INTRODUCTION
Fungal infections have been increased in recent years, and they are an important cause of mortality and morbidity in hospitalized patients1,2. This situation is mainly associated with the increasing number of immunocompromised patients, including patients of solid organ and bone marrow transplants, cancer and HIV patients, premature infants, the elderly and patients recovering from major surgeries3,4,5. Besides this, the rate of colonization in hospitalized individuals is considered higher than in general community. Clinical procedures, underlying disease and a longer hospital stay contribute to the rapid multiplication of colonizing agents that can cause infection6,7. The number of species of Candida yeast has increased over the last decades, and currently constitutes the predominant group of hospital-based fungal infections. Candida species are responsible for up to 78% of nosocomial fungal infections8,9. Although C. albicans is the main species isolated in patients with invasive fungal infections, non-albicans Candida species are becoming increasingly significant and the most important among them are: C. tropicalis, C. parapsilosis, C. glabrata, C. guilliermondii, C. krusei, and C. kefir2,10. Based on this information, this study aimed to identify and record the colonization and infection by Candida species in patients admitted to a general university hospital and mapped the distribution of the various clinical specimens in different sectors of the hospital, risk factors and the sensitivity of the isolates to antifungals.
MATERIALS AND METHODS
The study was conducted at the Hospital Universitário de Taubaté, Vale do Paraíba, São Paulo, Brazil. It is a large general university hospital, with 170 beds and receives patients mainly from the Brazilian public health system.
Clinical isolates from adults, children and neonates, who had been hospitalized for more than 72 h and with clinical suspicion of nosocomial infection, were included in this study. The classification whether as infection or colonization was carried out by the Infection Control Commission (Comissão de Controle de Infecção Hospitalar − CCIH) of the hospital, and was based on criteria defined by the Centers for Disease Control and Prevention and National Health Surveillance Agency (Agência Nacional de Vigilância Sanitária − Anvisa).
The yeasts were isolated from clinical specimens and medical equipment in different sectors of the hospital from February 2002 to February 2003, with the approval of the Ethics Committee of the hospital and Instituto de Ciências Biomédicas of the Universidade de São Paulo (number 702/CEP). Liquor, secretions (tracheal, wounds, maxillary, sputum, ear, oropharyngeal, abdominal, scrotal, anal, vaginal) catheter tip, vesical probe, blood, ascitic fluid, bronchial lavage, gastric lavage, intracaths, peritoneal fluid, pressure ulcers (bedsores) and bone fragments were all considered as clinical specimens for culture. The collection of the material for culture followed the recommendations prepared by the microbiology laboratory and CCIH.
Patient data related to age, gender, type of material to be analyzed, hospital sector, underlying disease, use of antifungal agents, corticosteroids, radiotherapy, chemotherapy and hospitalization time were recorded.
The yeasts were identified by their macroscopic, microscopic, reproductive and physiological characteristics according to the methods established by Kurtzman et al11 and by sugar assimilation using the commercial API 20C kit (bioMérieux Vitek Inc. Hazelwood, Missouri, USA). Definitive yeast identification was carried out molecularly using the ribotyping technique and the Uni-f and Uni-r primers followed by sequencing and analysis with the SeqManTM II (DNA Star Inc.) program12.
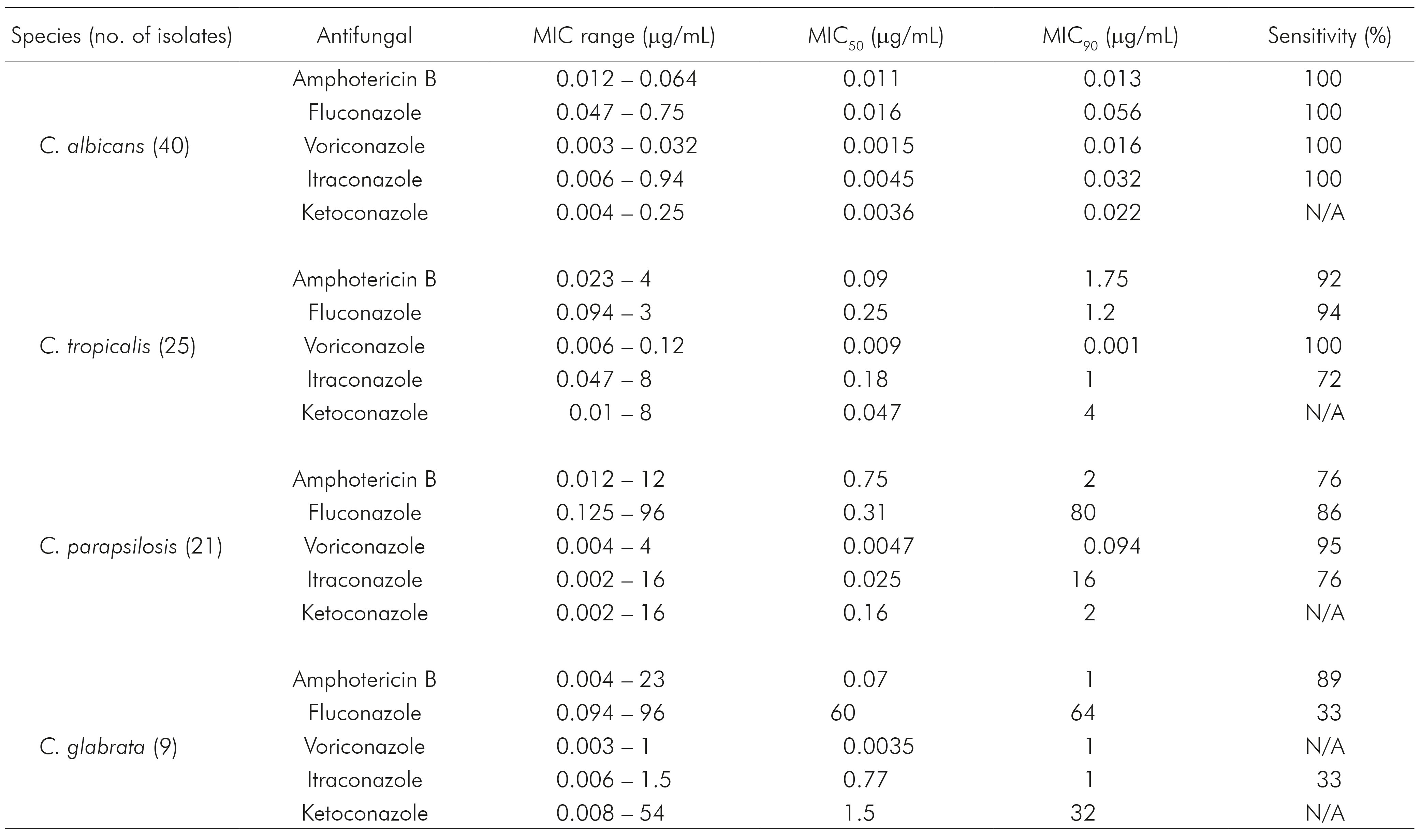
All yeasts isolates were evaluated against five antifungal agents (fluconazole, ketoconazole, itraconazole, voriconazole and amphotericin B), using the Etest(r) (bioMérieux, Solna, Sweden) method to establish the minimal inhibitory concentration (MIC). MIC interpretations follow the criteria established by M27A3 and M27S4E documents13,14.
Regarding to the amphotericin B and ketoconazole antifungals, the breakpoints were not discussed. However, values greater than 2 μg/mL for amphotericin B may be resistant, as shown by some studies. No report was found to ketoconazole. All tests used C. albicans (ATCC 90028), C. parapsilosis (ATCC 22019) and C. krusei (ATCC 6258) strains as quality controls.
RESULTS
During the study period, 954 clinical specimens and medical equipment were analyzed from 67 patients with clinical suspicion of nosocomial infection. One hundred positive cultures for Candida species were detected, which 74 were characterized as colonization cases and 26 as cases of nosocomial infection. In 43.4% of the infection cases, the patients died. Of all patients who developed these infections, 15 (65.2%) were previously colonized by the same yeasts.
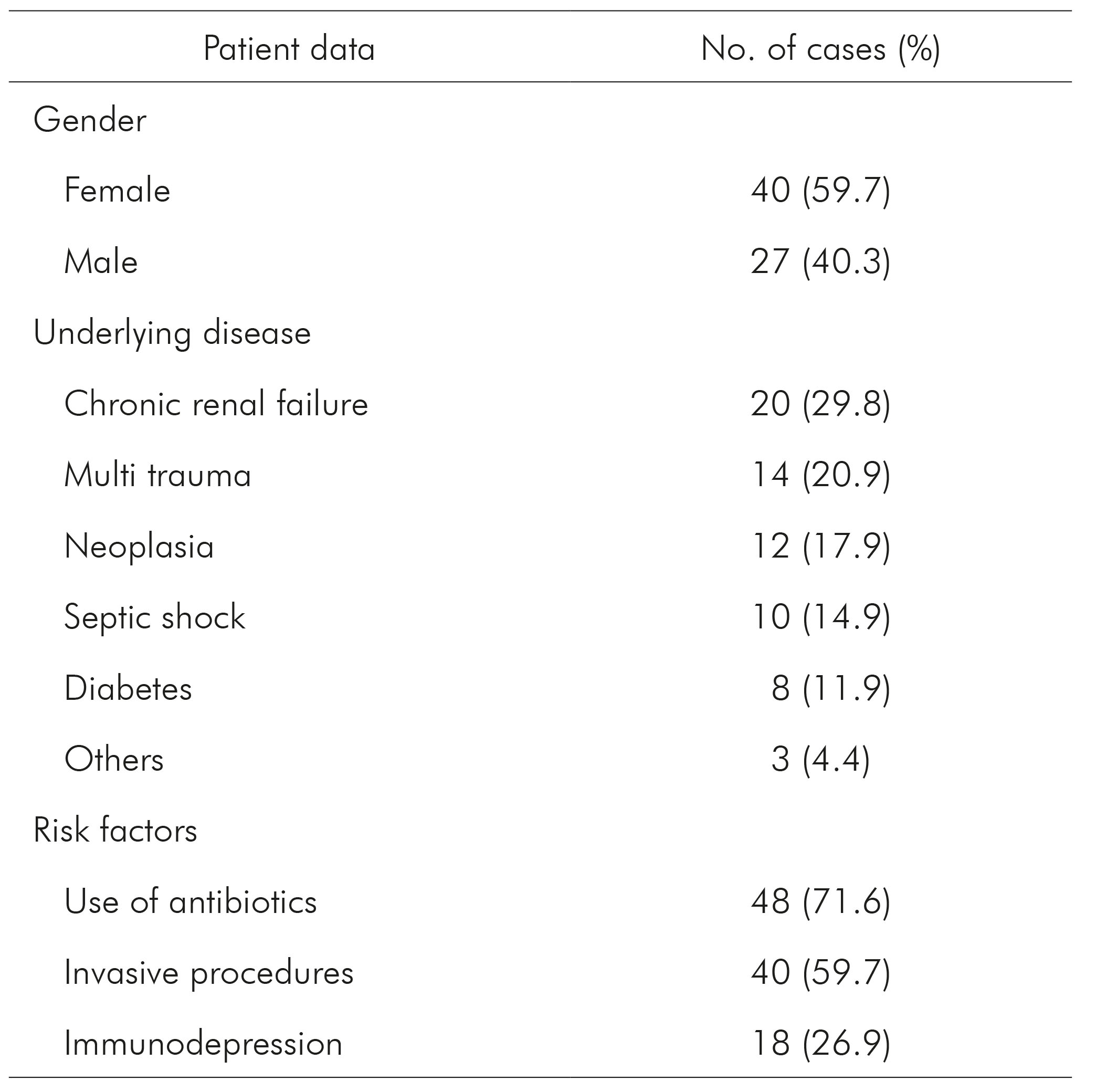
A comprehensive sampling of patient data such as gender, underlying diseases and risk factors is shown in table 1. This table shows higher rates in females, as well as highlighting the cases of chronic renal failure, multiple trauma and underlying pathologies like neoplasia. The use of antibiotics and invasive procedures is shown as the major risk factors for both colonization and infection.
Table 1 - Data of 67 patients admitted to the Hospital Universitário de Taubaté, Vale do Paraíba, São Paulo, Brazil, according to gender, underlying disease and risk factors
Of all isolates, the most frequent species was C. albicans (40%), whereas non-albicans Candida species were the most frequent in 71.5% of colonization cases and 52.2% of infection cases (Figure 1).
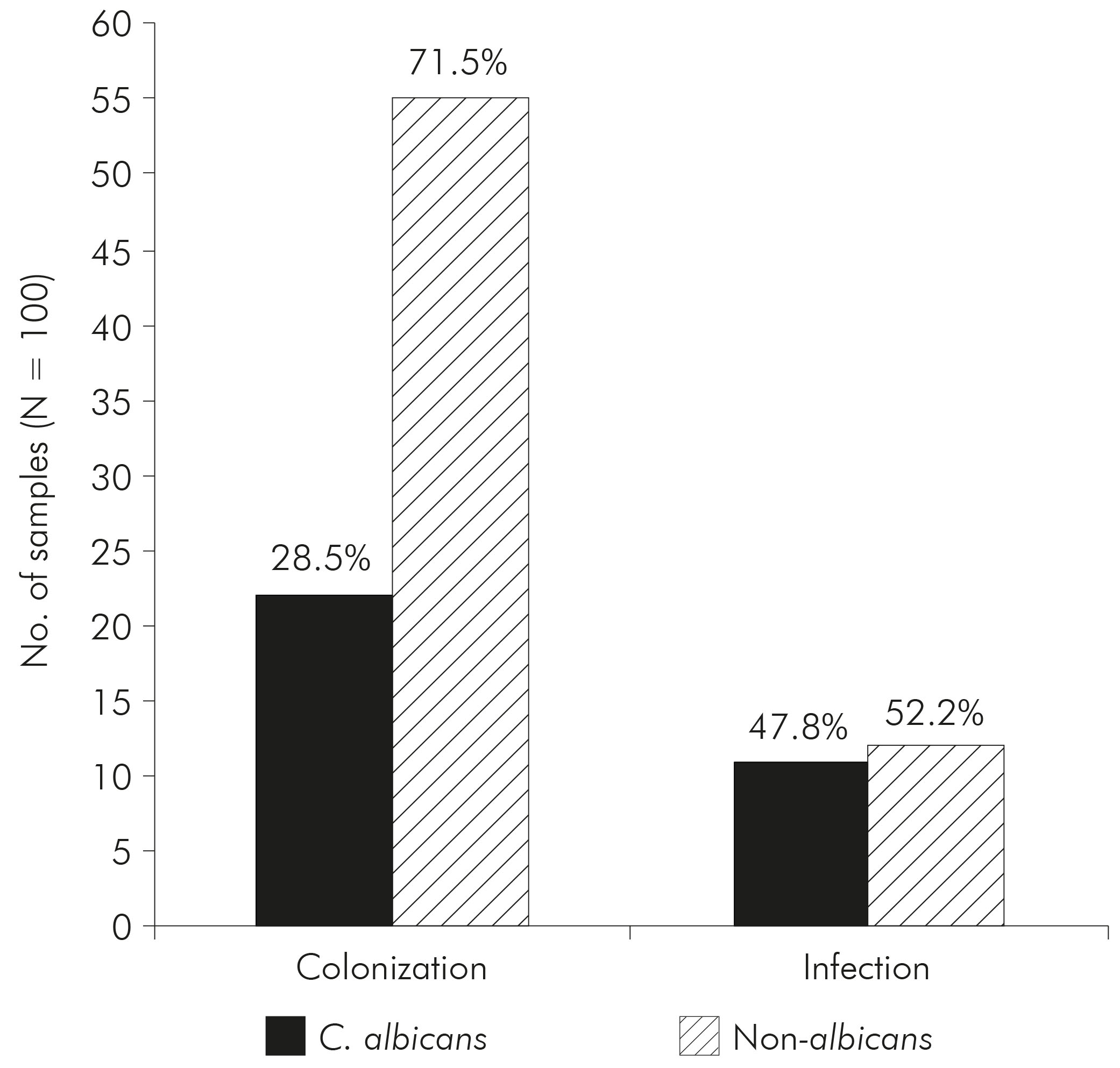
Figure 1 - Correlation of cases of nosocomial infection and colonization caused by C. albicans and non-albicans Candida species isolated from 67 patients admitted to the Hospital Universitário de Taubaté, Vale do Paraíba, São Paulo, Brazil
Tables 2 and 3 show that the majority of isolates for all species which occur from secretions and tip probes were predominantly cases of colonization. In addition, the table 3 shows that there was a predominance of C. albicans species in the secretions.
Table 2 - Occurrence and distribution of Candida species of hospital infection in clinical specimens and medical equipment in the Hospital Universitário de Taubaté, Vale do Paraíba, São Paulo, Brazil
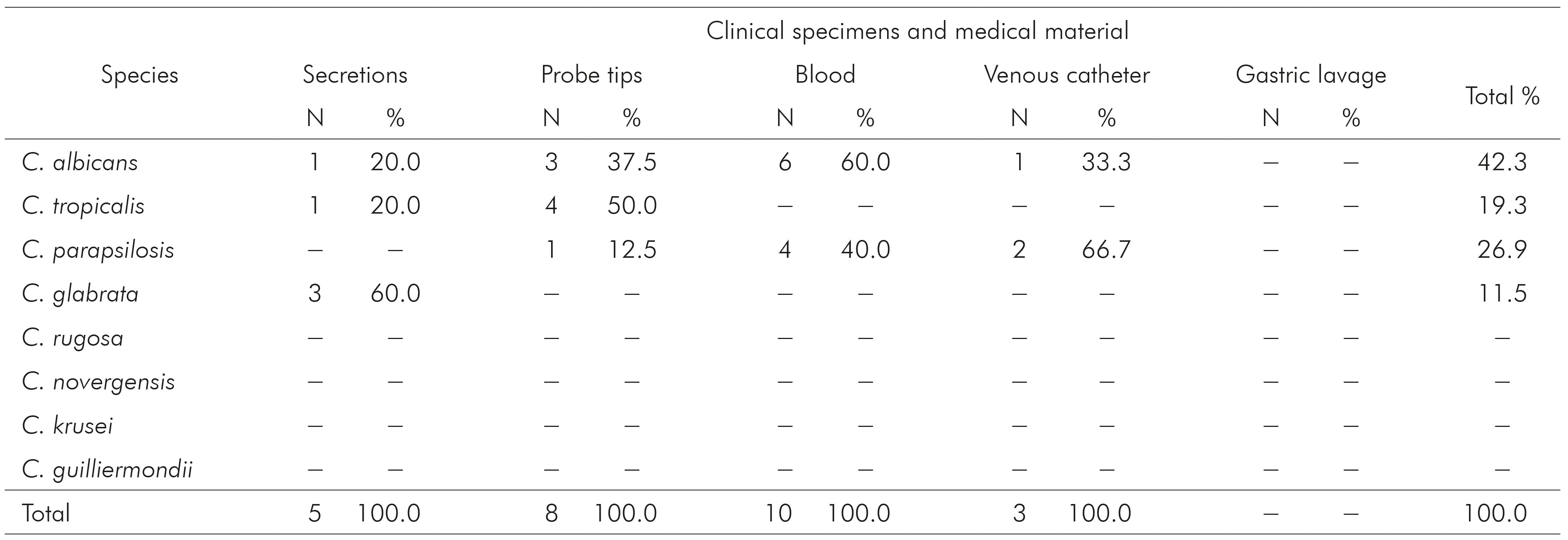
Conventional sign used: - Numeric data not equal to zero due to rounding.
Table 3 - Occurrence and distribution of Candida species of colonization in clinical specimens and medical equipment in the Hospital Universitário de Taubaté, Vale do Paraíba, São Paulo, Brazil

The hospital ward with the greatest number of Candida species isolations was the Intensive Care Unit (ICU), with 45% of isolates (Figure 2). In all hospital wards studied, the Candida species most frequently isolated was C. albicans.

Figure 2 - Distribution of 100 Candida spp. samples isolated from different clinical specimens and medical equipment, according to the hospital service, Hospital Universitário de Taubaté, Vale do Paraíba, São Paulo, Brazil
DISCUSSION
Candida yeasts are important due to the high frequency of colonization and infection in humans. During the period of this study, 100 samples of Candida were isolated from different medical equipment and clinical specimens of 67 patients admitted to different sectors of the hospital. Of this total, 26% were cases of infection and 74% were cases of colonization. Our results were similar to those found in the literature, which indicate that colonization by Candida is present in 5-15% of hospitalized patients but can reach extremes of 50-86%15.
Although exogenous nosocomial transmission by Candida has been reported, some studies showed that endogenous colonization is responsible for the large majority of severe candidiasis16,17. The colonization of multiple sites by Candida spp. is considered as a risk factor for the acquisition of invasive fungal infections in critically ill patients15. In this study, 65.2% of patients with acquired Candida infection had been previously colonized by this yeast. These data agree with other studies which reported that colonization by this fungus often precedes an invasive fungal infection15,18 and also revealed that most candidiasis were acquired by endogenous microbiota.
Early diagnosis of invasive candidiasis is difficult, usually reported at the end of the course of infection. This may be in part responsible for its high crude and attributable mortality rates19. In this study, the mortality rate among patients with Candida infection was 43.4%, a value that lies within the mortality rate attributed to this yeast, which is between 40-50%20, making this infection a major challenge for clinicians which work in tertiary hospitals in different countries.
In general, C. albicans was the most frequently isolated species, followed by C. tropicalis, C. parapsilosis and C. glabrata. There are significant geographical variations in the pattern of the Candida spp. strains isolated. While North America is noted to have a prevalence of C. glabrata, in South America there is a predominance of C. parapsilosis and C. tropicalis among non-albicans Candida species21. These data agree with the present study in relation to the main species isolated.
Non-albicans Candida species were predominated with 71.4% and 52.1% of the colonization cases and infection respectively, as the results of previous studies performed in tertiary hospitals in Brazil22,23,24,25.
There are few studies reporting the prevalence of Candida species related to candidiasis in different clinical samples. In the current study, C. albicans was the most frequently isolated species from blood and secretions, the latter being the source with the highest number of Candida spp. isolates. C. parapsilosis was the species most frequently found in venous catheter, confirming other studies that indicate that this species is the most important in candidemia24,26. C. tropicalis and C. glabrata were more common in the probe tips.
The ICUs were the hospital wards with the highest isolation of Candida spp. (45%). Invasive fungal infections, mainly cases of candidiasis, are very common in patients admitted to ICUs and are related to high mortality rates. Such patients, who are often critically ill, are more susceptible to colonization and hospital infection due to the severity of their condition and frequent invasive procedures27.
Risk factors associated with invasive candidiasis have been well established and have not changed substantially over the last two decades in relation to these factors, which include the exposure to broad-spectrum antibiotics, chemotherapy catheter, parenteral nutrition, neutropenia, hemodialysis, surgery and renal failure28. In this study, it was found that the use of broad-spectrum antibiotics, invasive procedures and immunosuppression were the main risk factors associated with cases of infection and colonization by Candida.
In terms of drug susceptibility, all the samples of C. albicans found in this study were susceptible to the antifungal agents tested, which is consistent with the information that this species is naturally susceptible to antifungal drugs for systemic use, although cases of acquired resistance to azoles have been reported29,30. The other Candida species have shown resistance to some antifungal drugs such as itraconazole. The C. glabrata species showed the greatest resistance, since this species is intrinsically less sensitive. Thus, it is extremely important to make the correct identification of the species in combination with the tests of susceptibility to establish the appropriate antifungal therapy.
CONCLUSION
This study presented epidemiological data of Candida infections at a university hospital in São Paulo State, which are important because it will be possible to compare them with future epidemiological surveillance at hospitals in that State, as well as other regions of Brazil. The presence of Candida yeast is still a common complication among patients admitted to tertiary hospitals, showing the importance of epidemiological investigations of these agents in this environment, especially about the appropriate preventive measures against such infections can be adopted.










 Curriculum ScienTI
Curriculum ScienTI