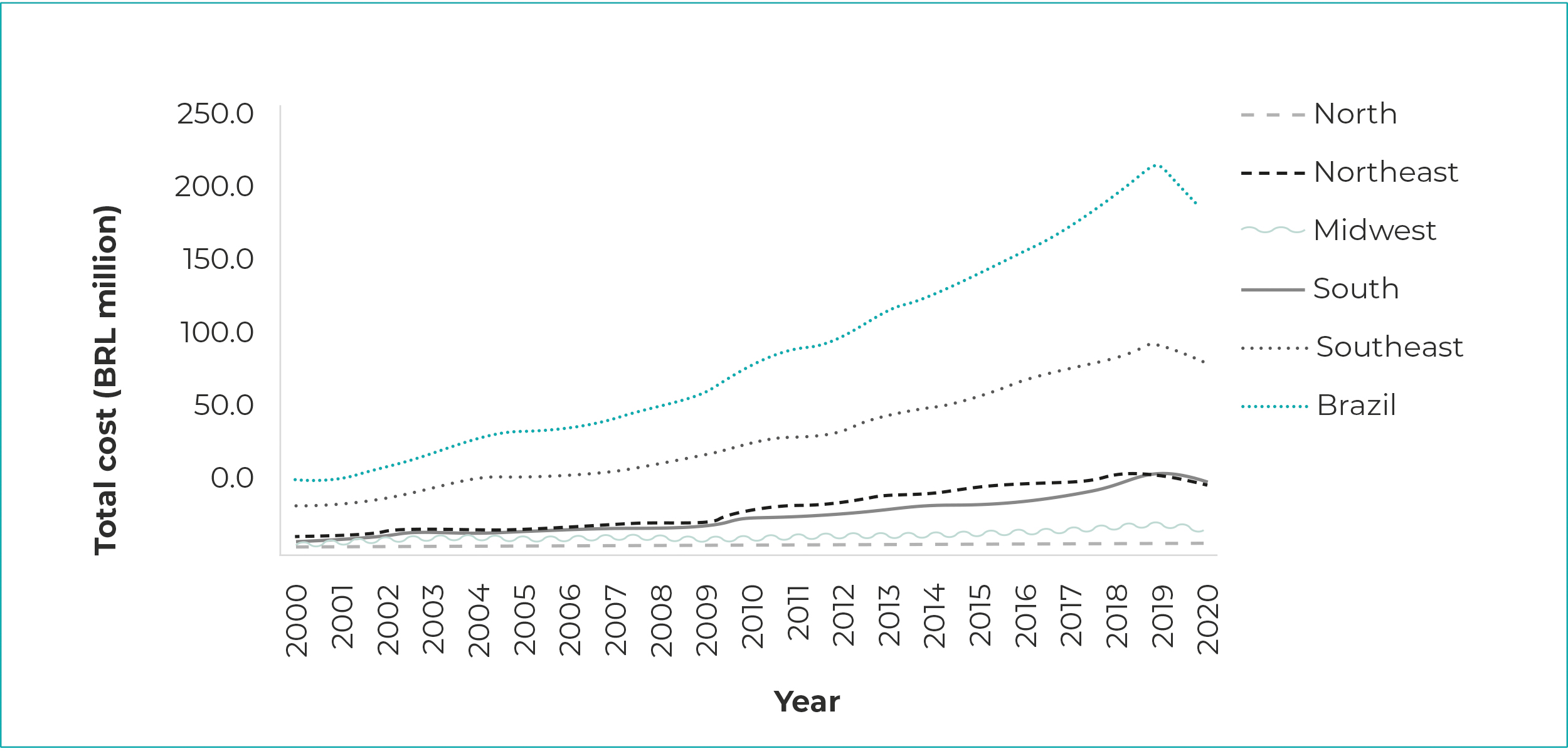
Figure 2 - Total cost [in Brazilian real (BRL) million] of hospital admission authorizations due to falls among the older population, by regions, Brazil, 2000-2020
The region with the highest proportion of hospitalizations due to falls was the Southeast, accounting for 54.4% of the country’s total hospitalizations, followed by the South (18.6%) and Northeast (17.8%) regions. With regard to the costs recorded, the Southeast region showed the highest proportion of the total cost of hospitalizations due to falls among older people in the country (57.3%), also followed by the South (19.2%) and Northeast (16.1%) regions, as shown in Table 2.
Table 2 - Absolute (N) and relative (%) frequencies of hospital admission authorizations due to falls among the older population, and total cost [in Brazilian real (BRL) million], by regions, Brazil, 2000-2020
| Region | Hospitalizations | Hospitalization costs | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | Average | Standard deviation | Total cost (BRL) | Total cost (%) | Averagea | Standard deviation | Total costb | ||
| North | 46,266 | 2.7 | 2,203.1 | 682.1 | 37,905,660.13 | 1.8 | 1.8 | 0.9 | 59,325,076.40 | |
| Northeast | 306,734 | 17.8 | 14,606.4 | 6,273.5 | 370,425,099.31 | 16.1 | 17.6 | 10.8 | 550,379,755.43 | |
| Midwest | 112,967 | 6.5 | 5,379.4 | 2,106.8 | 126,915,524.12 | 5.6 | 6.0 | 3.3 | 194,815,054.77 | |
| Southeast | 950,227 | 54.4 | 45,248.9 | 11,746.1 | 1,322,905,588.79 | 57.3 | 63.0 | 29.4 | 2,063,901,180.94 | |
| South | 325,065 | 18.6 | 15,479.3 | 5,190.3 | 441,674,214.73 | 19.2 | 21.8 | 12.1 | 689,823,382.54 | |
| Total | 1,746,097 | 100.0 | 16,583.4 | 16,561.6 | 2,315,395,729.75 | 100.0 | 110.3 | 26.4 | 3,558,244,450.08 | |
a) Amounts are expressed in BRL millions. b) Total cost adjusted for inflation, according to National Consumer Price Index-Extended (IPCA).
DISCUSSION
The total cost of hospital admissions due to falls among the older population was directly proportional to age, that is, progressively higher with increasing age. In addition, the largest number of hospitalizations was observed among female and in the Southeast region of the country.
Although older adults aged 80 years and older have had the lowest number of hospitalizations, when compared to the other age groups, their higher cost for the health care system is related to the longer average length of stay in hospital. In spite of the fact that comorbidities, polypharmacy and associated complications have not been the focus of this study and, according to the literature, they may contribute to increased costs and the average length of stay in hospital among this population.19
Another study, which analyzed hospitalizations due to falls among older people and their costs within the SUS between 2005 and 2010,19 showed that the average of stay in hospital increased with increasing age, and that older people aged 80 years and older presented the highest average length of stay in hospital, attributed to a higher frequency of comorbidities when compared to other age groups. However, the same study observed that the number of hospitalizations decreased with increasing age.
The identification of a higher frequency of hospitalizations among older female, compared to older male, observed in this study, corroborates the results of a similar research based on data from DATASUS, regarding Brazil, considering the period 2005 to 2010,19 when 59.7% of hospitalizations due to falls among older female were identified. Factors such as the highest incidence of osteoporosis, changes related to menopause, which may interfere with hormonal balance, as well as muscle mass reduction and a higher life expectancy for female, when compared to male, are possible causes for a higher prevalence of falls among this population group.1,20
Although the number of hospitalizations was higher among female, the length of stay in-hospital and mortality rate were higher among male. These findings corroborate the results of a study that analyzed the trends in morbidity and in-hospital case fatality case due to falls among older people in Brazil, in the period 1996 to 2012, whose authors, Abreu et al., attributed to the fact that male engage more often in risky behaviors, which would cause more severe falls.21
There was an increase in the number of hospitalizations and their total cost in the period 2000 to 2019, followed by a reduction in 2020. It is possible that the reduction in hospitalizations observed in the last year of the study period is related to the recommendation of social isolation as a control measure during the COVID-19 pandemic, when the older people stayed at home, thus reducing the risk of accidents.22 However, home isolation made it difficult to practice physical exercise among this population, which usually lead to a reduction in muscle mass and strength, enhancing the risk of falls6 and, consequently, the need - and opportunity - to implement prevention and health promotion measures, such as encouraging the practice of physical activities at home.23
The values of the table of SUS procedures were unified in 2008, when the Management System of the Table of Procedures Medicines and OPM of SUS (SIGTAP) was created, which allows to issue reports on the diagnostic, clinical and surgical procedures performed, medicines, orthotics, prosthetics and special materials used, as well as transplantations and prevention and health promotion measures. It was not possible to obtain these data over the period 2000 to 2007, due to the date of creation of the SIGTAP.
It could be seen that the number of hospitalizations due to falls and their costs were higher in the Southeast region, followed by the South and Northeast regions. This result can be explained by Brazil demographics profile. According to data from IBGE, the Southeast region concentrates about 50% of the older population, while the Northeast and South regions, 24.7% and 16.4% of this population, repectively.24 Other studies corroborate these findings and point to the Southeast, South and Northeast as the regions with the highest costs of hospitalizations due to falls among older adults in the country. The high frequency of comorbidities in the population of these regions possibly contributes to the greatest impact on expenditure on the services provided by public health.19,25 These data enable the implementation of public policies, priority actions and investments, especially the development of prevention strategies focused not only on vulnerable groups, but also on regions with a considerable proportion of susceptible ones.10
The variation in quality of information system records in different regions in the country may influence the results observed, as some evidence has shown that data on hospitalizations due to external causes, such as falls, are of higher quality in the South and Southeast regions.21
In addition to direct costs, it should also be taken into consideration the indirect costs resulting from the event, which represent economic and social costs due to premature deaths, incapacity for work, loss or reduction of productivity due to physical limitations and/or temporary or permanent absences from work, among individuals who experienced falls.6,26 In addition to social impact, falls among older people bring economic consequences to families, which may affect family income, given the need to bear extraordinary expenditures on the care and treatment of possible sequelae of the falls. Moreover, there is a natural increase in dependence among older people due to problems resulting from falls, which,27 in the face of a possible family burden, may affect the quality of life of all family members.
This study has as a limitation the use of secondary data, related to AIHs, which may not represent all hospitalizations due to falls in the SUS, given the possibility that some events have been recorded using other ICD-10 codes, such as those related to outcomes rather than the fall itself. In addition, hospitalization costs go beyond the AIH costs, and there may be expenditures on unplanned professionals and therefore not covered by the AIH, special table procedures of high complexity and other items, whose costs were not included. Moreover, the completion of the AIH in the SUS is sensitive to clinical knowledge, work processes design and data categorization. Another limitation of the study is the fact that new hospitalizations or the transfer of the same individual to another hospital is not identified by SIH/SUS, which may result in cumulative counts.
Despite this limitation, within the scope of the SUS, DATASUS has been widely used in the country, in studies that assess health care costs.11 Government databases constitute a reliable, legitimate source, enabling interventions and supporting decision-making.12,25 Furthermore, the values provided by DATASUS were related to the amount paid to health institutions, which may not correspond to the amount invested in the treatment of falls.
Although the financial support, showed in this study, was related to the health care for people who experienced falls outside health institutions, falls among older adults may lead to new falls, characterizing another limitation of this study, given that it was not possible to identify whether the new falls occurred inside health institutions and that they were related to individuals who experienced previous falls in outdoor environments.
Notwithstanding the study focuses on the analysis of economic costs of hospitalizations due to falls, it is worth mentioning that in health care settings, there is a human cost for professionals who are responsible for older people. When an individual who is hospitalized falls, this fact not only affects him or her and his family but also the reputation of the professional who is taking care of him or her, and depending on the severity of the event, it may result in reputational damage, leading this professional to face social stigmas, and cause impact on his professional and personal life. In addition, this cost can be high to health institutions regarding their public image, in view of the fragility of the work processes involved in the care of older people.
It can be concluded that the rates of hospitalizations due to falls among older people in the SUS increased in all regions of the country, during the period studied, generating high costs for the public health system in Brazil, except for the year 2020, when there was a reduction in hospitalization costs, possibly due to isolation measures during the COVID-19 pandemic.
Falls are considered, in most cases, preventable events. Therefore, public managers, health professionals and general society should establish effective strategies and measures aimed at their prevention, especially with regard to the older population, naturally more vulnerable given the aging process.
Greater investments in the prevention and health promotion measures, and particularly in the object of this study, are needed. Investments in falls prevention programs aimed at the older population. Such measures will contribute to a safer aging, reducing the risk of falls and providing better quality of life, resulting in reduction of hospitalizations and strengthening of community-based services by means of primary health care. The amount spent on the treatment of falls among older people justifies the investment in public health strategies, either in the promotion of inclusive practices and intersectoral actions, focused on healthy aging, or the acquisition of adequate appliances and furniture for the use of older people in their daily living.
REFERÊNCIAS
1. Luzia MF, Prates CG, Bombardelli CF, Adorna JB, Moura GMSS. Características das quedas com dano em pacientes hospitalizados. Rev Gaucha. Enferm. 2019;40(Esp): e20180307. DOI: 10.1590/1983-1447.2019.20180307 [ Links ]
2. Marinho CL, Nascimento V, Bonadiman, BSR, Torres SRF. Causas e consequências de quedas de idosos em domicílio. Braz. J. Hea. Rev. 2020; 3(3):6880-96. DOI: 10.34119/bjhrv3n3-225 [ Links ]
3. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. The medical costs of fatal falls and fall injuries among older adults. J Am Geriatr Soc. 2018;66(4):693-8. DOI: 10.1111/jgs.15304 [ Links ]
4. Miranda DP, Santos TD, Espírito Santo FH, Chibante CLP, Barreto EA. Quedas em idosos em ambiente domiciliar: uma revisão integrativa. REAID. 2017;(edição especial):120-9. DOI: 10.31011/reaid-2017-v.2017-n.0-art.560 [ Links ]
5. Oliveira SRN, Messias FML, Cândido JAB, Torres GMC, Figueiredo IDT, Pinto AGA, et al. Fatores associados a quedas em idosos: inquérito domiciliar. Rev Bras Promoç Saúde. 2021;34:10998. DOI: 10.5020/18061230.2021.10998 [ Links ]
6. Teixeira DKS, Andrade LM, Santos JLP, Caire ES. Quedas em pessoas idosas: restrições do ambiente doméstico e perdas funcionais. Rev. Bras. Geriatr. Gerontol. 2019;22(3):e180229. DOI: 10.1590/1981-22562019022.180229 [ Links ]
7. Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res. 2016;58:99-103. DOI: 10.1016/j.jsr.2016.05.001 [ Links ]
8. Agência Nacional de Vigilância Sanitária (BR). Gestão de riscos e investigação de eventos adversos relacionados à assistência à saúde [Internet]. Brasília (DF): Anvisa; 2017[citado 2021 maio 2]. 94 p. (Série segurança do paciente e qualidade em serviços de saúde; Caderno 7). Disponível em: Disponível em: https://www.segurancadopaciente.com.br/wp-content/uploads/2017/09/Caderno-7-Gest%C3%A3o-de-Riscos-e-Investiga%C3%A7%C3%A3o-de-Eventos-Adversos-Relacionados-%C3%A0-Assist%C3%AAncia-%C3%A0-Sa%C3%BAde.pdf [ Links ]
9. Falcão RMM, Costa KNFM, Fernandes MGM, Pontes MLF, Vasconcelos JMB, Oliveira JS. Risco de quedas em pessoas idosas hospitalizadas. Rev Gaucha Enferm. 2019;40(esp):e20180266. DOI: 10.1590/1983-1447.2019.20180266 [ Links ]
10. Vieira LS, Gomes AP, Bierhals IO, Farías-Antúnez S, Ribeiro CG, Miranda VIA, et al. Quedas em idosos no sul do Brasil: prevalência e determinantes. Rev Saude Publica. 2018;52:22. DOI: 10.11606/S1518-8787.2018052000103 [ Links ]
11. Ministério da Saúde (BR). Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Diretrizes metodológicas: diretriz de avaliação econômica. 2 ed. [citado 2021 out 1]. Brasília: Ministério da Saúde; 2014. 131 p. Disponível em: Disponível em: https://bvsms.saude.gov.br/bvs/publicacoes/diretrizes_metodologicas_diretriz_avaliacao_economica.pdf [ Links ]
12. Ministério da Saúde (BR). Departamento de Informática do SUS - DATASUS. Base de dados do Sistema de Informações Hospitalares do SUS - SIH/SUS [Internet]. [citado 2021 abr 5] Disponível em: Disponível em: http://www2.datasus.gov.br/DATASUS/index.php?area=0203&id=6926 [ Links ]
13. Silva EN, Silva MT, Pereira MG. Incerteza em estudos de avaliação econômica. Epidemiol Serv Saude. 2017;26(1):211-3. DOI: 10.5123/S1679-49742017000100022 [ Links ]
14. Instituto Brasileiro de Geografia e Estatística. Censo demográfico [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2021 [citado 2021 ago 28]. Disponível em: Disponível em: https://www.ibge.gov.br/estatisticas/sociais/administracao-publica-e-participacao-politica/9663-censo-demografico-2000.html?=&t=resultados [ Links ]
15. Ministério da Saúde (BR). Sistema de Informações Hospitalares (SIH). História. [Internet], 2020 [atualizado 2020 dez 4; citado 2021 set 04]. Disponível em: Disponível em: https://wiki.saude.gov.br/sih/index.php/P%C3%A1gina_principal [ Links ]
16. Silva EN, Silva MT, Pereira MG. Identifying, measuring and valuing health costs. Epidemiol Serv Saúde. 2016;25(2):437-9. DOI:10.5123/S1679- 49742016000200023 [ Links ]
17. Brasil. Ministério da Saúde. Portaria nº 529, de 1 de abril de 2013. Institui o Programa Nacional de Segurança do Paciente (PNSP) [Internet]. Diário Oficial da União. 1 abr. 2013 [citado 2021 maio 1]; Seção 1:43. Disponível em: Disponível em: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt0529_01_04_2013.html [ Links ]
18. Brasil. Ministério da Saúde. Resolução nº 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos e dispõe sobre as atribuições da Comissão Nacional de Ética em Pesquisa - Conep e dos Comitês de Ética em Pesquisa - CEP. Diário Oficial da União, Brasília (DF), 13 jun 2013 [citado 2021 ago 31]. Seção 1: Disponível em: Disponível em: https://bvsms.saude.gov.br/bvs/saudelegis/cns/2013/res0466_12_12_2012.html [ Links ]
19. Barros IFO, Pereira MB, Weiller TH, Anversa ETR. Internações hospitalares por quedas em idosos brasileiros e os custos correspondentes no âmbito do Sistema Único de Saúde. Revista Kairós Gerontologia. 2015;18(4):63-80. DOI: 10.23925/2176-901X.2015v18i4p63-80 [ Links ]
20. Instituto Brasileiro de Geografia e Estatística. Tábuas completas de mortalidade para o Brasil - 2015: breve análise de evolução da mortalidade no Brasil [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística ; 2016 [citado 2021 mai 7]. Disponível em: Disponível em: https://biblioteca.ibge.gov.br/visualizacao/periodicos/3097/tcmb_2015.pdf [ Links ]
21. Abreu DROM, Novaes ES, Oliveira RR, Mathias TAF, Marcon SS. Internação e mortalidade por quedas em idosos no Brasil: análise de tendência. Cienc Saude Colet. 2018;23(4):1131-41. DOI: 10.1590/1413-81232018234.09962016 [ Links ]
22. Hammerschmidt KSA, Santana RF. Saúde do idoso em tempos de pandemia Covid-19. Cogitare Enferm. 2020;25:e72849. DOI: 10.5380/ce.v25i0.72849 [ Links ]
23. Pereira E, Tanaka AK, Paczek R, Lana L. Consequências do isolamento social nos idosos em domicílio em tempos de pandemia por Covid-19. RBCEH. 2020;17(2):61. DOI: 10.5335/rbceh.v17i2.11959 [ Links ]
24. Instituto Brasileiro de Geografia e Estatística. Projeções da população do Brasil e Unidades da Federação por sexo e idade: 2010-2060 [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2018 [citado 2021 abr 8]. Disponível em: Disponível em: https://www.ibge.gov.br/estatisticas/sociais/populacao/9109-projecao-da-populacao.html?=&t=resultados [ Links ]
25. Silveira FJ, Oliveira VSL, Friedrich FO, Heinzmann-Filho JP. Internações e custos hospitalares por quedas em idosos brasileiros [Internet]. Sci Med. 2020;30(1):e36751. DOI: 10.15448/1980-6108.2020.1.35751 [ Links ]
26. Siqueira ASE, Siqueira-Filho AG, Land MGP. Análise do impacto econômico das doenças cardiovasculares nos últimos cinco anos no Brasil. Arq Bras Cardiol. 2017;109(1):39-46. DOI: 10.5935/abc.20170068 [ Links ]
27. Luzardo AR, Paula Júnior NF, Medeiros M, Wolkers PCB, Santos SMA. Repercussions of hospitalization due to fall of the elderly: health care and prevention. Rev Bras Enferm. 2018;71(Suppl 2):763-9. DOI: 10.1590/0034-7167-2017-0069 [ Links ]
Received: July 27, 2021; Accepted: December 13, 2021











 texto em
texto em 


