Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Epidemiologia e Serviços de Saúde
versión impresa ISSN 1679-4974versión On-line ISSN 2237-9622
Epidemiol. Serv. Saúde vol.31 no.1 Brasília 2022 Epub 22-Abr-2022
http://dx.doi.org/10.1590/s1679-49742022000100020
Research Note
COVID-19 vaccine hesitancy in a national sample of older Brazilians: the ELSI-COVID Initiative, March 2021
1 Fundação Instituto Oswaldo Cruz, Instituto René Rachou, Belo Horizonte, MG, Brazil
2 University of California, Fielding School of Public Health, Los Angeles, CA, United States
Objective:
To determine prevalence and factors associated with intention to get vaccinated against COVID-19 among older Brazilians.
Methods:
This was a cross-sectional study based on telephone interviews with participants of the Brazilian Longitudinal Study of Aging (ELSI-Brazil) aged 60 years and over, conducted in 70 municipalities in March 2021.
Results:
Among the 4,364 participants (mean age = 70.1 years), 91.8% intended to get vaccinated or had already been vaccinated, 2.5% did not intend to get vaccinated and 5.7% were undecided. Participants living in the North and Southeast regions were more likely to want to get vaccinated, as were those with two or more chronic diseases. Those who learned about COVID-19 from friends/family/social media were more likely to be undecided about vaccination (odds ratio = 3.15; 95%CI 1.28;7.77).
Conclusion:
The study identified one of the highest prevalence of intention to get vaccinated against COVID-19 described in the literature to date.
Keywords: COVID-19; Vaccines; Vaccination Refusal; Aged; Cross-Sectional Studies; Brazil
Study contributions
Main results
91.8% of the elderly informed that they intended to get vaccinated against COVID-19, by means of telephone interviews conducted in March 2021 with elderly people living in 70 Brazilian municipalities.
Introduction
In the global context, Brazil stands out as one of the countries most affected by the COVID-19 pandemic, coming in second place in terms of number of deaths: 401,186, as at April 29th 2021.1,2 Vaccines against COVID-19 are the most important strategy for controlling the pandemic.2 However, it is imperative that they be available and adhered to by the population. A meta-analysis based on 28 studies conducted in 2020 showed that the intention to get vaccinated against COVID-19 varied widely, from 50% to 90% across populations, with an overall average of 73%.2 In some scenarios, lower propensity to get vaccinated was observed among non-Whites or immigrants and/or among those with lower levels of education.2
Vaccination against COVID-19 in Brazil began in January 2021, through the Ministry of Health National Immunization Program. The populations selected as a priority for vaccination were health professionals, indigenous and quilombola communities and, successively, the different age groups among the elderly.3 The vaccines approved by the National Health Surveillance Agency (Agência Nacional de Vigilância Sanitária - ANVISA) and available in Brazil at the time of the study, were CoronaVac® and Oxford/AstraZeneca®.4,5
The objective of this study was to determine prevalence and factors associated with the intention to get vaccinated against COVID-19 among elderly Brazilians.
Methods
Design
This was a cross-sectional study of data on participants of the Brazilian Longitudinal Study of Aging (ELSI-Brazil). ELSI-Brazil is a household-based survey, conducted with a national sample representing the population aged 50 years or more. The survey is conducted in 70 municipalities, distributed over Brazil’s five major regions. In 2015-2016 the baseline cohort had 9,412 participants. The 2nd wave of ELSI-Brazil began in August 2019 and was interrupted in March 2020, due to the SARS-CoV-2 pandemic. More details about ELSI-Brazil can be seen on the survey website and in a previous publication.6
The ELSI-COVID-19 initiative is based on telephone interviews with participants of the 2nd wave of ELSI-Brazil,7 conducted in five rounds (Figure 1). All participants aged 60 years and older who were reached by the telephone survey conducted in March 2021 (Round 5) were selected for our analysis.

Figure 1 Schematic diagram of the Longitudinal Study of the Health of Older Brazilians (ELSI-Brazil) and the ELSI-COVID-19 Initiative
Variables
The study’s dependent variable was the intention to get vaccinated (yes; no; does not know/is undecided), measured by asking interviewees Do you intend to get vaccinated when the vaccine against COVID-19 becomes available? Those who had received at least the first dose of the vaccine were included in the ‘yes’ group.
The independent variables were: age group (in years: 60-69; 70-79; 80 and over); sex (male; female); years of schooling (up to 4; 5-8; 9-11; 12 and over); living in a rural zone or an urban zone; major Brazilian region of resident (North; Northeast; Midwest; Southeast; South); number of chronic diseases present (none; one; two or more), being registered with the Family Health Strategy; the main source from which interviewees obtained information about COVID-19 (Ministry of Health, traditional media - TV channels and newspapers - , family members, friends or social media; other sources); main reasons for vaccine hesitancy, among those who reported being hesitant (afraid of adverse reactions; does not feel sufficiently informed about the benefits; does not believe that vaccination protects against COVID-19; afraid that vaccination will harm you; not afraid of getting infected with coronavirus; doctor advised against vaccination; relatives and friends think you should not get vaccinated; have had COVID-19; afraid of injections; other reason). Chronic diseases considered were those previously described as being associated with increased risk of COVID-19 complications,8 namely: cardiovascular diseases (myocardial infarction, heart failure and/or angina pectoris); diabetes mellitus; chronic pulmonary diseases; obesity [body mass index (BM) ≥30 kg/m2]. Obesity was confirmed by taking physical measurements, while presence of the remaining conditions was based on self-reported medical diagnosis.
The answers to questions about COVID-19 were obtained in the fifth round of the telephone survey, while the remaining information was taken from the second face-to-face wave of ELSI-Brazil.
Statistical analysis
The descriptive analyses were based on means, standard deviation and estimates of prevalence along with their respective confidence intervals (95%CI). In order to examine the magnitude of differences between groups, odds ratios (ORs) were estimated by means of multinomial logistic regression, using models adjusted for sex and age, taking the ‘wants to get vaccinated/has been vaccinated’ category as the reference category. All the analyses took into consideration the weightings specifically derived for the telephone survey respondents and the sample parameters.7 The analyses were performed used Stata® (v.14).
Ethical aspects
The study projects were approved by the Research Ethics Committee of the Fundação Instituto Oswaldo Cruz in Minas Gerais, Certificate of Submission for Ethical Appraisal, No. 34649814.3.0000.5091, Opinion No. 2.111.911, issued on June 9th 2017, and Certificate of Submission for Ethical Appraisal, No. 33492820.3.0000.5091, Opinion No. 4.138.284, issued on July 6th 2020, respectively.
Results
Out of the 9,177 participants of the second face-to-face wave of ELSI-Brazil (August 2019 to March 2020), 6,309 (68.7%) answered the fifth round of telephone interviews (March 1st to 14th 2021) (Figure 1); 4,364 of these respondents were aged 60 or over and were included in this analysis (mean age was 70.1 years; standard deviation 7.9); 3,202 of the latter intended to get vaccinated, while 798 had already been vaccinated, totaling 4,000 individuals (91.8%; 95%CI 89.5;93.5). Prevalence of those who did not intend to get vaccinated was 2.5% (95%CI 1.9;3.4), while prevalence of those who did not know whether they would get vaccinated or who were undecided was 5.7% (95%CI 4.2;7.6), corresponding to 135 and 229 individuals, respectively (Table 1).
Table 1 Relative frequencies and results of the multivariate analysis and factors associated with intention to get vaccinated, among adults aged 60 or over, the ELSI-COVID-19 Initiative, March 1st to 14th, 2021
| Characteristics | n (%)a | Intention to get vaccinated against COVID-19 | ||||
|---|---|---|---|---|---|---|
| Already vaccinated or intention to get vaccinated (reference) | Does not intend to get vaccinated | Undecided or does not know | ||||
| %b (95%CIc) | %b (95%CIc) | ORd (95%CIc) | %b (95%CIc) | ORd (95%CIc) | ||
| Total sample | 4,364 (100.0) | 91.8 (89.5;93.5) | 2.5 (1.9;3.4) | - | 5.7 (4.2;7.6) | - |
| Age group | ||||||
| 60-69 | 2,270 (55.6) | 91.5 (88.6;93.7) | 2.3 (1.6;3.4) | 1.00 | 6.2 (4.4;8.7) | 1.00 |
| 70-79 | 1,447 (30.6) | 90.0 (84.3;93.7) | 3.5 (2.0;5.9) | 1.53 (0.77;3.02) | 6.5 (3.4;12.2) | 1.08 (0.48;2.47) |
| ≥80 | 647 (13.8) | 96.7 (94.5;98.0) | 1.4 (0.8;2.6) | 0.58 (0.28;1.20) | 1.9 (0.9;3.9) | 0.29 (0.13;0.66) |
| Sex | ||||||
| Female | 2,638 (49.3) | 92.4 (90.3;94.1) | 2.7 (2.0;3.7) | 1.00 | 4.9 (3.5;6.9) | 1.00 |
| Male | 1,726 (50.7) | 91.2 (87.3;93.9) | 2.4 (1.4;4.0) | 0.87 (0.48;1.57) | 6.5 (4.0;10.4) | 1.35 (0.70;2.60) |
| Years of schooling | ||||||
| <4 | 2,704 (35.9) | 91.9 (89.4;93.9) | 2.9 (1.9;4.4) | 1.00 | 5.2 (3.9;6.8) | 1.00 |
| 5-8 | 754 (27.2) | 94.1 (91.6;95.9) | 2.3 (1.4;3.8) | 0.75 (0.38;1.49) | 3.6 (2.2;5.8) | 0.61 (0.39;0.95) |
| 9-11 | 627 (8.1) | 91.9 (88.1;94.5) | 4.6 (2.6;8.0) | 1.55 (0.72;3.33) | 3.6 (2.1;5.9) | 0.61 (0.36;1.05) |
| ≥12 | 279 (28.8) | 89.3 (81.1;94.2) | 1.7 (0.5;5.5) | 0.60 (0.15;2.37) | 9.0 (4.6;16.7) | 1.68 (0.66;4.28) |
| Zone of residence | ||||||
| Urban | 3,682 (85.1) | 91.9 (89.5;93.8) | 2.5 (1.8;3.4) | 1.00 | 5.6 (4.1;7.7) | 1.00 |
| Rural | 682 (14.9) | 90.9 (85.8;94.2) | 3.0 (1.7;5.4) | 1.28 (0.66;2.48) | 6.1 (3.5;10.6) | 1.10 (0.58;2.11) |
| Region | ||||||
| Midwest | 531 (9.8) | 90.2 (84.3;94.1) | 3.6 (2.1;6.0) | 1.00 | 6.3 (3.4;11.1) | 1.00 |
| North | 148 (6.1) | 97.2 (93.4;98.8) | 0.3 (0.0;1.6) | 0.08 (0.01;0.46) | 2.5 (0.1;6.2) | 0.33 (0.10;1.02) |
| Northeast | 1,225 (25.6) | 92.6 (89.2;94.9) | 3.4 (2.1;5.4) | 0.90 (0.43;1.88) | 4.1 (2.6;6.4) | 0.63 (0.28;1.39) |
| Southeast | 1,831 (41.4) | 91.5 (87.2;94.4) | 1.7 (1.1;2.7) | 0.45 (0.22;0.94) | 6.8 (4.2;10.8) | 1.02 (0.47;2.21) |
| South | 629 (17.1) | 90.2 (83.2;94.5) | 3.5 (1.6;7.4) | 0.97 (0.38;2.48) | 6.3 (3.3;11.7) | 0.97 (0.38;2.48) |
| Number of chronic diseasesd | ||||||
| None | 2,042 (50.4) | 92.3 (89.8;94.2) | 2.7 (2.0;3.7) | 1.00 | 5.0 (3.4;7.4) | 1.00 |
| One | 1,411 (34.7) | 90.0 (84.8;93.5) | 1.9 (1.0;3.5) | 0.69 (0.36;1.33) | 8.1 (4.7;13.6) | 1.66 (0.82;3.39) |
| Two or more | 555 (14.9) | 96.0 (93.2;97.7) | 1.2 (0.6;2.3) | 0.41 (0.20;0.83) | 2.8 (1.4;5.6) | 0.54 (0.24;1.21) |
| Household registered with the Family Health Strategy | ||||||
| No | 1,502 (39.5) | 90.1 (85.5;93.4) | 2.8 (1.6;5.0) | 1.00 | 7.1 (4.3;11.5) | 1.00 |
| Yes | 2,783 (60.5) | 92.7 (90.7;94.3) | 2.4 (1.7;3.4) | 0.85 (0.42;1.91) | 4.9 (3.6;6.6) | 0.69 (0.38;1.26) |
| Main source of information about COVID-19 | ||||||
| Ministry of Health | 1,727 (40.7) | 93.5 (91.0;95.3) | 2.7 (1.6;4.6) | 1.00 | 3.8 (2.5;5.9) | 1.00 |
| Traditional media (TV channels and newspapers) | 1,499 (35.4) | 93.5 (87.7;96.7) | 1.2 (0.7;2.1) | 0.44 (0.20;0.94) | 5.3 (2.3;11.6) | 1.36 (0.49;3.79) |
| Family members, friends or social media | 275 (6.4) | 85.8 (77.1;91.5) | 3.6 (1.9;6.8) | 1.39 (0.59;3.24) | 10.6 (5.3;20.3) | 3.15 (1.28;7.77) |
| Other source or does not trust any of them | 677 (17.5) | 88.1 (82.8;91.9) | 4.2 (2.4;7.1) | 1.66 (0.77;3.58) | 7.7 (4.5;13.1) | 2.10 (1.02;4.31) |
| Sample size | 4,364 | 4,000e | 135 | 229 | ||
a) Percentages estimated taking column totals; b) Percentages estimated taking row totals; c) 95%CI: 95% confidence interval; d) OR: Odds ratio, estimated by multinomial logistic regression, taking the ‘wants to get vaccinated/has been vaccinated’ category as the reference category. Age group was adjusted for sex. Sex was adjusted for age group. The remaining estimates listed in the Table 1 are adjusted for sex and age group; d) Chronic diseases or conditions considered: cardiovascular disease (myocardial infarction, heart failure and /or angina pectoris), diabetes mellitus, chronic pulmonary diseases and obesity; e) 798 of these had already been vaccinated and were included in the ‘intention to get vaccinated’ category. Note: All estimates took into consideration the person’s weight and the complex design of the sample.
Table 1 also shows the participants’ characteristics and the results of the analyses of association. After adjusting for age and sex, lower odds of indecision were found among those aged 80 years or older (≥80 versus 60-69 years) (OR = 0.29; 95%CI 0.13;0.66) and among those with 5 to 8 years of schooling (5-8 versus ≤4 years) (OR = 0.61; 95%CI 0.39;0.95). Those living in the Northern region (OR = 0.08; 95%CI 0.01;0.46) and the Southeast region (OR = 0.45; 95%CI 0.22;0.94) were less likely not to want to get vaccinated, and a similar odds ratio was observed among those who sought information about COVID-19 from traditional media (OR = 0.44; 95%CI 0.20;0.94). Participants who sought information about COVID-19 from family, friends or social media (OR = 3.15; 95%CI 1.28;7.77), or who sought information from other sources or did not trust any of the sources cited (OR = 2.10; 95%CI 1.02;4.31), were more likely to be undecided about vaccination.
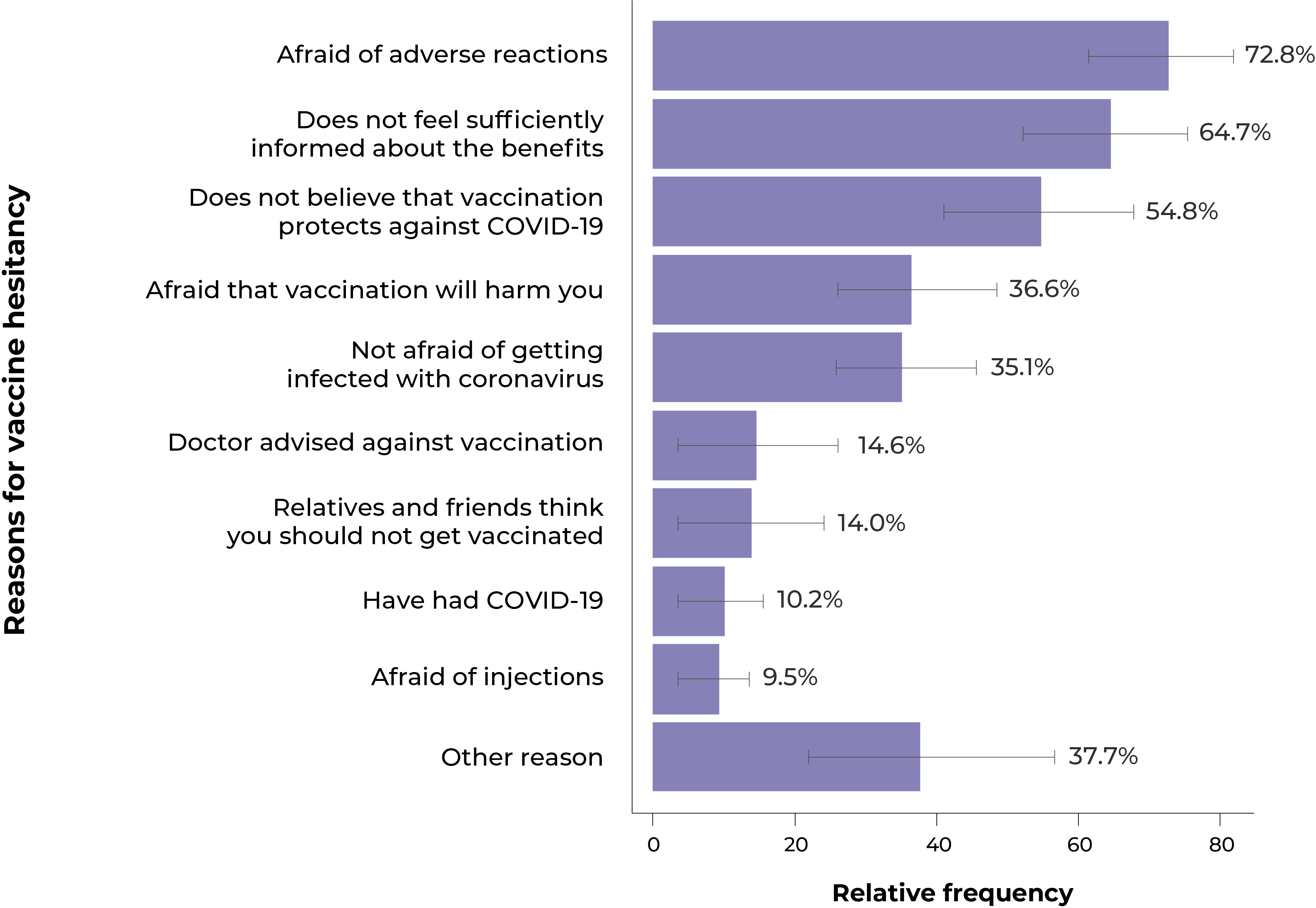
Figure 2 describes the main reasons for not getting vaccinated, among those who did not intend to get vaccinated or were undecided about the relevance of vaccination. The main reasons reported were fear of adverse reactions from the vaccine (72.8%), not feeling sufficiently informed about its benefits (64.7%), and not believing that the vaccine protects against COVID-19 (54.8%).
Discussion
The results of this study found one of the highest estimates of prevalence of intention to get vaccinated against COVID-19, compared to the findings of studies conducted in other countries, particularly in high-income countries.2,9 Vaccine uptake of around 90% in this study was higher than that found in a previous study, which used data from the fourth round of the ELSI-COVID-19 survey, conducted in November 2020.10 This increase is probably a consequence of the availability of vaccination in Brazil with effect from January 2021, the worsening of the epidemic and improvements in communication by different forms of media, including traditional media, given the recognition of the importance of immunization against COVID-19.
It is important to note that in this study, contrary to what has been found by studies conducted in some high-income countries,2,9 no significant disparities in the intention to get vaccinated among the Brazilian elderly were found according to level of education. Intention to get vaccinated varied little between the country’s major regions, although prevalence of intention to get vaccinated was higher among those living in the Northern region. This result is consistent with the dramatic crisis caused by the pandemic in that region in the early weeks of 2021.11
The factor most strongly associated with the intention to get vaccinated against COVID-19 was the source from which the elderly got information about the pandemic. Those who usually got information from friends and social media were three times more likely to be undecided about vaccination compared to those who got their information from the Ministry of Health or traditional media. Those who did not trust any source, or who were informed by other sources, were twice as likely not to want to get vaccinated.
The main advantage of the ELSI-COVID-19 initiative lies in its large population base.7 Despite this, its limitations include those inherent to surveys conducted by means of telephone interviews.7 Telephone interviews have the advantage of not exposing participants to risk of infection; however, they are prone to bias due to valid telephone numbers not being provided and/or telephone calls not being answered. The ELSI-COVID-19 Initiative response rate was approximately 70%. Using the weightings specifically derived to compensate for these losses, the sociodemographic characteristics of the study participants were similar to those of the Brazilian population of the same age.7 However, it is not possible to rule out the possibility of bias, due to factors not taken into consideration in our estimates.
Our results indicate wide adherence of Brazilian elderly people to vaccination against COVID-19. One of the most relevant results of our analysis was the strong association observed between the source of information about the pandemic and the intention to get vaccinated. Coordinated actions by the Ministry of Health, based on the best available scientific evidence, are needed to expedite the availability of vaccines, as well as the production of comprehensive information campaigns, emphasizing the impor-tance of vaccination and non-pharmacological prevention measures, even among vaccinated individuals and their contacts, until robust evidence emerges indicating that they are no longer necessary.
REFERENCES
1. COVID-19 Dashboard by the Center for Systems Science and Engineering at Johns Hopkins University (JHU) [Internet]. 2021 [citado 2021 abr 30]. Disponível em: https://coronavirus.jhu.edu/map.html [ Links ]
2. Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021 apr 8;39(15):2024-2034. doi: 10.1016/j.vaccine.2021.02.005. Epub 2021 Feb 6.PMID: 3372241. [ Links ]
3. Ministério da Saúde. Plano Nacional de Operacionalização. Entenda a ordem de vacinação contra a Covid-19 entre os grupos prioritários [Internet]. 2021 [citado 2021 jan 28]. Disponível em: http://www.gov.br [ Links ]
4. Ramasamy MN, Minassian AM, Ewer KJ, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2020 Nov 18; 396: 1979-93. doi: 10.1016/S0140-6736(20)32466-1 [ Links ]
5. Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021 Jan 9; 397(10269): 99-111. doi: 10.1016/S0140-6736(20)32661-1. Epub 2020 Dec 8.PMID: 33306989. [ Links ]
6. Lima-Costa MF, Andrade FB, Souza Jr. PRB, Neri AL, Duarte YAO, Castro-Costa E, et al. The Brazilian Longitudinal Study of Aging (ELSI-BRAZIL): objectives and design. Am J Epidemiol. 2018 Jul 1; 187(7):1345-53. doi: 10.1093/aje/kwx387 [ Links ]
7. Lima-Costa MF, Macinko J, de Andrade FB, de Souza Júnior PRB, de Vasconcellos MTL, de Oliveira CM. Iniciativa ELSI-COVID-19: metodologia do inquérito telefônico sobre coronavírus entre participantes do Estudo Longitudinal da Saúde dos Idosos Brasileiros. Cad. Saúde Pública. 2020 Oct 36(S3). doi: 10.1590/0102-311x00183120 [ Links ]
8. Center for Diseases Control and Prevention. Evidence used to update the list of underlying medical conditions that increase a person's risk of severe illness from COVID-19 [Internet]. 2020 [citado em 2020 dec 29]. Disponível em: https://cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html [ Links ]
9. Callaghan T, Moghtaderi A, Lueck JA, Hotez P, Strych U, Dor A, et al. Correlates and disparities of intention to vaccinate against COVID-19. Soc Sci Med. 2021 Mar;272:113638. Doi: 10.1016/j.socscimed.2020.113638. Epub 2021 Jan 4. [ Links ]
10. Macinko J, Seixas BV, Mambrini JVM, Lima-Costa MF. Which older Brazilians will accept a COVID-19 vaccine? Cross-sectional evidence from the Brazilian Longitudinal Study of Aging (ELSI-Brazil). BMJ Open, 2021;11:e049928. doi:10.1136/bmjopen-2021-049928 [ Links ]
11. Lima EEC, Gayawan E, Baptista EA, Queiroz BL. Spatial pattern of COVID-19 deaths and infections in small areas of Brazil. PLoS One. 2021 Feb 11;16(2):e0246808. doi: 10.1371/journal.pone.0246808. [ Links ]
Funding The baseline and second wave of ELSI-Brazil received support from the Department of Science and Technology/Science, Technology and Strategic Supplies Secretariat/Ministry of Health (DECIT/SCTIE/MS) (Files No. 404965/2012-1 and 28/2017) and also from the Elderly Health Coordination Sector of the Department of Strategic Programmatic Actions/Health Care Secretariat/Ministry of Health (File Nos. 20836, 22566, 23700 and 77/2019). The ELSI-COVID-19 survey is funded by DECIT/SCTIE and by the National Council for Scientific and Technological Development/Ministry of Science, Technology and Innovation (CNPq/MCTI), File No. 403473/2020- 9. Maria Fernanda Lima-Costa receives a study grant from CNPq/MCTI: File No. 301087/2019-9.
Received: July 13, 2021; Accepted: February 02, 2022











 texto en
texto en